Abstract
Background
The goal of this study was to examine the safety and feasibility of laparoscopic myomectomy (LM) for the management of symptomatic intramural uterine fibroids with weight greater than 80 g as compared to those less than 80 g.
Methods
In a prospective comparative study, 176 women with symptomatic uterine fibroids were scheduled for LM. They were divided into two groups, one with main uterine fibroid (intramural type) weight greater than 80 g and the other with fibroid weight less than 80 g. Outcome measures for the two groups were studied in terms of operation time, amount of blood loss, requirement of blood transfusion, and length of hospital stay.
Result
Operation time and amount of blood loss were significantly greater in the group with fibroid ≥ 80 g than in the group <80 g (121.5 ± 58.9 min versus 79.1 ± 28.6 min, p < 0.001; and 346.3 ± 299.6 ml versus 123.0 ± 89.7 ml, p < 0.001, respectively). However, there was no difference in the length of hospital stay and overall incidence of operative complications between these two groups. None of the women had any major complications. Nevertheless, 11 minor complications were noted, including two pelvic abscesses requiring a second laparoscopic treatment. There was no incidence of switching to laparatomy during the operation. Extreme intraoperative hemorrhage of more than 1000 ml occurred in 8 patients; however, all progressed to full recovery after blood transfusion. Rate of blood transfusion was significantly lower in the group with fibroid <80 g (3.2% versus 22.1%, p < 0.001).
Conclusions
Despite the increased operation time and blood loss, LM can be safely performed in the treatment of large uterine fibroid. However, high risk of blood transfusion in these patients has to be kept in mind.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Myomectomy, as an alternative treatment of symptomatic uterine fibroids, could avoid unnecessary hysterectomy and simultaneously preserve fertility. With the development of operative laparoscopy during the last two decades, a number of gynecologic problems have been resolved by this technique. Laparoscopic myomectomy (LM) is considered one of the major breakthroughs. However, it involves the repair of myometrium and removal of myoma from the abdomen and thus it requires more technical skill than many other laparoscopic procedures. Hence, it is a challenging surgical procedure for gynecologists and is relatively time-consuming that could result in greater blood loss than the traditional open procedure. To date, the only indications for LM are pedunculated and subserosal lesions [8].
Although laparoscopic technique for subserous and even intramural fibroids has been described, and the efficacy of LM was confirmed [2–4, 10, 11], laparoscopic management of large or deep intramural lesions is still controversial. There are very few articles discussing the use of laparoscopy in the removal of large intramural uterine fibroid in the English literature [13].
The difficulty in using laparoscopy in the management of a large fibroid results from the relatively limited operating field, the poor approaching angle of laparoscopic instruments, and the removal of the surgical specimen, all of which have been well documented. Taken together, these limitations increase the intricacy of laparoscopic excision of a large uterine fibroid. As a consequence, surgical morbidity may increase due to the prolonged manipulation. In view of such risks, the relative safety and feasibility of laparoscopic approach over conventional laparotomy may raise serious concerns. To shed light on this problem, we prospectively investigated the outcome of LM in the treatment of large uterine intramural fibroids. The average uterine weight of a parous woman is 80 g or more [5], and 80 g was taken as a cut-off value to define a large fibroid in this study.
Materials and methods
From January 2000 through December 2002, patients scheduled to undergo LM performed by one of the authors (C.J.W.) at Chang Gung Memorial Hospital were recruited for participation in this study. The indications for LM in these patients included menorrhagia, abdominal pain, bulk-related symptoms (urine frequency, or rectosigmoid compression), and infertility. Before the operation, the patients were informed of the risks and benefits of laparoscopic myomectomy, including the potential need to switch to laparotomy during the operation and the risks of intraoperative bleeding, transfusion, and adhesion. Written informed consent forms were obtained from all subjects.
Prior to the surgery, all patients underwent preoperative assessments, including detailed medical history, pelvic examination, and ultrasonography. Women with dominant fibroid size greater than 4 cm and fibroids of the intramural type were included, as were those with multiple fibroids. Women with no prior sexual activity and those in whom a surgical specimen had to be removed from the abdomen were excluded. Before operation, all patients received prophylactic antibiotics.
