Abstract
Background
Laparoscopic wedge resection (LWR) can be applied for the management of early gastric cancer without the risk of lymph node metastasis. Although LWR for early gastric cancer is one of the minimally invasive procedures, its radicality in cancer therapy is controversial. This study aimed to evaluate the long-term outcomes after LWR.
Methods
Data on 43 consecutive cases of LWR performed for preoperatively diagnosed mucosal gastric cancer were analyzed retrospectively in terms of long-term outcomes.
Results
No postoperative deaths occurred after LWR. Histologically, resected specimens showed submucosal invasion in 11 cases (26%) and positive surgical margins for cancer in 4 cases (9%). Three patients (7%) showed local recurrence near the staple line, and one patient (2%) died due to the local recurrence, but no lesional lymph node or distant recurrence occurred. The overall 5-year survival rate was 88%. The gastric remnant after LWR developed metachronous multiple gastric cancer in five cases (12%).
Conclusions
The findings show a relatively high incidence of positive surgical margin, local recurrence, and gastric remnant cancer after LWR. Although LWR can be performed for properly selected patients, periodic postoperative endoscopic examination is necessary to detect metachronous multiple gastric cancer and local recurrences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Local resection for early gastric cancer was first reported by Kitaoka et al. [1] in 1984. Laparoscopic wedge resection (LWR) is a procedure based on local resection [2]. This minimally invasive technique can be applied for the management of early gastric cancer without the risk of lymph node metastasis. However, because of the recent technical advances in endoscopic mucosal resection (EMR) and laparoscopically assisted distal gastrectomy (LADG) for early gastric cancer, the use of LWR for these lesions has gradually decreased. As a popular procedure for local resection of these lesions, EMR was introduced by some pioneer endoscopists in about 1978 [3, 4].
Compared with EMR, LWR offers the advantage of sufficient surgical margins, giving this method wider indications [5]. On the other hand, LADG, first performed by Kitano et al. [6] in 1991, was developed to treat early gastric cancer with the risk for lymph node metastasis. The advantage of LWR over LADG for the management of early gastric cancer without the risk of lymph node metastasis is that it preserves gastric function, maintaining a high quality of life without postgastrectomy syndromes such as dumping syndrome. However, the problem discouraging a wider application of LWR is the lack of long-term follow-up data. Although the procedure and long-term outcomes after EMR [3, 7] and LADG [8, 9] have been well studied, there are few reports on the long-term outcome after LWR [10–12].
In this study, we show short- and long-term follow-up data after LWR for 43 consecutive cases. Then we review our LWR experience with early gastric cancer to evaluate whether this local treatment was clinically safe and curative for cancer therapy.
Materials and methods
From January 1994 to December 1998, we surgically managed 397 cases of histologically proven early gastric cancer at Shikoku Cancer Center. The LWR procedure was performed for 43 (11%) of 397 patients.
The indications for LWR are (1) early gastric cancer within mucosal layer infiltration that does not invade the submucosal layer, with the depth of tumor invasion is confirmed by endoscopy or endoscopic ultrasound assessments, (2) no regional lymph node or distant metastasis confirmed by computed tomography (CT) scan, (3) lesion smaller than 2.1 cm for any type of cancer, and (4) lesion smaller than 6.1 cm only for elevated lesions of the intestinal type.
Lymph node dissection was not performed intraoperatively because the aforementioned lesions were verified as seldom showing lymph node metastasis [3, 4]. The LWR techniques by the lesion-lifting method have already been described [2]. We used preoperative endoscopic clipping around tumors to determine the resection line and confirmed intraoperatively that all the clips were in the resected specimen. If the resected specimen showed positive macroscopic surgical margins, the operation was converted to open surgery for additional resection.
Histologic examination was performed to determine tumor size, histologic type (intestinal or diffused), surgical margin, vertical invasion, and venous and lymphatic invasion. The clinicopathologic definition was based on the classification of the Japanese Gastric Cancer Association [13]. The patients had no adjuvant chemotherapy and were followed up by chest x-ray, ultrasound, or CT scan every 6 months and by endoscopic examination at 1-year intervals to detect a recurrent tumor or new lesions in the gastric remnant.
