Abstract
Background
Laparoscopic ventral hernia repair (LVHR) for morbidly obese patients with a body mass index (BMI) exceeding 35 kg/m2 has not been well investigated.
Methods
Hernia recurrence was evaluated by surveillance computed tomography. A p value less than 0.05 was considered significant.
Results
Between 2003 and 2006, LVHR was attempted for 27 patients with a BMI exceeding 35 kg/m2. There was one conversion to open surgery (3.7%). The 27 patients included 8 men (29.6%) and 19 women (70.4%) with a mean age of 48 years (range, 33–73 years). The mean BMI was 46.9 kg/m2 (range, 35–70 kg/m2). Nine patients (33%) were superobese (BMI > 50 kg/m2), and five patients (22.7%) underwent emergency LVHR because of small bowel obstruction. Concomitant LVHR with laparoscopic gastric bypass (LGB) was performed for 13 patients (48%). Primary, incisional, or recurrent incisional ventral hernia was present in 7 (26%), 15 (55%), and 5 (19%) patients, respectively. A large hernia (>50 cm2) was found in 20 patients (74%). The mesh used was porcine submucosal small intestine extracellular matrix for 15 patients (57%), Gore-Tex for 9 patients (35%), and Composix for 2 patients (8%). The mean hernia size was 158 cm2 (range, 12–806 cm2), and the mean mesh size was 374 cm2 (range, 117–2,400 cm2). The mean operative time was 190 min (range, 80–480 min), and the mean hospital length of stay (LOS) was 3.6 days (range, 1–11 days). Minor or major complications occurred in seven patients (25.9%), and five patients (18.5%) experienced recurrence during a mean follow-up period of 14.9 months (range, 3–32 months). Emergency setting, BMI, concomitant LGB, hernia type, hernia size, and mesh type had no statistically significant effect on operative time, LOS, morbidity, or recurrence rates.
Conclusions
For morbidly obese patients, LVHR is safe and effective, but it is associated with higher likelihood of recurrence, and patients should be appropriately informed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Incisional and primary ventral hernias represent a frequently encountered and sometimes frustrating problem for the general surgeon. Open repair of these hernias can be very challenging, with significant associated morbidity (20–40%) [1, 7]. Furthermore, depending on whether a simple suture or prosthetic repair is used, open ventral hernia repair is associated, with 46% and 23% recurrence rates respectively [4].
Laparoscopic ventral hernia repair (LVHR) has infused the field with new interest and enthusiasm. Despite the increasing popularity of LVHR among patients and surgeons together with markedly reduced rates of morbidity (to 20%) and recurrence (to 5%) [6, 9], its outcome for morbidly obese patients with a body mass index (BMI) greater than 35 kg/m2 has not been well investigated.
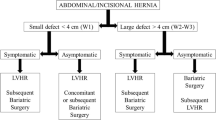
Because bariatric surgery has been established as the standard of care for the treatment of morbid obesity, morbidly obese patients with ventral hernias who present for laparoscopic gastric bypass (LGB) pose a quite frequent therapeutic dilemma. Previous findings have shown that these hernias should be repaired using mesh concomitant with LGB. Deferment of repair, or simple suture repair often results in recurrence and postoperative small bowel obstruction [5]. The management however, of specific challenging clinical scenarios regarding 1) the type of ventral hernia (primary, incisional, recurrent), 2) the hernia size, 3) the BMI, 4) the clinical setting (elective, or emergency repair), 5) the concomitant bariatric surgery (LVHR alone, or combined with LGB) and 6) the type of mesh, in morbidly obese patients with ventral hernias and their effect on morbidity and recurrence rates has not been well investigated.
Materials and methods
Patient characteristics and selection criteria
This retrospective study included morbidly obese patients with a BMI exceeding 35 kg/m2 who underwent LVHR between 2003 and 2006. Hernias that occurred in an area without a previous surgical incision were considered primary hernias. Those occurring in an area with a previous surgical incision were considered incisional hernias, and those occurring in an area with a previous surgical incision and at least one previous failed surgical repair were considered recurrent incisional hernias.
Hernias were considered small (<50 cm2) or large (>50 cm2). Similarly, according to their BMI, the patients were classified as morbidly obese (35–50 kg/m2) or superobese (>50 kg/m2). Hernia recurrence was evaluated by clinical examination every 3 months, and by surveillance computed tomography (CT) scan at 3 months, then annually thereafter. No patient was lost to follow-up evaluation. Morbidly obese patients with a ventral hernia undergoing LGB received a concomitant LVHR.
