Abstract
Background
The phenomenal progress of minimally invasive surgery has imparted its influence on conventional esophagectomy. Currently, more esophagectomies are being performed by laparoscopic and/or thoracoscopic methods. Esophagogastrectomy for the adenocarcinoma of the gastroesophageal (GE) junction has been a conventional treatment. The literature is limited regarding the laparoscopic approach to esophagogastrectomy. The aim of this study was to evaluate the outcome of laparoscopic esophagogastrectomy in the management of adenocarcinoma of the GE junction.
Methods
From January 1997 to February 2005, laparoscopic esophagogastrectomy was performed in 32 patients. Indication for operation was adenocarcinoma of the GE junction in all patients. Neo-adjuvant therapy was used in two patients (6.88%) only. Initially, our approach to intrathoracic anastomosis without thoracic and cervical access was to introduce the anvil of circular stapler through minilaparotomy incision (n = 22), but later we switched to trans-oral placement of anvil into the distal end of the esophagus (n = 10).
Results
There were 22 men and 10 women. Median age was 61.8 years (range, 39–72). There was no conversion. The laparoscopic esophagogastrectomy was completed in all patients. The pyloromyotomy and feeding jejunostomy were performed in all cases. The median intensive care unit stay was 1 day (range, 1–28); hospital stay was 7 days (range, 5–42). Mean estimated blood loss and mean operative time were 150 ml and 200 min, respectively. At mean follow-up of 14 months (range, 2–40), stage-specific survival was similar to that of other series.
Conclusion
In selected cases of adenocarcinoma of the GE junction, laparoscopic esophagogastrectomy offers as good as or better results than open operation in our institution with extensive advance endoscopic and open experience. This study shows that laparoscopic esophagogastrectomy has potential to meet oncologic criteria of clearance and provide the benefits of minimally invasive surgery as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The search for a safe and less traumatic method of removing the esophagus has been an ongoing challenge [4]. Due to the development of minimally invasive approaches to esophageal diseases and a better understanding of the biological behavior of the adenocarcinoma of the esophagus, several approaches have been described for minimally invasive esophagectomy, including thoracoscopic [3], thoracolaparoscopic [11], video mediastinoscopic [1], and totally laparoscopic approaches [4]. The changing histological findings of esophageal cancer point toward a higher incidence of adenocarcinoma of the esophagus during the past 20 years [7]. The adenocarcinoma of the cardia and gastroesophageal (GE) junction has traditionally been managed by total esophagectomy, subtotal esophagectomy by the Ivor–Lewis approach, and esophagogastrectomy. A few studies have described the laparoscopic approach to esophagogastrectomy [2, 15], but experience is very limited. The higher incidence of adenocarcinoma of the cardia and GE junction has placed greater responsibility on minimal access oncologic surgeons to explore newer approaches to esophagogastrectomy and to modify the existing technique to provide the best care to their patients.
We describe our technique of laparoscopic esophagogastrectomy with intrathoracic anastomosis without thoracic or cervical access. This technique has the potential to satisfy the oncological principles and also to provide the benefits of minimal access surgery.
Materials and methods
Patient population
We stored our data prospectively in an institutional review board-approved database that was analyzed at the end of the study. From January 1997 to February 2005, we performed laparoscopic esophagogastrectomy in 32 patients—22 males and 10 females, with a mean age of 61.8 years (range, 39–72). The primary criterion for inclusion in this study was resectable and histologically proven adenocarcinoma of the cardia and GE junction (Siewert and Stein classification [19]) in patients fit for operation. All patients were evaluated and staged by preoperative CT scan of the chest and abdomen and by upper gastrointestinal endoscopy. In the first 22 patients, we used the transabdominal approach to place the anvil of the circular stapler. We switched to transoral placement of the circular stapler anvil in the next 10 patients. Informed consent was obtained from all patients.
Operative technique
This operation is performed by a single team in two stages. The operating surgeon stands between the legs of the patients. The monitor and laparoscopic cart are kept at the head end of the patient and the surgeon with the camera stands on the right side of the patient. The second assistant surgeon and assisting staff nurse stand on the left side of the patient.
The patient is intubated with a single-lumen endotracheal tube for general anesthesia and is kept in the modified Lloyd–Davis with 20–30° reverse Trendelenberg position. Both lower limbs are placed in soft and padded stirrups and graduated elastic stocking are applied.
