Abstract
Aim
To compare the efficacy of laparoscopic sleeve gastrectomy (LSG) and BioEnterics intragastric balloon (BIB®) to lose weight and comorbidities after 12 months of follow-up before a more invasive bariatric procedure.
Methods
From January 2004 to December 2006, 40 patients underwent laparoscopic sleeve gastrectomy (LSG) as a first step in biliopancreatic diversion with duodenal switch. Controls (n = 80) were selected based on charts of patients who, during the same period, underwent BioEnterics intragastric balloon therapy. In both groups we considered: length of procedure, hospital stay, intraoperative or endoscopic complications, postoperative or postendoscopic complications, comorbidities at baseline, after 6 months (time of BIB removal), and after 12 months from baseline, and weight loss parameters [weight in kg, percentage excess weight less (%EWL), body mass index (BMI), and percentage excess BMI loss (%EBL)]. Results are expressed as mean ± standard deviation.
Results
Mortality, intra- and postoperative complications (in LSG group), and intra- and postendoscopic complications (in BIB group) were absent. Mean operative time in the LSG group was 120 ± 40 (range 60–200) min. Mean positioning time for BIB was 15 ± 5 (range 10–25) min. BMI at baseline was 54.1 ± 2.9 (range 45.1–55.9) kg/m2 and 54.8 ± 2.5 (range 45.1–56.2) kg/m2 in BIB and LSG groups, respectively. At 6-month follow-up, mean BMI was 46.2 ± 3.5 and 45.3 ± 5.5 kg/m2 in the BIB and LSG patients, respectively [p = not significant (ns)]. After 12 months BIB patients regained BMI, even if strictly followed with a diet regimen, while LSG patients continued to lose weight. Significant differences between groups were absent for the comorbidities considered.
Conclusions
Laparoscopic sleeve gastrectomy and BioEnterics intragastric balloon are two valid options for producing weight loss as a first-step procedure. LSG has all the related risks of general anesthesia, laparoscopic surgery, and digestive anastomosis, whereas BIB presents a very low rate of minor complications, such as psychological intolerance. For all these reasons, at this time, BIB is considered a better option than LSG as a first-step procedure in the short term (12 months).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity has become a major health problem in the last few decades. Bariatric surgery is now considered the only valid therapeutic option for morbidly obese patients but can be associated with significant risk, especially in patients affected by life-threatening comorbidities [4, 9, 19]. Moreover, the mesenteric fat can preclude optimal view for dissection maneuvers or tension-free intestinal anastomosis. For these reasons, several authors have suggested the need for a strategy to decrease these risks [1, 2, 5, 6]. Laparoscopic sleeve gastrectomy is a relatively new option originally published by Marceau et al. as a restrictive part of a duodenal switch malabsorptive procedure in an attempt to improve the results of biliopancreatic diversion without performing distal gastrectomy [16]. Recently, LSG has been proposed as a first step in the treatment of superobese patients or in patients with high operative risk prior to performing more complex bariatric procedures [2, 5, 16, 20].
BioEnterics intragastric balloon (BIB®) was originally placed for BMI reduction before bariatric surgical procedures to reduce all surgical and anesthesiological risks [10]. Busetto et al. demonstrated that preoperative treatment with the intragastric balloon reduced the risk of conversion to open surgery and the risk of intraoperative complications in superobese patients [5].
The aim of this study is to compare the efficacy of laparoscopic sleeve gastrectomy (LSG) and BioEnterics intragastric balloon (BIB®) to lose weight and comorbidities after 12 months of follow-up before a more invasive bariatric procedure.
Patients and methods
Patient selection
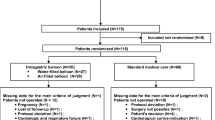
From January 2004 to December 2006, 40 patients underwent laparoscopic sleeve gastrectomy (LSG) as a first step in biliopancreatic diversion with duodenal switch. Controls (n = 80) were selected based on charts of patients who, during the same period, underwent BioEnterics Intragastric Balloon (BIB; Allergan, Irvine, CA, USA). These control patients were selected according to the rules of case-control studies. They were extracted from the prospective data base of our institution, with more than 1,000 BIB treated patients. To avoid the risk of systematic bias, two BIB patients matching one LSG were selected as controls only if they have the same sex, age (a difference of 3 months was tolerated), and BMI (a difference of 5 kg or 2 cm was tolerated). LSG patients represent the entire experience with this kind of bariatric procedure during the 3 years considered, and power calculation was not done. Demographics of both groups are reported in Table 1.
