Abstract
Background
The laparoscopic Nissen fundoplication has become a frequently performed procedure in infants and children who suffer from gastroesophageal reflux disease (GERD). In this study we describe our 8-year experience with 106 consecutive laparoscopic Nissen fundoplications.
Methods
From January 1994 to May 2002, we included 106 consecutive patients (57 neurologically normal (NN) and 49 neurologically impaired (NI)). The indications were symptomatic GERD, pulmonary symptoms or a combination of both. Patient’s outcome was assessed by symptom evaluation, technical examinations and a questionnaire.
Results
Mortality was 0% and conversion rate was 2.8%. Major postoperative complications occurred in 12 patients, mostly neurologically impairment. Dysphagia occurred in 23 patients of which 4 required dilatations and 2 a redo Nissen. Gas bloating occurred in 15 children, with spontaneous regression in all. Recurrent pneumopathies were seen in four children. Documented recurrence of reflux occurred in three symptomatic patients. Redo laparoscopic surgery was performed in six patients.
A questionnaire was sent to each patient’s parents. This showed that most patients had a normal or clearly improved quality of life (93.1% NN, 90.5% NI). Most patients were satisfied with the result and up to 39.5% gave a maximum satisfaction score.
Conclusion
The laparoscopic Nissen fundoplication can safely be performed with a low conversion rate and no surgical mortality in neurologically normal and neurologically impaired children. Neurologically impaired children are more susceptible to per- and postoperative complications. A good quality of life and a high index of satisfaction could be achieved in most patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastroesophagal reflux disease (GERD) is a common problem in the paediatric population. Infants often have symptoms like vomiting and regurgitation. Children often have heartburn, dysphagia, and respiratory symptoms. Studies [1, 2] have shown that GERD is a physiologic phenomenon that usually disappears when infants grow up. When GERD persists, it can cause complications like oesophagitis, chronic respiratory symptoms, failure to thrive, and even sudden infant death syndrome.
Since the development of minimally invasive surgery, laparoscopic Nissen fundoplication has become a regular therapeutic procedure in children and has gained much importance in the treatment of GERD in children. This study describes our experience with 106 consecutive laparoscopic Nissen fundoplications in infants and children.
Materials and methods
Patients
From January 1994 through May 2002, 106 laparoscopic Nissen fundoplications in children have been performed in our institution. Fifty-seven patients (53.8%) were neurologically normal (NN) and 49 patients (46.2%) were neurologically impaired (NI). The median age in the NN group was 4 years 11 months (range = 5 months to 18 years) and in the NI group it was 5 years and 6 months (range = 9 months to 18 years). There were 64 boys and 42 girls. Neurologic impairment was caused by perinatal asphyxia (n = 12), metabolic disorder (n = 3), trisomy 21 (n = 2), Williams syndrome (n = 2), autism (n = 1), battered child syndrome (n = 1), Arnold Chiari (n = 1), RETT syndrome (n = 1), and an unknown aetiology (n = 26). Fourteen patients had had a previous abdominal surgical procedure: ten preoperatively placed gastrostomy tubes (2 NN, 8 NI) and four repairs of a oesophageal atresia (4 NN).
Indications
Indication for surgery was always a symptomatic reflux presented by upper gastrointestinal symptoms, pulmonary symptoms, or a combination of both; 57.8% (n = 33) of the NN children had gastrointestinal symptoms, 21.1% (n = 12) had pulmonary symptoms, and 21.1% (n = 12) had both. In the NI children this was respectively 38.7% (n = 19), 32.7% (n = 16), and 28.6% (n = 14). Preoperative evaluation included an endoscopy, an upper gastrointestinal contrast series, and/or a 24-h pH study. In some cases manometry, scintigraphy, or bronchoscopy with bronchial lavage was performed. All of the patients who were operated on had documented symptomatic reflux. Table 1 shows the investigations performed and the percentage of reflux found by these investigations in both groups.
Technique
All procedures were performed under general anaesthesia with the patient in dorsal decubitus. The abdomen was insufflated through a Verres needle above the umbilicus. A five-trocar technique was used routinely. Trocars were placed above the umbilicus (camera port), in the right upper quadrant (liver retractor), in the left upper quadrant (stomach retractor), subxiphoidal, and between the camera port and the left upper quadrant (working channels).
