Abstract
Background
Laparoscopic resections of parenchymal organs are increasingly performed. However, little is known about the effects of laparoscopic fibrin sealant spray applications on intraabdominal pressure (IAP) and hemodynamics.
Methods
Cardiac and pulmonary monitoring was performed via two central venous pressure lines in the thoracic and abdominal vena cava, a pulmonary artery catheter, and a peripheral artery line. Air was sprayed into the abdomen at pressures of 2, 3, and 4 bar for 30 s. According to the group, a valve on a trocar was open or closed. To optimize fibrin sealant application, the sealant was sprayed at three different application pressures (2, 2.5, and 3 bar) and distances (2, 3.5, and 5 cm).
Results
All spray simulations caused a significant increase in the IAP. During the first 10 s of spraying, the IAP increase was 5 mmHg or less, but rose rapidly during the last 20 s of spraying. The IAP increase resulted in decreased pulmonary compliance. Pulmonary resistance and the central venous pressures of both the thoracic and abdominal vena cava increased. At application pressures of 3 and 4 bar, the IAP increase was greater than 2 bar of pressure, reaching IAP values exceeding 35 mmHg. Spray mist formation was primarily dependent on application pressure, whereas clot formation and surface coverage depended on both application pressure and distance. The best results were achieved with an application pressure of 2.5 bar and a distance of 5 cm from the surface.
Conclusions
This study shows that fibrin sealants can be used safely in laparoscopic procedures. Keeping the spray periods short and allowing air to escape from the abdomen can minimize the IAP increase. According to our results, a laparoscopic spray application of fibrin sealant should start with an insufflation pressure of 10 mmHg, an application pressure of 2.5 bar, and an application distance of 5 cm with a valve on the trocar left open.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic resections of parenchymal organs are increasingly performed, favored by surgeons for reducing postoperative pain, shortening hospital stay, and allowing patients to return more quickly to their activities. Complication and morbidity rates are equal to those for open surgery [1–5].
One challenge facing the surgeon during both laparoscopic and conventional organ resections is the control of bleeding. A variety of methods have been developed to help the surgeon stop bleeding. Together with techniques such as vascular stapling, mono- and bipolar coagulation, ultrasonic devices, argon beamers, and different topic agents, fibrin sealants are used frequently [1, 3, 6–11].
In conventional surgery, fibrin sealants are more effective if sprayed rather than dripped onto the resection surface. In laparoscopy, however, spraying the fibrin sealant may cause the IAP to rise because the spraying takes place in a closed abdomen and there is little possibility for air to escape. An increase in the intraperitoneal pressure may be detrimental to hemodynamic parameters such as mean arterial pressure, arterial carbon dioxide (CO2) concentration, respiratory resistance, and compliance, posing a potential danger to the patient [12–14].
We systematically analyzed the influence of intraperitoneal spray application on intraabdominal pressure (IAP) and its relevance for cardiopulmonary measurements. We also aimed to optimize the results of the spray application through varying of the application pressure and the distance to the target surface.
Materials and methods
Animals and anesthesia
Female German Landrace pigs (n = 5) weighing 56 to 62 kg were housed in the animal resource facilities at the Center for Experimental Medicine (Medizinisch Experimentelles Zentrum, Universität Leipzig, Germany) with the approval of the Institutional Animal Use Committee (Regierungspräsidium Leipzig, Germany). The animals were handled in accordance with the standards for the care and use of laboratory animals.
All the animals were deprived of food 24 h before surgery, but were allowed free access to water. General anesthesia was induced with an intramuscular injection of ketamine (7.5 mg/kg body weight [BW]), azaperon (15 mg/kg BW), and atropine (0.02 mg/kg BW) followed by intravenous etomidate (0.3 mg/kg BW) and ketamine (0.3 mg/kg BW). The animals were placed on heating blankets to maintain body temperature. They were intubated and mechanically ventilated (Julian, Dräger, Lübeck, Germany) with a positive end-expiratory pressure of 5 cm H2O at a tidal volume of 10 ml/kg or more. Anesthesia was maintained with isoflurane (1–2.5% in 50% oxygen [O2]) and continuous fentanyl injection (0.25 mg/h). Cis-atracurium was used to induce (0.15 mg/kg BW) and maintain (0.03 mg/kg BW) muscular relaxation. The respiratory rate was adjusted to achieve an end-tidal CO2 of 35 to 40 mmHg. Minute volume was adjusted by the anesthesiologist throughout the operation to maintain end-tidal CO2 below 55 mmHg.
