Abstract
Background
Coating prosthetic for hernia repair with a patient’s own cells could improve biocompatibility by decreasing inflammation and adhesion formation and by increasing tissue ingrowth and resistance to infection. The objective of this study was to prove the feasibility of prosthetic coating with stem cells and to assess its resistance to adhesion formation when implanted in an animal model.
Methods
Adult Lewis rat bone marrow stem cells were harvested and cultured. Stem cells were then implanted on three different prosthetics. The prosthetic with the best stem cell adherence was implanted intraperitoneally into six adult rats. Untreated prosthetic was implanted in control animals (n = 12). After 2 weeks, intra-abdominal adhesions were graded using an adhesion scoring scale by two surgeons who were blinded to the animal group. Data were analyzed using the Wilcoxon rank-sum test.
Results
Stem cells demonstrated the best adherence and growth on polyglactin prosthetics. After implantation, the stem cell-coated polyglactin prosthetic had <25% of its surface area covered with adhesions in five (83%) samples, whereas the control polyglactin group had only one sample (8.3%) with <25% adhesions, and seven of its samples (58.3%) had >50% surface area adhesions (p < 0.05).
Conclusions
The feasibility of hernia prosthetic coating with stem cells was demonstrated. Furthermore, stem-cell coated polyglactin prosthetic exhibited improved biocompatibility by decreasing adhesion formation in an animal model. Further study is needed to determine the factors that promote stem cell adherence to prosthetics and the in vivo prosthetic biomechanics after stem cell coating. This work is underway in our laboratory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The ideal prosthetic for hernia repair should promote tissue ingrowth, resist infection, and minimize adhesion formation and foreign body reaction. In addition, the prosthetic should retain its strength and biomechanical properties required for a durable hernia repair and maintain compliance for improved patient quality of life. Recent advances in prosthetic technology have included the development of lightweight polypropylene prosthetics that reduce the amount of inflammation and scarring compared with traditional heavyweight polypropylene prosthetics. There also are several composite prosthetics available that incorporate two different and opposing surfaces that take advantage of each surface’s engineered properties by promoting tissue ingrowth or providing an antiadhesive barrier. Several biologic bioprosthesis engineered from human or porcine acellular dermis, porcine small intestinal submucosa, and lyophilized acellular porcine dermal collagen and elastin also are commercially available.
Theoretically, if a prosthetic were coated with a tissue layer not recognized as foreign by the body’s immune system, such as a layer of its own cells, the prosthetic might be invisible to the immune system and result in improved biocompatibility. Advances in technology have made it possible to extract human mesenchymal stem cells from adipocytes [1]. Incorporating a patient’s own stem cells on currently available prosthetics for hernia repair may prevent or diminish the natural, foreign body immune response. Postoperatively, the stem-cell coated prosthetic would be recognized as “self,” thus minimizing the degree of inflammation, scarring, and intra-abdominal adhesion formation. In addition, the stem-cell coated biomaterial would provide a more functional scaffold that is capable of promoting ingrowth of fibroblasts, collagen deposition, neovascularization, and establishment of natural host defenses. The objective of this project was twofold: 1) to establish the feasibility of seeding a suitable prosthetic commonly used for hernia repair with mesenchymal stem cells; and 2) to test the hypothesis that stem-cell coated prosthetic implanted in vivo would lead to less intra-abdominal adhesion formation compared with that of uncoated mesh in control animals.
Methods
The experimental protocol was approved by our medical center’s Institutional Animal Care and Use Committee.
Establishing the feasibility of prosthetic coating
To establish the first objective of this study, we examined mesenchymal stem cell growth on three commonly used prosthetics: Ultrapro® (Ethicon, Inc., Cincinnati, OH); Vicryl® (Ethicon, Inc.); and Marlex® (C.R. Bard, Inc., Murray Hill, NJ). To obtain the rat’s mesenchymal stem cells, 1× phosphate-buffered saline (PBS) (Mediatech, Inc., Herndon, VA) was flushed through the cavity of the femurs and tibias of the Lewis rats. Collected bone marrow cells were plated into 75-cm2 flasks and cultured in low glucose (1 g/L) Dulbecco’s Modified Eagle’s Medium (Mediatech, Herndon, VA) supplemented with 10% fetal bovine serum (Sigma, St. Louis, MO) and antibiotics (100× antibiotic–antimycotic solution; Invitrogen, Grand Island, NY). Nonadherent cells were removed after 5 days, and the medium was replaced. Cells were analyzed by flow cytometry with CD29, 34, 45, and 90. Cells were CD34- and CD45-negative and 98% and 99% positive for CD29 and CD90, respectively.