The same operation was performed in each case. After retracting the left liver lobe, the minor omentum was divided, preserving the vagal branches to the liver. The right diaphragmatic crus was identified. After incising the overlying dorsal peritoneum and identifying the posterior vagal nerve, the posterior and right surface of the oesophagus was dissected. A Penrose drain was placed around the oesophagus as a traction device. With this Penrose drain, the oesophagus was pulled to the right and the left side was further dissected until the oesophagus was completely mobile. In general, approximately 3 cm of distal oesophagus had to be easily reduced underneath the diaphragm. Then the gastrophrenic ligament and a couple of short gastric vessels were divided to allow the construction of a loose fundoplication. The crura were approximated with one or two nonabsorbable sutures, taking care not to narrow the hiatus too tightly. The fundus was then pulled behind the oesophagus to the right side. Two nonabsorbable stitches were placed on the fundus and the body of the stomach to construct a short floppy wrap of about 1.5–2 cm. A third stitch was placed more distally, securing the wrap to the distal oesophagus. An intraoesophageal calibration tube was not used. A contrast study was performed 1 or 2 days after the procedure. If this investigation showed no signs of leakage or intrathoracic herniation, oral feeding was started.
Evaluation
During follow-up, patients were asked about the recurrence of symptoms and surgical side effects. If patients complained about reflux-associated symptoms, one or more technical investigations (endoscopy, 24-h pH study, contrast study, and/or manometry) were performed to identify true recurrence. At the 1-year follow-up, we offered all asymptomatic patients a control reflux work-up by means of a 24-h pH study. In 24 cases the patient and/or the patient’s parents gave consent.
A questionnaire about quality of life was sent to the patient’s parents when this study was done. We asked the parents to fill in the questionnaire together with their child. In cases of neurologic impairment, the questionnaire was completed by the parents. Because there is no current validated score in the literature to measure the postoperative quality of life in children after antireflux surgery, we asked them to compare the postoperative quality of life with the preoperative (worse/normal/improved) and to score their satisfaction from 0 to 10. A score of 0 was defined as being very discontent and a score of 10 as being very satisfied. This was done by marking the score on a graphical scale from 0 to 10.
Results
Peroperative
A laparoscopic Nissen fundoplication was possible in 103 of 106 patients. Conversion to the open procedure was necessary in three neurologically impaired children (2.8%). The reason for conversion was difficult visualisation of the anatomical structures. In two patients this was the result of a preoperatively placed gastrostomy tube and in one because of a concomitant extreme scoliosis.
Minor peroperative complications occurred in 8 (14.0%) neurologically normal children and in 6 (12.2 %) neurologically impaired children. The complications consisted of 8 bleedings (5 NN, 3 NI), 1 segmental infarction of the spleen (1 NN), 2 perforations of the pleura (2 NN), 2 serosal lesions of the stomach (2 NI), and 1 perforation of the pericardium (1 NI). All complications were easily controlled at the time of the operation and were without any consequence.
Associated surgery consisted of the placement of a gastrostomy tube in 24 patients (2 NN, 22 NI), a liver biopsy in 2 patients (2 NI), and a lung biopsy, which was performed transhiatal, in 1 patient (1 NN).
Postoperative
Major postoperative complications that occurred during the immediate postoperative course were seen in 12 patients (11.3%). Seven neurologically impaired patients had medical complications: one catheter sepsis, one status epilepticus, and five pneumonia. Complications requiring surgery were seen in both groups. In the neurologically normal group there was one intrathoracic herniation and one abdominal wall haematoma. In the neurologically impaired group two patients had an intrathoracic herniation and one patient needed a revision because of leakage of a preoperatively placed gastrostomy tube. In all three patients with an intrathoracic migration of the wrap, the migration was detected on a contrast study performed the day after the operation. They all successfully underwent immediate redo surgery, with reduction of the migrated wrap.
The median hospital stay was 4.5 days for the neurologically normal children (range = 2–11 days) and 9.3 days for the neurologically impaired children (range = 2–30 days). The median follow-up was 19.5 months (minimum = 6 months, maximum = 108 months).
During follow-up, reflux-associated symptoms occurred in 24 patients (15 NN, 9 NI). A reflux work-up by means of a contrast study, an endoscopy, and/or a 24-h pH study was performed in 19 (13 NN, 6 NI). Three work-ups (3 NN) showed evidence of recurrent GER. One patient improved spontaneously, one became asymptomatic with proton-pump inhibitors, and one required a redo laparoscopic Nissen fundoplication and is now asymptomatic. The details of these three patients are shown in Table 2. The 16 other work-ups (10 NN, 6 NI) were completely normal. Subsequent spontaneous improvement was seen in 11 patients (6 NN, 5 NI), improvement with proton-pump inhibitors in 2 patients (1 NN, 1 NI), and 3 patients (3 NN) still have persistent symptoms. Five patients (2 NN, 3 NI) had symptoms that were rather mild so that the patient and/or the patient’s parents did not accept the proposed reflux work-up. They all improved spontaneously.
