Abstract
Background
Nonrigid environments such as the human colon present unique challenges for the navigator in maintaining spatial orientation. Conventional wisdom suggests that a navigational aid, similar to a map, that provides critical shape information would be useful. This article presents a design concept for a colonoscopy navigational aid and the results of an experiment conducted to evaluate the display for supporting navigation and spatial orientation in simulated colonoscopy.
Methods
A navigational aid was designed to present shape information in an augmented reality display. A total of 14 untrained subjects performed a colonoscopy procedure in rigid and nonrigid colon models, with and without the navigational aid display, in a Latin square design. Performance measures such as time, distance or efficiency of travel, and location and direction error were recorded, together with subjective measures of confidence and workload.
Results
The results showed that, unlike navigating in rigid environments, the subjects spent more time navigating in the nonrigid environment (p < 0.01) and traveled a longer total distance (p = 0.01). The navigational aid had no effect on performance, as compared with the no aid condition. However, subjective measures showed that the subjects were more confident about their determination of location and direction (p < 0.01). They also preferred having the aid during navigation.
Conclusion
A navigational aid or map that provides shape information does not seem to improve performance in colonoscopy. In fact, it may lead to a false sense of security about location and orientation in the colon. The value of a map for training purposes remains to be examined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
“I saw a patient that was referred to Dr. Noloc from Dr. Lewob in the States. He is a famous guy and he sent a picture of a colon cancer and he said hepatic flexure colon cancer and Dr. Noloc scoped him and I was out in the hall and Dr. Noloc said come on in here and take a look at this and I said ‘Yeah, it is a left hepatic flexure colon cancer’ and Dr. Noloc put the x-ray machine on and sure enough it was splenic flexure. So, he would have gone to the OR and maybe taken out the wrong side.” Quote from an interview with a gastroenterologist about how difficult it is to orient in the colon, January 19, 2000. The names of the individuals are fictitious.
Colorectal cancer is the second leading cause of cancer death in North America [14, 15]. Colonoscopy is now widely used to investigate suspected colorectal disease and to screen for high-risk individuals [10]. Although colon cancer is successfully treated at a rate of 90% if detected at an early stage, the compliance rate for screening in the United States is only 30%. Resistance to regular colonoscopies is largely because the procedure is perceived by many to be extremely uncomfortable. The uncomfortable nature of the procedure results, among other things, from the frequent need for trial-and-error manipulations of the scope in navigating the colon. In performing the procedure, the endoscopist must manipulate the scope through the entire length of the patient’s large colon, with essentially 4 degrees of control freedom available: longitudinal (pushing and pulling), roll (twisting of the scope), and pitch and yaw (use of independent knobs at the proximal end of the scope).
For the novice endoscopist, disorientation, or “getting lost,” is one of the greatest problems in performing a colonoscopy [4, 7]. This leads to incomplete examination of the colon, potential missed detection of lesions, or incorrect location of tumors for surgery. Several factors contribute to disorientation in colonoscopy, including limited physical/motoric control and manipulability because of the colon’s dynamic nature and the lack of meaningful haptic feedback, a dearth of meaningful perceptual information for spatial orientation, and high cognitive demands [4]. These combine to increase the physical and mental workload for the endoscopist.
Perhaps most seriously, loops can potentially form anywhere along the length of the flexible scope. Looping in the colon is surprisingly common, reportedly occurring in 91% of cases [18]. The lack of meaningful haptic feedback makes it difficult to detect looping because of the scope’s stiffness and the high tension developed once it has been twisted inside the colon.
From the endoscopist’s point of view, the lack of full visual guidance during this procedure often is the key bottleneck determining the success of colonoscopy procedures. In fact, most endoscopists cannot determine the state of the scope in the colon on the basis of feel alone because the resistance to scope advancement is high throughout the length of the colon [3]. Without a direct view of the colon and the endoscope, the endoscopist occasionally must rely on guesswork to infer the location of the scope, and thus the location of a lesion. It stands to reason, therefore, that a navigational aid designed to provide the information necessary for the endoscopist to localize and orient accurately within the colon should significantly improve the safety, efficiency, and comfort of the procedure.
To date, limited effort has been invested toward the development of such navigational aids. Cirocco and Rusin [6] have advocated the use of fluoroscopy to guide colonoscopic examination and to aid in the learning of scope intubation techniques. However, most hospitals do not have the necessary equipment readily available in their endoscopy suites. Some endoscopists find fluoroscopy too time consuming because it requires interruption of the procedure for x-ray pictures. The x-rays provide only two-dimensional (2D) static images. Also, the patient is exposed to excessive radiation.