Once anesthesia was induced, 500 ml of crystalloid solution (Deltasect GmbH, Pfullingen, Germany) and 250 ml of 10% hydroxyethyl starch (Fresinus Kabi, Bad Homburg, Germany) were given as a short infusion. Thereafter, the crystalloid solution was given at a rate of 3 ml/h/kg BW.
A 1.1-mm intravascular catheter (Becton Dickinson, Singapore) was inserted into the right carotid artery after surgical exposure. A 7.5-Fr, 110-cm Swan-Ganz catheter (Edwards Lifesciences, Irvine, CA, USA) was inserted into the pulmonary artery via the internal jugular vein, and its position was verified by characteristic pulmonary arterial tracings. Finally, an 8.5-Fr central venous catheter (Becton Dickinson) was introduced into the inferior vena cava via a branch of the femoral vein.
Arterial and venous pressures were monitored using pressure transducers (Smiths Medical International Ltd, Kent, UK) and a monitor terminal (Hewlett Packard, Palo Alto, California, USA).
All transducers were placed at the level of the right atrium and zeroed. Pressures all were recorded with the pig in the supine position. Cardiac output was measured by thermodilution. A blood gas analyzer (Radilab 248; Chirion Diagnostics, Essex, Great Britain) was used for arterial and mixed venous blood gas measurements.
Experimental design
After all monitoring lines had been connected, there were no manipulations during a 15-min preoperative period to establish baseline conditions. Then preoperative control values were recorded and blood samples were drawn.
Part 1: Measuring IAP after 30 s of dynamic spray simulation
After baseline measurements, a pneumoperitoneum with an IAP of 10 mmHg was induced, followed by placement of two 5-mm trocars and one 10-mm trocar. The insufflator (Laparo CO2-Pneu 2232; Richard Wolf GmbH, Knittlingen, Germany) maintaining the pneumoperitoneum has two built-in safety features. If the IAP exceeds the adjusted value by more than 5 mmHg, it starts to aspire gas. Should the IAP continue rising to levels of 35 mmHg or higher, the insufflator turns itself off.
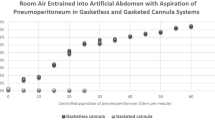
To facilitate handling, the catheter of the application device (Medimop Medical Projects Ltd., Ra’anana, Israel) was introduced into the trocar through a 5-mm steel tube. All experiments were performed twice, first with a valve on a trocar left open, allowing air to escape from the abdomen, and second, with all valves closed to prevent air leakage.
When the catheter of the application device had been introduced into the peritoneal cavity, the IAP, the central venous pressure (CVP) in the thorax (superior vena cava) and abdomen (inferior vena cava), pulmonary compliance, and airway resistance were recorded. Air then was sprayed for 30 s to simulate the spray application of a fibrin sealant, and IAP and CVPs were recorded. If the insufflator turned itself off before 30 s, this time was recorded. The animal was allowed a 5-min interval between spray simulations to recover. The experiment was conducted with application pressures of 2, 3, or 4 bar. Finally, the procedure was repeated with IAP increased from 10 to 15 mmHg (Fig. 1).
Part 2: Cardiac and pulmonary effects from 10 min of constantly elevated insufflation pressures
After part 1 of the procedure was completed, the peritoneum was desufflated. Hemodynamic values then were recorded and blood samples taken. For the next 30 min, no manipulations were performed, allowing the animal to recover. Immediately after the recovery period, measurements were completed and blood samples were drawn.
The experiment involved alternating intervals of pneumoperitoneum and desufflation. Each 10-min interval at an IAP of 10, 15, 20, or 25 mmHg was followed by a 15-min period with a desufflated peritoneum. Hemodynamic measurements were performed, and blood gas samples were drawn at the end of each interval (Fig. 2).
Part 3: Evaluation of application pressures and distances
Quixil (Omrix Biopharmaceuticals S.A., Rhode-St-Genèse, Belgium), a two-component liquid fibrin sealant, was used in the experiments. To improve visibility, a green food color (Schwartauer Werke, Bad Schwartau, Germany) was added to the fibrin sealant. The fibrin sealant was sprayed at a distance of 2, 3.5, or 5 cm from the application surface, with the distance being measured using a ruler placed intraabdominally. For each distance, the application pressure was set at 2, 2.5, or 3 bar. During each experiment, the IAP was set at 10 or 15 mmHg according to the group. After sealant had been sprayed, the camera was focused on the fibrin clot, and two surgeons assessed the results independently and semiquantitatively in terms of surface coverage, sealant distribution, and formation of spray mist.