Operative technique
Laparoscopic access to the abdominal cavity was gained by the use of a Veress needle or open blunt technique (Hasson type). Two or three additional 5-mm ports were placed as laterally as possible. The port placement did not change when the hernia repair was performed in conjunction with the gastric bypass. We normally used seven ports (two 12-mm and five 5-mm ports) for the gastric bypass, and these usually sufficed for the hernia repair as well. In the majority of cases, a 30° or 45° laparoscope was used.
Adhesiolysis was performed using Ultrashears (USSC, Norwalk, CT, USA). An appropriately sized mesh was placed intraperitoneally, extending at least 4 cm beyond the edges of the defect. The Surgisis Gold mesh (Cook Biotech Incorporated, West Lafayette, IN, USA) was most frequently used (57%), followed by the Gore-Tex dual plus mesh (W.L. Gore & Assoc, Flagstaff, AZ, USA) (35%) and Composix mesh (C.R. Bard, Inc, Cranston, RI, USA) used for 8% of the patients. The Surgisis Gold mesh was used for patients who had LVHR in an emergency setting or combined with LGB.
Patients with very large defects required two pieces of mesh sewn together. The mesh was secured with a minimum of four nonabsorbable sutures placed no more than 5 cm apart before intraperitoneal introduction. These sutures then were anchored transmurally with the aid of a percutaneous suture passer (reusable Carter-Thomason; Inlet Medical Inc, Eden Prairie, MN, USA). Circumferential fixation of the mesh was completed with tacks (5-mm tacking device; Autosuture/USSC, Norwalk, CT, USA) placed approximately 1.5 cm apart. All port sites larger than 5 mm were closed with sutures under laparoscopic visualization using the Carter-Thomason suture passer.
Statistical analysis
Statistical analysis of categorical data was performed using the chi-square test. A p value of 0.05 or less was considered significant.
Results
This study enrolled 27 patients with a BMI exceeding 35 kg/m2. The 27 patients included 8 men (29.6%) and 19 women (70.4%) with a mean age of 48 years (range, 33–73 years). The mean BMI was 46.9 kg/m2 (range, 35–70 kg/m2). The mean hernia size was 158 cm2 (range, 12–806 cm2), and the mean mesh size was 374 cm2 (range, 117–2,400 cm2). The mean mesh–defect ratio was 2.4:1. Table 1 summarizes the patient groups stratified by BMI, setting, procedure, type of hernia, hernia size, and type of mesh.
The mean operative time was 190 min (range, 80–480 min), and the mean hospital length of stay (LOS) was 3.6 days (range, 1–11 days). One patient (3.7%, 1/27) underwent conversion to an open incisional hernia repair because of a recognized bladder injury resulting from inadvertent incorporation of the bladder into the previous abdominal wall closure. Of the 27 patients (25.9%), 7 experienced minor or major complications. There we no mortalities (Table 2). The 30-day readmission rate was 11.1% (n = 3), and the reoperation rate was 7.4% (n = 2).
During a mean follow-up period of 14.9 months (range, 3–32 months), there were five recurrences (18.5%), all of which occurred among the first 16 patients in our series. The recurrences were attributable to inadequate overlap (n = 1), use of tacks alone without anchoring sutures (n = 2), use of too few sutures in relation to mesh size (n = 1), and use of absorbable sutures to sew two pieces of mesh together (n = 1). Four of five recurrences were asymptomatic, two of them not detected by clinical examination, but only on surveillance CT scan.
Although certain trends were noted, stratification by BMI, clinical setting, procedure, type of hernia, hernia size, and type of mesh showed no statistically significant effect on operative time (Fig. 1), LOS (Fig. 2), morbidity (Fig. 3), or recurrence rates (Fig. 4).
Discussion
Proved to be a safe and effective approach to the abdominal wall hernia, LVHR has become the standard of care [6]. As a result of this remarkable success, the indications for LVHR have been constantly revised and further expanded in the past few years to include the most challenging and complex surgical patients, who once represented contraindications to the laparoscopic approach. The use of LVHR for morbidly obese individuals with large recurrent incisional hernias or small bowel obstruction at presentation and the use of LVHR in combination with LGB certainly qualify as some of those challenging and complex scenarios for the use of LVHR.
Obesity is a known risk factor for the development of ventral hernias, and it has traditionally been considered a relative contraindication to laparoscopy [11]. The validity of this view has been questioned recently by new evidence demonstrating the efficacy and safety of LVHR for obese patients [2, 3, 5, 8, 10]. However, because most new evidence comes from small studies primarily consisting of patients with a BMI of 30 to 35 kg/m2, with morbidly obese patients representing only a small fraction (20–30%), definitive conclusions cannot be drawn [2, 3, 5, 10].
