Abstract
Background
Thoracic epidural analgesia (TEA) provides superior analgesia with a lower incidence of postoperative ileus when compared with systemic opiate analgesia in open colorectal surgery. However, in laparoscopic colorectal surgery the role of TEA is not well defined. This prospective observational study investigates the influence of TEA in laparoscopic colorectal resections.
Methods
All patients undergoing colorectal resection between November 2004 and February 2007 were assessed for inclusion into a prospective randomized trial investigating the influence of bisacodyl on postoperative ileus. All patients treated by laparoscopic resection from this collective were eligible for the present study. Primary endpoints were use of analgesics and visual analogue scale (VAS) pain scores. Secondary endpoint concerned full gastrointestinal recovery, defined as the mean time to the occurrence of the following three events (GI-3): first flatus passed, first defecation, and first solid food tolerated.
Results
75 patients underwent laparoscopic colorectal resection, 39 in the TEA group and 36 in the non-TEA group. Patients with TEA required significantly less analgesics (metamizol median 3.0 g [0–32 g] versus 13.8 g [0–28 g] (p < 0.001); opioids mean 12 mg [±2.8 mg standard error of mean, SEM] versus 103 mg [±18.2 mg SEM] (p < 0.001). VAS scores were significantly lower in the TEA group (overall mean 1.67 [± 0.2 SEM] versus 2.58 [±0.2 SEM]; p = 0.004). Mean time to gastrointestinal recovery (GI-3) was significantly shorter (2.96 [±0.2 SEM] days versus 3.81 [±0.3 SEM] days; p = 0.025). Analysis of the subgroup of patients with laparoscopically completed resections showed corresponding results.
Conclusion
TEA provides a significant benefit in terms of less analgesic consumption, better postoperative pain relief, and faster recovery of gastrointestinal function in patients undergoing laparoscopic colorectal resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In patients undergoing major open abdominal surgery, including open colorectal resection, thoracic epidural analgesia (TEA) provides superior analgesia and reduced duration of postoperative ileus when compared with systemic opioid analgesia [1–6].
TEA is currently used in multimodal recovery programs, in combination with early and enhanced feeding, early removal of drains and catheters, and enforced mobilization [7]. However, the benefit of TEA itself remains to be defined. Some authors consider TEA to be the most decisive intervention in reducing postoperative ileus, whilst others report no advantage over patient controlled intravenous opioid analgesia for patients undergoing laparotomy in an enhanced recovery program [8–10].
Laparoscopic colorectal surgery has gained wide acceptance; it is associated with reduced surgical trauma, less pain, quicker recovery, and shorter hospital stays [11–13]. Some authors question the benefits of laparoscopic surgery in a fast-track setting [14–16]. Especially the role of TEA in laparoscopic colorectal resection has yet not been defined. Some authors have shown that TEA is beneficial for pain relief, dietary intake, and length of hospital stay, but these findings are not consistently reproducible [17–20].
The aim of this prospective observational study was to investigate the influence of TEA compared to systemic opioid analgesia on postoperative pain relief and duration of ileus in patients undergoing elective laparoscopic colorectal resection.
Patients and methods
Patients
Between November 2004 and February 2007, all patients with elective open or laparoscopic colorectal resections at the Triemli Hospital in Zurich, Switzerland, were assessed for eligibility to be included in a prospective, randomized trial investigating the effect of bisacodyl versus placebo (trial submitted for publication). The trial was registered by the National Library of Medicine at www.clinicaltrials.gov under the number NCT00509327 and was approved by the local ethics committee. The subgroup of patients with planned laparoscopic resections was eligible for the present observational study. A subanalysis excluding all converted cases to evaluate the collective with laparoscopically completed resections was additionally performed. There was no difference in bisacodyl use between the TEA and non-TEA groups.