To enable detection of cultured stem cells after in vivo implantation, cells were marked by introducing enhanced green fluorescent protein (EGFP) into their genome using a retroviral vector. This was necessary because we wanted to be able to differentiate the stem cells from surrounding cells within the prosthetic after implantation. The plasmid used for transfection was transformed and grown using E. coli and isolated through alkaline lysis. The isolated plasmid was then transfected into a packaging cell line (Ecopack2, Clonetech Need City) for packaging into a replication incompetent retrovirus (pLEG FPC-1, Clonetech Need City). The retroviral vector was then introduced into the target rat mesenchymal stem cells. Mesenchymal stem cell growth was observed with fluorescent microscopy to visualize expression of EGFP.
DAPI nuclear staining
DAPI (4,6-diamidine-2′-phenylindole dihydrochloride) nuclear staining was used to help visualize and demonstrate stem cell growth on each prosthetic. Before coating the prosthetic with the mesenchymal stem cells, it was pretreated with 4 ml of a solution containing 2.1 g of citric acid, 0.5 ml of Tween 20, and 100 ml of distilled water. In addition, the stem cells were incubated for 5 min at room temperature. The prosthetic was then treated with 24 ml of a solution containing 11.8 g of citric acid, DAPI, and 100 ml of distilled water. Excess liquid was removed and prosthetic observed under fluorescence microscopy.
Stem cell implantation
When we had isolated and identified mesenchymal stem cells, they were implanted on three different prosthetics. Lewis rat mesenchymal bone marrow stem cells were harvested by aspirating media from culture flasks. Five milliliters of Accutase (in Dulbecco’s PBS and 0.5 mM EDTA, Innovative Cell Technologies, San Diego, CA) was added to each flask to detach stem cells. The flasks were then incubated at 37°C in 5% CO2 for 5 min and shaken by hand to detach remaining stem cells, which were collected into 50-ml polypropylene conical tubes. All flasks were rinsed with 10 ml of Dulbecco’s 1× PBS and added to the 50-ml tubes. Culture media was then added to the tubes to 50 ml total volume. A cell count of a 100 μl aliquot was then performed. The Accutase/PBS/culture media was aspirated and stem cells resuspended in 5 ml of culture media for a total volume of 3.0 × 106 cells/ml. Preseeding of 3.0 × 106 stem cells onto Ultrapro®, Vicryl polyglactin 910®, and Marlex® was accomplished using a 4 × 4-cm pieces of prosthetic within a sterile field. Each prosthetic was placed in a 6-cm dish coated with methacrylate 12% in ethanol to prevent cell adherence to the dish. All dishes were placed in an incubator for 1 h at 37°C with 5% carbon dioxide. After 1 h, an additional 5 ml of media was added and incubated for 24 h.
Standard growth curve MTT assay
To determine the number of cells incorporated onto each prosthetic, a standard growth curve MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltertrazolium bromide) assay was performed on known quantities of stem cells from culture. Six different cell concentrations were plated (0, 1.25 × 104, 2.5 × 104, 5.0 × 104, 1.0 × 105, 2.0 × 105) with 2.5 ml of cell culture media. Plates were incubated at 37°C, 5% CO2 for 1 h. Five hundred microliters of cell titer was then transferred to each MTT well and reincubated for another hour. One milliliter of each solution was removed from each well and placed into a cuvette (Bio-Rab Laboratories, Hercules, CA) for reading on the spectrophotometer (Beckman DU-64, Fullerton, CA) at 490 nm. The optical density reading was then plotted versus cell number to obtain our standard growth curve.
MTT assays were performed on days 1, 3, 7, 11, and 14 for each prosthetic type used in the experiment to confirm adequate cell numbers for seeding. Each piece of prosthetic was removed from its original dish and placed in a sterile 10-cm dish with 12 ml of PBS (Sigma, St. Louis, MO). Prosthetic in PBS was placed on an Innova 2000 Platform Shaker at 60 rpm. After 5 min on the shaker, 5 ml of cell culture medium was added and placed on the orbital shaker on low power for 5 min. The medium was aspirated, and 5 ml of fresh cell culture medium and 1 ml of MTT reagent was added and incubated for 1 h. One milliliter aliquots were then added to a cuvette for spectrophotometer reading at 490 nm. Appropriate dilutions were made if needed to each aliquot with 1XPBS before reading.