More recent developments have steered away from the use of radiation for tracking. Saunders et al. [17, 18] have shown that by using magnetic endoscope imaging, a nonradiographic technique for imaging the colonoscope shaft in real-time, performance of colonoscopy can be improved. In particular they have presented a computer-generated 2D display of the scope shaft inside the patient, with anatomic markers to indicate the positions of the various organs surrounding the colon, as well as gray shadings to create a 3D effect. The preliminary result for one expert endoscopist showed that although time to task completion was not improved, the number of attempts at straightening loops in the scope was reduced.
Other researchers have experimented with mechanical solutions such as a robotic colonoscope [5, 16], oblique transparent cylinders [20], use of a body with graduated stiffness to gain more control over the behavior of the scope [2], circumvention of the need to perform a colonoscopy entirely by doing virtual colonoscopies [1], or use of wireless ingestible capsules (for small bowel inspection) [9, 13, 19].
With the exception of the magnetic imaging technique, none of these proposed solutions addresses the problem of orientation in real time, with or without loop formation. The reason may well be the nonrigid nature of the colon itself, which stretches and moves within the abdominal cavity in response to physical manipulation of the scope. Thus, current navigational aids in the form of real-time, segmental, or 3D maps are available only in computer simulations. For example, the “map” feature on the colonoscopy simulator, GI Mentor, Simbionix, Ltd., Lod, Israel for procedural skills training provides users with a view of the scope’s progress through the colon. This map is intended for use when the endoscopist is stuck and needs to see the cause of the obstruction. It also may be useful for teaching purposes. However, it is not clear whether such an aid can help in learning to navigate in colonoscopy, or whether the use of such an aid during training can become a crutch. No systematic study has been conducted to evaluate the effectiveness of such a navigational aid for colonoscopy performance.
In this study, a real-time display of the scope’s shape was designed, and an experiment conducted to determine the effectiveness of this display for navigation in the colon. It was hypothesized that a navigational aid would be useful for orienting in navigation, especially in a nonrigid environment such as the colon. In addition, it was expected that the aid would provide the user with a sense of assurance, which often is missing in blind navigation. To test these hypotheses, a mock-up of an endoscopy unit was set up using regular clinical endoscopy equipment and simulated colons.
Materials and methods
Display design
A ShapeTape sensor (model S1280CS, Measurand, Inc., Fredericton, NB, Canada) [12]) was used to track the position and shape of the colonoscope. The ShapeTape comprises a series of fiber optic sensor pairs encased in a narrow strip of flexible spring steel and elastomers and configured to measure twist and bend. Along the 96-cm length of the tape, 16 pairs of sensors are placed 6 cm apart. Analogue sensor signals are digitized and used to calculate the position of each sensor pair relative to the first proximal pair of sensors.
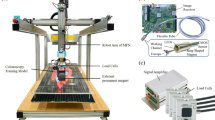
The prototype used in the current investigation had an SGI O2 workstation to generate a graphic model of the scope using imaging software written in C++ and OpenGL. Thus, by coupling the ShapeTape with an endoscope, the position, direction, and shape of the endoscope could be tracked in real time relative to an origin at the proximal end of the scope. The shape of the tape was rendered in real time as a cylindrical object with a tapered end on a perspective grid plane (see insert in Fig. 1). The graphic image depicting the scope was rendered in cyan, whereas the background of the display was in gray. The display space above the grid represented the abdominal cavity, with the size of the space and graphics scaled to the scope and task space. By insertion of the adapted scope into a simulated colon (see Task Environment section), the information displayed showed the location of the beginning of the scope, starting at the insertion point, as well as the length and shape of the scope inside the colon, all in real time.
Subjects
The participants in this study were 14 untrained subjects (6 female and 8 male graduate and undergraduate students at the University of Toronto and Tufts University). The subjects were paid $20 for their participation. All the subjects signed an institutional review board–approved informed consent form.
Training
The subjects were given a short tutorial on the anatomy of the colon using textbook illustrations as well as a demonstration on how to use the colonoscope and how to interpret the navigational aid display. Because many colonoscopy procedures are routinely performed by gastroenterology fellows who have not had extensive prior experience manipulating the colonoscope and are learning “on the job” [4], the subjects were given only one practice trial with the navigational aid display. All the subjects were comfortable with control of the scope after the practice.
