Abstract
Background
Bladder and sexual dysfunction are well-documented complications of rectal cancer surgery. This study aimed to determine whether laparoscopy can improve the outcome of these dysfunctions or not.
Methods
The study included 63 of the 116 patients who underwent surgery for rectal cancer between 2002 and 2006. Bladder and male sexual function were studied by means of a questionnaire on the basis of the International Prostatic Symptom Score (IPSS) and International Index of Erectile Function (IIEF). In addition, bladder function was determined by means of postvoid residual urine measurement and uroflowmetry. Postoperative functions were compared with the preoperative data to detect subjective functional deterioration. Outcomes were compared between patients who underwent open (group 1, n = 29) and laparoscopic (group 2, n = 34) total mesorectal excision.
Results
Only minor disturbances of bladder function were reported for one patient (3%) in group 1 and three patients (9%) in group 2 (p > 0.05). Impotency after surgery was experienced by 6 of 17 preoperatively sexually active males (29%) in group 1 and 1 of 18 males (5%) in group 2 (p = 0.04). Similarly, 5 of 10 women (50 %) in group 1 and 1 of 14 women (7%) in group 2 felt that their overall level of sexual function had decreased as a result of surgery (p = 0.03).
Conclusions
Open rectal cancer resection is associated with a higher rate of sexual dysfunction, but not bladder dysfunction, compared with laparoscopic surgery. Laparoscopic rectal cancer surgery offers a significant advantage with regard to preservation of postoperative sexual function and constitutes a true advance in rectal cancer surgery compared with the open technique. The proposed advantages can be attributed to improvement in visibility by the magnification feature of laparoscopic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bladder and sexual dysfunction are recognized complications of rectal carcinoma resection. The incidence of these complications was high before the introduction of total mesorectal excision (TME), with reported values of 10% to 30% for bladder dysfunction and 40% 60% for sexual dysfunction [1–4]. The main cause of dysfunction seems to be injury to the autonomic nerves in the pelvis and along the distal aorta. The incidence of genitourinary dysfunction depends on the type of operation performed, the plane of dissection, the ligation level of the inferior mesenteric artery, the degree of preservation of the autonomic nerves, and the extent of pelvic dissection [5–10].
In 1982, TME was introduced as the standard method for treatment of rectal cancer [5]. With the TME technique, the rectum is mobilized circumferentially under direct vision, with sharp dissection along the parietal pelvic fascia. This procedure, combined with an awareness of the pelvic autonomic nerve pathways, minimizes sexual and urinary dysfunction.
Recent studies have demonstrated that mesorectal excision for rectal cancer has resulted in a low frequency of serious bladder and sexual dysfunction [6, 9]. Even with incorporation of autonomic nerve-preserving techniques in TME, urinary and sexual dysfunction remain recognized complications for 0% to 12% and 10% to 35% of patients, respectively [7–12].
Laparoscopic TME for cancer is technically feasible, with acceptable complication rates and short-term oncologic outcomes comparable with those for open surgery [13–17]. However, little is known about the incidence of urinary or sexual dysfunction after laparoscopic TME. Theoretically, a magnified view of the pelvis may facilitate autonomic nerve identification. The current study aimed to assess the frequency of sexual and urinary dysfunction among a consecutive series of patients with rectal cancer who underwent laparoscopic and open TME.
Patients and methods
Patients
This study compared sexual and bladder function retrospectively between patients who underwent laparoscopic TME and those who had open TME for rectal cancer. The patients who underwent partial mesorectal excision, the patients who experienced local or systemic recurrences, and those who died for any reason were excluded from the study. Questionnaires and uroflowmetric analyses were completed between October 2006 and March 2007. To detect subjective functional deterioration, the questions comprised pre- and postoperative urogenital function.
Surgical procedure
The technique for TME as described by Heald [5] involved complete removal of the mesorectum and the mesentery containing the inferior mesenteric artery and vein by meticulous sharp dissection of the avascular plane, the so-called “holy plane,” between the parietal and visceral pelvic fascia. Autonomic nerve preservation consisted of identifying and sparing the preaortic superior hypogastric plexus and the bilateral hypogastric nerves that join the sacral parasymphatethic nerves (nervi erigentes) to form the inferior hypogastric plexus anterolaterally on both sides. At this point, little autonomic nerves branching off the inferior hypogastric plexus directly into the rectum required division, and damage to the inferior hypogastric plexus itself was avoided.