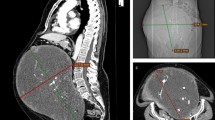
The procedure was conducted with the patient in the dorsolithotomy Trendelenburg position with both legs protected by elastic bandages; a Foley catheter was inserted for constant urinary drainage. A uterine manipulator was placed into the uterus. Videolaparoscopy was performed with a 10-mm principal trocar introduced through the umbilicus. Two ancillary cannulas were placed under laparoscopic visualization: one 5-mm cannula in the right lower quadrant lateral to the inferior epigastric arteries and one 5-mm cannula in the left lower quadrant. For the patients with uterine size greater than 14 weeks’ gestation, a 1-cm vertical skin incision was made with a number 11 blade at the midpoint between the umbilicus and the xyphoid process (Lee-Huang point) [6] where a 10-mm principal cannula was inserted. Two puncture sites, one 5 mm and the other 5 mm, were made in the lower abdomen at the paramedian line at the level of the umbilicus. If more portal sites were needed, other cannulas were introduced at the paramedian line, just above the pubic hairline. Once cannula placement was complete, adhesions were lysed as necessary.
After identifying the location of all fibroids, a transverse incision was made on the serosa overlying the largest tumor using a unipolar electrode. The incision was extended into the pseudocapsule down to the characteristically pearly white substance of the tumor. Additional fibroids located at the same area were removed through the same incision. However, for nonadjacent fibroids, creating a new incision was necessary. A myoma screw or second puncture was then inserted into the fibroid to apply traction while a probe (or any instrument that functions as a probe) was used to bluntly dissect in the cleavage plane to leverage the tumor against the uterine wall and pry it out of its bed. The unipolar electrode was used to dissect pseudocapsule attachments further. Vessels were electrocoagulated by Kleppinger forceps before being cut. After fibroid removal, the uterine defect was irrigated. Bleeding points were identified and controlled with electrocoagulation.
The uterine surgical defect was closed in layers. If excessive myometrium and serosa were present, these were trimmed off. Using a 0 monofilament poliglecaprone 25 (Monocryl, Ethicon Inc, Somerville, NJ) on a large curved needle to make a deep and wide (1 cm from the cut edge of the incision) bite. An original 90 cm suture line would be trimmed to 30 cm long for the sake of carrying out continuous suturing inside the peritoneal cavity freely. Entering the uterus with a needle throughout the serosa to the myoma bed and emerging at the superficial level in a U shape, the needle was then grasped and reapplied in a reverse fashion. Intracorporeal knot tying was used at that time. A continuous non-running-lock suture with 1-cm increments was then carried out, with each suture penetrating the full thickness of the myometrium, following a method similar to that applied during laparotomy.
Specimens were removed through posterior colpotomy: a wet sponge on ring forceps was inserted behind the cervix to distend the top of the posterior vagina. Unipolar scissors were used to make a transverse colpotomy incision. Excised fibroids were stored in the posterior cul-de-sac. After completing these procedures, the CO2 insufflator and videolaparoscopic system were turned off temporarily, after which the colpotomy incision was extended laterally by digital pressure. A long Heaney retractor was placed into the posterior cul-de-sac, where it was used to depress the rectum. The fibroids were then grasped directly with a tenaculum. Medium and large fibroids were morcellated with a scalpel or scissors so that they could be removed from the pelvis. After removal of all fibroids, the colpotomy incision was closed with 2-O polyglycolic acid suture. Pneumoperitoneum was re-established at this time, and the peritoneal cavity was irrigated and lavaged until fluid was clear. A suction drain (Jackson-Pratt drain) was introduced through a 5-mm access site if indicated. If the specimen had to be removed from the abdominal wall, a 12-mm electromechanical morcellator (Storz, Tuttlingen, Germany) was used to ease extraction of the specimen. All port sites were sutured with 3-O polyglycolic acid suture at the level of the fascia to prevent herniation. The skin was approximated by sterile adhesive tape.
Statistics
Descriptive statistics (mean ± SD, range, percentage) were used to summarize patient demographics and operation results. Continuous variables were compared with Student’s t-test and categorical values with Pearson χ2 analysis and Fisher’s exact test. All probability values were two-sided. Significance was accepted at probability below 5%. SPSS for Windows version 9.0 (SPSS Inc., Chicago, IL) was used for the statistical calculations.
Results
A total of 506 women underwent LM during the study period, and 302 of them were included into the protocol. Only 176 women had a main fibroid of the intramural type. Among them, 63 had a main uterine fibroid weighing <80 g, and 113 others had one weighing ≥80 g. The characteristics of the patients are summarized in Table 1. The two groups were similar in terms of age, body weight, and history of cesarean section. The history of vaginal delivery was significantly lower in the ≥80 g group.
The indications for LM for the patients are listed in Table 2. Nine patients in the ≥80 g group and seven in the <80 g group underwent concomitant adnexal surgery, and 15 patients in the ≥80 g group and nine patients in the <80 g group required lysis of minimal to mild pelvic adhesion. In addition, there was one patient in the <80 g group undergoing Güillian suspension for the correction of retroverted uterus. No additional procedure was performed in any of the other patients.
