Abstract
Background
Fast-track (FT) recovery protocols have demonstrated advantages over historical recovery routines after open colectomy; however, their impact in recovery after laparoscopic colectomy is not clearly defined. This study was designed to determine whether patients who recover on FT protocol after laparoscopic colectomy have a shorter length of stay (LOS) and fewer complications compared with patients who recover on standard (non-FT) protocol.
Methods
A cohort of consecutive patients with colon cancer who underwent completed laparoscopic-assisted right hemicolectomy from 2005–2007 was identified. Univariate and multivariate logistic analyses were performed to identify risk factors for increased LOS and postoperative complications with recovery protocol as the primary predictor.
Results
A total of 197 patients were included: 115 (58%) patients recovered on a non-FT protocol, and 82 (42%) patients on FT protocol. Univariate analysis showed no differences with respect to age, gender, body mass index, or American Society of Anesthesiologists (ASA) class between groups. The median (interquartile range) LOS was 4 (range, 3–6) days and 3 (range, 3–4) days for the non-FT and FT recovery patients, respectively (p < 0.001). On multivariate analysis, independent risk factors for increased LOS were complications (p < 0.001) and non-FT recovery (p = 0.007). Non-FT recovery also was associated with increased complications (56 vs. 29%, p = 0.0002); this remained significant on multivariate analysis (p < 0.001). Readmissions were similar (p = 1.0) between recovery groups. No mortalities were observed at 30 days.
Conclusions
Fast-track recovery is independently associated with a shorter LOS and decreased morbidity after laparoscopic right hemicolectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the era of evidence-based medicine, the efficacy of traditional recovery regimens have been questioned by fast-track (FT) and enhanced recovery (EHR) protocols, which were first developed and implemented in Europe [1, 2]. These protocols theoretically minimize physiologic alterations during the perioperative period, thus enabling a decreased hospital length of stay (LOS). The key components of these protocols are delineating patient expectations, avoidance of nasogastric (NG) tubes and preoperative bowel cleansing, appropriate analgesia, early oral feeding and ambulation, limitation of fluid shifts, and early discontinuation of bladder catheters, and avoidance of transabdominal drains.
Regarding these specific practices, a recent Cochrane systematic review assessed 13 randomized, controlled trials and evaluated early commencement of feeding, one of the key elements of FT protocols. It concluded that early feeding is safe and that it reduces the risk of postoperative complications [3]. Moreover, a systematic review of enhanced recovery programs concluded that these regimens are safe and do shorten postoperative LOS after open colectomy [4].
In addition to changes in postoperative recovery practices, minimally invasive surgical techniques, such as laparoscopy, have altered expectations and postoperative treatment of patients. Laparoscopic (LAP) colectomy is clearly associated with many advantages over open techniques, including reduced postoperative pain, earlier recovery of bowel function with earlier resumption of diet, and shorter LOS [5, 6]. Many of the elements of FT protocols, such as avoidance of NG tubes and bowel preps, have already been integrated into the recovery regimens of LAP patients [7, 8]. These changes in recovery raise the question as to whether FT recovery protocols will be of any added value in recovery after LAP colectomy. Results obtained with FT protocols after open colectomy have been shown to be similar to those of LAP patients who undergo standard, non-FT recovery [9, 10]. To date, the recovery of LAP patients on FT protocols has been insufficiently studied.
We hypothesized that adding FT recovery to a LAP approach will further enhance recovery and lead to shorter LOS and fewer complications. Therefore, the goal of this study was to examine the impact of FT recovery protocol after LAP right hemicolectomy for colon cancer with the primary endpoints of LOS and postoperative morbidity.
Methods
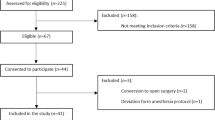
After Institutional Board Review approval, we performed a query of a prospectively maintained divisional database to identify all patients who underwent elective LAP-assisted right hemicolectomy for colon cancer between January 1, 2005 and December 31, 2007 at our institution. Patients who underwent hand-assisted laparoscopic surgery (HALS) or who underwent conversion to laparotomy were excluded. Demographic, treatment, and outcome variables were independently reviewed for accuracy.
Patients were categorized into two groups (non-FT and FT) based on their preoperatively assigned recovery protocol. During mid 2006, a standardized FT order set became available within our division. After this date the FT order set was routinely used by four surgeons and never used by three surgeons. All consecutive patients who underwent laparoscopic assisted right hemicolectomy for cancer and who were placed on this protocol preoperatively comprised the FT group. The non-FT group include all (n = 62) patients before 2006 (i.e., before FT was available), 24 patients of the three surgeons who never used fast track order sets, and 29 patients of surgeons who used FT but for whom the FT order set was not completed preoperatively and thus fell into the non-FT group.