In addition, certain controversies still exist. Although we have shown previously that the outcomes of LVHR are comparable for obese and nonobese individuals [10], others have reported higher morbidity and recurrence rates for morbidly obese patients undergoing LVHR [6]. Furthermore the existing experience with concomitant LVHR and LGB and the use of biomaterials for the morbidly obese population have been both positive [5] and negative [8]. Finally, certain questions such as the feasibility, safety, and durability of LVHR for morbidly obese patients with recurrent incisional ventral hernias or incarcerated hernias with obstructive symptoms have not been addressed.
On the basis of our results, the mean operative time of 190 min and the LOS of 3.6 days observed in this study were slightly higher than reported in the existing literature (Table 3). This is likely related to the characteristics of our patient population (Table 1). A significant percentage of our patients had a BMI greater than 50 kg/m2 (33%) as well as large (74%), incisional (55%) or recurrent (19%) hernias. Our results show that all these characteristics were associated with a longer operative time (Fig. 1), and that large hernia size also was associated with longer LOS (Fig. 2). In accordance with our findings, Heniford et al. [6] also reported a longer operative time after LVHR for patients with a BMI exceeding 35 kg/m2 and recurrent incisional ventral hernias. In addition, 48% of our patients had a concomitant LGB, and 19% presented with small bowel obstruction, both of which were associated with a longer LOS (Fig. 2). Surprisingly, concomitant LGB or emergency surgery did not increase the operative time for LVHR (Fig. 1).
For morbidly obese patients, LVHR has been associated with increased morbidity (18.5% for BMI > 35 kg/m2 vs 11.6% for BMI < 35 kg/m2) [6] and a greater incidence of mesh infection [3]. In our study, the rates were 14.8% for minor and 11.1% for major morbidity. The morbidity rate was greater for patients with large hernias. In agreement with previous observations [6], the LVHR morbidity rate was higher for patients with recurrent incisional ventral hernias. According to our results, superobesity, an emergency setting, and concomitant LGB did not increase the morbidity (Fig. 3), suggesting that in experienced hands, LVHR is safe and should be considered even in such extreme and complex situations.
Although Heniford et al. [6] also reported an increased likelihood of recurrence (7.8% vs 2%) for morbidly obese patients undergoing LVHR, the 18.5% recurrence rate observed in this study is considered high and may reflect the complexity of our population. On the basis of our results, morbidly obese patients undergoing LVHR in an emergency setting are more likely to experience a recurrence (40%, 2/5 vs 14.3%, 3/21). It is possible that inclusion of such patients also may have contributed to the high recurrence rate observed in this study.
Interestingly, in contrast to what is believed [8] the use of biomaterial in this study was not associated with a higher recurrence rate. Although morbid obesity and recurrent incisional ventral hernias have been associated, respectively, with four- and sixfold increases in recurrence rates [6, 8], our results showed that superobesity and recurrent incisional hernias were associated with only a small increase in recurrence rates, as compared with morbidly obesity (22.2% vs 16.7%, respectively) and primary ventral hernias (20% vs 14.3%, respectively). Ideally, those defects should be repaired after maximum weight loss is accomplished.
Unfortunately, we and others have found that deferring the hernia repair until later or repairing the hernia primarily with sutures has been associated with an increased incidence of early postoperative small bowel obstruction [5]. In fact, two of the patients in this study (one with a BMI of 70 kg/m2) who presented with intestinal obstruction had undergone laparoscopic Roux-en-Y gastric bypass the day before. The incarcerated umbilical hernia in the one case and the incisional ventral hernia in the other case were not repaired in conjunction with the gastric bypass. Further review of our results also demonstrates that all five recurrences were attributable to technical errors, and thus could have been prevented by the following recommendations:
-
1.
Nonabsorbable suture should be used to sew meshes together. A male patient with a weight of 152 kg had a large (450 cm2) recurrent incisional hernia in the area where the two 20 × 30-cm meshes were sewn together with absorbable suture.
-
2.
A minimum of 4-cm overlap is necessary to prevent recurrence. One patient in our study presented with a small bowel obstruction that recurred as a result of only a 2-cm overlap at one side of the hernia.
-
3.
A combination of nonabsorbable sutures and tacks should be used for mesh fixation because one recurrence occurred due to the use of tacks only.
-
4.
The number of sutures for mesh fixation should depend primarily on the mesh size and not on the hernia size. In addition to the four anchoring sutures at each side of the mesh, additional sutures should be placed every 4 to 6 cm when large size meshes are used. Only four anchoring sutures were used in two of our patients with large recurrent incisional hernias.