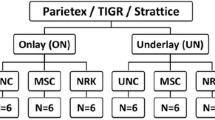
Animal studies
The experimental group of six rats underwent implantation of Vicryl Polyglactin 910® (PG) prosthetic that was preseeded with stem cells for 10 days. Twelve rats underwent implantation of the same prosthetic without stem cells and served as our control group. Each piece of control prosthetic was placed in a coated, 6-cm dish with 6 ml of media and maintained in the incubator for 10 days before implantation to match the preimplantation treatment of the stem cell-coated mesh group.
For the implantation of the prosthetic, inhaled isoflurane (continuously delivered mask inhalant 0.75% to 4.0%) was used as the anesthetic agent. Before incision, the abdomen was shaved free of hair and prepped with Betadine® and 70% alcohol solutions. A midline incision was made and the peritoneal cavity entered. A 2 cm × 2 cm piece of PG prosthetic, either from the experimental or control group, was then sutured to the anterior abdominal wall as an underlay away from the midline using interrupted 4-0 Goretex® sutures. The midline fascia was then closed with a running 3-0 PDS suture and the skin approximated with a slowly absorbable suture and surgical staples. Buprenex analgesia (0.5 mg/kg sq) was given every 6 h postoperatively as needed. Trained vivarium personnel observed all wounds daily and administered all analgesics. After 14 days the rats were euthanized. At necropsy, a midline incision was made and adhesions to each prosthetic were scored by two graders blind to the study group using the modified Diamond scale (Table 1). Each prosthetic was then excised en bloc with the abdominal wall. Each sample was divided in half for histological analysis.
Statistics
Descriptive statistics including means and standard deviations or counts and percentages were calculated. As the adhesion scores are measured on an ordinal scale, the Wilcoxon rank-sum test was used to compare the experimental and control groups. The SAS® software, version 9.1 (SAS Institute, Cary, NC), was used for the analysis. A p value < 0.05 was considered statistically significant.
Results
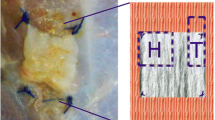
The standard growth curve that was generated using the MTT assay is shown in Fig. 1. Flow cytometry results confirmed stem cell purity (Fig. 2). No stem cell attachment was identified on Ultrapro®. Marlex® revealed maximal incorporation of stem cells at day 4 of incubation, whereas PG revealed the greatest quantity of stem cell incorporation on incubation day 10. Figure 3 shows the number of stem cells that were successfully incorporated into each prosthetic type over time. The successful incorporation of stem cells on the prosthetic was also confirmed by microscopy that helped visualize cell growth (Fig. 4) and fluorescent microscopy that helped visualize EGFP expression (Fig. 5) and DAPI staining (Fig. 6) on mesenchymal stem cells.
Polyglactin was chosen as the prosthetic for animal implantation, because it was able to incorporate the largest quantity of stem cells at day 10 of incubation. After 14 days, the explanted stem cell-coated PG prosthetic had <25% of the prosthetic surface area covered with adhesions in 83% of samples (5/6); the control PG group had only 1 sample (8.3%) with <25% adhesions, and 7 of its samples (58.3%) had >50% surface area adhesions (p < 0.05).
Discussion
In this study, we demonstrated the feasibility of incorporating mesenchymal stem cells onto a commonly used hernia prosthetic (Vicryl® mesh). We further documented that implantation of a stem cell-coated prosthetic intra-abdominally leads to fewer adhesions compared with a control group in a rat model.