Task environment
To address the rigidity issue, both a rigid and a nonrigid simulated colon model were built and used as the two independent task environments. As evaluated by two experienced colorectal surgeons, the nonrigid colon model was, at a first approximation, representative of a real colon environment as experienced through a colonoscope in terms of both visual appearance and mechanical compliance. The rigid colon was identical in visual appearance to the nonrigid one, but was not compliant.
Equipment
A 180-cm video colonoscope (Pentax EC-3830L, Pentax Precision Instrument, Corp., Orangeburg, NY), a Pentax EPM-3300 video processor, and a light source were used for the experiment. A 27-in. Sony PVM monitor (Sony Corp., San Diego, CA) was used to display the endoscopic image, together with the navigational aid, in an augmented reality display (Fig. 1).
Task
The task was a modified colonoscopy procedure within the simulated colon using the endoscopic image with or without the navigational aid illustrated in Fig. 1. The subjects were asked to guide the colonoscope from the rectum through the colon as quickly and safely as possible, as in a real colonoscopy. The safety constraint was emphasized by the caution that perforation of the colon would result from continued pushing when the tip of the scope was against the wall of the colon or if loops were generated and not subsequently released. No subject perforated the colon during the experiment. Unbeknownst to the subjects, the trials were always stopped when the simulated splenic flexure was reached, although they were told that the trials were to terminate at random points during the procedure. They also were told that no trials would reach the cecum.
The subjects were told that, in addition to “good performance” with the scope (i.e., traversing the colon quickly and safely), they were required to keep track of how far they had traveled inside the colon. At the end of each trial, the displays were turned off and the subjects were asked to indicate the location and orientation of the scope’s end inside the colon. The subjects did this by marking an arrow on a paper drawing of the colon with major segments clearly labeled to indicate the position of the scope end with respect to the colon, as well as the direction in which subjects believed the scope was pointing (Fig. 2).
Experimental design
Each of the 14 subjects performed one trial in both the rigid and nonrigid colons, with and without the navigational aid, for a total of four trials. The design used was a 2 × 2 (2 colon rigidities × 2 display options) Latin square.
Dependent measures
Performance measures were time to task completion, total distance traveled (or efficiency of motion), and accuracy of location and direction of the colonoscope end point. The variable total distance traveled deserves some explanation because subjects always ended up at the same point within the same simulated colon, suggesting that the distance was a constant quantity. However, the meandering of the scope tip inside the colon can trace out an effectively longer trajectory, especially when local disorientation occurs, indicating the efficiency of travel.
As described earlier, the data on accuracy in location and direction were collected via paper drawings at the end of each trial (Fig. 2). These were measured by first scanning the individual drawings and markings into digital format, and then scoring manually by calculating the error in absolute distance and absolute angle on the global frame of reference. Subjective ratings of confidence were collected at the same time as the location and direction measures, using a 5-point scale. A rating of 1 indicated low confidence that the location or direction was correct, whereas a rating of 5 indicated high confidence of a correct answer.
Cognitive effort, or mental workload, involved in spatial orientation was measured using the standardized NASA TLX (Task Load Index) questionnaire [8]. At the end of each trial, the subjects were asked to fill out a NASA TLX questionnaire using all six dimensions: 1. mental demand, 2. physical demand, 3. temporal demand, 4. performance, 5. effort, and 6. frustration.
Other subjective measures included preference rankings and usefulness ratings of the navigational aid display. In particular, at the end of the experiment, subjects rank ordered their preference for the navigational aid display or no aid, and rated its “usefulness” on a scale from 0 (very useless) to 10 (very useful).
Results
A two-way analysis of variance (ANOVA) was conducted for each dependent measure. The results of the analyses show that the display did not affect colonoscopy performance (see Table 1 for summary statistics). The total time (F[1,52] = 17.95; p < 0.01) and total distance traveled (F[1,52] = 7.02; p = 0.01) were significantly longer in the nonrigid colon than in the rigid colon (Table 2). None of the other performance measures (i.e., efficiency, location error, and direction error) nor the subjective workload differed between the two colon conditions. There was a significant difference in confidence ratings for both location and direction determinations as a function of display. The subjects were more confident in their answers judging location (F[1,52] = 9.54; p < 0.01) and direction (F[1,52] = 24.04; p < 0.01) of the scope when using the navigational aid than when using no aid (Table 3). There was no significant interaction between display and colon rigidity in any of the performance and subjective measures. The subjects preferred the navigational aid display over the no aid display, and rated the usefulness of the aid as 8.3 ± 1.6, compared with 0.9 ± 1.3 for no aid, on a scale from 0 (very useless) to 10 (very useful).