Patients who underwent laparoscopic surgery had TME according to the same oncologic principles outlined for open surgery. The transurethral catheter placed preoperatively was removed on the first postoperative day.
Assessment of urinary function
The questionnaire consisted of questions relating to difficulty emptying the bladder, feeling of incomplete bladder emptying, urgency, leakage of urine, dysuria, dribbling, and need for self-catheterization on the basis of the International Prostatic Symptom Score [18]. In addition, bladder function was determined by means of postvoid residual urine measurement and uroflowmetry. Bladder dysfunction was classified as major for patients with incontinence or self-catheterization and as minor for those with the other symptoms.
Assessment of sexual function
The International Index of Erectile Function [19] was used to assess male sexual function, with an emphasis on the domain for evaluation of erectile function, ejaculatory function, libido, orgasm, and overall sexual satisfaction. Female sexual function was assessed by evaluation of libido, orgasm, vaginal lubrication, dyspareunia, and sexual satisfaction. All the questions had four possible answers: never, rare, frequent, or always. The first two categories were classified as absence of a specific symptom and the latter two as presence of a specific symptom. The questions comprised preoperative and postoperative urogenital functions to determine subjective functional deterioration.
Statistical analysis
Differences between the two groups (open vs laparoscopic TME) in terms of age and distances of tumor and anastomosis from the anal verge (quantitative data) were analyzed with a Mann-Whitney U test. Differences in the remaining patients as well as treatment and tumor characteristics (categorical data) were calculated using a chi-square test. Postoperative urogenital functions were compared with the preoperative data and between the open and laparoscopic groups using the chi-square test. Statistical significance was set at the 5% level. Data were analyzed by using SPSS for windows, version 12.0 (SPSS, Inc., Chicago, IL, USA).
Results
Study population
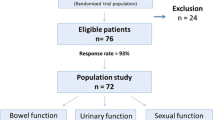
From 2002 to 2006, 116 consecutive patients underwent surgery for rectal cancer, defined as adenocarcinoma within 15 cm of the anal verge. The median follow-up period was 22 months (range, 7–70 months). Recurrence of cancer (local recurrence for 5 patients, distant metastases for 18 patients, and both for 2 patients) developed in 21 patients (18%). Postoperative death claimed four patients (3%). Six patients (5%) underwent partial mesorectal excision. We excluded these patients (n = 31), which involved those who experienced local or systemic recurrences, those who died of surgery-related causes, and those who underwent partial mesorectal excision.
A total of 85 patients who underwent TME for rectal cancer were eligible to participate in the bladder and sexual function study. Of these 85 patients, 63 (74%) completed questionnaires (34 who had laparoscopic TME, 29 who had open TME). The compliance figures were similar between the two groups. The reasons for noncompliance included physical problems, no desire to participate, irrelevance (old age), status of not well enough, information too personal, and no partner.
Patient demographics, operative details, and histologic data are shown in Table 1. There was no statistically significant difference between the groups in terms of age, sex distribution, number and types of operative procedures performed, or tumor (T) and nodal (N) stages of the resected specimens. The majority of tumors were stage pT2 or pT3 and had a nodal status of pN0. The abdominoperineal excision rates were higher in the open surgery group, but this difference was not statistically significant (p > 0.05).
Urinary function
The data on urinary function are sumarized in Table 2. Even before rectal cancer surgery, 3% to 7% of the patients with rectal cancer often or always experienced one or more symptoms of urinary dysfunction. There was no significant difference in urinary symptoms between the patients who had open TME (group 1) and those who had laparoscopic TME (group 2), either in the preoperative occurence of symptoms or as a consequence of the operation. None of the patients required long-term intermittent self-catheterization.
The amount of residual urine exceeded 200 ml for one patient (group 2). Urinary dysfunction (minor dysfunction) was experienced by one woman and two men. We could not determine a relationship between the degree of bladder dysfunction and patient age because of the relatively small patient cohort in this study.
Female sexual function
The results of sexual function among the women are listed in Table 3. Before their operations, 24 women (92%) with a median age of 59 years (range, 39–75 years) were sexually active. The mean age of the two women not sexually active before their operations was 76 years (range, 75–77 years).