The use of mesenchymal stem cells in medicine has gained much attention recently as a source of easily isolated cells with profound proliferative and regenerative capacities. After several early experiments documenting the potential benefit and applications of stem cells [2–7], Olivares et al. in 2004 described the transplantation of mesenchymal stem cells into infarcted rat myocardium with subsequent improved cardiac performance and histological evidence of regenerated myocardium and angiogenesis [8]. In addition, Shin et al. demonstrated the role of mesenchymal stem cells in tissue engineering by using a biodegradable scaffold with mesenchymal stem cells to aid in bone regeneration [9]. The authors were able to engineer an interconnected pore system within a novel biologic scaffold that allowed mesenchymal stem cell-derived osteoblasts to attach and aid in bone regeneration. Similarly, we report the first study to our knowledge of successful incorporation of stem cells on a commonly used prosthetic for hernia repair. Furthermore, we demonstrated that such incorporation varies based on mesh type. Although the Vicryl Polyglactin 910® prosthetic had the best stem cell attachment, stem cells attached to a lesser degree on Marlex® and not at all on the lightweight mesh (Ultrapro®). These differences are likely related to the unique composition and structure of these bioprosthetics. We elected to use these three prosthetics as scaffolds because of their porous structure that we believed would promote the incorporation of the mesenchymal stem cells. Marlex® is a macroporous, nonabsorbable, monofilament prosthetic made of polypropylene that weighs 80–85 g/m2 with a pore size of 1–2 mm. The rough surface of each individual polypropylene fiber and the texture of the fiber weave promote fibroblast proliferation and tissue ingrowth after implantation in humans. Kapischke et al. demonstrated the precoating of polypropylene prosthetic with living human fibroblasts adherent to polypropylene after 2 weeks of culture with gradual filling of the prosthetic interstices after 3 weeks of culture [10]. The authors acknowledged that collagen and other extracellular matrix components were required to negate the hydrophobic properties of polypropylene to allow fibroblast colonization. Despite these properties, we found that the incorporation of stem cells on this prosthetic was less than ideal and therefore decided not to use it for implantation in the animal model. The second prosthetic we used, Ultrapro®, is a lightweight, macroporous, composite prosthetic that weighs 28 g/m2 with 3- to 4-mm pore size that has been manufactured to reduce excessive inflammation, scarring, and stiffness without compromising the safety and effectiveness of hernia repair [11]. We were surprised to see no incorporation of stem cells on this scaffold. Possible factors for this phenomenon could include the large pore size of this prosthetic or the presence of the absorbable poliglecaprone-25 (copolymer containing glycolide and e-caprolactone) monofilament fibers in addition to the nonabsorbable polypropylene fibers. It is possible that a pore size threshold exists at which stem cell adhesion is impaired. We also cannot exclude a possible toxic or antiadhesive effect of the absorbable component of this prosthetic on the stem cells; however, further study is needed to evaluate this.
The Vicryl® knitted prosthetic that consists of polyglactin 910, which is an absorbable copolymer made from 90% glycolide and 10% L-lactide with an average pore size of 0.5 mm, demonstrated the best stem cell adherence. This prosthetic supported stem cell growth and was ready for implantation 11 days after seeding with purified rat bone marrow stem cells. This may not come as a surprise as the polylactic-co-glycolic acid (PLGA) polymer has been used before as a biologic scaffold in tissue engineering for proliferation of mesenchymal tem cells, chondrocytes, and osteogenic cells [2, 3, 12]. Kyzer et al. successfully coated polyglycolic acid prosthetic with fibroblasts before implantation into rats and showed increased levels of hydroxyproline content at 14 days [4]. Kay et al. showed that the PLGA polymer’s hydrophobicity limited adhesion, proliferation, and function of osteoblasts and chondrocytes [5]. Newer studies have chemically modified the PLGA polymer with NaOH treatment or galactose to enhance cellular adhesion and function [6, 7]. Other studies have tethered ligands and signaling growth factors to the polymer to promote cell proliferation and differentiation [12].
Given the results of our study, it may be concluded that the pore size of the prosthetic may be the determining factor of stem cell adherence to the prosthetic, because the best incorporation (Vicryl®) had the smallest pore size (0.5 mm), the one (Ultrapro®) with no adhesion had the largest (3–4 mm), and the intermediate pore size mesh (Marlex® 1–2 mm) demonstrated intermediate adhesiveness.
Our study also confirmed our second hypothesis regarding reduced adhesion formation to the stem cell-coated mesh after implantation. The reduced formation of adhesions is indicative of less inflammation induced by the prosthetic possibly due to the presence of its own cells on the coated prosthetic that minimize the foreign body reaction. This finding may have important implications for hernia repair. If the presence of own stem cells on the prosthetic minimizes adhesion formation then this may decrease bowel obstruction and fistulization. Furthermore, the decreased foreign body reaction also may prevent the excessive fibrosis that leads to a change in abdominal wall compliance and sense of stiffness and discomfort for the patient and is more pronounced after the implantation of heavier weight and smaller pore size prosthetic [13].