Thoracic epidural analgesia
Thoracic epidural analgesia was considered for every patient. Contraindications were previous back surgery, severe spondylarthrosis, coagulopathy or patient refusal. In the TEA group, before induction of general anesthesia, a thoracic epidural catheter (Espocan® 18-G, Braun, Melsungen, Germany) was positioned using the loss-of-resistance technique between Th8 and Th12. An intrathecal position was excluded by a bolus injection of 3 ml lidocaine 2% (Rapidocain®; Sintetica, Mendrisio, Switzerland). Ropivacaine 0.3% (Naropin®; AstraZeneca, Zug, Switzerland) was then administered continuously at 6–12 ml/h during surgery. Postoperatively, the thoracic epidural catheter was left in situ and a solution consisting of 48 ml 0.125% bupivacaine (Duracain®, Sintetica, Mendrisio, Switzerland) with 2 ml fentanyl (Fentanyl-Curamed®, Opopharma, Zurich, Switzerland), was administered for continuous analgesia during the first five postoperative days.
Surgical and anesthetic procedure
All patients received standardized bowel preparation (2 l sodium sulfate/macrogol solution; Cololyt®, Spirig Pharma, Egerkingen, Switzerland). During induction of anesthesia, all patients received preoperative single-shot antibiotics (cefuroxime 1.5 g and metronidazole 1 g intravenously). General anaesthesia with endotracheal intubation was performed using a standard technique with propofol (Disoprivan®, AstraZeneca, Zug, Switzerland), fentanyl (Fentanyl-Curamed®, Opopharma, Zurich, Switzerland), sevoflurane (Sevorane®, Abbott, Baar, Switzerland), and rocuronium (Esmeron®, Organon, Pfäffikon, Switzerland). Laparoscopic surgery was performed with a four-port technique with removal of the specimen through a small transverse incision in the lower abdomen. For left-sided colectomy, medial mobilization including visualization of the ureter was used. The anastomosis was performed using a double stapling technique with a circular end-to-end anastomotic stapler (Premium Plus CEEATM 31 mm, Tyco Healthcare, Switzerland). In right-sided colectomy, the colon was also mobilized medially. Resection and anastomosis were performed extracorporally via a transverse incision in the middle right abdomen with an end-to-end, single-layer running suture (BiosynTM 4.0, Tyco Healthcare, Switzerland). The nasogastric tube (NGT) was routinely removed at the end of the anesthesia.
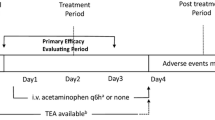
Postoperative regimen
All patients received a basic analgesia of 0.5–1 g oral paracetamol (Dafalgan®, Bristol-Myers Squibb, Baar, Switzerland) every 6 hours. For additional pain relief metamizol (Novalgin®, Sanofi-Aventis, Meyrin, Switzerland) was used as first-line reserve and morphine or its derivates as second-line reserve. Patient-controlled analgesia (PCA) with intravenous morphine was considered for a minority of patients. TEA was checked every day by the anesthetic pain service and removed on postoperative day five. Nutrition was started on the first postoperative day. We used a five-step diet protocol, starting with limited fluids (1000 ml/day), followed by free fluids, soft food, light meals, and normal diet. Progress to the next step required bowel movement, absence of nausea, and toleration of the previously given nutrition.
Data analysis
Primary endpoints were consumption of analgesics and visual analogue scale (VAS) pain scores during the first eight postoperative days. To allow comparison, all opioids were converted to an equivalent morphine dose. The daily quantity of PCA-administered morphine was recorded and added to the on-demand quantity of morphine. VAS scores were assessed during the morning ward rounds by the responsible intern. Secondary endpoint was recovery of gastrointestinal function, defined as the mean time to the occurrence of the following three events (GI-3): first flatus passed, first defecation, and first solid food tolerated. Furthermore, frequency of NGT reinsertion, frequency of postoperative vomiting, and length of hospital stay were monitored. Other variables recorded were patient demographics, administration of laxatives (bisacodyl), morbidity of TEA, and surgical and medical morbidity.