Results
Part 1: Effects from 30 s of dynamic spray simulation
Intraabdominal pressure
In all five pigs, the simulation of an intraabdominal fibrin sealant application made the IAP rise. At an IAP of 10 mmHg and with an open valve, the mean IAP change with an application pressure of 3 bar was 47% higher than with an application pressure of 2 bar (31.8 ± 1.7 vs 16.8 ± 2.8 mmHg; p < 0.001). This change also was observed at other application pressures with the valve closed (Tables 1 and 2).
The IAP rose by no more than 5 mmHg during the first 10 s of spraying, but rose rapidly during the last 20 s. At application pressures of 2 bar with a closed valve and 3 and 4 bar with an open or closed valve, the pressure limit (IAP ≥ 35 mmHg) of the insufflator was reached before the 30-s spray period was completed. With the valve closed, the IAP changes were greater and the pressure limit of the insufflator was reached sooner. At 4 bar, the pressure limit of the insufflator was reached in less than 10 s, before measurements could be completed. With the insufflation set at 15 mmHg and with spraying performed at 2 bar, the IAP reached higher maximum values than at an insufflation pressure of 10 mmHg. At higher application pressures (3 and 4 bar), the insufflation pressure made very little difference (Tables 1 and 2). Because the pressure limit was consistently reached in less 10 s at 3 bar with a closed valve, experiments at 4 bar with a closed valve were omitted (Table 2).
Intrathoracic venous pressure
Valve open
Increased IAP induced a CVP rise in the upper vena cava. At an application pressure of 2 bar, the CVP rose by 15% after spray simulation (8.3 ± 1.4 vs 9.5 ± 2.5 mmHg). These pressure changes were not significant. At application pressures of 3 and 4 bar, the CVP increases were 20% (p < 0.05) and 18%, respectively (Table 3 and Fig. 3).
Valve closed
With the valve closed, the increase in CVP at an application pressure of 2 bar was 15% (8.5 ± 1.3 vs 9.8 ± 2.3 mmHg; p < 0.05) At 3 bar, there was a 5% increase (7 ± 1 vs 7.3 ± 1.5 mmHg) (Table 4). At this pressure, not all measurements could be completed because of the rapid IAP increase (Table 2).
Intraabdominal venous pressure
Valve open
The CVP of the inferior vena cava rose with increasing IAP. At an application pressure of 2 bar, there was a 28% increase in CVP (14.1 ± 3.1 vs 18 ± 2.9 mmHg; p < 0.05). When spraying was simulated at a pressure of 3 bar, CVP increased by 44% (13 ± 2 vs 18.7 ± 3.2 mmHg; p < 0.05). With a pressure of 4 bar, a 35% increase in CVP (13 ± 2.1 vs 17.5 ± 1.9 mmHg; p < 0.05) was measured during spray simulation (Table 3 and Fig. 4).
Valve closed
With the valve closed, the 2-bar spray simulation caused a 67% increase (12.8 ± 2.6 vs 21.4 ± 7.6 mmHg; p < 0.05) in the CVP of the inferior vena cava. A pressure of 3 bar caused a 95% increase (12.7 ± 3.8 vas 24.7 ± 10 mmHg) (Table 4).
Pulmonary compliance
Valve open
There was a decrease in compliance after spray simulation. At an application pressure of 2 bar, compliance decreased by 23% (32.2 ± 5.4 vs 24.9 ± 3.8 ml/mbar; p < 0.05). Spraying with a pressure of 3 bar caused a 32% decrease (29.8 ± 3.8 vs 20.3 ± 2 ml/mbar; p < 0.05). Spraying at a pressure of 4 bar caused a 33% decrease in compliance (31.1 ± 4.4 v 20.8 ± 2.8 ml/mbar; p < 0.05).
Valve closed
When the valve was closed, the compliance decrease was 32% (30.2 ± 4 vs 20.6 ± 2.2 ml/mbar; p < 0.05) at an application pressure of 2 bar. At a pressure of 3 bar, there was a 31% decrease in compliance (35.3 ± 0.1 vs 24.3 ± 5.3 ml/mbar).