Our findings are promising; however, further study is needed to better understand the factors that augment or inhibit stem cell growth on prosthetics and if this differentiation can be induced or driven by soluble growth factors or tissue engineered biologic scaffolds. A better understanding may make it possible to grow stem cells on other commonly used prosthetics or may lead to the development of new prosthetics that offer an ideal scaffold for the growth of stem cells. The structural changes of the stem cell-coated prosthetic over time and its incorporation into the host tissues, including tensile strength and compliance testing, needs further study. Ultimately, this concept needs to be evaluated in the human as current studies have shown that mesenchymal stem cells are able to provide a patient with an autologous source of multipotent cells.
Conclusions
Mesenchymal stem cells can successfully incorporate onto Vicryl® prosthetic and reduce the quantity of intraabdominal adhesions in a rat model. Mesenchymal stem cells may diminish the foreign body response to hernia prosthetics and provide enhanced biocompatibility with improved patient quality of life. Further study is needed and is currently underway in our laboratory.
References
Fraser JK, Schreiber R, Strem B, Zhu M, Alfonso Z, Wulur I, Hedrick MH (2006) Plasticity of human adipose stem cells toward endothelial cells and cardiomyocytes. Nat Clin Pract Cardiovasc Med 3(Suppl 1):S33–S37
Fan H, Hu Y, Zhang C, Li X, Lv R, Qin L, Zhu R (2006) Cartilage regeneration using mesenchymal stem cells and a PLGA-gelatin/chondroitin/hyaluronate hybrid scaffold. Biomaterials 27:4573–4580
Wu W, Feng X, Mao T, Feng X, Ouyang HW, Zhao G, Chen F (2007) Engineering of human tracheal tissue with collagen-enforced poly-lactic-glycolic acid non-woven mesh: a preliminary study in nude mice. Br J Oral Maxillofac Surg 45:272–278
Kyzer S, Kadouri A, Levi A, Ramadan E, Levinsky H, Halpern M, Chaimoff C (1997) Repair of fascia with polyglycolic acid mesh cultured with fibroblasts–experimental study. Eur Surg Res 29:84–92
Kay S, Thapa A, Haberstroh KM, Webster TJ (2002) Nanostructured polymer/nanophase ceramic composites enhance osteoblast and chondrocyte adhesion. Tissue Eng 8:753–761
Park GE, Pattison MA, Park K, Webster TJ (2005) Accelerated chondrocyte functions on NaOH-treated PLGA scaffolds. Biomaterials 26:3075–3082
Yoon JJ, Nam YS, Kim JH, Park TG (2002) Surface immobilization of galactose onto aliphatic biodegradable polymers for hepatocyte culture. Biotechnol Bioeng 78:1–10
Olivares EL, Ribeiro VP, Werneck de Castro JP, Ribeiro KC, Mattos EC, Goldenberg RC, Mill JG, Dohmann HF, dos Santos RR, de Carvalho AC, Masuda MO (2004) Bone marrow stromal cells improve cardiac performance in healed infarcted rat hearts. Am J Physiol Heart Circ Physiol 287:H464–H470
Shin M, Abukawa H, Troulis MJ, Vacanti JP (2007) Development of a biodegradable scaffold with interconnected pores by heat fusion and its application to bone tissue engineering. J Biomed Mater Res A 84A:702–709
Kapischke M, Prinz K, Tepel J, Tensfeldt J, Schulz T (2005) Precoating of alloplastic materials with living human fibroblasts: a feasibility study. Surg Endosc 19:791–797
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12:63–69
Liu HW, Chen CH, Tsai CL, Lin IH, Hsiue GH (2007) Heterobifunctional poly(ethylene glycol)-tethered bone morphogenetic protein-2-stimulated bone marrow mesenchymal stromal cell differentiation and osteogenesis. Tissue Eng 13:1113–1124
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V (2002) Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 103:208–214
Acknowledgments
This study was in part funded by the Society of American Gastrointestinal and Endoscopic Surgeons.
Disclosures
Drs. Charles J. Dolce, Dimitrios Stefanidis, Jennifer E. Keller, K. Christian Walters, William L. Newcomb, H. James Norton, Amy E. Lincourt, Kent W. Kercher, B. Todd Heniford, and Jessica J. Heath, have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dolce, C.J., Stefanidis, D., Keller, J.E. et al. Pushing the envelope in biomaterial research: initial results of prosthetic coating with stem cells in a rat model. Surg Endosc 24, 2687–2693 (2010). https://doi.org/10.1007/s00464-010-1026-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1026-x