The StatView program, version 5 (SAS Institute, Inc., Cary, NC, USA) was used for all statistical analysis. The overall survival was calculated by the Kaplan-Meier method and analyzed by the log-rank test.
Results
As shown in Table 1 LWR was attempted for 43 patients (13 women and 30 men) with a median age of 64 years. Intraoperatively, the median operating time was 145 min (range, 60–315), and the estimated median blood loss was 40 g (range, 15–540 g). Four cases (9%) were converted to open surgery because the resected specimen showed positive macroscopic surgical margins. No postoperative death occurred, but there were six cases (14%) of postoperative complications (2 cases of wound infection and 4 cases of antral stenosis). All tumors in the four cases of antral stenosis were located in the lower third of the stomach. One of the four cases required distal gastrectomy due to the persistent gastric stasis. A regular diet was resumed at a median of 3 days (range, 2–6 days), and the median hospital stay was 12 days (range, 5–52 days). Clinicohistologic characteristics of the cases are shown in Table 1.
Histologically, the resected specimens were 0.5 to 6.0 cm in size. In 11 cases (26%), submucosal invasion had occurred, and 4 cases had microscopically positive surgical margins (9%). One case showed venous invasion (2%). Histologic examinations led to additional local resection for two patients whose microscopic surgical margin was positive (Table 2). A negative surgical margin was confirmed by histologic examination of the additionally resected specimen in both of these cases. The remaining two patients with a positive surgical margin did not undergo the additional resection because of old age (91 years) and synchronous advanced cancer other than gastric cancer, respectively.
In the long-term outcome analysis, the median follow-up period for all the patients was 80 months. In this study, there was no lesional lymph node or distant recurrence. However, three patients (7%) showed local recurrence near the staple line. One of these (2%) was the patient with a positive surgical margin who did not undergo the additional resection because of old age (Table 2). This patient subsequently died due to local recurrence. The remaining two local recurrences were experienced by patients who had additional resection for the positive surgical margins (Table 2). At this writing, these two patients are still alive without recurrence.
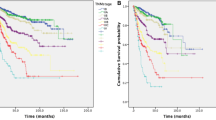
Two patients died of cancers other than gastric cancer, and four patients died of a non-malignancy-related disease. The overall 5-year survival rate was 88% by the Kaplan-Meier method (Fig. 1). The gastric remnant after LWR developed metachronous multiple gastric cancers in five cases (12%). To treat the remnant gastric cancer, distal or total gastrectomy was performed for three cases, and two patients underwent EMR. The cumulative 5-year prevalence rate of metachronous multiple gastric cancer after LWR was estimated to be 14% by the Kaplan-Meier method (Fig. 2).
Kaplan-Meier estimates for the cumulative prevalence of gastric remnant cancer after laparoscopic wedge resection (LWR). The cumulative 5-year prevalence was estimated at 14%. Data on 35 cases managed by postoperative endoscopic examinations at our hospital with a follow-up period longer than 1 year after LWR were analyzed
Discussion
In this study, we performed open partial gastrectomy (distal or proximal) for 320 cases of histologically proven early gastric cancer. Histologic examination in these cases showed no positive surgical margin (0%), which was significantly lower than in cases of LWR (9%) according to chi-square testing (data not shown). We also had no local recurrence after the partial gastrectomy (0%), which was significantly different from that seen after LWR (7%) according to chi-square testing (data not shown). Finally, the cumulative 5-year prevalence rate for metachronous multiple gastric cancers after partial gastrectomy was estimated to be 3%, which again was significantly lower than after LWR (14%) according to the log-rank test (data not shown).
Although the comparison between LWR and partial gastrectomy was a retrospective analysis and not a prospective, randomized trial, our results indicate that tumors removed by LWR are prone to having positive surgical margins, local recurrence near the staple line, and a gastric remnant with a background mucosa of metachronous multiple gastric cancers. However, the overall 5-year survival rate after partial gastrectomy (93%) is not significantly different from that obtained after LWR (88%) according to the log-rank test (data not shown).
