Abstract
Background
We report 104 consecutive cases of hand-assisted laparoscopic (HAL) colectomy over 5 years performed by a single surgeon.
Methods
Data were gathered prospectively and include patient demographic data, diagnosis, operating time, conversion rate, length of hospital stay, and complications. Virtually all patients presenting for elective resection with benign disease and metastatic cancer were treated using HAL techniques.
Results
The mean age was 61 years; 48% of patients had diverticulitis; 21%, colorectal cancer; 18%, benign polyps. In addition, 55% of patients underwent sigmoid or left colectomy; 27%; right hemicolectomy; 9%, low anterior resection, and two double resections were performed. Mean operating room time was 135 minutes; in 12% of the patients conversion to open surgery became necessary, in most cases requiring only a small extension of the HAL incision. Mean and median discharge was postoperative day 4 and postoperative day 3, respectively. There was 1 death (1%) and 21% of patients had complications, 12% of them major.
Conclusions
Hand-assisted laparotomy colectomy is a safe and effective procedure. The data in terms of length of hospital stay and operative time compare favorably with published data for conventional laparoscopic (CL) colectomy. Although further study is necessary, it appears that HALS confers all of the advantages of CL for colectomy, with no obvious drawbacks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopy has greatly improved surgical outcomes in many areas of abdominal surgery. Laparoscopic cholecystectomy and antireflux surgery have become the gold standard for acute and elective indications, virtually replacing their open counterparts. Other procedures, specifically laparoscopic colectomy, have not enjoyed similar universal acceptance. The reasons for this are many: a steep learning curve, uncertainty about the procedure’s effectiveness for malignancy, long operating time, and lack of tactile feedback, among others. Multiple series, however, have shown that laparoscopic approaches to colorectal disease result in more rapid patient recovery [7, 10, 11, 13]. There remain uncertainties about the adequacy of laparoscopic colectomy for curable malignancy, the most common elective indication for colectomy [16], although recent work suggests that survival is not compromised [5, 8].
The first laparoscopic colectomy, performed by Jacobs in 1990, was termed “laparoscopically assisted” because a mini-laparotomy was required at the end of the procedure to deliver the specimen and perform mesenteric ligation, bowel division, and anastomosis [6]. In fact, most surgeons performing laparoscopic colectomy need to make an incision measuring at least 2.5 cm for specimen extraction, and most surgeons also use this incision to facilitate mesenteric and bowel division, and the anastomosis.
In 1993 hand-assisted laparoscopic colectomy was described as a hybrid procedure [12]. It was proposed with the thought that a slightly larger incision to accommodate the surgeon’s hand, made at the start of the procedure, would eliminate many of the drawbacks noted above. The evolution of hand-assist devices has eliminated some of the more cumbersome aspects of the procedure, but technical problems remain. Despite the larger incision, it appears that HAL surgery is more like conventional laparoscopy (CL) than like open surgery. A randomized single center study [14], and the interim report of a randomized multicenter clinical trial [9] concluded that HAL colectomy retains the clinical benefits of traditional laparoscopic surgery including diminished postoperative pain, faster return of bowel function, and shorter hospital stay and return to normal activity. Several advantages of the hand-assisted approach were emphasized: the inserted hand can provide tactile feedback, better organ retraction, blunt dissection, and better control of bleeding as needed.
The senior author (DGB) began to perform HAL colectomies in 1999 and saw no difference in clinical outcome compared to his experience with CL colectomy (unpublished data). Additional benefits were recognized: shorter operative times and the ability to deal with more complex pathology. Thus, since 2000, all laparoscopic colon cases except stoma construction have been performed using HAL techniques. All HAL bowel resections performed by the senior author are included in this report.
Materials and methods
From 1999 to 2004, 104 HAL colectomies were performed at two community hospitals in the Boston suburban area by a single surgeon. All data were prospectively entered into a registry. All patients presenting for elective resection with benign large bowel disease (excluding ulcerative colitis), endoscopically nonresectable polyps as well as selected patients with large bowel cancer for palliation were offered HAL colectomy. Because of the known risk of complications, patients with morbid obesity (BMI >40) and those requiring emergent procedures were not offered HAL colectomy.
