Abstract
Background
Neoadjuvant therapies have significantly improved local control and survival of patients with rectal cancer. Nevertheless, although a complete pathologic response can be achieved in 30% of cases, a transabdominal surgical resection is always required. This study aimed, for the first time, to test in the literature the feasibility of local excision combined with transanal endoscopic microsurgery (TEM) as a surgical option for patients treated with neoadjuvant chemoradiation.
Methods
Between July 1997 and December 2002, 30 patients with rectal cancer affected by an extraperitoneal tumor entered a protocol consisting of neoadjuvant chemoradiation followed by surgery. The surgical treatment, consisting of open surgery, local excision, or TEM, was planned according to the patient’s clinical response after chemoradiation and distance from the anal verge.
Results
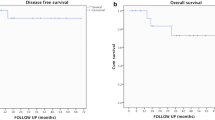
A significant clinical downstaging was observed in eight patients. Five of these patients underwent TEM, and three had local excision. Consequently, open surgery was performed for 22 patients. Histology showed six cases of complete pathologic response: three in the open surgery group and three in the transanal excision group. After a mean follow-up period of 47 months, the disease-free survival rate was 77% in the open surgery group and 100% in TEM or local excision group.
Conclusions
The findings suggest the complementary feasibility of TEM and local excision after neoadjuvant chemoradiation. However, randomized trials are needed to confirm the oncologic safety of this approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adenocarcinoma of the rectum is one of the most common causes of mortality attributable to cancer in western countries. The 5-year survival rate after surgical treatment does not exceed 50% because of local recurrence and distant metastases [1, 2]. Historical data show that in the absence of distant metastases, the prognosis is related to local invasion and lymph node involvement.
Local recurrence causes severe deterioration of clinical conditions and quality of life, and the median survival time is 10 to 12 months [3, 4]. Fecal incontinence and tenesmus are frequently reported. Pain, a significant cause of clinical worsening, is very difficult to treat effectively [5].
Total mesorectal excision (TME) and neoadjuvant treatments have been shown to improve the results of rectal cancer treatment, reducing the local recurrence rate [6] and improving survival [7]. As a consequence, the use of neoadjuvant treatment and radical surgery, including total mesorectal excision, is now considered to be an effective approach for patients with rectal cancer. It is reported that radiotherapy alone determines a complete pathologic response in about 30% of patients [8].
On this basis, Marks et al. [9] in 1988 first reported the use of neoadjuvant high-dose radiation therapy with full-thickness transanal excision in a series of 16 patients affected by early rectal cancer. Their article confirmed that local excision of early pretreated tumors can be performed safely with low morbidity and mortality rates and a local recurrence rate ranging from 0% to 3%. Because of infiltrated margins, two-step surgery was performed in less than 5% of all patients.
Similar results have been confirmed by more recent papers [10–13]. Concerning transanal endoscopic microsurgery (TEM), Lezoche et al. [14] recently reported the results for 40 patients with T2 rectal cancer treated using preoperative therapy and TEM excision. The local recurrence rate after a mean follow-up period of 56 months was 5%, and the results in terms of survival were similar to those for a group of patients treated with laparoscopic resection.
Although TEM and local excision have been described as surgical options after neoadjuvant therapy, they never have been used in combination. These two techniques, both characterized by a transanal approach, have similar oncologic effectiveness, but a substantial technical difference. Local excision is extremely useful for very low rectal tumors where TEM cannot be performed. On the other hand, TEM also can remove lesions of the upper rectum.
This report describes the results for a series of 30 consecutive patients with rectal cancer who underwent neoadjuvant therapy followed by open surgery, TEM, or local excision depending on the clinical restaging performed after chemoradiation and the distance of the tumor from the anal verge. This study aimed to verify the feasibility of this complementary transanal approach in selected cases.
Materials and methods
From July 1997 through December 2002, 98 patients with rectal cancer were observed at the Campus Bio-Medico University and considered for enrollment in a prospective protocol that included preoperative chemoradiation and surgical treatment. The protocol was approved by the institutional review board at our university.
All the patients underwent a pretreatment workup that included thoracic, abdominal, and pelvic CT scan; transanal ultrasound; barium enema of the rectum; pancolonoscopy (including biopsy); complete proctologic evaluation (digital examination and proctoscopy); and tumor marker (carcinoembryonic antigen, cancer antigen 19.9) levels.
The inclusion criteria required tumor location with the lower pole of the tumor ranging 0 to 10 cm from the anal verge; histologically proven adenocarcinoma; age younger than 75 years; clinical stage T2–T4, any N or M0; no prior pelvic radiotherapy; no synchronous other than in situ cervix or nonmelanoma skin malignancies; absence of cardiovascular contraindications; granulocyte count greater than 300 per ml; hemoglobin concentration greater than 10 g/ml; platelet count greater than 100,000 per ml; serum creatinine value lower than 1.5 mg/dl; no major undercurrent disease; and informed consent.
