Abstract
Background
Surgical impact may be associated with enhanced tumor growth and chemoresistance. This study aimed to evaluate the effect of surgical impact on the mRNA expression of survivin, epidermal growth factor receptor (EGFR), and human epidermal receptor (HER2) in tumors after pneumoperitoneum versus laparotomy.
Methods
Nude mice were inoculated intraperitoneally with human gastric cancer cells (MKN45). Then laparotomy, carbon dioxide (CO2) pneumoperitoneum, and anesthesia alone were performed randomly, after which EGFR, HER2, and survivin mRNA expression using reverse transcription-polymerase chain reaction (RT-PCR) was evaluated.
Results
The expression of EGFR and HER2 mRNA increased significantly after the experiment. However, it was higher after laparotomy than after CO2 pneumoperitoneum at almost all examined time points. Survivin mRNA expression increased significantly in the first 48 h, then returned to the control level. It was higher after laparotomy than after CO2 pneumoperitoneum 48 h after the surgical procedures.
Conclusion
The expression of EGFR, HER2, and survivin increased after each surgical procedure. However it was lower after CO2 pneumoperitoneum than after laparotomy. This might be associated with changes in the chemosensitivity of the remnant cancer cells after surgery, supporting the use of minimally invasive surgery for cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgery is accepted worldwide as an essential method for treating gastrointestinal malignant tumors. At the same time, the survival benefits for patients undergoing adjuvant chemotherapy after surgery are well known [1, 2]. Recently, molecular cancer-targeting agents such as trastuzumab (Herceptin) for Her2 inhibition and cetuximab for epidermal growth factor receptor (EGFR) inhibition have been developed and used with anticancer agents for the control of dormant cancer cells after surgery [3–5].
Surgical impact may be associated with enhanced postoperative tumor growth and chemoresistance. Recently, postoperative enhancement of the resistance to chemotherapy has been reported [6]. Additionally, alterations in apoptosis induced by surgical stress and chemotherapeutic agents have been noted repeatedly during the postoperative period [7, 8].
The system represented by EGFR, human epidermal receptor (HER2), and survivin interferes with chemotherapeutic agents, which depend on apoptosis in their action. Both EGFR and HER2 are transmembrane tyrosine kinase receptors and members of the EGFR family. The binding of different legends to their extracellular domain initiates a signal transduction cascade that can affect many aspects of tumor cell biology including cell proliferation, apoptosis, adhesion, migration, and differentiation [9, 10].
Survivin is a well-known inhibitor of apoptosis protein. It is expressed in solid tumors such as those of lung, esophagus, stomach, colon, pancreas, and breast, but it is almost not found in normal adult tissues [11]. Upregulation of survivin plays a vital role in resistance to chemotherapy and radiotherapy [12]. Survivin has the ability to inhibit apoptosis via the inhibition of caspase-3, -7, and -9 in cells [13–18]. Findings have shown that the survivin level is upregulated by the expression of HER2 and EFGR via activation of the phosphoinositide 3 kinase (PI3 K)-signaling pathway. Conversely, survivin level and apoptosis resistance are decreased when cells are treated with the HER2-specific inhibitor, Herceptin [3, 19].
To clarify the impact of surgical procedures on the mRNA expression of EGFR, HER2, and survivin, we evaluated their levels in tumors after carbon dioxide (CO2) pneumoperitoneum versus laparotomy in a nude mouse model with peritoneal dissemination of human gastric carcinoma.
Materials and methods
Cell preparation
All cell culture reagents were purchased from Gibco BRL, Life Technologies (Rockville, MD, USA). The MKN45 poorly differentiated human gastric carcinoma cell line was grown in RPMI 1640 medium supplemented with 10% fetal bovine serum and an antibiotic/antimycotic agent containing 100 IU/ml of penicillin, 0.1 mg/ml of streptomycin, and 2.5 × 10−4 mg/ml of amphotericin B. The cells were cultured in dishes in a 5% CO2 atmosphere at 37°C.
To prepare tumor cells for inoculation, cells in the exponential growth phase were harvested by 0.25% trypsin-ethylenediaminetetraacetic acid (EDTA), then washed and resuspended in phosphate-buffered saline (PBS). Cell viability was determined by trypan blue exclusion, and only single-cell suspensions of more than 90% viability were used.