Discussion
The results show that the navigational aid did not improve task completion time or efficiency of travel. This is similar to results reported by Saunders et al. [17] for the nonradiographic magnetic imager. As expected, navigating through a rigid environment was easier than navigating through a nonrigid environment, as evidenced by the time and distance results.
In general, location and direction judgments in spatial orientation were poor, with location errors averaging190 mm and direction errors ranging 60° to 110° from the true direction of the endoscope. This large direction error most likely resulted from the fact that direction was coupled with location in the colon. That is, as shown in Fig. 2, a forward-facing scope in the descending colon would be directed at 90° relative to the global frame of reference, and a forward-facing scope in the transverse colon would be directed at 180°. Thus, if the subject misjudged the location of the scope tip to be in the descending colon, but correctly judged the scope to be facing forward, the direction error could be as large as 90°. Indeed, on several occasions, the subjects thought that the scope was still in the descending colon when it was in fact in the transverse colon.
Surprisingly, no significant effect of display condition on location and direction errors was found, despite the fact that the very nature of the displays strongly suggested that performance with the navigational aid would be superior. One reason for this result is that subjects had not learned to map the spatial frame of reference provided by the displays to the 2D drawing of the colon. There was, however, a significant main effect with respect to the display factor in terms of subjects’ confidence in their location and direction estimates. This may represent a false sense of confidence.
Assessment of weighted overall workload using the NASA TLX questionnaire showed that, contrary to expectation, workload was not significantly different between the rigid and nonrigid colon conditions. These results may be attributable to the relatively simple and short length of the colon models, which were similar in length to a sigmoidoscopy rather than a colonoscopy. Had the colons been longer and more complex, the effects may have been more pronounced. Subjects’ workload while using the no aid display was not higher, which was not surprising (although somewhat counterintuitive). Indeed, it has been shown that sometimes when a task load is too high, subjective workload decreases [21].
Usefulness ratings concurred with our hypothesis. The no aid display rated as 1 (very useless) on an 11-point scale (0 to 10), and the navigational aid display rated as 8.5 (close to very useful). These ratings also concurred with the order of preference ratings for the displays. All the subjects preferred the navigational aid display over the no aid display.
Conclusion
Unlike large-scale rigid environments for navigation, in which invariant features typically exist to specify the spatial configuration of the environment, even if it is a dynamic environment (as characterized by other moving bodies within the space), the nonrigid colon is an enclosed self-contained environment that makes it difficult for the endoscopist to maintain an accurate cognitive map of the environment. There are no external anchors such as the sun, sky, magnetic north, or gravitational force for maintaining spatial orientation. Because colonoscopy is primarily a visually guided procedure, visualization of spatial information, particularly explicit shape information, was proposed as a solution that could help support spatial orientation in colonoscopy. In addition, the proposed navigational aid display, illustrated conceptually in Fig. 1, also may reduce the cognitive load in orientation and navigation during a colonoscopy. Furthermore, it could be used as a training tool for novice endoscopists to use in visualizing the outcomes of their scope manipulations, especially given the lack of haptic feedback to aid learning. Such visual feedback might be particularly useful for first-year fellows learning to perform colonoscopies for the first time [11].
Although such a display may not necessarily reduce the total time required for an experienced endoscopist to perform an examination, it would at least be likely to reduce the number of painful scope manipulations [17], as well as the uncertainty in locating lesions and tumors. Confidence in the spatial orientation task also was higher with the navigational display than without it. One cautionary note in designing any display enhancement is that it may lead to a false sense of confidence, which could be especially dangerous when accurate spatial estimation is important, as in locating tumors for surgery.
Clearly, an important consideration in evaluating this research is the fact that our subjects were not experienced endoscopists. We reasoned, however, that in light of our global objectives, which were related to the ability to comprehend and make use of the spatial information provided by the navigational aid, the absence of surgical experience on the part of our subjects should not invalidate our findings relative to those objectives. Nevertheless, it also is clear that as a practical evaluation of an enabling technology, any transfer of the validity of our results to actual colonoscopy procedures remains to be demonstrated. The next logical step in future research is to test the usefulness of the navigational aid display for training novice endoscopists, as well as its transferability to actual colonoscopy performance and its value for patient outcome.