Stage 1: Mobilization of the esophagus and the stomach
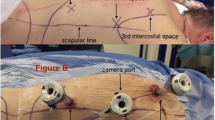
The pneumoperitoneum is established with a Veress needle. A total of five ports are used for laparoscopic access. Placement of the ports is as follows:
-
1.
Supraumbilical (3–5 cm above the umbilicus) 10-mm port for 30° optics
-
2.
Subxiphoid or epigastric 5-mm port for liver retraction
-
3.
Right midclavicular subcostal 5-mm port for left-hand working instrument (e.g., grasping)
-
4.
Left midclavicular subcostal 10-mm port for right-hand working instruments (e.g., dissection, cutting, clipping, and harmonic shears)
-
5.
Left anterior axillary 5- or 10-mm port at the level of the umbilicus for gastric retraction.
A thorough general survey is done after ports are introduced under vision. The left lobe of the liver is retracted anteriorly with the instrument from the epigastric port. The lesser omentum is incised close to hepatic attachment from the first part of the duodenum to the cardia. All lymph nodes and fatty tissue are cleared from the celiac axis origin toward the left gastric pedicle. Complete nodal clearance is achieved at the origin of the common hepatic artery and splenic artery. The left gastric artery and vein are individually ligated with silk ligature or clipped and divided. Using 10-mm Babcock forceps, the entire stomach is lifted during this maneuver to achieve adequate exposure. Starting from the anterior arcuate ligament, the entire soft tissue is dissected anteriorly along the right and left crura. Using a 30° scope, the dissection becomes easier and the entire growth is lifted by blunt and harmonic shears dissection. The infiltrated part of the crura is also excised with growth en bloc, if involved. Then the posterior mediastinum is entered, and care is taken to identify and protect the pleura.
The next step is to divide the gastrocolic omentum between the stomach and the transverse colon, saving the right arteries and vascular arcade. Further proximal dissection divides the gastrosplenic omentum and the short gastric vessels. The gastric fundus is dissected from the superior pole of the spleen. The pancreaticogastric ligament is divided. During this step, the posterior vagus nerve is also divided. The attachments between the posterior wall of the stomach and pancreas are divided up to the first part of the duodenum.
Next, the lower end of the esophagus is mobilized circumferentially through the hiatus and an adequate margin of the esophagus, approximately 5 cm proximal to growth, is dissected. A 10-mm Babcock forceps is used for retracting the fundus caudally, which aids in mediastinal dissection of the esophagus as well as in mediastinal lymph nodal clearance achieved by 5-mm harmonic shears. The looping of the GE junction by umbilical tape is avoided to prevent tumor spill. During the mediastinal dissection, the lymph nodes and soft tissue are dissected, protecting the mediastinal pleura on either side. After identifying the site of division of the esophagus (in situ flexible endoscope may be used), stay sutures are applied proximally. The anterior wall of the esophagus is transected first using a 5-mm curved harmonic shear. Pursestring suture is applied sequentially to the cut end of the anterior wall of the esophagus to secure the anvil. Similarly, the posterior wall is transected and pursestring suture is completed. Then we proceed to the second stage of the procedure.