Animal models
Male 6- to 7-week-old BALB/c nude mice were obtained from Seac Yoshitomi (Tokyo, Japan) and maintained under specific pathogenic-free laboratory conditions. All procedures were performed according to the Animal Experimentation and Ethical Guidelines of Oita University. The animals were kept 1 week before tumor inoculation, and the animal weight was 25 to 30 g at that time.
To make the murine peritoneal dissemination model, the mice were intraperitoneally injected with MKN45 cells (3 × 106 cells) as previously described [20]. Then the mice were exposed to laparotomy, CO2 pneumoperitoneum, or anesthesia alone (35 mice per each group), or used as a control condition (5 mice).
Using adhesive tape, the mice were fixed to the operating table in a supine position. In the laparotomy group, after anesthesia, a 3-cm laparotomy was made along the midline. Abdominal contents were exposed for 25 min. Then the incision was closed using polyglycolic acid sutures 3-0, and the animal was allowed to recover. In the CO2 pneumoperitoneum group, CO2 pneumoperitoneum was created and maintained for 25 min under pressure of 7- to 10-cm H2O as previously reported, and this pressure was tolerated by the mice [21]. In the anesthesia group, each mouse underwent only diethyl ether anesthesia for 25 min. In the control group, the mice were killed immediately with diethyl ether overinhalation.
The effect of surgical procedures on survivin, EGFR, and HER2 mRNA expression in peritoneal tumors was evaluated. On day 21 after preparation of the peritoneal dissemination model, the mice were exposed to laparotomy, CO2 pneumoperitoneum, anesthesia only, or immediate killing without any surgical procedure. After 1, 6, and 48 h and 1 and 2 weeks, the animals (7 mice per time point) were killed, and tumor nodules were collected. All nodules were frozen immediately in liquid nitrogen, then stored at –80°C.
Analysis of EGFR, HER2, and survivin mRNA expression by reverse transcription-polymerase chain reaction (RT-PCR)
Briefly, total RNA from tumor tissue in the parietal peritoneum (subcutis) was isolated by an automated procedure using the BioRobot EZ1 RNA tissue Mini Kit (Qiagen, Tokyo, Japan) according to the manufacturer’s instructions, and purified total RNA was stored at –80°C. Total RNA (1 μg) was reverse transcribed at 22°C for 10 min, then at 37°C for 60 min and 80°C for 5 min. Amplification with specific primers for human EGFR, HER2, survivin, and glyceraldehyde-3 phosphate dehydrogenase (GAPDH) was performed (1 min at 94°C for denaturing, 1 min at 54°C [GAPDH], 56°C [EGFR], 55°C [HER2], or 60°C [survivin] for annealing, and 1 min at 72°C for extension, for 33 cycles). The primer sequences used were those shown in Table 1 [22–24]. The amplified products were electrophoresed with 6× Loading Buffer Triple Dye (Wako, Nippon Gene, Tokyo, Japan) on 1.8% agarose gels, with GAPDH used as an internal control and for estimating mRNA-relative expression. Bands were analyzed using scanning densitometry by image J analysis software (U.S. National Institutes of Health, Bethesda, MD, USA).
Statistical analysis
Survivin, EGFR, and HER2 mRNAs were expressed as a ratio to GAPDH mRNA. The data then were expressed as mean ± standard deviation. Associations between variables were tested using analysis of variance (ANOVA). The groups then were compared post hoc using Student’s t-test. A p value less than 0.05 was considered statistically significant.
Results
Expression of EGFR mRNA after surgical procedures
Using RT-PCR, we examined EGFR mRNA expression in the parietal peritoneal tumors after laparotomy versus CO2 pneumoperitoneum. In the laparotomy and CO2 pneumoperitoneal groups, EGFR mRNA expression started to increase 1 h after the experiment and then continued to increase progressively until 48 h. After that, EGFR mRNA expression in both groups started to decrease. However, they did not reach the control level until the end of the 2-week observation period.
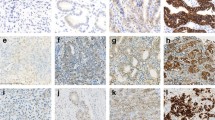
At all check points, a significant difference in EGFR mRNA expression was observed between both treatment groups and the control group (p < 0.1). Moreover, EGFR mRNA expression was significantly higher 1 h (p < 0.05), 6 h, 48 h, and 1 week (p < 0.01) after laparotomy than after CO2 pneumoperitoneum. No significant difference was found between laparotomy and CO2 pneumoperitoneum 2 weeks after surgery. In the anesthesia-only group, the expression of EGFR mRNA was significantly higher than in the control group 1 h after the experiment (p < 0.01), then started to decrease toward the control level soon after the 6-h point (Fig. 1A, B).