Undesired surgical side effects were seen in 38 patients (27 NN, 11 NI). Gas bloating occurred in 15 patients (9 NN, 6 NI), with spontaneous improvement in all. Dysphagia was seen in 23 patients (18 NN, 5 NI) in which 15 patients (10 NN, 5 NI) improved spontaneously, 4 patients (4 NN) required dilatations, 2 patients (2 NN) had a laparoscopic redo at, respectively, 21 days and 1 year postoperatively, and 2 patients (2 NN) still have persistent complaints although they havd a completely normal functional work-up.
In the asymptomatic patients we routinely offered a control 24-h pH study at 1 year after surgery. This was accepted by 24 patients (16 NN, 8 NI). Pathologic reflux was seen in 3 patients (3 NN). An asymptomatic herniation occurred in 2 patients (2 NI; 1 month and 2 years 2 months postoperatively) and they are still in follow-up and are still asymptomatic.
Postoperative recurrent pneumopathies were seen in 7.4% (n = 4) of the children who had preoperative pulmonary symptoms. Three patients, however, showed improvement of their symptoms after the procedure and one was lost during follow-up.
Seven neurologically impaired children died during follow-up. This was due to their medical condition and was not related to the surgical procedure.
Altogether we had to perform a redo Nissen in 5.6% (n = 6). An early redo was performed in three patients because of migration of the fundoplication. A late redo was done because of dysphagia in two children and proven reflux in one symptomatic patient.
Quality of life and satisfaction
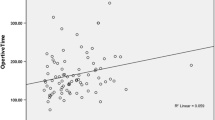
A questionnaire on the quality of life and satisfaction was sent to each patient’s parents. We received 76 answered questionnaires. Table 3 shows that up to 93.1% of the neurologically normal and 90.5% of the neurologically impaired children had a normal or improved quality of life. The full spread of the satisfaction scores is shown in Figure 1. Thirty patients (39.5%) gave the maximum score.
Discussion
Gastroesophageal reflux disease has become an important issue in the paediatric population. Although the exact prevalence of GERD is difficult to evaluate, Gibbons et al. [3] estimate that GERD represents approximately 4% of all paediatric hospital admissions. In most children a spontaneous resolution can be expected [1, 2, 4, 5], but in some cases complications such as oesophagitis, pneumopathies, bradycardia, and apnea can occur. Laparoscopic Nissen fundoplication as treatment for GERD has become very popular since the development of minimally invasive surgery. The efficiency and safety of this procedure has been shown in several studies [6–10].
The first large study on laparoscopic Nissen fundoplication was published by Rothenberg et al. [10]. They analysed 220 consecutive laparoscopic Nissen fundoplications in children. In 99.1% of his patients the procedure could be done laparoscopically; in 0.9% a conversion was necessary. Postoperative complications occurred in 7.3% and consisted mostly of dysphagia and gastrostomy-related problems. In 3.2% of the patients there was a recurrence of reflux that required a redo Nissen, all due to an anatomical failure of the fundoplication (intrathoracic herniation and dehiscence of the fundoplication). It appears that Rothenberg’s complication ratio is less than ours. However, his group of patients consisted of only 27 neurologically impaired children (12.2%), whereas ours was 49 (46.2%).
It is generally accepted that neurologically impaired children are complex patients and should be studied separately from neurologically normal children when it comes to GERD and Nissen fundoplication [7]. The presenting symptoms often differ from those of the neurologically normal group. Subjective symptoms like heartburn and abdominal pain are less frequent than objective symptoms like regurgitation, failure to thrive, vomiting, and haematemesis, indicating a more advanced and often more complicated stage of the disease. Because of their neurologic impairment, they are also more susceptible to early postoperative complications, especially pulmonary infections. This is mostly the result of poor oropharyngeal handling of their saliva with aspiration. We also found that performing a Nissen fundoplication in these children is often more difficult because of a preoperatively placed gastrostomy tube and other comorbidities like extreme scoliosis. In our series, this resulted in a higher conversion rate in this group. That these children are more prone to per- and postoperative complications has also been shown in a recent study by Esposito et al. [7]. They studied the postoperative complications in 80 neurologically impaired children after a laparoscopic antireflux procedure. Postoperative complications were seen in 24 patients (30%). A redo procedure was even necessary in five patients: two had a migration of the fundoplication and three were still symptomatic despite the antireflux procedure.