Statistical analysis
Data are shown as median [range] or mean [standard error of mean, SEM], as appropriate. The qualitative data were compared statistically using the Fisher’s exact test. If the quantitative data showed normal distribution parameters, they were compared parametrically using a paired Student’s t-test, else the Mann–Whitney U-test was applied. Regardless of the statistical tests selected, the level of significance was defined as p ≤ 0.05 (GraphPad InStat®, GraphPad Software, Inc., San Diego, CA).
Results
Two hundred patients with elective colorectal resection were enrolled into the prospective, randomized trial on the effect of bisacodyl versus placebo (NCT00509327). Thirty-one patients discontinued the study. Seventy-five patients underwent laparoscopic resection and were eligible for this prospective observational study (Fig. 1). In 15 patients the operation was converted to open resection. No significant difference between groups in demographic characteristics was noted (Table 1). The majority of patients underwent rectosigmoid resection (n = 65, 85.3%). Primary indication was diverticular disease (n = 63, 84%).
With the exception of paracetamol (TEA mean 19.7 g [±1.5 g] versus 15.6 g [±1.7 g]; p = 0.074), patients with TEA required significantly less metamizol (median 3.0 g [0–32 g] versus 13.8 g [0–28 g]; p < 0.001) or opioids (mean 12 mg [±2.8 mg] versus 103 mg [±18.2 mg], p < 0.001) during the first eight postoperative days. To assess the opioid consumption during TEA and after removal, days 1–4 and 5–8 were analyzed separately. During the first 4 days, opioid consumption was significantly lower in the TEA group whereas during days 5–8, after TEA removal, the difference was no longer significant (Table 2). In patients with TEA, the quantity of opioids needed did not increase after removal (days 1–4: mean 6.6 mg [±1.8 mg], days 5–8: mean 5.6 mg [±1.5 mg]; p = 0.684) whereas in the non-TEA group a significant decrease after 4 days was seen (days 1–4: mean 83.9 mg [±13.8 mg], days 5–8: mean 17.6 mg [±8.3 mg]; p < 0.001).
Overall VAS pain scores during the first eight days were significantly lower in the TEA group (mean 1.67 [±0.2] versus 2.58 [±0.2]; p = 0.004). Daily VAS pain scores are shown in Fig. 2.
Recovery of gastrointestinal function (GI-3) occurred significantly earlier in patients with TEA (2.96 [±0.2] days versus 3.81 [±0.3] days; p = 0.025). Of the single parameters defining GI-3, a significant difference was observed in time to first stool (mean 2.9 [±0.3] days versus 3.8 [±0.3] days; p = 0.038). Time to first passed flatus was shorter by 1 day but not significantly so (median 1 day [1–7 days] versus 2 days [1–6 days]; p = 0.091). Time to solid food tolerance did not differ (4 days [2–11 days and 2–30 days, respectively]; p = 0.210).
Frequency of NGT reinsertion, postoperative vomiting, and length of hospital stay did not differ significantly between the groups (Table 3).
In the subgroup of laparoscopic resection with all converted cases excluded, the results were similar to the main collective. No significant difference in bisacodyl use occurred (TEA 17, non-TEA 12; p = 0.799). Again, with the exception of paracetamol (TEA mean 19.1 g [±1.0 g] versus 14.1 g [±1.0 g]; p = 0.057), consumption of analgesics was significantly lower in the TEA group. GI-3 occurred significantly earlier. In this collective, time to first flatus was also shorter by 1 day, but reached significance (Table 4). Frequency of NGT reinsertion (TEA n = 1 versus non-TEA n = 0, p = 1.000), postoperative vomiting (TEA n = 6 versus non-TEA n = 5, p = 1.000) and length of hospitalization (TEA n = 9 versus non-TEA n = 11, p = 0.357) did not reach levels of significance. Analysis of postoperative pain in this sub-group is shown in Fig. 3.