Relative expression of epidermal growth factor receptor (EGFR) mRNA in human gastric tumors after carbon dioxide (CO2) pneumoperitoneum and laparotomy in tumor-bearing mice (7 mice per each time point, 5 control mice). A Reverse transcription-polymerase chain reaction (RT-PCR) representation. B Time course after the experiment. *p < 0.05. **p < 0.01 (compared with laparotomy). ‡ p < 0.01 (compared with the control group). L laparotomy; P or pneumo CO2 pneumoperitoneum; C control; NS not significant
Expression of HER2 mRNA after surgical procedures
We examined HER2 mRNA expression by RT-PCR and found that it started to increase significantly in the laparotomy and CO2 pneumoperitoneal groups 1 h after the experiment, then continued to increase significantly and progressively until 48 h in the laparotomy and CO2 pneumoperitoneal groups. Thereafter, HER2 mRNA expression in both groups started to decrease but did not reach the control level until the end of the 2-week observation period.
Similar to EGFR, HER2 mRNA expression was significantly higher in both treatment groups than in the control group at all check points (p < 0.01). Also, HER2 mRNA expression was significantly higher after laparotomy than after CO2 pneumoperitoneum at all examined time points (p < 0.05 at 1 h and p < 0.01 at 6 h, 48 h, and 1 week, then again p < 0.05 at 2 weeks). Additionally, HER2 mRNA expression in the anesthesia group was low but significantly higher at 6 h and 48 h after the experiment than in the control group (p < 0.01). It then started to fall toward the control level after 48 h (Fig. 2A, B).
Human epidermal receptor (HER2) mRNA-relative expression in human gastric tumors after carbon dioxide (CO2) pneumoperitoneum and laparotomy in tumor-bearing mice (7 mice per each time point, 5 control mice). A Reverse transcription-polymerase chain reaction (RT-PCR) representation. B Time course after the experiment. *p < 0.05. **p < 0.01 (in comparison with laparotomy). ‡ p < 0.01 (in comparison with the control group). L laparotomy; P or pneumo CO2 pneumoperitoneum; C control
Expression of survivin mRNA after surgical procedures
We examined the expression of survivin mRNA after the surgical procedures to clarify whether it was affected like EGFR and HER2 or not. Survivin mRNA expression significantly increased in the three groups at 6 h but continued to increase only in the laparotomy and CO2 pneumoperitoneum groups until 48 h (p < 0.01). Then it decreased toward the control level in all the groups. A significant difference in mRNA expression between the laparotomy and CO2 pneumoperitoneum groups was observed only at 48 h after the experiment (p < 0.05) (Fig. 3A, B).
Survivin mRNA-relative expression in human gastric tumors after carbon dioxide (CO2) pneumoperitoneum and laparotomy in tumor-bearing mice (7 mice per each time point, 5 control mice). A RT-PCR representation. B Time course after the experiment. *p < 0.05 (in comparison with laparotomy). ‡ p < 0.01 (in comparison with the control group). L laparotomy; P or pneumo CO2 pneumoperitoneum; C control; NS not significant
Discussion
In this study, both the laparotomy and CO2 pneumoperitoneum surgical procedures were able to activate postoperative mRNA expression of EGFR, HER2, and survivin to different degrees. To our knowledge, this is the first report to describe the effect of surgical procedures on the mRNA expression of these factors in tumors. Because EGFR, HER2, and survivin have a role in cancer growth and chemoresistance, it is important to examine the changes in their mRNA expression after laparotomy and CO2 pneumoperitoneum [3, 12, 14–16, 19].
To clarify the surgical impact on mRNA expression of EGFR, HER2 and survivin, mice with human gastric cancer disseminated in their peritonea were prepared, and laparotomy and CO2 pneumoperitoneum were used as surgical procedures in this study. This animal model is popularly used to compare the surgical impact of open and laparoscopic surgery on cancer growth and progression because it is a simple and convenient model [20, 21].
Recently, using the same model, we have reported for the first time, to our knowledge, that the surgical impact of laparotomy and CO2 pneumoperitoneum could enhance the activity of nuclear factor kappa B (NFκB) and the mRNA expression of migration inhibitory factor (MIF) and TNFα in human gastric cancer [25]. Also, this previous study shows the possibility that the tumor growth could be affected not only by the extent of surgical stress but also by the location and the size of tumor. Therefore, it seems that these factors may affect HER2, EGFR, and survivin mRNA expression.