We also noticed that intrathoracic herniation was more common in the neurologically impaired children. This type of herniation has been a well-known phenomenon in open antireflux surgery, occurring more often in neurologically impaired children. Pearl et al. [11] states that the success ratio of the procedure is dependent on the neurologic status of the patient and that the major cause of failure is intrathoracic herniation. Because of concomitant spasticity, convulsions, or recurrent pneumopathies, neurologically impaired children have often a problem of straining which can cause this herniation. Scoliosis has also been defined as a contributing factor.
Evaluating the recurrence of reflux in the paediatric population is complex. We noticed that 22.6% (n = 24) of the children in our study had reflux-associated symptoms during follow-up. In most cases a functional investigation was accepted. The majority of these patients, however, were found normal on investigation. Only three neurologically normal patients had documented reflux (2.8%). Three other patients continued to have persistent reflux symptoms, despite completely normal investigation.
The recurrence rate after laparoscopic Nissen fundoplication has been reported in the literature to range from 2.1% to 8.7% [6, 10, 12] overall and from 6.25% to 13% specifically in the neurologically impaired children [7, 13]. However, this higher incidence of recurrence in neurologically impaired children was not seen in our series. A possible explanation could be postoperative intrathoracic herniation. Studies have shown that this anatomical failure is an important cause for recurrence [12–14]. Kawahara et al. [13], who studied the lower oesophageal sphincter’s motor activities associated with recurrence of GERD after a fundoplication in neurologically impaired children, saw that all their patients with recurrence of reflux had an anatomical failure. This was associated with transient lower oesophageal relaxations that occurred more frequently and that the relaxation was more profound. This herniation was seen on the postoperative contrast study in two neurologically impaired children and was treated immediately. Therefore, these patients were not counted as having a possible failure due to an anatomical failure during follow-up. We operate immediately if a herniation is detected by the early postoperative contrast study, especially in neurologically impaired children, who are not always able to express their complaints during follow-up. We also think that an anatomical failure is not the only cause for recurrence of symptoms. In our series three symptomatic patients with documented recurrence did not have an anatomical failure, and three patients with documented wrap failure were completely asymptomatic. These findings were also reported in other studies [7, 12]. We think that other mechanisms that are not well known yet also play an important role in the development of recurrence of symptoms.
We not only performed a reflux work-up in the symptomatic patients, we also tried to perform a 24-h pH study in the asymptomatic patients at 1-year follow-up. This was accepted by 24 patients (16 NN, 8NI). It was striking to see that three neurologically normal children showed evidence for reflux on their 24-h pH study. We compared the graphical data of these patients with the data of a symptomatic patient. Although both patients were defined as having pathological reflux according to the standard computerised criteria, we saw that one of the asymptomatic patients never had a pH far below 3 and that he had been drinking acid containing liquids (coca-cola) which resulted in a fall of pH. We also think that such a curve may reflect an effect of food stasis and subsequent acid fermentation. It is therefore of paramount importance to add a visual interpretation of the curves to the computerised data and to search for a correlation between symptoms and pathologic technical findings before diagnosing a true recurrence of reflux.
Dyphagia and gas bloating are important side effects of laparoscopic antireflux surgery [8, 15]. Early dysphagia is mostly caused by postoperative oedema, but in some cases an approximation of the crura that is too tight or a wrap that is too tight could be the cause [8]. In our series, dysphagia disappeared spontaneously most of the time, but six cases eventually required further treatment: two patients needed a laparoscopic redo and four patients needed dilatations. It is our experience that dysphagia did not occur frequently in the group of neurologically impaired children. Possible explanations are that neurologically impaired children are more restricted in expressing their complaints and that many of these patients are fed through a gastrostomy tube so that dysphagia cannot occur.
Gas bloating is defined as an uncomfortable abdominal feeling due to accumulation of air in the stomach, often associated with the inability to belch. In our series this was a common phenomenon in both groups, but it always disappeared spontaneously. In the group of neurologically impaired children with a gastrostomy tube, this problem could easily be resolved by opening the gastrostomy button.
The goal of this study was not only to determine the incidence of postoperative reflux and procedure-related symptoms, but also to get an idea about the quality of life and general satisfaction after a laparoscopic Nissen fundoplication. Although some children still had reflux- or procedure-related complaints, 93.1% of the neurologically normal and 90.5% of the neurologically impaired children who sent back their questionnaires had a normal or clearly improved quality of life. Concerning the patient’s satisfaction, 84.1% of the neurologically normal and 87.6% of the neurologically impaired children gave a score of 5 or more and up to 39.5% gave the maximum score. Five patients, however, reported a quality of life that was worse than that preoperative. We tried to discover the cause of this discontent. There was one patient who had documented psychological problems, one patient with mucoviscidosis, two patients who did not mention any complaints during follow-up, and one patient whose mother had psychological problems and did not fill in the questionnaire accurately.