Peak airway resistance
Valve open
The increase in IAP after spray simulation caused the peak airway resistance to rise. At an application pressure of 2 bar, the peak airway resistance increased by 16% (23 ± 2.2 vs 26.7 ± 4 mmHg; p < 0.05). A 26% increase (24.6 ± 1.7 vs 31 ± 3.6 mmHg; p < 0.05) was measured after spray simulations with a pressure of 3 bar. Spraying with a pressure of 4 bar caused a 59% increase in the peak airway resistance (23 ± 2.3 vs 36.5 ± 3.3 mmHg; p < 0.05).
Valve closed
At an application pressure of 2 bar with the valve closed, there was a 30% increase (23.6 ± 2.6 vs 30.6 ± 4 mmHg; p < 0.05) in peak airway resistance. The peak airway resistance increased 40% (21 ± 0 vs 35 ± 0 mmHg).
Part 2: Effects from 10 min of constantly elevated IAP
Partial arterial CO2
Partial arterial CO2 (paCO2) pressure increased with increasing IAP in all the pigs. The average paCO2 correlated with the rising IAP (r = 0.95). Arterial CO2 returned to near baseline values (45.4 ± 3.4 vs 42.9 ± 2.3 mmHg) 15 min after peritoneum desufflation (Fig. 5).
Arterial pH
With increasing IAP, pH decreased in all the pigs. The pH changes correlated with the IAP changes (r = –0.96). The arterial pH returned to near baseline values after 15 min of peritoneum desufflation (7.461 ± 0.025 vs 7.484 ± 0.016) (Fig. 5).
Pulmonary compliance
Pulmonary compliance decreased as insufflation pressures increased. The graph of the averages showed a correlation (r = –0.99). After 15 min without pneumoperitoneum, the average compliance returned to near baseline values (42.8 ± 3.3 vs 43.8 ± 3.1 ml/mbar) (Fig. 5).
Airway peak and plateau resistance
Airway peak resistance and plateau resistance both increased, correlating with rising intraperitoneal pressures (r = 0.99), whereas the resistances returned almost to normal after 15 min of peritoneum desufflation (20.6 ± 1.7 v 18.7 ± 0.6 and 18.7 ± 1.2 v 16.7 ± 0.6 mmHg) (Fig. 5).
Intrathoracic and intraabdominal venous pressures
Intraabdominal pressure correlated with increasing central venous pressures of the upper vena cava or the inferior vena cava at r values of 0.89 and 0.99, respectively. At release of the pneumoperitoneum, the pressures returned to near baseline values (6.8 ± 1.7 vs 6.7 ± 1.2 and 6.3 ± 1.4 v 7 ± 1 mmHg, respectively) (Fig. 5).
Cardiac output
At an IAP of 10 mmHg, the cardiac output increased compared with baseline values (5.2 ± 0.2 vs 6.6 ± 0.9 l/min). With increasing insufflation pressures, the cardiac output changed by an average of 0.35 l/min. These changes were not significant.
Arterial mean pressure
The IAP increase had no significant influence on the mean arterial pressure (average increase, 10.4 mmHg).
Pulmonary mean arterial pressure
The average change in pulmonary mean arterial pressure from the baseline value (15 mmHg) was 1.3 mmHg as the IAP increased. The changes were not significant.
Pulmonary arterial wedge pressure
Compared with baseline values, the pulmonary arterial wedge pressure increased by an average of 2.5 mmHg when the insufflation pressure was raised, but the increase was not significant.
Cardiac frequency
At an insufflation pressure of 10 mmHg, the cardiac frequency increased by a mean of 9 beats/min. Insufflation pressures of 15, 20, and 25 mmHg led to an average decrease of 8 beats/min without reaching statistical significance.
Part 3: Evaluation of application pressures and distances
The formation of spray mist and the clotting of the fibrin sealant were dependent on the application pressure and distance from the target (Table 5). Spray mist formation was dependent primarily on the spray pressure, whereas clot formation and surface coverage depended on both application pressure and distance.
Distance of 2 cm
At close distances, the sealant was sprayed mainly toward the edge of the clot, forming a ring approximately 4 cm in diameter and leaving little fibrin sealant in the center of the application surface.