In the current study, EGFR and HER2 mRNA expression was significantly increased from the basal control level in both the laparotomy and CO2 pneumoperitoneum groups, then maintained at a significantly higher level than the basal level at least during our 2-week observation period. Interestingly, EGFR and HER2 mRNA expression was significantly higher after laparotomy than after CO2 pneumoperitoneum. Moreover, survivin mRNA expression increased significantly from the control level in both groups until 48 h after surgical procedures and was significantly higher after laparotomy than after CO2 pneumoperitoneum, but only 48 h after each procedure.
These data suggest that the impact of surgery on mRNA expression of EGFR, HER2, and survivin remains for a long duration, and that upregulation of their mRNA expression may depend on the extent of the surgical procedure. Besides surgical stress, several different mechanisms such as wound healing, hypoxia, and acidosis may be associated with the expression of these genes after laparotomy and CO2 pneumoperitoneum [26–29]. It seems that further studies are necessary to clarify the mechanism that regulates these genes after surgery.
Recently, is reported that cancer cell growth and cancer cell chemoresistance to anticancer agents such as taxols and cisplatin can develop by upregulation of EGFR and HER2, which enhances survivin expression in human cancer via the activation of the PI3 K-signaling pathway [13–18]. Conversely, survivin levels and apoptosis resistance were decreased when cells were treated with the HER2-specific inhibitor, Herceptin [3]. Moreover, enhanced expression of survivin in cancer cells is correlated with a poor prognosis and a decrease in the overall survival of cancer patients due to promotion of cancer growth and inhibition of apoptosis [30, 31].
Our study shows upregulation of mRNA expression of EGFR, HER2, and survivin by surgical impact, which may induce chemoresistance in the remnant cancer cells after surgery. Therefore, neoadjuvant chemotherapy or surgery with minimal invasiveness may be considered for cases in which postoperative chemotherapy is required. In addition, cancer molecular targeting therapy may be more effective after surgery because of the postoperative upregulation of EGFR, HER2, and survivin.
In clinical settings, the staging of cancer is the most important factor in the choice of treatment methods. Especially, staging laparoscopy is useful for the diagnosis of peritoneal dissemination to avoid unnecessary laparotomy [32]. Our results suggest that unnecessary exploration to detect peritoneal dissemination can cause activation of cancer cells. After staging laparoscopy, if the advanced cancer lesion is completely removed by surgery, the residual microscopic cancer cells must be considered [1, 33, 34].
Recently, reports have shown postoperative adjuvant chemoradiation therapies to be useful for the treatment of advanced cancer [1, 2]. Therefore, clinicians have begun to apply laparoscopic surgery with minimal invasiveness for advanced cancer because effective adjuvant chemotherapy can be started during the early period after surgery [35].
In conclusion, this study shows enhanced mRNA expression of EGFR, HER2, and survivin after surgery. These increased levels of expression, which are greater after laparotomy than after CO2 pneumoperitoneum, may result in enhanced postoperative chemoresistance in residual cancer cells, but this needs further study. The application of the minimally invasive surgery to the advanced cancer should be accepted after the technical feasibility of the extensive lymphadenectomy has been established, and it still is a matter of controversy because of the unexpected port-site metastasis or immunologic effect of CO2 pneumoperitoneum for patients. Further basic and clinical studies are necessary to clarify the impact of open and laparoscopic surgery on the remnant cancer cells after surgical procedures.