Five (50%) of the 10 patients in the open TME group and 1 (7%) of the 14 patients in the laparoscopic TME group felt that their overall level of sexual function had decreased “quite a lot” or “severely” as a result of surgery. These women reported multiple contributing factors. The ostomy caused a negative change in sexual life for one patient in open abdominoperineal resection (embarrassment, image, “I feel damaged”). Two of five patients in the open group without an ostomy felt that bowel changes made their sexual life worse. One believed that her partner was reluctant to have sex with her after surgery, and one believed her partner was afraid of hurting her. Two women reported a loss of spontaneity. All patients with sexual dysfunction reported the problem of a dry vagina during intercourse after surgery. These patients said their vagina “feels smaller or tighter” since surgery.
Male sexual function
The results of sexual function among the men are listed in Table 4. Potency was defined as the ability to achieve an erection sufficient for vaginal penetration and orgasm. Before surgery, 17 of the 18 male patients in group 1 (open) and 18 of the 19 male patients in group 2 (laparoscopic) were sexually active with normal potency. Postoperatively, 6 patients (35%) in group 1 and 1 patient (6%) in group 2 experienced impotency.
Compared with open surgery, laparoscopic TME significantly preserved the ability to achieve orgasm and to ejaculate. Among the six men in the open TME group, five had inability to ejaculate, and all of them had diminished erectile function. In the laparoscopic TME group, the only patient affected had both erectile and ejaculatory dysfunction. Hence, the overall rate of male sexual dysfunction after surgery was 6 of 17 men in the open surgery group compared with 1 of 18 men who underwent laparoscopic TME.
The effect of clinical and pathologic factors on sexual dysfunction also were analyzed. Men and women were pooled together, and analyses of sexually active patients were performed. Laparoscopic surgery was found to be the only significant factor affecting sexual function (Table 5).
Discussion
Normal bladder and sexual function is controlled by sympathetic input from the superior hypogastric plexus and parasymphathetic input from the pelvic splanchnic nerves. These nerves are susceptible to injury during mesorectal resection. In simple terms, injury to the sympathetic supply results in bladder instability and ejaculatory difficulties, whereas injury to the parasymphathetic supply results in poor detrusor contraction and erectile dysfunction [20, 21].
The global assesment showed that the incidence of bladder dysfunction was low after both the laparoscopic and open approaches, with no difference between the two groups in terms of a change in median International Prostatic Symptom Score scores for the men or the women. Only one patient (3%) in the open TME group and three patients (9%) in the laparoscopic TME group had minor urinary dysfunction that did not require long-term intermittent self-catheterization. This value compares with the findings in previous studies, which have reported incidences of bladder denervation after rectal resection ranging from 8% to 54% [22, 23]. Although total autonomic denervation of the bladder is unusual, urodynamic studies show a significant decrease in effective bladder capacity and increases in first sensation to void and residual urinary volume [22]. Many of these earlier studies did not use current TME techniques. Since the introduction of TME and the recognized need for autonomic nerve preservation, the incidence of bladder complications appears to have diminished to a level of 0% to 4% [9, 10]. In addition, some of the studies comparing laparoscopic and open TME observed little difference in rates of bladder dysfunction, similar to the current study [20, 23].
In comparision, sexual dysfunction remains a significant problem after TME. This was particularly the case for the 35 sexually active men in the current study, with 7 (20%) experiencing sexual dysfunction, compared with 6 (25%) of 24 sexually active women. These figures compare favorably with those of older studies that reported male impotence rates of 18% to 34% and ejaculatory problem rates of 19% to 54% [3, 24] and are similar to recent studies using TME, in which impotence is reported to be 11% to 25% [8, 9, 25].
The preaortic plexus may be damaged during ligation of the inferior mesenteric artery (IMA) at its origin on the anterior surface of the aorta. The superior hypogastric plexus and the origin of the hypogastric nerves are in direct posterior relation to the IMA and the superior rectal artery as it travels caudally. These sympathetic fibers are easily incorporated into the IMA pedicle if blunt or finger dissection is used to sweep the IMA off the front of the aorta (Fig. 1). Damage at this site can be avoided by the use of sharp dissection under direct vision with either diatermy or scissors. The correct plane that separates the sympathetic fibers from the back of the IMA is developed by dividing the zygosis (white line) of the sigmoid colon mesentery to the peritoneum of the posterior abdominall wall and dissecting medially on the mesocolic fat until the IMA is identified with the sympathetic fibers adherent or immediately posterior to it. In addition, this plane of dissection is continuous caudally with the extrafascial plane of rectal dissection that allows the thin fascial envelope of the mesorectum, the fascia propria, to be left intact during rectal dissection.