Preoperative chemoradiation was started within 10 days after completion of tumor staging. All the patients underwent concomitant chemotherapy and irradiation according to the following schedule: 5-fluorouracil (5-FU) 1,000 mg/m2 for 5 days in continuous intravenous (IV) infusion, cisplatinum (CDDP) 60 mg/m2 IV bolus on day 1, and 29 mg/m2 of PLAFUR-5 [15] or 15 mg/m2 of PLAFUR-5 modified in continuous venous infusion for 5 days. Both 5-FU and CDDP in continuous venous infusion were administered the first and last weeks of radiotherapy. The cisplatinum administration method (bolus or IV) was decided on the basis of toxicity data. Concurrent radiotherapy was delivered with standard fractionation (1.8 Gy/day) 5 days per week for a total dose of 50.4 Gy. A linear accelerator with 6 to 10 MV of nominal energy was used in all cases. A multiple-angled fields technique and immobilization devices were adopted to reduce intestinal irradiation.
Clinical restaging was planned 6 weeks after neoadjuvant treatment. This included thoracic abdominal and pelvic computed tomography (CT) scan, transanal ultrasound, proctoscopy, barium enema, and tumoral marker levels. The response to presurgical treatment was always evaluated by the radiologist together with the surgeon, the medical oncologist, and the radiotherapist. Surgery was performed 6 to 8 weeks after completion of neoadjuvant treatment.
Patients were considered eligible for transanal excision only in presence of a significant clinical response. We considered a clinical response as significant if the following were observed:
-
No mesorectal involvement on ultrasound or CT scan (ycT1-2).
-
No lymph node involvement (ycN0). Loco-regional lymph nodes were defined as positive if they appeared larger than 1 cm in diameter on ultrasound or CT scan.
-
No fixity at digital examination.
-
Mucosal involvement reduced to a scar smaller than 2 cm in diameter at proctoscopy.
The study design is summarized in Fig. 1. Informed consent for transanal excision was never denied by eligible patients.
Transanal excision was performed with conventional local excision or TEM, depending on the tumor distance from the anal verge: local excision in the case of lesions located 4 cm or less from anal verge and TEM for upper tumors. Candidates for transanal excision were evaluated the day before surgery by the treating surgeon, who assessed tumor distance from the anal verge and technical feasibility. At this time, the surgeon also decided the type of technique (TEM or conventional) to be performed.
Conventional local excision consisted of a full-thickness excision performed with electrocautery using a Parks dilator. Routine fresh-sampling histologic examination of the specimen margins was performed. The rectal wall was closed with absorbable sutures.
Transanal endoscopic microsurgery was performed according to the technique previously described by Buess et al. [16]. Carbon dioxide insufflation and a stereoscopic optical system allowed the surgeon to observe a three-dimensional operating field. Special endoscopic tools provided good visualization of the rectal lumen and the possibility of suction and washing out, allowing good excision of the lesion and wound suturing. After histologic confirmation that specimen margins were negative, the procedure was concluded by closure of the rectal wall with a continuous suture secured by silver clips.
For all the cases, intra- and postoperative morbidity as well as mortality data were prospectively collected. After discharge from the hospital, all the patients underwent strict follow-up assessment. This included a clinical evaluation every 30 days for the first year as well as transanal ultrasound or pelvic Magnetic resource (MR), proctoscopy, marker levels, and digital examination every 2 months for the first year and every 4 months for the second year. A colonoscopy was performed 6 months after surgery. A total body CT scan was performed 6, 12, 24, and 36 months after surgery.
Results
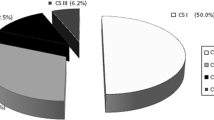
On the basis of the inclusion criteria, 30 of 98 patients (mean age, 64 years; range, 49–75 years; 21 men and 9 women) entered the protocol. The most common reasons for exclusion were age (35 patients) and the presence of distant metastases (20 patients). Table 1 presents the patients’ characteristics, and Table 2 presents the results of pretreatment staging. In all cases, chemoradiation could be fully delivered. Data regarding this treatment are presented in Table 3.
All the patients underwent clinical restaging 6 to 8 weeks after completion of treatment (Table 4). Tumor downstaging was documented in 19 patients, but 8 of 19 patients showed a significant response. In one case, an upstaging that consisted of multiple hepatic metastases was shown.