Details of procedures
All patients underwent mechanical bowel preparation prior to surgery. A dose of broad spectrum antibiotics was given on call to the operating room. No epidural blocks were used.
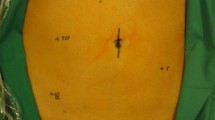
The procedures were performed using a variety of hand-assist devices (Pneumosleeve [Dexterity Surgical, Roswell, GA], HandPort [Smith & Nephew Endoscopy, Andover, MA], GelPort [Applied Medical, Rancho Santa Margarita, CA], and LapDisk [Ethicon Endo-Surgery, Cincinnati, OH]). The hand-assist device was always placed in the midline, after insufflation of the abdomen, through a 7-cm incision (measured after insufflation). Two additional trocars were placed: for left colectomies, a 10-mm trocar was placed in the upper midline for the camera, and a 12-mm trocar was placed in the right lower quadrant; for right colectomies, a 10-mm trocar was placed in the upper midline for the camera, and a 5-mm trocar was placed on the left side (Fig. 1). Occasionally, an additional 5-mm trocar was placed on the left side to assist in mobilizing the splenic flexure for left colectomy.
For left sided resections, the surgeon stands on the patient’s right, using his left (non-dominant) hand for retraction and dissection. The bowel is divided at the distal margin using an endoscopic linear stapler (Ethicon Endo-Surgery, Cincinnati, OH), and the mesentery is divided with the Harmonic Scalpel (Ethicon Endo-Surgery, Cincinnati, OH) or linear stapler to the proximal point of resection. The bowel is then exteriorized, divided, and the anvil for a circular stapler (Ethicon Endo-Surgery, Cincinnati, OH) placed. The bowel is then replaced, pneumperitoneum is established, and the anastomosis is constructed transanally.
For right sided resections, the surgeon stands on the patient’s left, using his left hand for retraction and dissection. The bowel is mobilized and then exteriorized through the HAL incision, and the bowel is divided and reanastomosed using conventional open techniques. Rarely, intracorporeal division of the bowel and/or mesentery becomes necessary.
Primary outcome variables were operating time, conversion rate, length of hospital stay, and complications. These data were entered at the time of occurrence.
Data were analyzed using the Microsoft Excel X software package (Microsoft Corporation, Redmond WA). Statistical significance was determined with analysis of variance (ANOVA) or Student’s t-test, where appropriate. A p value of <0.05 was considered significant. Standard deviation of the mean and ranges were presented in parentheses in the reports.
Results
Data analysis included all patients, including those who were converted to open procedures.
Demographics
The mean age in this series was 61 ± 16 years. Gender distribution was about equal, with 54 female patients.
Diagnosis and procedures
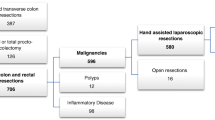
The diagnoses and procedures are listed in Table 1. Most of the patients had recurrent or complicated diverticulitis (48%); nine had fistulas (5 colovesical, 4 colovaginal). Mobilization of the splenic flexure required in 23% of the patients, about half of all sigmoid or left coletomies.
The next most common disease encountered was cancer (22%). Most of cancer patients were known to have metastatic disease (15 patients) and were treated for palliation. Five patients had cancer detected in a polyp, and 3 patients had significant medical comorbidities that were thought to make open resection relatively contraindicated.
Patients with benign colonic polyps (18%) and other indications (intussusception, diverticular bleeding, carcinoid, lipoma, stricture) accounted for the remainder of patients. Approximately 42% of the patients in this series had prior abdominal surgery.
Time
Operative time averaged 135 (range: 70–280) minutes. Patients undergoing right colectomy had shorter mean operative times at 108 (range: 76–170) minutes than those undergoing left, sigmoid colectomy, or LAR at 150 (97–280) minutes. Patients converted to open procedures had an average operating time of 177 (65–366) minutes.