Our experience showed that laparoscopic TME can be performed safely and efficiently by surgeons who have adequate experience with the laparoscopic technique. Laparoscopic TME has some advantages over the open approach. The laparoscopic amplification of the inner image helps the operator to identify the interspace of loose connective tissue between the visceral and the parietal pelvic fascia. The 30° laparoscope may serve as the third eye of the surgeon, which can reach the narrow lesser pelvis, breaking through the blind zone and contributing a magnifying effect that makes it easier for the surgeon to identify and protect the pelvic autonomic nerve fiber and plexus (Figs. 2 and 3).
A significant difference in male sexual dysfunction was observed between the two groups. Interestingly, the rates of impotence and ejaculatory problems were similar, suggesting that both parasymphathetic and symphathetic nerves are equally at risk of injury and indicating that the most likely site of damage is at the lateral pelvic plexus where both autonomic systems converge. Another explanation attributes this to the proximity of the autonomic nerves to the anterolateral mesorectal fascia of Denonvillier [26, 27]. Accurate dissection in this plane can be easier, particularly during laparoscopic surgery, because of magnification features, and this may account for erectile function being the component of male sexual function most commonly affected by open surgery.
Because the stages of the tumors and the types of operation performed were similar between the two groups, the difference in sexual dysfunction must relate to technical differences between the two surgical approaches. Some studies have reported data on sexual dysfunction after laparoscopic TME. One study described a higher rate of male sexual dysfunction after laparoscopic resection than after open resection [23]. The sample size of Quah et al. [23] was small, comprising 15 patients who underwent laparoscopic TME and 22 patients who had open TME. A second study reporting on sexual dysfunction after laparoscopic TME found a nonsignificant trend toward male sexual dysfunction after laparoscopic TME [20]. More sexual dysfunction is seen after open TME [28]. Because the literature contains limited information, at this writing, it is difficult to draw meaningful conclusions regarding sexual function after laparoscopic TME.
Attention to autonomic nerve preservation is of paramount importance, particularly in low rectal resection, if bladder and sexual dysfunction is to be avoided. In our study, the rate of bladder denervation was low. The nerve damage must have occurred after the nerve to the bladder had branched off in the deep narrow pelvis where precise visualization and dissection may be more difficult.
Our data support the conclusion that rectal cancer surgery decreased male and female sexual function, but that the introduction of the laparoscopic technique significantly increased the number of patients with preserved genital function. In addition, surgically acquired bladder dysfunction, observed rather infrequently in both groups, was not enhanced by the introduction of laparoscopic surgery. The proposed advantages of laparoscopic technique, namely, improved visibility afforded by a magnified, well illiminated field of view, appear to aid the surgeon when confronted with technical surgical difficulties.
References
Chang PL, Fan HA (1983) Urodynamic studies before and/or after abdominoperineal resection of the rectum for carcinoma. J Urol 130:948–951
Kinn AC, Ohman U (1986) Bladder and sexual function after surgery for rectal cancer. Dis Colon Rectum 29:43–48
Santangelo ML, Romano G, Sassaroli C (1987) Sexual function after resection for rectal cancer. Am J Surg 154:502–504
Fazio VW, Fletcher J, Montague D (1980) Prospective study of the effect of resection of the rectum on male sexual function. World J Surg 4:149–152
Heald RJ (1988) The ‘holy Plane’: of rectal surgery. J R Soc Med 81:503–508
Pocard M, Zinzindohoue F, Haab F, Caplin S, Parc R, Tiret E (2002) A prospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer. Surgery 131:368–372
Masui H, Ike H, Yamaguchi S, Oki S, Shimada H (1996) Male sexual function after autonomic nerve-preserving operation for rectal cancer. Dis Colon Rectum 39:1140–1145