Transanal excision group
On the basis of tumor distance from the anal verge, TEM was indicated for five patients and conventional excision for three patients (Table 5). There was no perioperative mortality. Two postoperative complications were recorded in the TEM group: one case of transient fecal incontinence and one case of rectal bleeding. The mean postoperative time to these complications was 5.3 days (range, 3–13 days). In one patient, residual islets of adenocarcinoma were found in perirectal fat (ypT3). For this reason, the patient underwent an anterior resection of the rectum. A complete pathologic response was observed in three patients.
The mean follow-up period was 37 months (range, 24–66 months). No patient was lost to follow-up evaluation. One patient experienced a mucosal recurrence 10 months after surgery and underwent an abdominoperineal resection. There were no cases of lymph node recurrence or distant metastases. At this writing, all the patients are free of disease.
Open surgery group
A total of 22 patients underwent open surgery, but because of one peritoneal carcinomatosis case diagnosed at the time of surgery, a total mesorectal excision was performed for 21 patients, and a temporary stoma was intraoperatively performed in 3 cases. There was no perioperative mortality. For two patients, postoperative anastomotic leakage required a temporary stoma. The mean postoperative time was 8 days (range, 6–14 days). A complete pathologic response was observed in three patients.
The mean follow-up period was 48 months (range, 25–76 months). No patient was lost to follow-up evaluation. The disease-free survival rate was 77%. Local recurrence occurred in three cases (13%).
Discussion
Surgeons consider the transanal approach to be an appealing option because it results in no mortality, less frequent and rarely life-threatening morbidity, shorter operation time, and a shorter hospital stay [17]. In addition, it allows rectum preservation and avoids the risk of a stoma.
A complete pathologic response rate of 30% after neoadjuvant therapy has been reported in the literature. In addition, Habr-Gama et al. [18] showed that after neoadjuvant chemoradiation, stage 0 rectal cancer is associated with excellent long-term results irrespective of surgical treatment. On this basis, a therapeutic strategy for patients with rectal cancer that includes neoadjuvant treatment and transanal excision or open surgery according to tumor downstaging is an appealing therapeutic algorithm. It could combine mini-invasivity and radicality, avoiding overtreatment for a consistent subset of patients. The choice of two local surgical approaches allows for better results in terms of organ sparing with rectal continence salvage, independently of tumor location.
To our knowledge, we have reported the first experience of TEM and local excision matched as a part of a protocol. However, some considerations should be formulated.
First, in our experience, the use of transanal excision was conditional on the identification of downstaged patients, and we substantially failed to recognize candidates correctly. In this sense, several authors have yet described some difficulties, such as radiation-induced fibrosis that interferes with tumor staging [1–20].
Second, when a local excision was planned, it seemed quite difficult to recognize safely the whole area of the initial tumor. The tumoral mass was reduced; healthy mucosa was regenerated; and a small scar often was the only residue of the initial tumor. Under these conditions, the absence of neoplastic tissue in the surgical margins and in the perirectal fat certainly does not imply that the surgeon performed a radical resection. Moreover, it probably could justify the two cases of salvage surgery in the transanal excision group. In conclusion, only a strict follow-up program can justify a transanal approach, and the patients should always be informed about the possibility of a salvage surgery.
Further studies are needed to identify certain molecular markers of tumoral aggressiveness and responsiveness to presurgical treatment. More effective diagnostic tools are required to identify true complete response patients. Findings have shown positron emission tomography (PET) to be an effective diagnostic instrument for identifying small areas of neoplastic tissue with greater sensitivity than conventional tools [21]. Until these aspects are clarified, the use of transanal treatments should be restricted to highly selected patients that can cooperate with strict follow-up programs.