Surgical and medical morbidity did not differ between groups. Five patients (13%) in the TEA group had minor TEA-related complications (Table 5). In one patient (3%) the TEA had to be removed on postoperative day 1 (failure of analgesic effect) and in three patients (8%) on postoperative day 2 (paresis of ipsilateral leg, hypotension). No patient suffered from major TEA-related morbidity such as epidural hematoma, abscess or nerve damage. No surgical intervention for TEA related complications were necessary.
Discussion
Our study shows that TEA resulted in a significantly lower analgesic consumption and lower VAS pain scores during the observation period. Patients required less additional metamizol or opioids. The major effect was observed during the first four postoperative days. The difference in opioid consumption between the two groups was no longer significant following TEA removal. Opioid consumption remained constant in the TEA group after removal of the epidural catheter, implying that TEA provides effective analgesia without a rebound phenomenon after removal.
VAS pain scores were significantly lower during the first three postoperative days and again on days 6 and 7. On days 4 and 5 the figures did not reach significance, but only by a narrow margin (p = 0.054 and p = 0.059, respectively). VAS score on day 8 did not differ. Although the catheter was removed on day 5, the analgesic benefit of TEA seems to continue until day 7. The results for postoperative pain relief in patients with laparoscopic resections are inconsistent in the current literature and no study has assessed the VAS pain scores beyond postoperative day 4. Whereas Neudecker et al. were not able to show any significant improved pain relief in a prospective randomized trial with ten patients in each arm, two other reports demonstrated better VAS scores during the first 48 hours in the TEA group [18–20]. The optimal duration of TEA postoperatively is not well established. Some authors suggest removal on the second postoperative day [14, 21]. Senagore et al. removed the catheter 18 h postoperatively and were unable to demonstrate a significant effect on VAS pain scores after removal [19]. In the randomized trial of Taqi et al., TEA was continued up to day 3, again showing no significant differences in pain perception after removal [18].
According to the data in this study, the beneficial effect of TEA persists up to postoperative day 7. Most patients, especially the elderly, may not be discharged on the second postoperative day but rather on day 5 or 6 , so that, providing daily clinical controls are present, TEA should be left in place up to 5 days.
Return of gastrointestinal function was significantly shorter in patients with TEA. This corresponds to the findings of Senagore et al. and Taqi et al., who were able to show an improved analgesia and earlier return of bowel function in patients with TEA [17–19]. Incidence of NGT reinsertion or postoperative vomiting did not differ between the groups, which was surprising, as the non-TEA group received a larger quantity of opioids. Liberal use of anti-emetics (metoclopramide) for nausea may explain this finding in this collective.
Length of hospital stay did not decrease in our study. The median duration of 11 days is rather long compared with the current literature, where 2–7 days are mentioned [14, 16, 22]. The patients in this study were not enrolled in a specific fast-track program. Factors such as waiting time for subsequent stays in rehabilitation institutions or prolongation of hospitalization for social reasons may explain this finding.
Current multimodal therapy programs for colorectal surgery include TEA, avoidance or early removal of drains, early oral feeding, and enforced mobilization [7, 15, 16, 22]. As a single intervention, TEA has been shown to be the most important factor in reducing postoperative ileus in conventional surgery [9, 10]. As laparoscopic technique leads to a decrease in pain, inflammatory reaction, and postoperative ileus by itself, the question remains whether TEA is needed at all [12, 13, 23, 24]. Morbidity from TEA has to be considered. In the current study, minor complications occurred in five patients (13%). Paresis and hypotension could be managed by removal of the TEA or, in case of paresis during insertion, by repositioning of the catheter. No major complications such as epidural hematoma, abscess or neurological damage occurred. The risk for such complications is very small (0.01–0.7%) and the benefit of TEA justifies its use [21, 25, 26]. The use of local anesthetics (in this study duracain 0.125%) increases the parasympathetic tone, thus accelerating gastrointestinal recovery. The addition of the opioid fentanyl improves analgesia. The combination of these two drugs has been shown to be synergistic [3–5]. Thoracic application spares the lumbar and sacral nerves so that motor and sensory deficits (urinary retention, paralysis, hypotension) are minimal.