Laparoscopic sleeve gastrectomy
Under general anesthesia the patient was placed in lithotomic position. CO2 pneumoperitoneum was induced by Veress needle, then five trocars were positioned. The first step was to open the gastrocolic ligament attached to the stomach, usually starting 4–8 cm from the pylorus. Then the gastric greater curvature was freed up to the cardio-esophageal junction. At this time the anesthesiologist inserted a 34-Fr orogastric tube directed toward the pylorus. Then the stomach was resected with linear staplers parallel to orogastric tube along the lesser curve. The excision line was reinforced with a running suture, a methylene blue test was performed, and a subcostal left drain was placed. Finally, the resected stomach was removed.
BIB positioning
After sedation (2 mg/kg I.V. propofol) the patient was placed in a lateral decubitus position, esophagus, stomach, and duodenum were examined, and the Helicobacter pylori test performed. The instrument was retrieved and the BIB was inserted in the stomach, inflation was performed under direct vision by using saline (500 ml) and methylene blue (10 ml) solution. After 6 months the BIB was removed by endoscopy after complete deflation and with a dedicated instrument.
Study outline
In both groups we considered: length of procedure, hospital stay, intraoperative or endoscopic complications, postoperative or postendoscopic complications, comorbidities at baseline, after 6 months (time of BIB removal), and after 12 months from baseline, and weight loss parameters (kg, %EWL, BMI and %EBL). Results are expressed as mean ± standard deviation and range for numerical variables and absolute numbers. Statistical analysis was done by means of Student’s t-test for numerical variables and χ 2-test or Fisher’s exact test for categorical variables. Values of p < 0.05 was considered significant.
Results
Mortality, intra- and postoperative complications (in LSG group), and intra- and postendoscopic complications (in BIB group) were absent. Mean operative time in the LSG group was 120 ± 40 (range 60–200) min. Mean positioning time for the BIB was 15 ± 5 (range 10–25) min. Mean hospital stay was 2 ± 1 and 5 ± 2 days in BIB and LSG patients, respectively. BMI at baseline was 54.1 ± 2.9 (range 45.1–55.9) kg/m2 and 54.8 ± 2.5 (range 45.1–56.2) kg/m2 in BIB and LSG groups, respectively. All patients were present at follow-up. At 6-months follow-up mean BMI was 46.2 ± 3.5 and 45.3 ± 5.5 kg/m2 in BIB and LSG patients, respectively (p = ns). After 12 months BIB patients regained weight, even if strictly followed with a diet regimen, while LSG patients continued to lose weight. In fact at this follow-up mean BMI was 48.1 ± 4.1 and 43.1 ± 7.2 kg/m2 in BIB and LSG groups, respectively (p = ns) (Table 2). A similar incidence of failure (weight loss <10%) was recorded in both groups (2/40 and 4/80; 10%).
The correlation between weight loss and comorbidities in both groups at 6-month follow-up is reported in Table 3. Significant differences between groups were absent for the comorbidities considered. Sixteen patients in the LSG group and 12 patients in the BIB group suffered from joint pain at baseline. At 6-months follow-up pain and disability had completely resolved in 2 of the 16 LSG patients and 2 of the 12 BIB patients. Joint pain improvement and less drug consumption was recorded in six and two patients of the LSG and BIB group, respectively. Ten patients in the LSG group and eight patients in the BIB group suffered from type II diabetes with high hemoglobin A1c (HbA1c) levels at baseline. Complete regression of hyperglycemia with HbA1c normalization was observed in two patient of BIB group. Hyperglycemia fell around normal cutoff range (60–110 mg/dl) in ten and six patients of the LSG and BIB group, respectively. Ten patients in the LSG group and eight patients in the BIB group suffered from obstructive sleep apnea syndrome (OSAS) at baseline. After 6 months follow-up this comorbidity was resolved in all patients of both groups. Eight patients of both groups were affected by dyslipemia at baseline. After 6 months follow-up only a slight improvement was recorded in four patients of both groups. Twenty-two patients in the LSG group and 24 patients in the BIB group suffered from hypertension at baseline. At this time diastolic hypertension of 95–100 mmHg and normal systolic parameters were recorded in four patients of both groups. Complete resolution without drug consumption was observed at 6-month follow-up. In 14 patients of the LSG group and 16 patients of the BIB group only systolic hypertension was recorded (150–200 mmHg) at baseline. In ten patients of both groups the hypertension fell to normal values with less drug consumption, while the remaining patients remaining unchanged. In four patients of both groups both systolic and diastolic hypertension was recorded at baseline. In all these patients at 6-month follow-up the normal values were reached with less drug dosage.