The operative time for the first 30 cases was also significantly longer than that for the latter 80 cases, at 170 minutes versus 125 minutes (Fig. 3).
Conversion
Any extension of the HAL incision was considered a conversion. Thirteen cases (12%) were converted, most requiring only a small extension of the HALS incision. The conversion rate was 17% for the first 30 cases, and it then reached a plateau between 11% and 13%, suggesting a learning curve of 30 cases (Fig. 2).
Conversions were required in 5 patients with diverticulitis (3 sigmoid resections, 2 LAR). One patient had a colovesical fistula. One of these patients accounts for the only death in this series. Three patients were converted for an air leak at the anastomosis; 2 others had adhesions. For 4 patients with cancer, the procedure was converted because of bulky or fixed tumors (2 right colon, 2 left colon). Two patients with polyps were converted, 1 for a rectal tear during stapler insertion, 1 because of an inability to localize the lesion. One patient with Crohn’s disease and one for Hartman’s reversal were converted for adhesions.
Length of stay
Mean length of hospital stay was 4.0 (±2.6) days; median length of stay was 3 days. Patients undergoing right colectomy did not have significantly shorter lengths of stay than those undergoing left or sigmoid colectomy or LAR. Patients who were converted to open procedures had a length of stay of 5.5 days. All patients were passing flatus and tolerating a regular diet at the time of discharge.
There were 4 readmissions (4%): 1 patient who was discharged on postoperative day (POD) 3 after a right colectomy was readmitted on POD 5 for SBO; 1 patient who underwent a sigmoid colectomy and was discharged on POD 4 was readmitted on POD 7 for a pelvic abscess; 1 patient who underwent a right colectomy and was discharged on POD 2 was readmitted on POD 12 for a perianastomotic phlegmon; 1 patient who underwent a transverse colectomy and was discharged on POD 5 was readmitted on POD 22 with a colocutaneous fistula.
Mortality
The single death in this series occurred in a 68-year-old female who underwent an open (converted) LAR for diverticulitis and a colovesical fistula. She had oxygen- and steroid-dependent COPD and coronary artery disease. After an uneventful 8-day postoperative course, after which she was walking, passing flatus, and eating, the patient developed unexplained renal failure, which spiraled into multi-system organ failure. Contrast enema, CT scan, and subsequent laparotomy failed to find an intra-abdominal source of sepsis. She died 22 days postoperatively.
Complications
There were no intraoperative complications related to the HAL device or the trocars. Twenty-one complications occurred postoperatively. Major complications (12 patients) were defined as those that prolonged hospital stay, required readmission or reoperation, or were potentially life-threatening. One patient experienced an early bowel obstruction/delayed ileus, requiring readmission on POD 5, 2 days after discharge. This responded to conservative treatment. One patient, a mildly obese patient (BMI 31) with steroid-dependent COPD experienced a wound dehiscence from the HAL incision requiring reoperation and repair. This patient and the patient who ultimately died represent the only reoperations. There was one pelvic abscess that responded to CT-guided drainage and intravenous antibiotics, one peri-anastomotic phlegmon that also responded to antibiotics and bowel rest. No anastomotic leak was identified on contrast enema in these patients. There were two deep venous thomboses and four incisional hernias seen on a mean follow-up of 2.3 years. There was one anastomotic bleed requiring transfusion. One patient developed a colocutaneous fistula that closed spontaneously. Minor complications in 11 patients were wound infections. None of the patients with colorectal cancer had trocar or hand-port site recurrence.