No distant or lesional lymph node recurrence took place in this study. This suggests that the concept of LWR for early gastric cancer without the risk of lymph node metastasis was correct. If the surgical margin is negative, LWR is comparable with partial gastrectomy for these cases in terms of radicality for cancer therapy. There have been several reports about long-term outcome including local recurrence after LWR for early gastric cancer. Kobayashi et al. [10] treated 11 cases of early gastric cancer with LWR, observing no local recurrence and two cases of metachronous multiple gastric cancers. Hiki et al. [12] reported 16 cases of early gastric cancer removed by LWR, with no recurrence during a 60-month follow-up period. Ludwig et al. [11] managed 12 cases using LWR for early gastric cancer and did not observe any recurrence over 77 months postoperatively.
This reported absence of local recurrence after LWR for early gastric cancer differs from our results. One of the reasons for this difference is that we performed LWR for all tumors on any lesion. In contrast, the cited studies used LWR only for anterior wall or greater curvature lesions and laparoscopic intragastric resection for posterior or lesser curvature lesions [10, 11]. Laparoscopic intragastric resection is a procedure based on local resection for the treatment of mucosal gastric tumor [14]. This method is suitable for the removal of posterior or lesser curvature gastric lesions with adequate surgical margins. In our study, three of four tumors that showed positive microscopic surgical margin were located on the lesser curvature (Table 2). Posterior or lesser curvature lesions are difficult to resect using endoscopic linear staplers in LWR because access and traction are limited. Forcing the removal of lesser curvature gastric lesions by LWR may result in a positive microscopic surgical margin.
The other possible explanation is the size of the tumor. Our indication of tumor size for LWR was less than 2.1 cm for any type of cancer or less than 6.1 cm only for elevated lesions of the intestinal type. In contrast, the indication for LWR in the cited studies was less than 2.5 or 3 cm even for the intestinal type [10, 11]. In our study, we used preoperative endoscopic clipping around tumors to determine the resection line and confirmed intraoperatively that all the clips were in the resected specimen. Despite this method, the cases with one tumor 3 cm in size and those with two tumors larger than 4 cm showed a positive microscopic surgical margin (Table 2). In terms of surgical margin, large lesions (>3 cm) may be a contraindication for LWR. This probably happens because the resection margin should be parallel to the circular edge of the tumor. However, the actual resection line by linear staplers was linear. Therefore, preoperative endoscopic clipping may not be sufficient for the removal of a large tumor. The use of intraoperative frozen section should be taken into consideration to confirm the microscopic surgical margin.
Kobayashi et al. [10] reported two cases of antral stenosis after local resection. In our study, when linear staplers were used to remove tumors in the antral area, the direction of the resection line was set at a right angle to the longitudinal axis of the stomach to avoid antral stenosis. This was followed by flexible endoscopic intraoperative observation to confirm that no intraluminal narrowing was seen. Despite these precautions, we had four cases of antral stenosis, all of which were tumors located in the lower third of the stomach. Moreover, one of the four patients had to undergo partial gastrectomy due to persistent gastric stasis. This complication probably resulted from gastric wall thickening in the antral area due to postoperative swelling or injury to the branch of the nerve of Latarjet on the lesser curvature associated with antral motion. Lesions in the lower third of the stomach may not be an indication for LWR due to the high incidence of this complication.
A better solution for these contraindications for LWR, such as the large tumors and the difficult tumor locations, is to use LADG. Because of the recent technical advances in LADG for early gastric cancer, the reported long-term outcomes are comparable with those for open partial gastrectomy [8, 9]. On the other hand, a new technique of EMR, termed endoscopic submucosal dissection (ESD), has been developed in Japan. The ESD procedure removes mucosal lesions by the dissection of the submucosal layer under the lesion using endoscopic knives [15]. This allows the en bloc resection of larger lesions. The ESD procedure is not necessarily limited by lesion size, and it is predicted to replace conventional surgery for certain stages of early gastric cancer without the risk of lymph node metastasis [7]. The tumors that had been indicated for LWR can be managed currently using ESD.