The FT orders were signed preoperatively; thus, patients were assigned to the FT or standard (non-FT) recovery protocols before undergoing surgery. The seven specific components of the FT protocol include: (1) preoperative patient education regarding to expectations of surgery and of recovery, i.e., the components of the FT protocol; (2) no bowel preparation; (3) analgesia with routine oral nonsteroidal anti-inflammatory medications and minimization of opioid pain management; (4) discontinuation of NG by the morning of postoperative day 1; (5) early feeding beginning on postoperative day 1 with 800-ml full liquid diet with advancement to soft diet on postoperative day 2; (6) enforced ambulation on the day of surgery; and (7) removal of the bladder catheter on postoperative day 1.
Standard recovery included routine bowel preparation, NGT use, and diet advancement from clears to soft diet according to surgeon preference. Both protocols have the same discharge criteria, which are defined as: patient tolerating a soft diet for >8 hours with evidence of return of bladder and bowel function (gas or stool), adequate pain control (visual analog scale score <5), and no evidence of surgical complication.
Differences in clinically important baseline characteristics and postoperative outcomes were compared between the non-FT and FT cohorts by using univariate analysis using Student’s t test for continuous variables, and χ2 for binary variables. For the comparative analyses, our primary endpoint was increased LOS. Increased LOS was defined as ≥4 days, based on a median split of the combined LOS for both groups. A univariate analysis was performed to identify risk factors for increased LOS, followed by multivariate logistic analysis with recovery protocol as the primary predictor. Separate univariate and multivariate logistic regression analyses, in which the endpoint was the occurrence of any postoperative complication, also were performed to identify variables associated with complications.
For all analyses, p values ≤0.05 were considered statistically significance, and all tests were two-sided. Univariate results are reported as median (interquartile range) or frequency (percent); multivariate results are reported as odds ratios (OR) with 95% confidence intervals (CI).
Results
During a 2-year period, a total of 197 patients underwent LAP-assisted right hemicolectomy for colon cancer and were included: 115 patients (58%) recovered on a standard protocol (non-FT), and 82 (42%) patients recovered on the FT protocol. Baseline characteristics of the two recovery protocol groups are shown in Table 1. Patients who were assigned to recover on FT and non-FT protocols were not significantly different with respect to age, gender, body mass index (BMI), and American Society of Anesthesiologists (ASA) status.
Short-term outcomes are shown in Table 2. The FT group had earlier tolerance of soft diet (day 2 vs. day 3, p = 0.0001), earlier bowel movement (day 2 vs. day 3, p = 0.005), shorter LOS (3 vs. 4 days, p = 0.0004), and had fewer postoperative complications (29 vs. 56% p = 0.0002) than the non-FT group. There was no difference in the proportion of patients who required postoperative NGT insertion (10 vs. 8%, p = 0.66) or readmission (2.3 vs. 2.9%, p = 1.0) between the two recovery groups.
On univariate analysis, the following variables were shown to be risk factors for increased LOS (Table 3): age, ASA class 3 or 4, complications, and non-FT recovery. On multivariate logistic regression analysis both complications and non-FT recovery remained independently associated with increased LOS (Table 3).
To assess the relationship between type of recovery protocol and postoperative complications, univariate and multivariate logistic analyses of risk factors associated with complications was performed (Table 4). On univariate analysis, age, ASA class 3/4, and non-FT recovery were all risk factors for postoperative complications. However, on multivariate analysis only ASA class 3/4 and non-FT recovery remained independent risk factors for postoperative complications (p = 0.002 and p = 0.0008, respectively).
Specific complications are listed in Table 5. FT patients were significantly less likely to experience hypovolemia requiring fluid boluses, hyper-/hypokalemia, volume overload requiring diuretics, and wound infections. There was no statistical significant difference between the FT and non-FT groups in anastomotic leak rates, intra-abdominal abscesses and readmissions, and there was no mortality within 30-days in this series.
Discussion
The findings of our study suggest that FT recovery not only resulted in a shorter LOS but also was associated with fewer observed complications in those patients assigned to undergo FT recovery. These results agree with other reports that claim advantages of FT recovery programs after open colonic surgery [2, 11]. This series, however, is one of the first reports to date to compare non-FT to FT recovery after laparoscopic colectomy in a large patient cohort who underwent a single operation type for a single disease process.
Although FT recovery practices are advocated by several authors to reduce postoperative morbidity and enable earlier patient discharge, the benefit of these protocols often is questioned due to lack of standardization, protocol variability, and failure to match patients with similar operations and disease processes [4, 9, 10]. To further complicate the matter, certain aspects of FT protocols have already been incorporated in modern evidence-based standard recovery regimens.
In our institution we clearly define the FT recovery protocol and discharge criteria to our patients preoperatively and educate them about our multimodal approach. Our FT protocol is standardized in a perioperative order set, which is in placed preoperatively. Surgeons, anesthesiologists, nurses, and house and ancillary staff follow the same protocol and discharge criteria with little to no variation. In addition this protocol was instituted during the study period and was routinely utilized.