Discussion
This study, which represents the largest published experience to date on HAL colectomy, confirms the safety and effectiveness of HAL in colorectal surgery as a standard approach with operative times, length of stay, and complications comparable with what has been reported in previous studies of HAL and CL colectomy. We describe a consecutive series of 104 HAL colectomies by a single surgeon. Since 1999, we have used the HAL approach exclusively for virtually all elective colon resections for benign disease, and for palliation of cancer. Our report demonstrates that HAL techniques can be used as a first-line procedure in bowel resections with good outcomes. Although this study was not designed specifically to compare the HAL approach with open or CL techniques, our data compares favorably with published data on CL colon surgery, suggesting that HAL is more analogous to CL than to open techniques (Table 2).
The Spanish Randomized Trial comparing CL colectomy with HAL colectomy concluded that HAL simplified difficult intraoperative situations, thereby reducing the need for conversion, and that it should be considered a useful adjunct when difficult situations arise during CL [14]. In that study, there was no significant difference in length of hospital stay or operative time between the 2 groups. Conversion rate was higher in the CL group (22% versus 7%), although surprisingly, this was not statistically significant, which raises questions about the power of the study. The HAL group had significantly higher postoperative levels of the inflammatory mediators C-reactive protein and interleukin-6, but this did not seem to affect clinical outcome. It is unclear from the report how many surgeons performed the various procedures and how many cases each performed prior to the study. Our data suggest a learning curve of 30 cases before the conversion rate and operative time plateau (Figures 2 and 3) The HALS Study group trial concluded that HALS retains the benefits of minimally invasive surgery and may allow the surgeon to perform complex operations more easily [3].
Studies published to date evaluating HAL surgery, and HAL colectomy in particular, have small numbers of patients (Table 3). Additionally the HALS Study group included a large number of surgeons with varying levels of experience. Five of the 8 institutions participating in the study were in Europe or South America with very different healthcare delivery systems, making length of stay data heterogeneous [4]. These issues combine to muddy the data, making comparison with current study somewhat speculative.
Our patient population matches well with other reported series in terms of diagnosis and procedures performed (Tables 1 and 3) [2, 3, 9, 14]. Operative time in our series is also similar to previous studies. One would anticipate that, as in this series, operative time would decrease with experience.
Our conversion rate is 12% (13 patients), which is in the higher range of other published HAL studies. This relatively high conversion rate may reflect the fact that 44% of our patients had previous abdominal surgery; 7 of the 13 conversions had prior laparotomies. In addition, we did not exclude patients with complex or difficult pathology, such as diverticular or Crohn’s fistulas, bulky or fixed tumors, or carcinomatosis, which predictably makes the procedure more difficult. The improved tactile feedback with HALS affords greater confidence in attempting these cases. The curve displayed in Figure 3 shows that the conversion rate plateaus after about 50 cases to approximately 10%. Case distribution was equal throughout the 110 cases. This “learning curve” is similar to what has been observed in CL cases, with the difference that success rate seems to be higher from the beginning. A previous study reported a success rate of 20% for the first 10 procedures, 60% for the second 10, and 80% after the first 30 (where the plateau was reached) in CL colon surgery [1].
Our length of hospital stay data compare favorably with other reports about HALS procedures (Table 3). The difference in feeding policy between centers makes comparison for length of stay data very difficult. All of our patients were offered clear liquids the day of surgery, and they were advanced to a regular diet when they passed flatus. This is identical to management of our patients undergoing open colectomy. All patients were tolerating a regular diet at the time of discharge.
We perform our incision for the HAL device in the midline because the mobilized colon is a midline structure, and we feel there is good access to the right as well as to the left side from the midline. It also keeps the lateral abdomen free of incisions should an ostomy ever become an issue, and it allows for easy conversion to an open procedure if necessary. In fact, most of the conversions only required a small extension of the HAL incision.
We did not notice any trocar site or HAL incision site recurrence in any of our patients operated on for colon cancer. Although trocar site recurrence is a concern [16], a recent prospective study comparing laparoscopic with open colectomy for cancer does not show any difference in survival between the two groups [8], and a randomized multi-center trial demonstrated oncological noninferiority for the laparoscopic approach [5]. There are no studies specifically evaluating HAL colectomy for cancer. Most HAL devices function as a wound protector, which should theoretically protect the HAL wound from tumor implantation.