The outcomes for the two groups are summarized in Table 3. The duration of operation, mean amount of blood loss, and requirement of blood transfusion were significantly less for the <80 g group than for the ≥80 g group. Eight patients suffered from intraoperative blood loss of more than 1000 ml; all of them belonged to the ≥80 g group. The extreme blood loss was mainly caused by bleeding during multiple uterine incisions for the removal of more than three fibroids in four patients (3 in one patient, 7 in one patient, and 8 in two patients), and a solitary huge fibroid larger than 10 cm in four patients (10, 10, 11, and 12 cm). All these patients recovered fully after blood transfusion with two to six units of whole blood and/or two to six units of packed red blood cells and antibiotic therapy with cefamezine 1 g every 6 h for 2 days.
The duration of hospital stay and overall complication rate were similar in the two groups. No major complications, such as ureter injuries, bladder injury, or bowel injury occurred in any of the cases. Two patients in the ≥80 g group experienced postoperative ileus. The condition lasted for 3 days and spontaneously subsided after flatus passage. Three patients developed low-grade fever (<38.5°C), all in the ≥80 g group. They made full recovery after fluid challenge and antibiotic therapy with cefamezine 1 g every 6 h and gentamicin 60 mg administered every 8 h for 3 days. Two patients developed urinary tract infection, one in each group. Both of them recovered fully after infusion of cefamezine 1 g every 6 h for 3 days. Two patients in the ≥80 g group developed uterine hematoma. Both of them received oral cephalosporin 500 g every 6 h for 7 days, and the hematoma regressed, as confirmed by ultrasound 3 months postoperatively. Two other patients were readmitted and required further treatment due to abscess formation and oozing at myomectomy site on postoperative day 5, one in each group. Both of them were treated with laparoscopy uneventfully. A morcellator was used for the removal of fibroids in 28 patients, two in the <80 g group, and 26 in the ≥80 g group. In all other cases the specimens were removed from vagina smoothly.
Twenty-six of the 176 patients in this study attempted to conceive, and 10 pregnancies were achieved in 7 patients. The time interval between surgery and the first pregnancy ranged between 1 and 12 months (mean: 6 months). All pregnant courses were uneventful, and spontaneous uterine rupture did not occur at any delivery. Vaginal delivery occurred in two women (3 pregnancies), and 5 (7 pregnancies) underwent cesarean section. Adhesions were noted at the site of myomectomy in 2 patients who underwent cesarean section.
Discussion
Since Semm [12] first reported laparoscopic myomectomy with vaginal extraction, LM has become a mature surgical technique and is commonly employed by gynecologic laparoscopists for their patients who meet the treatment criteria. Laparoscopic myomectomy has a better cosmetic effect and faster recovery than the abdominal approach. However, surgeons might have greater potential risks in dealing with large fibroids; for example, protracted procedure and potential surgical complications might challenge the surgeon’s operative skills and patience. No clear-cut definition has been put forth to demonstrate how big a uterine fibroid should be considered a limitation for LM.
Three major concerns regarding the execution of LM are as follows: the removal of large fibroids out of the abdomen, the repair of the uterine incision, and the control of operative blood loss. First, removal of fibroids out of the abdomen can be via a trans-abdominal or trans-vaginal route. In this regard, removal of specimen via posterior colpotomy is a merited in laparoscopic procedures associated with good cosmetic result and rapid recovery; however, potential ascending infection might occur and parenteral antibiotic infusion postoperatively will be indicated. Although portal extension combining with fibroid slicing can be useful in removing the specimens [9], the 2- to 4-cm extension of the incision is associated with higher postoperative pain, which decreases its practical application. Introduction of a more efficient power morcellator has made removal easier [1]. In this study, we spent an average of 30 min to remove fibroids weighing 300 g or more transvaginally; meanwhile, only 15 min was required when we used power morcellator.
Second, the repair of the uterine incision is important not only because it is a method of hemostasis but also it decides the integrity of the myometrium. Moreover, it also influences the postoperative adhesion formation. In laparotomy, the conventional uterine closure is done in two to three layers, decreasing the potential for uterine dehiscence, fistula, and adhesion formation. Nevertheless, this maneuver is difficult to be done laparoscopically. In cases where the defect is deep or large, the excessive myometrium and serosa should be trimmed off, after which a large curved needle should be used to take a deep and wide bite in one layer for the repair of the defect. A continuous non-running-lock suture with 1-cm increments enhances the strength of the uterine wall, similar to the sutures that are used in cesarean delivery. Adherence to these closure principles will reduce the frequency of uterine dehiscence and the likelihood of hematoma formation deep inside the myometrium.