References
Bond J (1999) Virtual colonoscopy-promising, but not ready for widespread use (editorial). N Engl J Med 341: 20
Brooker JC, Saunders BP, Shah SG, Williams CB (2000) A new variable-stiffness colonoscope makes colonoscopy easier: a randomized controlled trial. Gut 46: 801–805
Cao CGL (2001) Designing for spatial orientation in nonrigid endoscopic environments. Proceedings of the 45th Annual Meeting of the Human Factors and Ergonomics Society, pp 1259–1263
Cao CGL, Milgram P (2000) Case studies of disorientation in minimally invasive surgery. Proceedings of 44th Annual Meeting of the Human Factors and Ergonomics Society and XIVth Triennial Congress of the International Ergonomics Association 4: 169–172
Carrozza MC, Arean A, Accoto D, Menciassi A, Dario P (2003) A SMA-actuated miniature pressure regulator for a miniature robot for colonoscopy. Sensors Actuators A 105: 119–131
Cirocco WC, Rusin LC (1996) Fluoroscopy: a valuable ally during difficult colonoscopy. Surg Endosc 10: 1080–1084
Cotton PB, William CB (1990) Practical gastrointestinal endoscopy. Blackwell Scientific Publications, London, UK pp 99–143
Hart SG, Staveland LE (1988) Development of NASA TLX: results of empirical and theoretical research. In: Hancock PA, Meshkati N (eds) Human mental workload. Elsevier, Holland pp 139–183
Iddan G, Meron G, Glukhovsky A, Swain P (2000) Wireless capsule endoscopy. Nature 405: 417
Lieberman DA, De Garmo PL, Fleischer DE, Eisen GM, Helfand M (2000) Patterns of endoscopy use in the United States. Gastroenterology 118: 619–624
Mahmood T, Darzi A (2004) The learning curve for a colonoscopy simulator in the absence of any feedback: no feedback, no learning. Surg Endosc 18: 1224–1230
Measurand, Inc. Retrieved xxxx at http://www.measurand.com. Cited 16 May 2006
Meron G (2000) The development of the swallowable video capsule (M2A). Gastrointest Endosc 6: 816–819
National Cancer Institute (2006) Colon and rectum: U.S. racial/ethnic cancer patterns. Retrieved May 15, 2006 at http://www.cancer.org/docroot/PRO/content/PRO_1_1_Cancer_Statistics_2006_Presentation.asp
National Cancer Institute of Canada (2006) 2006 Canadian Cancer Statistics. Retrieved May 15, 2006 at http://www.ncic.cancer.ca/ncic/internet/standard/0,3621,84658243_328386486__langId-en,00.html
Ng WS, Phee SJ, Seow C, Davies BL (2000) Development of a robotic colonoscope. Digest Endosc 12: 131–135
Saunders BP, Bell GD, Williams CB, Bladen JS, Anderson AP (1995) First clinical results with a real-time electronic imager as an aid to colonoscopy. Gut 36: 913–917
Shah SG, Saunders BP, Brooker JC, Williams CB (2000) Magnetic imaging of colonoscopy: an audit of looping, accuracy, and ancillary maneuvers. Gastrointest Endosc 52: 1–8
Sidhu R, Sanders DS, McAlindon ME (2006) Gastrointestinal capsule endoscopy: from tertiary centres to primary care. Br J Med 332: 528–531
Tsumura T, Torii A, Fujita S, Takeda J, Hikita H, Nishikawa H, Ochi J, Miura K (2003) Usefulness of oblique transparent cylinders in facilitating colonoscopy. Digest Endosc 15: 121–124
Tulga MK, Sheridan TB (1980) Dynamic decisions and workload in multitask supervisory control. IEEE Transact Systems Man Cybernetics 10: 217–232
Acknowledgments
Funding for this research was provided by the National Science and Engineering Research Council of Canada, the Institute for Robotics and Intelligent Systems/PRECARN, and a Tufts University Faculty Research Award. In-kind support was provided by Measurand, Inc., Pentax Canada, Pentax, Inc., and DASIE International. The writing of this article was made possible by support from the Tufts Mellon Award.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cao, C.G.L. Guiding navigation in colonoscopy. Surg Endosc 21, 480–484 (2007). https://doi.org/10.1007/s00464-006-9000-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-9000-3