References
Yu W, Whang I, Suh I, Averbach A, Chang D, Sugarbaker PH (1998) Prospective randomized trial of early postoperative intraperitoneal chemotherapy as an adjuvant to resectable gastric cancer. Ann Surg 228:347–354
Han SW, Oh DY, Im SA, Park SR, Lee KW, Song HS, Lee NS, Lee KH, Choi IS, Lee MH, Kim MA, Kim WH, Bang YJ, Kim TY (2009) Phase II study and biomarker analysis of cetuximab combined with modified FOLFOX6 in advanced gastric cancer. Br J Cancer 100:298–304
Asanuma H, Torigoe T, Kamiguchi K, Hirohashi Y, Ohmura T, Hirata K, Sato M, Sato N (2005) Survivin expression is regulated by coexpression of human epidermal growth factor receptor 2 and epidermal growth factor receptor via phosphatidylinositol 3-kinase/AKT signaling pathway in breast cancer cells. Cancer Res 65:11018–11025
Jonker DJ, O’Callaghan CJ, Karapetis Cs, Zalcberg JR, Tu D, Au HJ, Berry SR, Krahn M, Price T, Simes RJ, Tebbutt NC, vanHazel G, Wiezbicki R, Langer C, Moore MJ (2007) Cetuximab for the treatment of colorectal cancer. N Engl J Med 357:2040–2048
Pinto C, Di Fabio F, Siena S, Cascinu S, Rojas Llimpe FL, Ceccarelli C, Mutri V, Gianetta L, Giaquinta S, Funaioli C, Berardi R, Longobardi C, Piana E, Martoni AA (2007) Phase II study of cetuximab in combination with FOLFIRI in patients with untreated advanced gastric or gastroesophageal junction adenocarcinoma (FULCETUX study). Ann Oncol 18:510–517
Coffey JC, Wang JH, Smith MJ, Laing A, Bouchier-Hayes D, Cotter TG, Redmond HP (2005) Phosphoinositide 3-kinase accelerates postoperative tumor growth by inhibiting apoptosis and enhancing resistance to chemotherapy-induced apoptosis. J Biol Chem 280:20968–20977
Lee SW, Gleason N, Blanco I, Asi ZK, Whelan RL (2002) Higher colon cancer tumor proliferative index and lower tumor cell death rate in mice undergoing laparotomy vs insufflation. Surg Endosc 16:36–39
Qadri SS, Wang JH, Coffey JC, Alam M, O’Donnell A, Aherne T, Redmond HP (2005) Surgically induced accelerated local and distant tumor growth is significantly attenuated by selective COX-2 inhibition. Ann Thorac Surg 79:990–995
Akiyama T, Sudo C, Ogawara H, Toyoshima K, Yamamoto T (1986) The product of the human c-erbB-2 gene: a 185-kilo Dalton glycoprotein with tyrosine kinase activity. Science 232:1644–1646
Gravalos C, Jimeno A (2008) HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol 19:1523–1529
Altieri DC (2003) Validating survivin as a cancer therapeutic target. Nat Rev Cancer 3:46–54
Longlley DB, Johnston PG (2005) Molecular mechanisms of drug resistance. J Pathol 205:275–292
Shin S, Sung BJ, Cho YS, Kim HJ, Ha NC, Hwang JI, Chung CW, Jung YK, Oh BH (2001) An anti-apoptotic protein human survivin is a direct inhibitor of caspase-3 and -7. Biochemistry 40:1117–1123
Wang Q, Greene MI (2005) EGFR enhances survivin expression through the phosphoinositide 3 (IP-3) kinase signaling pathway. Exp Mol Bathol 79:100–107
Qiu L, Wang Q, Di W, Jiang Q, Schefeller E, Derby S, Wanebo H, Yan B, Wan Y (2005) Transient activation of EGFR/AKT pathway and expression of survivin contribute to reduced sensitivity of human melanoma cells to betulinic acid. Int J Oncol 27:823–830
Peng XH, Cao ZH, Xia JT, Carlson GW, Lewis MM, Wood WC, Yang L (2005) Real-time detection of gene expression in cancer cells using molecular beacon imaging: new strategies for cancer research. Cancer Res 65:1909–1917
Ikeguchi M, Liu J, Kaibara N (2002) Expression of survivin mRNA and protein in gastric cancer cell line (MKN45) during cisplatin treatment. Apoptosis 7:23–29
Nakamura M, Tsuji N, Asanuma K, Kobayashi D, Yagihashi A, Hirata K, Torigoe T, Sato N, Watanabe N (2004) Survivin as a predictor of cis-diammine dichloroplatinum sensitivity in gastric cancer patients. Cancer Sci 95:44–51
Peng XH, Karna P, Cao Z, Jiang BH, Zhou M, Yang L (2006) Cross-talk between epidermal growth factor receptor and hypoxia inducible factor-1α signal pathways increase resistance to apoptosis by upregulating survivin gene expression. J Biol Chem 281:25903–25914