Distance of 3.5 cm
When the distance was increased, the diameter of the clot also increased to an average of 5 cm. More of the fibrin sealant still was deposited at the edge of the clot than in the center.
Distance of 5 cm
After the spray distance was increased to 5 cm, the diameter of the clot was approximately 6.5 cm. The fibrin sealant was distributed equally in the center and on the edge of the clot (Fig. 6).
Pressure of 2 bar
When the sealant was sprayed at 2 bar, not all the sealant was delivered to the surface, but some dripped from the tip of the catheter. There was only a narrow spread of the sealant spray mist.
Pressure of 2.5 bar
This medium pressure caused no sealant dripping from the tip of the catheter. The spread of the mist was wider than with a pressure of 2 bar, and the mist consisted of fine sealant drops.
Pressure of 3 bar
Higher application pressures produced a fine mist without any sealant dripping from the tip of the catheter. The spread of the sealant was wider than at 2.5 bar. Spraying with a pressure of 3 bar deposited more fibrin sealant at the edge than in the center of the fibrin clot.
Discussion
Fibrin sealants have been shown to provide effective hemostasis after resections of parenchymal organs [15–17]. Despite the wide use of fibrin sealants, little is known about the effects of spray application in a closed abdomen (e.g., during laparoscopy). This study investigated the effects of spray application on the IAP and sought to determine both the optimal application pressure and the ideal application distance for spraying the fibrin sealant.
Because human and porcine physiology are similar, the use of pigs in experimental models is frequent and widely accepted [18–22]. We chose pigs with a mean weight of 60 kg so that instruments equivalent to those used during human laparoscopic procedures could be used.
Effect of spray application on intraabdominal pressure
During the laparoscopic spray application, there was a rapid rise in intraperitoneal pressure. This rise was attributable to the high application pressure of 1,500 to 3,000 mmHg (2–4 bar). When the sealant was sprayed with a pressure of 4 bar, the IAP exceeded the 35 mmHg limit every time, reaching a mean IAP of 36.7 ± 2.1 mmHg after only 24 ± 1 s. Because of the rapid increase in IAP when spraying is performed with a pressure of 4 bar, we omitted the spray simulations at 4 bar with the valves closed (Table 2). The results suggest that application pressures greater than 3 bar should not be used. When the valve was left open, allowing air to escape, the increase in IAP was not as great as when the valve was closed and the increase in pressure was slower. We conclude that the IAP increase can be slowed down when air is allowed to escape through an open valve on the trocar, as described by Bishoff et al. [23].
Patients tolerate laparoscopic procedures well when the IAP is set at 12 mmHg or less [13, 24]. To ensure a minimal IAP increase, the spraying period should not exceed 10 s. The experiments showed that the IAP increase during the first 10 s was not greater than 5 mmHg. Insufflation of the pneumoperitoneum with pressures of 10 mmHg or less will help to reduce the effects of spray application because the maximum IAP is dependent on the initial insufflation pressure.
Effects of CO2 pneumoperitoneum
Peritoneal insufflation of CO2 is a common way of creating a pneumoperitoneum. The elevated IAP compresses the vessels of the abdomen and simultaneously increases the intraabdominal and subcutaneous absorption of CO2 [25]. As a result, the pressure of the inferior vena cava increases, and venous return from the lower body parts decreases. An increase in arterial CO2 load causes a reduction in arterial pH. Elevated IAP exerts a direct influence on respiratory function by reducing excursions of the diaphragm, leading to elevated intrapleural and intrathoracic pressures. Elevated pressures lead to reduced compliance, with increased airway and central venous pressures, diminishing venous return to the heart.
The study indicated that the venous pressure in the abdominal vena cava reached higher values than in the thoracic vena cava (at 25 mmHg insufflation pressure, 27.7 ± 1.5 vs 9.5 ± 2.1 mmHg). This is likely attributable to the greater compression of the abdominal vena cava as a result of the gas insufflation. The experiments showed a high degree of correlation (r = 0.99) between insufflation pressure and abdominal venous pressure. Therefore, the abdominal venous pressure provides a good measure of the IAP. The described changes also have been detected where gases such as helium and air were used to create the pneumoperitoneum, indicating that the changes depend on the insufflation pressure rather than the physiologic effects of the gas used [19].
The cardiac and pulmonary changes seen after 10 min of pneumoperitoneum with insufflation pressures of 10, 15, 20, and 25 mmHg all returned to near baseline values after 15 min with desufflation of the pneumoperitoneum. Healthy animals appear to tolerate and compensate well for elevated intraperitoneal pressures, recovering rapidly.