It is very likely that because of these improvements in our technique, no recurrences were observed in the last 11 morbidly obese patients who underwent LVHR during a period of 14 months.
This study had several weaknesses that need to be acknowledged. This was a small case series without a nonobese control group. Therefore, definitive conclusions cannot be drawn. In addition, the number of patients included in each subgroup was small, and although certain trends in outcome parameters were observed, none was statistically significant. It is likely that a larger study may show stronger statistical associations between the compared outcome parameters. Furthermore although no patients were lost to follow-up evaluation, the mean length of the follow-up period in this study was intermediate, resulting in possible underestimation of the long-term recurrence rate.
Despite these weaknesses, some conclusions can be drawn. For superobese patients, LVHR is safe and feasible without any significant increase in operative time, LOS, or morbidity, and only a modest increase in recurrence rates. Morbidly obese patients who present with incarcerated hernias and intestinal obstruction did not experience a significant increase in operative time, LOS, or morbidity and thus may benefit from LVHR.
In contrast, recurrence appears to be clearly higher in the emergency setting, and careful adherence to proper mesh fixation despite the encountered technical challenges and often suboptimal exposure is very important to the achievement of comparable results with elective repairs. Morbidly obese patients with ventral hernias undergoing LGB should have concomitant LVHR. Our findings show a small increase in operative time, but no increase in LOS, morbidity, or recurrence.
Because morbidity and recurrence rates are higher (although not to an unacceptable extent) among morbidly obese patients with incisional or recurrent incisional ventral hernias, it is better to repair the hernias laparoscopically the first time because previous open failed repairs decrease the durability of subsequent LVHR. Despite a notable increase in morbidity, LVHR still should be considered for morbidly obese patients with large hernias because LOS and recurrence remained comparable with those for patients with smaller defects. The use of absorbable biomaterials should be considered when concerns for possible contamination or infection exist because recurrence was not increased in the current study when such mesh was used.
In addition, routine postoperative surveillance with abdominal CT scan is recommended because many of these recurrences are asymptomatic and difficult to diagnose clinically due to the patients’ body habitus, and if left unrecognized may result in intestinal obstruction.
In conclusion, LVHR is safe and effective for morbidly obese patients, but it is associated with higher likelihood of recurrence, and patients should be appropriately informed. With increasing experience and refinements in technique, expected recurrence rates should be lower than those currently reported.
References
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24:95–101
Birgisson G, Park AE, Mastrangelo Jr MJ, Witzke DB, Chu UB (2001) Obesity and laparoscopic repair of ventral hernias. Surg Endosc 15:1419–1422
Bower CE, Reade CC, Kirby LW, Roth JS (2004) Complications of laparoscopic incisional ventral hernia repair: the experience of a single institution. Surg Endosc 18:672–675
Costanza MJ, Heniford BT, Arca MJ, Gagner M (1998) Laparoscopic repair of recurrent ventral hernias. Am Surg 64:1121–1127
Eid GM, Mattar SG, Hamad G, Cottam DR, Lord JL, Watson A, Dallal RM, Schauer PR (2004) Repair of ventral hernias in morbidly obese patients undergoing gastric bypass should not be deferred. Surg Endosc 18:207–210
Henniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic of ventral hernias: nine years’ experience of 850 cases. Ann Surg 238:391–400
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378–382
Novitsky YW, Cobb WS, Kercher KW, Mathews BD, Sing RF, Heniford TB (2006) Laparoscopic ventral hernia repair in obese patients. Arch Surg 141:57–61
Raftopoulos I, Vanuno D, Khorsand J, Kouraklis G, Lasky P (2003) Comparison of open and laparoscopic prosthetic repair of large ventral hernias. JSLS 7:227–232
Raftopoulos I, Vanuno D, Khorsand J, Ninos J, Kouraklis G, Lasky P (2002) Outcome of laparoscopic ventral hernia repair in correlation with obesity, type of hernia, and hernia size. J Laparoendosc Adv Surg Tech A 12:425–429
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid dependent patients and low recurrence with prefascial polypropelene mesh. Am J Surg 171:80–84
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the 10th World Congress of Endoscopic Surgery Meeting, Berlin, Germany, September 2006
Rights and permissions
About this article
Cite this article
Raftopoulos, I., Courcoulas, A.P. Outcome of laparoscopic ventral hernia repair in morbidly obese patients with a body mass index exceeding 35 kg/m2 . Surg Endosc 21, 2293–2297 (2007). https://doi.org/10.1007/s00464-007-9406-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9406-6