Lastly, significant blood loss requiring blood transfusion still remains a major complication in the removal of large fibroids; therefore several precautions need to be taken to decrease intraoperative blood loss. First, oxytocin infusion should begin in the operating room immediately after anesthesia is initiated. In this way, uterine contraction will be induced, and uterine perfusion can be simultaneously reduced, decreasing the blood bulk within the uterus would be decreased [14]. Second, bilateral uterine artery ligation before myomectomy can decrease the chance of massive intraoperative blood loss [7]. Third, gonadotropin-releasing hormone (GnRH) agonists may be administered before the commencement of myomectomy. In this regard, the GnRH agonist could reduce the size of the fibroids significantly [15]. In spite of their usefulness, none of these methods were used in the present study; they can be helpful means of controlling bleeding in the future.
Another issue of concern is where to put the trocars and how to handle the instruments smoothly without the hindrance of the large uterus. Focusing on this problem, we can place the main trocar midway between the xyphoid process and the umbilicus and the accessory trocars lateral to umbilicus [6]. By making this modification, a larger intraperitoneal manipulation space can be achieved without interference from the uterus.
In conclusion, in view of the rapid progress and technical advancements in laparoscopy in the last two decades, we tend to overemphasize its benefits while neglecting potential drawbacks. The role of LM in dealing with large intramural fibroids needs to be evaluated and studied in greater depth. In this study, the procedure has been shown to be more time consuming, and the incidences of blood transfusion was greater in the ≥ 80 g group than in the <80 g group. However, the complication rate and duration of hospital stay were similar in these two groups. Most important, the data indicate that fibroids with an average weight of 200 g could be safely and effectively removed by laparoscopic techniques. The findings in this study should be considered preliminary at this time, and further randomized and prospective studies are necessary.
References
Carter JE, McCarus SD (1997) Laparoscopic myomectomy. Time and cost analysis of power vs. manual morcellation. J Reprod Med 42: 383–388
Donnez J, Mathieu PE, Bassil S, Smets M, Nisolle M, Berliere M (1996) Laparoscopic myomectomy today. Fibroids: management and treatment: the state of the art. Hum Reprod 11: 1837–1840
Dubuisson JB, Chapron C, Fauconnier A (1997) Laparoscopic myomectomy. Operative technique and results. Ann N Y Acad Sci 828: 326–331
Hasson HM, Rotman C, Rana N, Sistos F, Dmowski WP (1992) Laparoscopic myomectomy. Obstet Gynecol 80: 884–888
Langlois PL (1970) The size of the normal uterus. J Reprod Med 4: 220–228
Lee CL, Huang KG, Jain S, Wang CJ, Yen CF, Soong YK (2001) A new portal for gynecologic laparoscopy. J Am Assoc Gynecol Laparosc 8: 147–150
Liu WM, Tzeng CR, Yi-Jen C, Wang PH (2004) Combining the uterine depletion procedure and myomectomy may be useful for treating symptomatic fibroids. Fertil Steril 82: 205–210
Munro MG, Brill AI (2002) Gynecologic endoscopy. In Berek JS, Hillard PJA, Adashi EY (eds). Novak’s Gynecology, 13th edition. Baltimore, Lippincott Williams & Wilkins, p 714
2Nezhat C, Nezhat F, Bess O, Nezhat CH, Mashiach R (1994) Laparoscopically assisted myomectomy: a report of a new technique in 57 cases. Int J Fertil Menopausal Stud 39: 39–44
Nezhat C, Nezhat F, Silfen SL, Schaffer N, Evans D (1991) Laparoscopic myomectomy. Int J Fertil 36: 275–280
Seinera P, Arisio R, Decko A, Farina C, Crana F (1997) Laparoscopic myomectomy: indications, surgical technique and complications. Hum Reprod 12: 1927–1930
Semm K (1979) New methods of pelviscopy (gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy and adnectomy. Endoscopy 11: 85–93
Sinha R, Hegde A, Warty N, Patil N (2003) Laparoscopic excision of very large myomas. J Am Assoc Gynecol Laparosc 10: 461–468
Wang CJ, Yuen LT, Yen CF, Lee CL, Soong YK (2004) A simplified method to decrease operative blood loss in laparoscopic-assisted vaginal hysterectomy for the large uterus. J Am Assoc Gynecol Laparosc 11: 370–373
Zullo F, Pellicano M, De Stefano R, Zupi E, Mastrantonio P (1998) A prospective randomized study to evaluate leuprolide acetate treatment before laparoscopic myomectomy: efficacy and ultrasonographic predictors. Am J Obstet Gynecol 178: 108–112
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, C.J., Yuen, L.T., Lee, C.L. et al. Laparoscopic myomectomy for large uterine fibroids. Surg Endosc 20, 1427–1430 (2006). https://doi.org/10.1007/s00464-005-0509-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0509-7