Stage 2: Resection of specimen and creation of mediastinal esophagogastric anastamosis
A minilaparotomy is performed by extending the supraumbilical port and the distal tumor-bearing esophagus with stomach is delivered out using a plastic sheath to protect the wound in order to prevent port site metastasis. The proximal stomach is transected with a 5-cm distal margin from the gross tumor using a TLC 55 linear cutter stapler (Ethicon Endo-Surgery). Pyloromyotomy is performed at this stage to avoid gastric stasis. Then, anterior gastrotomy is performed to accommodate the circular stapler. The anvil is introduced into the abdominal cavity after applying silk suture to its rod. The stomach is placed back in the peritoneal cavity. Minilaparotomy is closed with polypropylene sutures and a camera port is re-created. The left midclavicular trocar is removed, the skin incision is extended, and the circular stapler is inserted into the peritoneal cavity after adequate dilatation of the port site. One or two stitches may be placed on the rectus sheath to prevent gas leak. The anvil is introduced into the proximal esophagus and the pursestring is tied securely. The silk applied to the anvil’s central port plastic cap is used to pull the rod out of the esophagus. The anvil can be introduced into the esophagus via (1) minilaparotomy or (2) through the tran-oral route using EEA 25 (Autosuture) after dismantling the spring and flap of the anvil or the CDH21 anvil (Ethicon Endo-Surgery) in toto and using Ryle’s tube to attach the anvil rod and pass the whole assembly to the distal esophagus, transected (Fig. 1) with ETS-FLEX 45 (Ethicon Endo-Surgery), and retrieve the anvil after making a hole at the cut end by harmonic shears. The stomach is kept stretched using Babcock forceps in the lower abdomen. The shaft is introduced into the stomach through a gastrotomy (Fig. 2). The stapler rod is rotated to pierce the stapled line on the stomach. The Babcock forceps in the right midclavicular port is used to handle the stapler and to give thrust proximally. The grasper in the left anterior axillary port is used to give traction to the anvil (Fig. 3). This maneuver is highly effective in docking the central rod to the anvil. End-to-end intrathoracic esophagogastrostomy is formed by firing the stapler from outside (Fig. 4). The stapler is removed and do-nuts are checked. The anastomosis is checked by methylene blue instillation. The gastrotomy is closed using single-layer continuous extramucosal sutures. The anastomosis is checked by insufflating the segment with air or methylene blue. A few reinforcing stitches are placed if necessary. A nasogastric tube is passed into the stomach under laparoscopic guidance. A sump drainage tube is placed near the anastomotic site.
A feeding jejunostomy tube is placed laparoscopically by first attaching a limb of the proximal jejunum (approximately 25 cm distal to the ligament of Treitz) with endosuturing. A 5-mm trocar is placed close to the attached jejunal loop and a 12-Fr silicone feeding tube is introduced into the attached jejunal loop through a hole created with harmonic shears. The entry site of the feeding tube is tied with a pursestring suture and the jejunal loop is further tacked to the abdominal wall to seal the feeding tube entry site.
Results
Of the 32 patients, 22 were male (68.75%) and 10 were female (31.25%), with a mean age of 61.8 years (range, 39–72). Preoperative indication for operation was adenocarcinoma of the GE junction in all patients. Neoadjuvant therapy was used in two patients (6.88%). All procedures were performed at the GEM Hospital. All operations were performed by a single surgeon (C.P.). There was no history of previous abdominal surgery in any of the patients. Pyloromyotomy was performed in all patients. A laparoscopic feeding jejunostomy was placed in all patients at the end of the procedure. There was no conversion to the open approach. Two-field lymphadenectomy was performed in all patients. A mean of 15 lymph nodes were harvested (range, 9–32). Mean operative time was 200 min (range, 180–310). The mean estimated blood loss was 150 ml (range, 50–700). The median intensive care unit stay was 1 day (range, 1–28), time to oral intake was 4 days (range, 3–25), and hospital stay was 7 days (range, 5–42).
There was no 30-day postoperative mortality. Postoperative morbidity included anastomotic leak in one patient, and two patients had delayed gastric emptying. Anastomotic leak was confirmed radiologically and was managed conservatively. Of the two patients who developed regurgitation from delayed gastric emptying, one was managed with oral erythromycin. Another patient required nasogastric suction and prolonged hospitalization. The median follow-up was 14 months (range, 2–40). The 3-year survival for stages I, IIa, IIb, and III was 62, 42, 46, and 15%, respectively.
Discussion
Esophageal resection for esophageal cancer continues to be a technical tour de force for the surgeon because of the technical difficulties involved in the procedure and aggressive biological behavior of the tumor, with consequent high morbidity and mortality. Traditionally, the left transthoracic or thoracoabdominal approach, as described by Oshawa [16] and Marshall [12], was preferred by many surgeons for the treatment of esophageal carcinoma of the lower third and cardia [4]. The Ivor–Lewis approach is another landmark in esophageal resection, and it is used when a sizeable amount of stomach needs to be resected to achieve tumor-free margin in the treatment of cancer of the cardia and GE junction cancer. Due to violation of the thoracic cavity, morbidity and mortality continued to be high.