Discussion
Laparoscopic sleeve gastrectomy and BioEnterics intragastric balloon have recently been introduced as first-step bariatric procedures to minimize surgical risk in patients before undergoing a second, more invasive, bariatric procedure [1, 2, 10, 14, 18, 20]. Laparoscopic sleeve gastrectomy was usually followed by either laparoscopic duodenal switch or Roux-en-Y gastric bypass [1, 14, 20]. BioEnterics intragastric balloon can be followed by any kind of bariatric surgical procedure [2, 10].
Recently Milone et al. [18], in patients with BMI >50 kg/m2, indicated that laparoscopic sleeve gastrectomy is superior to BioEnterics intragastric balloon positioning in terms of both mean weight loss (45.5 versus 22.3 kg) and %EWL (35% versus 24%). BMI decreased from 69 to 53 kg/m2 and from 59 to 51 kg/m2 in LSG and BIB patients, respectively. Comorbid conditions decreased in 90% of patients in both groups. The authors concluded that LSG was a safe procedure and that BIB was safe and well tolerated by 93% of their patients. They concluded that, although the BIB procedure shows efficacy in reducing weight, LSG does so faster and to a greater degree, thus suggesting that this may be a superior procedure as a first stage for superobesity. In the present study, mean weight loss parameters at time of BIB removal were similar to those observed at 6-month follow-up in patients treated by laparoscopic sleeve gastrectomy. A similar nonsignificant pattern was observed for comorbidities. After another 6 months of follow-up, patients treated with BIB regain weight, as shown also in other experiences, while patients with sleeve gastrectomy continued to lose weight [2].
The basic issue is to consider the complications that can occur in both these procedures. BIB is a less invasive endoscopic procedure, without general anesthesia and all the potential complications related to laparoscopic surgery and wide stapled suture as in laparoscopic sleeve gastrectomy. In the literature several experiences have stressed that BIB is a reversible and safe procedure with a very low rate of complications [2, 10, 11, 23]. In BIB, serious complications, such as bowel obstruction and gastric perforation, were occasionally but rarely reported [8, 10, 23]. The most frequent complication was patient balloon intolerance, which can lead to balloon removal [8, 10, 23]. BIB deflation and rupture are historical complications linked to older manufactured devices or to technical errors in their placement. Other minor complications are gastroesophageal reflux and peptic ulcer that can be easily treated by drugs [8, 10, 23]. Complications of laparoscopic sleeve gastrectomy reported in the literature seem to have a higher rate and to be frequently life threatening [7, 14, 23]. Melissas et al. [17] in their study reported a 15.8% rate of postoperative hemorrhage, treated with blood transfusion. In the same report the rate of leak of the upper part of the excision line was 5.5%. Roa et al. [21] report a rate of 1/30 major complications in sleeve gastrectomy (staple-line leak treated by further surgery under general anesthesia). Major complications ranging between 13% and 15.3% have been reported by other studies [6, 14]. Gastric remnant dilation was also described as an LSG complication requiring further surgery, such as re-sleeve gastrectomy [3, 15].
More recently, in 2007, Gumbs et al. [12, 13] reported a review on 646 patients who underwent laparoscopic sleeve gastrectomy, with 0.6% mortality rate. In this study they report 4.5% reoperation rate and 0.9% leak rate. During 2008 several other experiences have been reported on technique and indications of laparoscopic sleeve gastrectomy. Rubin et al. [22] report on 120 consecutive patients with four (3.33%) intraoperative complications (technical problems, n = 2; short vessels bleeding, n = 2), without laparoscopic conversion and postoperative complications. Kueper et al. [14] report on 16 patients with two (12.5%) postoperative complications: one wound infection and one bleeding requiring relaparoscopy.
Conclusions
Laparoscopic sleeve gastrectomy and BioEnterics intragastric balloon are two valid options for producing weight loss as a first-step procedure. At 6-month follow-up efficacy in terms of weight loss and comorbidity improvement is the same in both procedures. At 12-month follow-up LSG patients presented a greater but not significant weight loss as compared with BIB-treated patients. LSG has all the related risk of general anesthesia, laparoscopic surgery, and digestive anastomosis, while BIB presents a very low rate of minor complications, such as psychological intolerance. LSG complications can be life threatening, requiring reoperation under general anesthesia. BIB complications are usually resolved by endoscopic removal. LSG is an irreversible procedure, while BIB is completely reversible. For all these reasons, at this time, we consider BIB a better option than LSG as a first-step procedure in the short term (12 months). Further prospective evaluations are mandatory for these procedures to establish in which patients and procedure BIB or LSG are really useful or a fashionable trend.