In conclusion we can say that children with GERD have complex symptoms and associated pathology. Laparoscopic Nissen fundoplication can be performed safely with a low conversion rate and no surgical mortality. Neurologically impaired children, however, are more susceptible to per- and postoperative complications. A Redo Nissen was necessary in 5.6% and was always performed laparoscopically. Variations between postoperative symptoms and the objective assessment occur, and we think it is important to search for a correlation between these symptoms and pathologic findings before defining it as a true reflux. In most cases, however, spontaneous improvement of symptoms was seen. A high index of satisfaction and good quality of life could be achieved in most patients.
References
Carré IJ (1985) The natural history of the partial thoracic stomach in children. Arch Dis Child 34:344–353
Hassall E (2005) Decisions in diagnosing and managing chronic gastroesophageal reflux disease in chidren. J Pediatr 146:S3–S12
Gibbons TE, Stockwell J, Kreh RP (2001) Population-based epidemiology of gastroesophageal reflux disease in hospitalized U.S. children. Gastroenterology 20:419
Nelson SP, Chen EH, Syniar GM, Christoffel KK (1997) Prevalence of symptoms of gastroesophageal reflux during infancy. A paediatric practice-based survey. Paediatric Practice Research Group. Arch Pediatr Adolesc Med 151:569–572
Nelson SP, Chen EH, Syniar GM, Christoffel KK (2000) Prevalence of symptoms of gastroesophageal reflux during childhood. A pediatric practice based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med 154:150–154
Esposito C, Montupet P, Amici G, Desruelle P (2000) Complications of laparoscopic antireflux surgery in childhood. Surg Endosc 14:622–624
Esposito C, Van Der Zee DC, Settimi A, Doldo P, Staiano A, Bax NM (2003) Risks and benefits of surgical management of gastroesophageal reflux in neurologically impaired children. Surg Endosc 17:708–710
Hossein A, Captier G, Lopez M, Forgues D, Galifer RB (2001) Evaluation of 142 consecutive laparoscopic fundoplications in children: Effects of the learning curve and technical choice. J Pediatr Surg 36:921–926
Mattioli G, Esposito C, Lima M, Garzi A, Montinaro L, Cobellis G, Mastoianni L, Aceti MG, Falchetti D, Repetto P, Pini Prato A, Leggio S, Torri F, Ruggeri G, Settimi A, Messina M, Martino A, Amici G, Riccipetitoni G, Jasonni V (2002) Italian multicenter survey on laparoscopic treatment of gastroesophageal reflux disease in children. Surg Endosc 16:1666–1668
Rothenberg S (1998) Experience with 220 consecutive laparoscopic Nissen fundoplications in infants and children. J Pediatr Surg 33:274–278
Pearl RH, Robi DK, Ein SH, Shandling B, Wesson DE, Superina R, Mctaggart K, Garcia VF, O’Connor JA, Filler RM (1990) Complications of gastroesophagal antireflux surgery in neurologically impaired versus neurologically normal children. J Pediatr Surg 11:1169–1173
Graziano K, Teitelbaum DH, McLean K, Hirschl RB, Coran AG, Geiger JD (2003) Recurrence after laparoscopic and open Nissen fundoplication. Surg Endosc 17:704–707
Kawahara H, Nakajima K, Yagi M, Okuyama H, Kubota A, Okada A (2002) Mechanisms responsible for recurrent gastroesophagal reflux in neurologically impaired children who underwent laparoscopic Nissen fundoplication. Surg Endosc 16:767–771
Kawahara H, Imura K, Nakajima K, Yagi M, Kamata S, Okada A (2000) Motor function of the oesophagus and the lower oesophageal sphincter in children who undergo laparoscopic Nissen fundoplication. J Pediatr Surg 35:1666–1671
Pimpalwar A, Najmaldin A (2002) Results of laparoscopic antireflux procedures in neurological impaired children. Semin Laparosc Surg 9:190–196
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathei, J., Coosemans, W., Nafteux, P. et al. Laparoscopic Nissen fundoplication in infants and children: analysis of 106 consecutive patients with special emphasis in neurologically impaired vs. neurologically normal patients. Surg Endosc 22, 1054–1059 (2008). https://doi.org/10.1007/s00464-007-9578-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9578-0