Several studies have investigated the effects of elevated intraperitoneal pressures on human physiology [12–14, 26, 27]. It was concluded that for patients in American Society of Anesthesiologists (ASA) categories 1 and 2, the hemodynamic effects of a pneumoperitoneum are not clinically relevant and disappear after desufflation. However, ASA 3 and 4 patients need to be monitored closely [13]. This suggests that short periods of increased IAPs, such as occur during spray application, also may be tolerated well in ASA 1 and 2 patients.
Influence of application pressure and distance on spraying efficiency
The outcome of the spray application was dependent on the application pressure and the distance from the application surface. We achieved homogeneous results when spraying at a distance of 5 cm with an application pressure of 2.5 bar. Given the nature of this experiment, the evaluation is semiquantitative because objective evaluation of spraying is hard to achieve. To improve objectivity, two surgeons assessed all spray experiments independently. The formation of spray mist, surface coverage, and sealant distribution were rated from 1 (poor) to 3 (best result) according to Table 3.
In our experiment, an intraabdominally placed ruler measured the distance from the tip of the catheter to the application surface. During laparoscopic operations in humans, no ruler is placed intraabdominally. The surgeon therefore will need to take into account that the distance as shown on the monitor may not be correct because the angle between the tip of the application device and the camera will influence the picture created.
The sealant was sprayed with application pressures varying from 2 to 3 bar (1,500–2,250 mmHg). The experiment showed that mist formation improved with higher pressures (2.5–3 bar), as compared with application of the sealant with a pressure of 2 bar. On the other hand, higher pressures caused the IAP to rise more rapidly and reach higher values (21.5 vs 31.3 mmHg).
The maximum IAP reached during spray application with the valve open and a pressure of 2 bar was higher with an insufflation pressure of 15 mmHg than with a pressure of 10 mmHg (21.5 vs 16.8 mmHg). At higher insufflation pressures, there were little influence on the maximum IAP (31.8 vs 31.3 mmHg). This indicates that the increase in IAP depends less on the insufflation pressure and more on the application pressure and whether air is allowed to escape. Insufflation pressure did not have any effect on the spray result, probably because of the great difference between application pressure and insufflation pressure, the ratio of insufflation pressure to application pressure being 1:150.
Depending on the medical condition of each patient, the surgeon will need to find the best compromise between application pressure for spraying, duration of spraying, and an insufflation pressure compatible with a tolerable increase in IAP.
This study indicates that fibrin sealants can be used safely in laparoscopic procedures. Nevertheless, and attempt should be made to minimize the IAP increase by keeping the spray periods short and allowing air to escape from the abdomen.
On the basis of our results, laparoscopic spray application of fibrin sealants should start at an insufflation pressure of 10 mmHg, an application pressure of 2.5 bar, and an application distance of 5 cm with a valve on the trocar left open.
References
Cherqui D, Husson E, Hammoud R, Malassagne B, Stephan F, Bensaid S, Rotman N, Fagniez PL (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232: 753–762
Mala T, Edwin B, Rosseland AR, Gladhaug I, Fosse E, Mathisen O (2005) Laparoscopic liver resection: experience of 53 procedures at a single center. J Hepatobiliary Pancreat Surg 12: 298–303
Edwin B, Mala T, Mathisen O, Gladhaug I, Buanes T, Lunde OC, Soreide O, Bergan A, Fosse E (2004) Laparoscopic resection of the pancreas: a feasibility study of the short-term outcome. Surg Endosc 18: 407–411
Farges O, Jagot P, Kirstetter P, Marty J, Belghiti J (2002) Prospective assessment of the safety and benefit of laparoscopic liver resections. J Hepatobiliary Pancreat Surg 9: 242–248
Cherqui D (2003) Laparoscopic liver resection. Br J Surg 90: 644–646