In our study implementation of FT recovery regimen was associated with earlier return of gastrointestinal function and tolerance of diet (p = 0.0001) for the FT group compared with the non-FT group. Furthermore, patients of the FT group had decreased LOS and postoperative morbidity compared with the non-FT group. Notably these results were obtained without any apparent increase in the rate of readmission in the FT group. These results highlight the fact that FT routines can provide additive patient benefit to the laparoscopic approach.
Our findings are in agreement with the results of a clinical trial that demonstrated that FT multimodal rehabilitation programs further enhanced postoperative recovery after laparoscopic sigmoidectomy [12]. Although our results agree with their conclusions, our study is of a larger cohort of patients who underwent the same operation for a single disease process.
As expected, postoperative morbidity was associated with advanced ASA class, whereas FT recovery was independently associated with decreased risk for the occurrence of postoperative complications. This suggests that FT recovery could potentially have a role in improving outcomes for the high-risk patient. Although we cannot draw conclusions at this juncture on the cause of increased wound infections in the non-FT group, which is likely multifactorial, we can only speculate that a prolonged stay in the hospital renders patients susceptible to infections.
Several limitations of this study merit discussion. Patients were assigned to FT vs. non-FT recovery in an uncontrolled, nonrandomized manner; however, in general this assignment was a temporal issue during our study period and does not represent a difference in patient demographics or surgeon use. Despite adjustment for baseline differences in clinically important variables between recovery groups in our statistical models, such as ASA class, the possibility exists that the differences observed in this study were due to other nonmeasured confounding variables. As a tertiary referral center, referral bias may limit the generalizability to nonacademic centers or those without a similar level of complexity and volume of laparoscopic colorectal surgery. Due to the retrospective nature of our study protocol compliance was not assessed; our analysis used an intention-to-treat approach based on assigned recovery protocol, which represents what can reasonably be expected for patients who are assigned to FT recovery protocols. Despite these limitations, this study demonstrates clinically important results and is one of the largest to date that quantifies the impact of recovery protocols after laparoscopic colectomy on LOS and morbidity.
In summary laparoscopic right hemicolectomy patients who are preoperatively assigned to recover on a FT protocol are observed to have a decreased LOS and morbidity compared with those who recover on a standard recovery regimen. In this series, other independent predictors of increase LOS included the occurrence of postoperative complications, whereas higher ASA status and non-FT recovery were independently associated with increased morbidity.
References
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Basse L, Thorbol JE, Lossl K, Kehlet H (2004) Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum 47:271–277 (discussion 277-278)
Andersen HK, Lewis SJ, Thomas S (2008) Early enteral nutrition within 24 h of colorectal surgery versus later commencement of feeding for postoperative complications [review]. The Cochrane Library 2008, Issue 2:1–25
Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, Gouma DJ, Bemelman WA (2006) Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg 93:800–809
Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287:321–328
Noel JK, Fahrbach K, Estok R, Cella C, Frame D, Linz H, Cima RR, Dozois EJ, Senagore AJ (2007) Minimally invasive colorectal resection outcomes: short-term comparison with open procedures. J Am Coll Surg 204:291–307
Vermeulen H, Storm-Versloot MN, Busch OR, Ubbink DT (2006) Nasogastric intubation after abdominal surgery: a meta-analysis of recent literature. Arch Surg 141:307–314
Bucher P, Mermillod B, Gervaz P, Morel P (2004) Mechanical bowel preparation for elective colorectal surgery: a meta-analysis. Arch Surg 139:1359–1364 (discussion 1365)
Basse L, Hjort Jakobsen D, Billesbolle P, Werner M, Kehlet H (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232:51–57
Basse L, Jakobsen DH, Bardram L, Billesbolle P, Lund C, Mogensen T, Rosenberg J, Kehlet H (2005) Functional recovery after open versus laparoscopic colonic resection: a randomized, blinded study. Ann Surg 241:416–423
Senagore AJ, Duepree HJ, Delaney CP, Brady KM, Fazio VW (2003) Results of a standardized technique and postoperative care plan for laparoscopic sigmoid colectomy: a 30-month experience. Dis Colon Rectum 46:503–509
Raue W, Haase O, Junghans T, Scharfenberg M, Muller JM, Schwenk W (2004) ‘Fast-track’ multimodal rehabilitation program improves outcome after laparoscopic sigmoidectomy: a controlled prospective evaluation. Surg Endosc 18:1463–1468
Disclosures
Drs. Tsikitis, Holubar, Dozois, Cima, Pemberton, and Larson have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsikitis, V.L., Holubar, S.D., Dozois, E.J. et al. Advantages of fast-track recovery after laparoscopic right hemicolectomy for colon cancer. Surg Endosc 24, 1911–1916 (2010). https://doi.org/10.1007/s00464-009-0871-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0871-y