Conclusions
This report summarizes a single surgeon’s prospective collection of data of HAL bowel surgery. We agree with previously published studies that the HAL approach to colorectal disease is safe and effective, and has outcomes similar to published data for CL surgery. In the present series no obvious drawbacks for HAL colorectal surgery have been identified. The adequacy of HAL techniques for malignant colorectal disease needs further study. Although the learning curve seems similar to that for CL bowel resection, the overall success rate, in terms of conversion, is higher, which may make HAL techniques more accessible to general surgeons. In addition, improved tactile feedback may facilitate the completion of more complex procedures or more difficult pathology.
References
Begos DG, Arsenault J, Ballantyne GH (1996) Laparoscopic colon and rectal surgery at a VA hospital. Analysis of the first 50 cases. Surg Endosc 10: 1050–1056
Cobb WS, Lokey JS, Schwab DP, Crockett JA, Rex JC, Robbins JA (2003) Hand-assisted laparoscopic colectomy: a single-institution experience. Am Surg 69: 578–580
Darzi A (2000) Hand-assisted laparoscopic colorectal surgery. Surg Endosc 14: 999–1004
Darzi A (2001) Hand-assisted laparoscopic colorectal surgery. Semin Laparosc Surg 8: 153–160
The Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopic ally assisted and open colectomy for colon cancer. N Engl J Med 350: 2050–2059
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1: 144–150
Khalili TM, Fleshner PR, Hiatt JR, Sokol TP, Manookian C, Tsushima G, Phillips EH (1998) Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum 41: 832–838
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363: 1187–1192
Litwin DE, Darzi A, Jakimowicz J, Kelly JJ, Arvidsson D, Hansen P, Callery MP, Denis R, Fowler DL, Medich DS, O’Reilly MJ, Atlas H, Himpens JM, Swanstrom LL, Arous EJ, Pattyn P, Yood SM, Ricciardi R, Sandor A, Meyers WC (2000) Hand-assisted laparoscopic surgery (HALS) with the HandPort system: initial experience with 68 patients. Ann Surg 231: 715–723
Muckleroy SK, Ratzer ER, Fenoglio ME (1999) Laparoscopic colon surgery for benign disease: a comparison to open surgery. JSLS 3: 33–37
Ramos JM, Beart RW Jr, Goes R, Ortega AE, Schlinkert RT (1995) Role of laparoscopy in colorectal surgery. A prospective evaluation of 200 cases. Dis Colon Rectum 38: 494–501
Romanelli JR, Kelly JJ, Litwin DE (2001) Hand-assisted laparoscopic surgery in the United States: an overview. Semin Laparosc Surg 8: 96–103
Schwenk W, Bohm B, Muller JM (1998) Postoperative pain and fatigue after laparoscopic or conventional colorectal resections. A prospective randomized trial. Surg Endosc 12: 1131–1136
Targarona EM, Gracia E, Garriga J, Martinez-Bru C, Cortes M, Boluda R, Lerma L, Trias M (2002) Prospective randomized trial comparing conventional laparoscopic colectomy with hand-assisted laparoscopic colectomy: applicability, immediate clinical outcome, inflammatory response, and cost. Surg Endosc 16: 234–239
Targarona EM, Gracia E, Rodriguez M, Cerdan G, Balague C, Garriga J, Trias M (2003) Hand-assisted laparoscopic surgery. Arch Surg 138: 133–141; discussion 141
Wexner SD, Cohen SM (1995) Port site metastases after laparoscopic colorectal surgery for cure of malignancy. Br J Surg 82: 295–298
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schadde, E., Smith, D., Alkoraishi, A.S. et al. Hand-assisted laparoscopic colorectal surgery (HALS) at a community hospital. Surg Endosc 20, 1077–1082 (2006). https://doi.org/10.1007/s00464-006-2002-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-2002-3