Schwartz M, Madariaga J, Hirose R, Shaver TR, Sher L, Chari R, Colonna JO, Heaton N, Mirza D, Adams R, Rees M, Lloyd D (2004) Comparison of a new fibrin sealant with standard topical hemostatic agents. Arch Surg 139: 1148–1154
Frilling A, Stavrou GA, Mischinger HJ, de Hemptinne B, Rokkjaer M, Klempnauer J, Thorne A, Gloor B, Beckebaum S, Ghaffar MF, Broelsch CE (2005) Effectiveness of a new carrier-bound fibrin sealant versus argon beamer as haemostatic agent during liver resection: a randomised prospective trial. Langenbecks Arch Surg 390: 114–120
Poon RT (2004) Recent advances in techniques of liver resection. Surg Technol Int 13: 71–77
Mankad PS, Codispoti M (2001) The role of fibrin sealants in hemostasis. Am J Surg 182: 21S–28S
Jackson MR (2001) Fibrin sealants in surgical practice: an overview. Am J Surg 182: 1S–7S
Nur I, Lyahovetsky Y, Bar L, Schon M (2005) Commercial fibrin sealants are not equivalent in a rabbit liver-resection model which quantitatively evaluates hemostasis and formation of adhesions. Eur Surg Res 37: 159–165
Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, Buchler MW (2004) Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg 21: 95–105
Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, Fuchs KH, Jacobi C, Jansen FW, Koivusalo AM, Lacy A, McMahon MJ, Millat B, Schwenk W (2002) The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc 16: 1121–1143
O’Malley C, Cunningham AJ (2001) Physiologic changes during laparoscopy. Anesthesiol Clin North America 19: 1–19
Katkhouda N (2004) New hemostatic agents in general open and laparoscopic surgery. Surg Technol Int 13: 65–70
Pruthi RS, Chun J, Richman M (2004) The use of a fibrin tissue sealant during laparoscopic partial nephrectomy. BJU Int 93: 813–817
Carless PA, Anthony DM, Henry DA (2002) Systematic review of the use of fibrin sealant to minimize perioperative allogeneic blood transfusion. Br J Surg 89: 695–703
Weaver ME, Pantely GA, Bristow JD, Ladley HD (1986) A quantitative study of the anatomy and distribution of coronary arteries in swine in comparison with other animals and man. Cardiovasc Res 20: 907–917
Horvath KD, Whelan RL, Lier B, Viscomi S, Barry L, Buck K, Bessler M (1998) The effects of elevated intraabdominal pressure, hypercarbia, and positioning on the hemodynamic responses to laparoscopic colectomy in pigs. Surg Endosc 12: 107–114
Greif WM, Forse RA (1999) Cardiopulmonary effects of the laparoscopic pneumoperitoneum in a porcine model of adult respiratory distress syndrome. Am J Surg 177: 216–221
Quintel M, Pelosi P, Caironi P, Meinhardt JP, Luecke T, Herrmann P, Taccone P, Rylander C, Valenza F, Carlesso E, Gattinoni L (2004) An increase of abdominal pressure increases pulmonary edema in oleic acid-induced lung injury. Am J Respir Crit Care Med 169: 534–541
Knolmayer TJ, Bowyer MW, Egan JC, Asbun HJ (1998) The effects of pneumoperitoneum on gastric blood flow and traditional hemodynamic measurements. Surg Endosc 12: 115–118
Bishoff JT, Cornum RL, Perahia B, Seay T, Eliason S, Katus M, Morey A, Gresham V, Pusateri A, Murcin LA, Tuthill D, Friedman S (2003) Laparoscopic heminephrectomy using a new fibrin sealant powder. Urology 62: 1139–1143
Ishizaki Y, Bandai Y, Shimomura K, Abe H, Ohtomo Y, Idezuki Y (1993) Safe intraabdominal pressure of carbon dioxide pneumoperitoneum during laparoscopic surgery. Surgery 114: 549–554
Sharma KC, Kabinoff G, Ducheine Y, Tierney J, Brandstetter RD (1997) Laparoscopic surgery and its potential for medical complications. Heart Lung 26: 52–64
Schmandra TC, Mierdl S, Bauer H, Gutt C, Hanisch E (2002) Transoesophageal echocardiography shows high risk of gas embolism during laparoscopic hepatic resection under carbon dioxide pneumoperitoneum. Br J Surg 89: 870–876
Nguyen NT, Wolfe BM (2005) The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg 241: 219–226
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Druckrey-Fiskaaen, K.T., Janssen, M.W.W., Omidi, L. et al. Laparoscopic spray application of fibrin sealant effects on hemodynamics and spray efficiency at various application pressures and distances. Surg Endosc 21, 1750–1759 (2007). https://doi.org/10.1007/s00464-007-9235-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9235-7