Matsui Y, Inomata M, Tojigamori M, Sonoda K, Shiraishi N, Kitano S (2005) Suppression of tumor growth in human gastric cancer with HER2 overexpression by an anti HER2 antobody in a murine model. Int J Oncol 27:681–685
Suematsu T, Shiromizu A, Yamaguchi K, Shiraishi N, Adachi Y, Kitano S (1999) Convenient murine pneumoperitoneal model for the study of laparoscopic cancer surgery. Surg Laparo Endo Per 9:279–281
Narita T, Taga T, Sugita K, Nakazawa S, Ohta S (2001) The autocrine loop of epidermal growth factor receptor–epidermal growth factor/transforming factor alpha in malignant rhabdoid tumor cell lines: heterogeneity of autocrine mechanism in TTC 549. Jpn J Cancer Res 92:269–278
Revillion F, Hornez L, Peyrat JP (1997) Quuatification of c-erbB-2 gene expression in breast cancer by competitive RT-PCR. Clin Chem 43:2114–2120
Zhang T, Fields JZ, Ehrlich SM (2004) The chemopreventive agent sulindac attenuates expression of the antiapoptotic protein survivin in colorectal carcinoma cells. J Pharmacol Exp Ther 308:434–437
Anwar TA, Shiraishi N, Ninomyia S, Tajima M, Inomata M, Kitano S (2009) Activation of nuclear factor kappa B (NFκB) and induction of migration inhibitory factor (MIF) in tumors by surgical stress of laparotomy vs CO2 pneumoperitoneum: an animal experiment. Surg Endosc. doi:10.1007/s00464-009-0609-x
Abramovitch R, Marikovsky M, Meir G, Neeman M (1999) Stimulation of tumor growth by wound-derived growth factors. Br J Cancer 79:1392–1398
Rupec RA, Baeuerle PA (1995) The genomic response of tumor cells to hypoxia and reoxygenation: differential activation of transcription factors AP-1 and NFκB. Eur J Biochem 234:632–640
Lundberg O, Kristoffersson A (2005) Reduction of abdominal wall blood flow by clamping or carbon dioxide insufflation increases tumor growth in the abdominal wall: an experimental study in rats. Surg Endosc 19:720–723
Hsieh HL, Sun CC, Wu CB, Wu CY, Tung WH, Wang HH, Yang CM (2008) Sphnigosine 1-phosphate induces EGFR expression via Akt/NFκB and ERK/Ap-1 pathways in rat vascular smooth muscle cells. J Cell Biochem 103:1732–1746
Islam A, Kageyama H, Takada N, Kawamoto T, Takayasu H, Isogai E, Ohira M, Hashizume K, Kobayashi H, Kaneko Y, Nakagawara A (2000) High expression of survivin, mapped to 17q25, is significantly associated with poor prognostic factors and promotes cell survival in human neuroblastoma. Oncogene 19:617–623
Kawasaki H, Altieri DC, Lu CD, Toyoda M, Tenjo T, Tanigawa N (1998) Inhibition of apoptosis by survivin predicts shorter survival rates in colorectal cancer. Cancer Res 58:5071–5074
Mayo SC, Austin DF, Sheppard BC, Mori M, Shipley DK, Billingsley KG (2009) Evolving preoperative evaluation of patients with pancreatic cancer: does laparoscopy have a role in the current era. J Am Coll Surg 208:87–95
Tagliabue E, Agresti R, Carcangiu ML, Ghirelli C, Morelli D, Campiglio M, Martel M, Giovanazzi R, Greco M, Balsari A, Menard S (2003) Role of HER2 in wound induced breast carcinoma proliferation. Lancet 362:527–533
Jarnagin WR, Delman K, Kooby D, Mastorides S, Zager J, Brennan MF, Blumgart LH, Federoff H, Fong Y (2000) Neoadjuvant interleukin-12 immunogene therapy protects against cancer recurrence after liver resection in an animal model. Ann Surg 231:762–771
Wei JM, Shiraishi N, Goto S, Yasuda K, Inomata M, Kitano S (2008) Laparoscopy-assisted distal gastrectomy with D1 + β compared with D1α lymph node dissection. Surg Endosc 22:955–960
Acknowledgment
This work was supported in part by a Grant-in-Aid for Scientific Research (no. 050916) from the Ministry of Education, Science, Culture, and Sports, Japan.
Disclosures
Anwar Tawfik Amin, Norio Shiraishi, Shigeo Ninomiya, Masaaki Tajima, Masafumi Inomata, and Seigo Kitano have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amin, A.T., Shiraishi, N., Ninomiya, S. et al. Increased mRNA expression of epidermal growth factor receptor, human epidermal receptor, and survivin in human gastric cancer after the surgical stress of laparotomy versus carbon dioxide pneumoperitoneum in a murine model. Surg Endosc 24, 1427–1433 (2010). https://doi.org/10.1007/s00464-009-0793-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0793-8