References
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345: 638–646
Theodoropoulos G, Wise WE, Padmanabhan A, Kerner BA, Taylor CW, Aguilar PS, Khanduja KS (2002) T-level downstaging and complete pathologic response after preoperative chemoradiation for advanced rectal cancer result in decreased recurrence and improved disease-free survival. Dis Colon Rectum 45: 895–903
Cass AW, Million RR, Pfaff WW (1976) Patterns of recurrence following surgery alone for adenocarcinoma of the colon and rectum. Cancer 37: 2861–2865
Joffe J, Gordon PH (1981) Palliative resection for colorectal carcinoma. Dis Colon Rectum 24: 355–360
Esnaola NF, Cantor SB, Johnson ML, Mirza AN, Miller AR, Curley SA, Crane CH, Cleeland CS, Janjan NA, Skibber JM (2002) Pain and quality of life after treatment in patients with locally recurrent rectal cancer. J Clin Oncol 20: 4361–4367
Wiig JN, Tveit KM, Poulsen JP, Olsen DR, Giercksky KE (2002) Preoperative irradiation and surgery for recurrent rectal cancer: will intraoperative radiotherapy (IORT) be of additional benefit? A prospective study. Radiother Oncol 62: 207–213
Ruo L, Tickoo S, Klimstra DS, Minsky BD, Saltz L, Mazumdar M, Paty PB, Wong WD, Larson SM, Cohen AM, Guillem JG (2002) Long-term prognostic significance of extent of rectal cancer response to preoperative radiation and chemotherapy. Ann Surg 236: 75–81
Habr-Gama A, de Souza PM, Ribeiro U Jr, Nadalin W, Gansl R, Sousa AH Jr, Campos FG, Gama-Rodrigues J (1998) Low rectal cancer: impact of radiation and chemotherapy on surgical treatment. Dis Colon Rectum 41: 1087–1096
Marks G, Mohiuddin M, Goldstein SD (1988) Sphincter preservation for cancer of the distal rectum using high-dose preoperative radiation. Int J Radiat Oncol Biol Phys 15: 1065–1068
Bonnen M, Crane C, Vauthey JN, Skibber J, Delclos ME, Rodriguez-Bigas M, Hoff PM, Lin E, Eng C, Wong A, Janjan NA, Feig BW (2004) Long-term results using local excision after preoperative chemoradiation among selected T3 rectal cancer patients. Int J Radiat Oncol Biol Phys. 60(4): 1098–1105 Nov 15
Ruo L, Guillem JG, Minsky BD, Quan SH, Paty PB, Cohen AM (2002) Preoperative radiation with or without chemotherapy and full-thickness transanal excision for selected T2 and T3 distal rectal cancers. Int J Colorectal Dis 17: 54–58
Schell SR, Zlotecki RA, Mendenhall WM, Marsh RW, Vauthey JN, Copeland EM III (2002) Transanal excision of locally advanced rectal cancers downstaged using neoadjuvant chemoradiotherapy. J Am Coll Surg 194: 584–590, discussion 590–591
Kim CJ, Yeatman TJ, Coppola D, Trotti A, Williams B, Barthel JS, Dinwoodie W, Karl RC, Marcet J (2001) Local excision of T2 and T3 rectal cancers after downstaging chemoradiation. Ann Surg 234: 352–358, discussion 358–359
Lezoche E, Guerrieri M, Paganini AM, D’Ambrosio G, Baldarelli M, Lezoche G, Feliciotti F, De Sanctis A (2005) Transanal endoscopic versus total mesorectal laparoscopic resections of T2-N0 low rectal cancers after neoadjuvant treatment: a prospective randomized trial with a 3-years minimum follow-up period. Surg Endosc 19(6): 754–756
Valentini V, Coco C, Cellini N, Picciocchi A, Rosetto ME, Mantini G, Marmiroli L, Barbaro B, Cogliandolo S, Nuzzo G, Tedesco M, Ambesi-Impiombato F, Cosimelli M, Rotman M (1999) Preoperative chemoradiation with cisplatin and 5-fluorouracil for extraperitoneal T3 rectal cancer: acute toxicity, tumor response, sphincter preservation. Int J Radiat Oncol Biol Phys 45: 1175–1184
Buess G, Hutterer F, Theiss J, Bobel M, Isselhard W, Pichlmaier H (1984) A system for a transanal endoscopic rectum operation. Chirurg 55: 677–680
Winde G, Nottberg H, Keller R, Schmid KW, Bunte H (1996) Surgical cure for early rectal carcinomas (T1): transanal endoscopic microsurgery vs anterior resection. Dis Colon Rectum 39: 969–976
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr, Silva e Sousa AH Jr, Campos FG, Kiss DR, Gama-Rodrigues J (2004) Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg 240: 711–717
Gavioli M, Bagni A, Piccagli I, Fundaro S, Natalini G (2000) Usefulness of endorectal ultrasound after preoperative radiotherapy in rectal cancer: comparison between sonographic and histopathologic changes. Dis Colon Rectum 43: 1075–1083
Kahn H, Alexander A, Rakinic J, Nagle D, Fry R (1997) Preoperative staging of irradiated rectal cancers using digital rectal examination, computed tomography, endorectal ultrasound, and magnetic resonance imaging does not accurately predict T0,N0 pathology. Dis Colon Rectum 40: 140–144
Calvo FA, Domper M, Matute R, Martinez-Lazaro R, Arranz JA, Desco M, Alvarez E, Carreras JL (2004) 18F-FDG positron emission tomography staging and restaging in rectal cancer treated with preoperative chemo radiation. Int J Radiot oncol Biol phys 55(2): 528–535
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caricato, M., Borzomati, D., Ausania, F. et al. Complementary use of local excision and transanal endoscopic microsurgery for rectal cancer after neoadjuvant chemoradiation. Surg Endosc 20, 1203–1207 (2006). https://doi.org/10.1007/s00464-005-0567-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0567-x