References
Almogy G, Crookes PF, Anthone GJ (2004) Longitudinal gastrectomy as a treatment for the high risk super-obese patients. Obes Surg 14:492–497
Angrisani L, Lorenzo M, Borrelli V, Giuffré M, Fonderico C, Capece G (2006) Is bariatric surgery necessary after intragastric balloon treatment? Obes Surg 16:1135–1137
Baltasar A, Serra C, Perez N, Bou R, Bengochea M (2006) Re-sleeve gastrectomy. Obes Surg 16:1535–1538
Buchwald M, Williams SE (2004) Obesity surgery worldwide. Obes Surg 14:1157–1164
Busetto L, Segato G, De Luca M et al (2004) Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: a case control study. Obes Surg 14:671–676
Cottam D, Qureshi FG, Mattar SG et al (2006) Laparoscopic sleeve gastrectomy as an initial weight loss procedure for high risk patients with morbid obesity. Surg Endosc 20:859–863
Eisendrath P, Cremer M, Himpens J, Cadiere GB, Le Moine O, Deviere J (2007) Endotherapy including temporary stenting of fistulas of the upper gastrointestinal tract after laparoscopic bariatric surgery. Endoscopy 39:625–630
Eynden FV, Urbain P (2001) Small intestine gastric balloon impact on treated by laparoscopic surgery. Obes Surg 11:646–648
Flum DR, Salem L, Elrod JB et al (2005) Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA 294:1903–1908
Genco A, Bruni T, Doldi SB et al (2005) BioEnterics Intragastric Balloon: the Italian experience with 2,515 patients. Obes Surg 15:1161–1164
Genco A, Cipriano M, Bacci V et al (2006) Bioenterics Intragastric Balloon (BIB): a double blind, randomised, controlled, cross-over study. Int J Obes 30:129–133
Gumbs A, Gagner M, Dakin G et al (2007) Sleeve gastrectomy for morbid obesity. Obes Surg 17:562–569
Hamoui N, Anthone GJ, Kaufman HS, Crookes PF (2006) Sleeve gastrectomy in the high-risk patients. Obes Surg 16:1445–1449
Kueper MA, Kramer KM, Kirschniak A et al (2008) Laparoscopic Sleeve Gastrectomy: standardized technique of a potential stand-alone bariatric procedure in morbidly obese patients. World J Surg 32:1462–1465
Langer FB, Bohdjalin A, Felberbauer FX et al (2006) Does gastric dilatation limit the success of sleeve gastrectomy as a sole operation for morbid obesity? Obes Surg 16:166–171
Marceau P, Biron S, Bourque RA et al (1993) Biliopancreatic diversion with a new type of gastrectomy. Obes Surg 3:29–35
Melissas J, Kuokouraki S, Askoxylakis J et al (2007) Sleeve gastrectomy – a restrictive procedure? Obes Surg 17:57–62
Milone L, Strong V, Gagner M (2005) Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for superobese patients (BMI > or = 50). Obes Surg 15:612–617
O’Brien PE, McPhail T, Chaston TB et al (2006) Systematic review of medium-term weight loss after bariatric operations. Obes Surg 16:1032–1040
Regan JP, Inabnet WB, Gagner M (2003) Early experience with two stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 13:861–864
Roa PE, Kaidar-Person O, Pinto D et al (2006) Laparoscopic Sleeve Gastrectomy as treatment for morbid obesity: technique ad short-term outcome. Obes Surg 16:1323–1326
Rubin M, Yehoshua RT, Stein M et al (2008) Laparoscopic Sleeve Gastrectomy with minimal morbidity. Early results in 120 morbidly obese patients. Obes Surg
Sallet JA, Marchesini JB, Paiva DS et al (2004) Brazilian multicenter study on the intragastric balloon. Obes Surg 14:991–998
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Genco, A., Cipriano, M., Materia, A. et al. Laparoscopic sleeve gastrectomy versus intragastric balloon: a case-control study. Surg Endosc 23, 1849–1853 (2009). https://doi.org/10.1007/s00464-008-0285-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0285-2