The groups did not differ in surgical or medical morbidity. Anastomotic leakage occurred in two patients in each group. Consistent with other reports, continuous TEA was not associated with an increased risk of anastomotic leakage in this collective [27, 28].
To eliminate the influence of the converted cases, a subanalysis of laparoscopically completed operations was conducted. The results were similar to the main collective and highlight the importance of TEA in laparoscopic colorectal surgery. Patients without TEA consumed overall less opioids than in the main collective. This is explained by the fact that ten patients with conversion and supposedly higher analgesics requirement were excluded in this group. In the TEA group the trend was converse, a fact we could not explain. However, only five patients had conversion in this group and further analysis may not be sensible. VAS pain scores were significantly lower in the TEA group during the first 2 days and again on day 7. No significance was reached during the other days, but a clear trend towards lower pain levels in the TEA group is shown.
This study is the largest analyzing the effect of TEA in laparoscopic colorectal resection. Some limitations may be discussed, including the fact that it is a subgroup analysis of a larger randomized trial. A possible bias concerning bisacodyl has been excluded, as there was no difference between groups (p = 0.358). Postoperative systemic opioid regimen in the non-TEA group was not standardized, as a minority of patients received a PCA pump. However, the amount of PCA morphine was monitored together with the other opioids and equivalent total doses were calculated.
Conclusion
TEA in patients with laparoscopic colorectal resections provides a significant benefit in terms of reduced use of analgesics, lower VAS pain scores, and faster gastrointestinal recovery with minimal morbidity. These results support the use of TEA in minimal invasive colorectal surgery and suggest that TEA has a positive analgesic effect until postoperative day 7.
References
Mann C, Pouzeratte Y, Boccara G, Peccoux C, Vergne C, Brunat G, Domergue J, Millat B, Colson P (2000) Comparison of intravenous or epidural patient-controlled analgesia in the elderly after major abdominal surgery. Anesthesiology 92:433–441
Rigg JRA, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, Collins KS (2002) Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet 359:1276–1282
Steinberg RB, Liu SS, Wu CL, Mackey DC, Grass JA, Ahlen K, Jeppsson L (2002) Comparison of ropivacaine-fentanyl patient-controlled epidural analgesia with morphine intravenous patient-controlled analgesia for perioperative analgesia and recovery after open colon surgery. J Clin Anesth 14:571–577
Carli F, Trudel JL, Belliveau P (2001) The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery. Dis Colon Rectum 44:1083–1089
Gendall KA, Kennedy RR, Watson AJM, Frizelle FA (2007) The effect of epidural analgesia on postoperative outcome after colorectal surgery. Colorectal Dis 9(7):584–598
Scott NB, James K, Murphy M, Kehlet H (1996) Continuous thoracic epidural analgesia versus combined spinal/thoracic epidural analgesia on pain, pulmonary function and the metabolic response following colonic resection. Acta Anaesthesiol Scand 40:691–696
Wind J, Polle SW, Fung Kon Jin PHP, Dejong CHC, von Meyenfeldt MF, Ubbink DT, Gouma DJ, Bemelman WA (2006) Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg 93:800–809
Zutshi M, Delaney CP, Senagore AJ, Mekhail N, Lewis B, Connor JT, Fazio VW (2005) Randomized controlled trial comparing the controlled rehabilitation with early ambulation and diet pathway versus the controlled rehabilitation with early ambulation and diet with preemptive epidural anesthesia/analgesia after laparotomy and intestinal resection. Am J Surg 189(3):268–272