Between these two advanced technologies, the indications for LWR have gradually decreased. In fact, recent studies show that the incidence of LADG is increasing, whereas that of LWR is decreasing [16–18]. However, LWR may have a comeback for the management of early gastric cancer with the risk of lymph node metastasis when used in combination with sentinel node navigation surgery. The feasibility of the sentinel node concept is currently under study [18].
In conclusion, although LWR can be performed for properly selected patients, extreme care must be taken with the surgical margin when LWR is performed for large tumors and posterior or lesser curvature tumors. Moreover, periodic postoperative endoscopic examination is necessary to detect metachronous multiple gastric cancers and local recurrences.
References
Kitaoka H, Yoshikawa K, Hirota T, Itabashi M (1984) Surgical treatment of early gastric cancer. Jpn J Clin Oncol 14:283–293
Ohgami M, Otani Y, Kumai K, Kubota T, Kim YI, Kitajima M (1999) Curative laparoscopic surgery for early gastric cancer: five years experience. World J Surg 23:187–192, discussion 192–183
Tada M, Murakami A, Karita M, Yanai H, Okita K (1993) Endoscopic resection of early gastric cancer. Endoscopy 25:445–450
Takekoshi T, Baba Y, Ota H, Kato Y, Yanagisawa A, Takagi K, Noguchi Y (1994) Endoscopic resection of early gastric carcinoma: results of a retrospective analysis of 308 cases. Endoscopy 26:352–358
Ohgami M, Otani Y, Kitajima M (1997) Laparoscopic surgery for early gastric cancer: its advantage and pitfall. Gan To Kagaku Ryoho 24:532–537
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Gotoda T (2007) Endoscopic resection of early gastric cancer. Gastric Cancer 10:1–11
Kitano S, Shiraishi N, Kakisako K, Yasuda K, Inomata M, Adachi Y (2002) Laparoscopy-assisted Billroth I gastrectomy (LADG) for cancer: our 10 years’ experience. Surg Laparosc Endosc Percutan Tech 12:204–207
Ikenaga N, Nishihara K, Iwashita T, Suehara N, Mitsuyama S (2006) Long-term quality of life after laparoscopically assisted distal gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A 16:119–123
Kobayashi T, Kazui T, Kimura T (2003) Surgical local resection for early gastric cancer. Surg Laparosc Endosc Percutan Tech 13:299–303
Ludwig K, Klautke G, Bernhard J, Weiner R (2005) Minimally invasive and local treatment for mucosal early gastric cancer. Surg Endosc 19:1362–1366
Hiki Y, Sakuramoto S, Katada N, Shimao H (2000) Combined laparoscopic–endoscopic procedure in stomach carcinoma. Chirurg 71:1193–1201
Japanese Gastric Cancer A. (1998) Japanese classification of gastric carcinoma: 2nd English edition. Gastric Cancer 1:10–24
Ohashi S (1995) Laparoscopic intraluminal (intragastric) surgery for early gastric cancer: a new concept in laparoscopic surgery. Surg Endosc 9:169–171
Gotoda T, Kondo H, Ono H, Saito Y, Yamaguchi H, Saito D, Yokota T (1999) A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: report of two cases. Gastrointest Endosc 50:560–563
Kitano S, Shiraishi N (2004) Current status of laparoscopic gastrectomy for cancer in Japan. Surg Endosc 18:182–185
Shimizu S, Noshiro H, Nagai E, Uchiyama A, Tanaka M (2003) Laparoscopic gastric surgery in a Japanese institution: analysis of the initial 100 procedures. J Am Coll Surg 197:372–378
Kitagawa Y, Kitano S, Kubota T, Kumai K, Otani Y, Saikawa Y, Yoshida M, Kitajima M (2005) Minimally invasive surgery for gastric cancer: toward a confluence of two major streams: a review. Gastric Cancer 8:103–110
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nozaki, I., Kubo, Y., Kurita, A. et al. Long-term outcome after laparoscopic wedge resection for early gastric cancer. Surg Endosc 22, 2665–2669 (2008). https://doi.org/10.1007/s00464-008-9795-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9795-1