Maas CP, Moriya Y, Steup WH, Kiebert GM, Kranenbarg WM, van de Velde CJ (1998) Radical and nerve-preserving surgery for rectal cancer in The Netherlands: a prospective study on morbidity and functional outcome. Br J Surg 85:92–97
Nesbakken A, Nygaard K, Bull-Njaa T, Carlsen E, Eri LM (2000) Bladder and sexual dysfunction after mesorectal excision for rectal cancer. Br J Surg 87:206–210
Havenga K, Enker WE, McDermott K, Cohen AM, Minsky BD, Guillem J (1996) Male and female sexual and urinary function after total mesorectal excision with autonomic nerve preservation for carcinoma of the rectum. J Am Coll Surg 182:495–502
Enker WE, Havenga K, Polyak T, Thaler H, Cranor M (1997) Abdominoperineal resection via total mesorectal excision and autonomic nerve preservation for low rectal cancer. World J Surg 21:715–720
Kim NK, Aahn TW, Park JK, Lee KY, Lee WH, Sohn SK, Min JS (2002) Assessment of sexual and voiding function after total mesorectal excision with pelvic autonomic nerve preservation in males with rectal cancer. Dis Colon Rectum 45:1178–1185
Pikarsky AJ, Rosenthal R, Weiss EG, Wexner SD (2002) Laparoscopic total mesorectal excision. Surg Endosc 16:558–562
Zhou ZG, Hu M, Li Y, Lei WZ, Yu YY, Cheng Z, Li L, Shu Y, Wang TC (2004) Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 18:1211–1215
Morino M, Allaix ME, Giraudo G, Corno F, Garrone C (2005) Laparoscopic versus open surgery for extraperitoneal rectal cancer: a prospective comparative study. Surg Endosc 19:1460–1467
Lezoche E, Guerrieri M, De Sanctis A, Campagnacci R, Baldarelli M, Lezoche G, Paganini AM (2006) Long-term results of laparoscopic versus open colorectal resections for cancer in 235 patients with a minimum follow-up of 5 years. Surg Endosc 20:546–553
Lelong B, Bege T, Esterni B, Guiramand J, Turrini O, Moutardier V, Magnin V, Monges G, Pernoud N, Blache JL, Giovannini M, Delpero JR (2007) Short-term outcome after laparoscopic or open restorative mesorectal excision for rectal cancer: a comparative cohort study. Dis Colon Rectum 50:176–183
Mebust W, Roizo R, Schroeder F, Villers A (1991) Correlation between pathology, clinical symptoms and course of the disease. In: Cockett AT, Aso V, Chatelain C et al (eds) Proceeding of the international consultation on benign prostatic hyperplasia. WHO, Geneva, pp 51–62
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou PJ (2005) Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg 92:1124–1132
Keating JP (2004) Sexual function after rectal excision. ANZ J Surg 74:248–259
Chang PL, Fan HA (1983) Urodynamic studies before and/or after abdominoperineal resection of the rectum for carcinoma. J Urol 130:948–951
Quah HM, Jayne DG, Eu KW, Seow-Choen F (2002) Bladder and sexual dysfunction following laparoscopically assisted and conventional open mesorectal resection for cancer. Br J Surg 89:1551–1556
Cosimelli M, Mannella E, Giannarelli D, Casaldi V, Wappner G, Cavaliere F, Consolo S, Appetecchia M, Cavaliere R (1994) Nerve-sparing surgery in 302 resectable rectosigmoid cancer patients: genitourinary morbidity and 10-year survival. Dis Colon Rectum 37(Suppl):S42–S46
Enker WE (1992) Potency, cure, and local control in the operative treatment of rectal cancer. Arch Surg 127:1396–1402
Lindsey I, Guy RJ, Warren BF, Mortensen NJ (2000) Anatomy of Denonvilliers’ fascia and pelvic nerves, impotence, and implications for the colorectal surgeon. Br J Surg 87:1288–1299
Kinugasa Y, Murakami G, Uchimoto K, Takenaka A, Yajima T, Sugihara K (2006) Operating behind Denonvilliers’ fascia for reliable preservation of urogenital autonomic nerves in total mesorectal excision: a histologic study using cadaveric specimens, including a surgical experiment using fresh cadaveric models. Dis Colon Rectum 49:1024–1032
Marijnen CA, van de Velde CJ, Putter H, van den Brink M, Maas CP, Martijn H, Rutten HJ, Wiggers T, Kranenbarg EK, Leer JW, Stiggelbout AM (2005) Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 23:1847–1858
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asoglu, O., Matlim, T., Karanlik, H. et al. Impact of laparoscopic surgery on bladder and sexual function after total mesorectal excision for rectal cancer. Surg Endosc 23, 296–303 (2009). https://doi.org/10.1007/s00464-008-9870-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9870-7