Holte K, Kehlet H (2002) Prevention of postoperative ileus. Minerva Anesthesiol 68(4):152–156
Kehlet H, Holte K (2001) Review of postoperative ileus. Am J Surg 182:3S–10S
Hildebrandt U, Kessler K, Plusczyk T, Pistorius G, Vollmar B, Menger MD (2003) Comparison of surgical stress between laparoscopic and open colonic resections. Surg Endosc 17:242–246
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91:1111–1124
Abraham NS, Byrne CM, Young JM, Solomon MJ (2007) Meta-analysis of non-randomized comparative studies of the short-term outcomes of laparoscopic resection for colorectal cancer. ANZ J Surg 77:508–516
Basse L, Jakobsen Hjort D, Bardram L, Billesbølle P, Lund C, Morgensen T, Rosenberg J, Kehlet H (2005) Functional recovery after open versus laparoscopic colonic resection. Ann Surg 241:416–423
Basse L, Madsen JL, Billesbølle P, Bardram L, Kehlet H (2003) Gastrointestinal transit after laparoscopic vs. open colonic resection. Surg Endosc 17:1919–1922
King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH, Kipling RM, Kennedy RH (2006) Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 93:300–308
Senagore AJ, Whalley D, Delaney CP, Mekhail N, Duepree HJ, Fazio VW (2001) Epidural anesthesia-analgesia shortens length of stay after laparoscopic segmental colectomy for benign pathology. Surgery 129:672–676
Taqi A, Hong X, Mistraletti G, Stein B, Charlebois P, Carli F (2007) Thoracic epidural analgesia facilitates the restoration of bowel function and dietary intake in patients undergoing laparoscopic colon resection using a traditional, nonaccelerated, perioperative care program. Surg Endosc 21:247–252
Senagore AJ, Delaney CP, Mekhail N, Dugan A, Fazio VW (2003) Randomized clinical trial comparing epidural anaesthesia and patient-controlled analgesia after laparoscopic segmental colectomy. Br J Surg 90:1195–1199
Neudecker J, Schwenk W, Junghans T, Pietsch S, Böhm B, Müller JM (1999) Randomized controlled trial to examine the influence of thoracic epidural analgesia on postoperative ileus after laparoscopic sigmoid resection. Br J Surg 86:1292–1295
Fearon KCH, Ljungqvist O, von Meyenfeldt M, Revhaug A, Dejong CHC, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24:466–477
Raue W, Haase O, Junghans T, Scharfenberg M, Müller JM, Schwenk W (2004) “Fast-track” multimodal rehabilitation program improves outcome after laparoscopic sigmoidectomy. Surg Endosc 18:1463–1468
Schwenk W, Böhm B, Haase O, Junghans T, Müller JM (1998) Laparoscopic versus conventional colorectal resection: a prospective randomised study of postoperative ileus and early postoperative feeding. Langenbecks Arch Surg 383:49–55
Kehlet H (2006) Future perspectives and research initiatives in fast-track surgery. Langenbecks Arch Surg 391:495–498
Horlocker TT, Wedel DJ (2000) Neurologic complications of spinal and epidural anesthesia. Reg Anesth Pain Med 25:83–98
Dawson SJ, Small H, Logan MN, Geringer S (2000) Case control study of epidural catheter infections in a district general hospital. Comm Dis Public Health 3:300–302
Holte K, Kehlet H (2001) Epidural analgesia and risk of anastomotic leakage. Reg Anesth Pain Med 26:111–117
Ryan P, Schweitzer SA, Woods RJ (1992) Effect of epidural and general anaesthesia compared with general anaesthesia alone in large bowel anastomosis. Eur J Surg 158:45–49
Acknowledgement
We thank Dr. Karen Delport, MD, for assistance in preparing the manuscript in English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zingg, U., Miskovic, D., Hamel, C.T. et al. Influence of thoracic epidural analgesia on postoperative pain relief and ileus after laparoscopic colorectal resection. Surg Endosc 23, 276–282 (2009). https://doi.org/10.1007/s00464-008-9888-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9888-x