Esophagogastrectomy without thoracotomy represents an excellent surgical option in the treatment of adenocarcinoma of the GE junction. The advantages of the transhiatal approach include no patient repositioning and no need for single lung ventilation [1]. For adenocarcinoma of the distal esophagus and cardia, tumor multicentricity is not a problem, and the proximal dissection can be limited to 5 cm above the gross level of the tumor [5, 8]. This concept led to the development of esophagogastrectomy. Due to progress in the field of minimal access surgery, laparoscopic esophagogastrectomy is now being reported. The number of patients studied is very small. Nguyen et al. [15] reported one case of laparoscopic esophagogastrectomy, and Costi et al. [2] reported three cases.
Laparoscopic transhiatal esophagectomy was first described by DePaula et al. [4] from Brazil in a series that included many patients with end-stage achalasia from Chagas’ disease and one patient had adenocarcinoma of the lower third of the esophagus. Swanstrom et al. [20] reported totally laparoscopic esophagectomy in nine patients. Both groups described the laparoscopic transhiatal approach to esophagectomy. Watson et al. [21] first described totally endoscopic Ivor–Lewis esophagectomy. Nguyen et al. [13] also reported minimally invasive Ivor–Lewis esophagectomy. Laparoscope allows safe dissection of the esophagus transhiatally up to the level of the inferior pulmonary vein and, in expert hands, up to the carina. Combining the laparoscopic mobilization of the stomach, laparoscopic esophagogastrectomy provides the least invasive approach to the management of adenocarcinoma of the GE junction without compromising oncologic principles. Since 1997, we have been performing minimally invasive esophagectomy for esophageal carcinoma and selecting laparoscopic esophagogastrectomy for GE junction adenocarcinoma. We reported intrathoracic stapled anastomosis of the esophagus to the stomach in 2002 [17]. Costi et al. [2] reported three cases of this procedure without any intraoperative or postoperative complications. In their series, the mean operative time was 347 min and mean blood loss was 360 ml. The mean postoperative stay was 9 days. Luketich et al. [10] reported the largest series of 222 patients undergoing minimally invasive esophagectomy. The 3-year survival for our stage I, IIa, IIb, and III patients was similar to that of their series. Rizk et al. [18] studied the impact of complications on outcomes after resection for esophageal and GE junction carcinoma. They found that of 510 patients studied, 27% had complications directly attributable to surgical technique, such as an anastomotic leak, a paralyzed vocal cord, or chylothorax. They also found that technical complications have a major negative impact on survival after esophagogastrectomy for cancer. Ellis et al. [6] reviewed the results of 408 open esophagogastrectomies in the treatment of cardial carcinoma and found that 30-day postoperative mortality was 2.5%, with additional in-hospital mortality of 1.2%; 30.7% of patients had complications, of which 18% were major. Only one report has compared open esophagectomy with minimally invasive esophagectomy [14]. This study favored minimally invasive esophagectomy due to shorter operating time, reduced blood loss, and reduced intensive care unit and hospital stay in this group. There have been concerns regarding the adequacy of surgical margins, adequacy of lymphadenectomy, and port site tumor implant in laparoscopic procedures for cancer [9]. Tactile identification of the tumor during open surgery ensures an adequate margin of resection, which is lost in laparoscopic surgery. Intraoperative endoscopy adequately delineates the proximal and distal margin. In our series, all margins of resection were tumor free. We performed a limited two-field lymphadenectomy including mediastinal and upper abdominal (celiac and hepatic pedicle) lymph nodes, and the mean number of lymph nodes harvested in our series was 15. From our experience, laparoscopy provides an excellent view of the posterior mediastinum after esophageal hiatal dissection. We adhered to all surgical principles to avoid port site recurrence. The majority of our cases harbored bulky tumors, and minilaparotomy of 3 or 4 cm provided adequate access to deliver the specimen. The specimen was placed in a protective bag to prevent direct contact of the tumor with the surgical wound. During a mean follow-up of 14 months, we did not observe any wound or port site recurrence. Seven of 32 patients with adenocarcinoma of the GE junction developed metastatic disease.
The low morbidity and 3-year survival rate in our study compare favorably with those observed for open esophagogastrectomy. A major disadvantage of laparoscopic esophagogastrectomy, as with all other advanced laparoscopic procedures, is the steep learning curve.
Esophagogastrectomy has been accepted as a treatment of choice for adenocarcinoma of the GE junction. Due to the advent of minimally invasive surgery, laparoscopic esophagogastrectomy is being increasingly reported. Conceptually, it provides all the benefits of minimally invasive surgery and fulfills the oncologic criteria of clearance. We recommend this procedure for skilled hands only, and we predict that it may replace conventional surgery for the treatment of adenocarcinoma of the GE junction. Standardization of the technique and long-term outcome data from randomized, prospective, controlled, and multiinstitutional studies are needed.
References
Bonavina L, Incarbone R, Bona D, Peracchia A (2004) Esophagectomy via laparoscopy and transmediastinal endodissection. J Laparoendosc Adv Surg Tech A 14: 13–16
Costi R, Himpens J, Bruyns J, Cadiere GB (2004) Totally laparoscopic transhiatal esophago-gastrectomy without thoracic or cervical access. The least invasive surgery for adenocarcinoma of the cardia? Surg Endosc 18: 629–632
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37: 7–11
DePaula AL, Hashiba K, Ferreira EA, de Paula RA, Grecco E (1995) Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc 5: 1–5
Ellis FH Jr, Gibb SP, Watkins E Jr (1988) Limited esophagogastrectomy for carcinoma of the cardia. Indications, technique, and results. Ann Surg 208: 354–361
Ellis FH Jr, Heatley GJ, Krasna MJ, Williamson WA, Balogh K (1997) Esophagogastrectomy for carcinoma of the esophagus and cardia: a comparison of findings and results after standard resection in three consecutive eight-year intervals with improved staging criteria. J Thorac Cardiovasc Surg 113: 836–848
Enzinger PC, Mayer RJ (2003) Esophageal cancer. N Engl J Med 349: 2241–2252
Hennessy TP, Keeling P (1987) Adenocarcinoma of the esophagus and cardia. J Thorac Cardiovasc Surg 94: 64–68
Johnstone PA, Rohde DC, Swartz SE, Fetter JE, Wexner SD (1996) Port site recurrences after laparoscopic and thoracoscopic procedures in malignancy. J Clin Oncol 14: 1950–1956
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, Schauer PR, Close JM, Fernando HC (2003) Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238: 486–495
Luketich JD, Schauer PR, Christie NA, Weigel TL, Raja S, Fernando HC, Keenan RJ, Nguyen NT (2000) Minimally invasive esophagectomy. Ann Thorac Surg 70: 906–912
Marshall (1938) Carcinoma of the esophagus: successful resection of lower end of esophagus with reestablishment of esophageal gastric continuity. Surg Clin North Am 18: 643
Nguyen NT, Follette DM, Lemoine PH, Roberts PF, Goodnight JE Jr (2001) Minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 72: 593–596
Nguyen NT, Follette DM, Wolfe BM, Schneider PD, Roberts P, Goodnight JE Jr (2000) Comparison of minimally invasive esophagectomy with transthoracic and transhiatal esophagectomy. Arch Surg 135: 920–925
Nguyen NT, Roberts P, Follette DM, Rivers R, Wolfe BM (2003) Thoracoscopic and laparoscopic esophagectomy for benign and malignant disease: lessons learned from 46 consecutive procedures. J Am Coll Surg 197: 902–913
Oshawa T (1933) The surgery of the oesophagus. Nippon Geka Hokan 10: 605
Palanivelu C (2002) Laparoscopic esophagogastrectomy. In: Palanivelu C (ed) Textbook of laparoscopic surgery. GEM Foundation, Coimbatore, India, pp 293–300
Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, Brennan MF, Rusch VW (2004) The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 198: 42–50
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85: 1457–1459
Swanstrom LL, Hansen P (1997) Laparoscopic total esophagectomy. Arch Surg 132: 943–949
Watson DI, Davies N, Jamieson GG (1999) Totally endoscopic Ivor Lewis esophagectomy. Surg Endosc 13: 293–297
Acknowledgment
We thank Sister Malalthi Hariharan for providing logistic support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palanivelu, C., Prakash, A., Parthasarathi, R. et al. Laparoscopic esophagogastrectomy without thoracic or cervical access for adenocarcinoma of the gastroesophageal junction. Surg Endosc 21, 16–20 (2007). https://doi.org/10.1007/s00464-005-0418-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0418-9