Abstract
Multiple reports have outlined the potential benefits of the laparoscopic approach to colon surgery. Recently, randomized control trials have demonstrated the safety of applying these techniques to colorectal cancer. This study examined the long-term follow-up assessment of patients after laparoscopic colorectal cancer resections and compared them with a large prospective database of open resections. A total of 231 resections were performed for adenocarcinoma of the colon or rectum between 1992 and 2004. Of these 231 resections, 93 were rectal (40.3%) and 138 were colonic (59.7%). A total of 8 (3.2%) of the resections were performed as emergencies, and 27 (11.7%) were converted to open surgery. The mean follow-up period was 35.84 months (range, 0–132 months). The disease recurred in 51 of the patients (22.1%) before death, involving 14 (6.1%) local and 37 (16%) distant recurrences. Only two patients had wound recurrences (0.8%), and both patients had widespread peritoneal recurrence at the time of diagnosis. The overall survival rate was 65.3% at 60 months and 60.3% at 120 months. The disease-free survival rate was 58% at 60 months and 56% at 120 months. Laparoscopic techniques can be applied to a wide range of colorectal malignancies without sacrificing oncologic results during a long-term follow-up period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic techniques were first applied to colon cancer surgery in 1990 [21]. Multiple reports have outlined the potential benefits of a laparoscopic approach for both benign and malignant [3, 4, 6, 7, 8, 10, 16, 18, 22, 23] colorectal disease. Recently, randomized control trials have demonstrated the safety of using laparoscopic techniques for colon cancer [14, 20]. These trials have used rigorous inclusion criteria and proscribed thresholds for conversion, resulting in relatively high conversion rates [20]. Furthermore, the regions of the transverse colon and the rectum have yet to be fully evaluated in a randomized fashion.
Evaluation of the benefits offered by laparoscopic colorectal resection may be underestimated when the procedure is used in a selective manner. Our center was involved in the prospective randomized evaluation of laparoscopic resection for colon cancer (COST Study) [20]. Since completing accrual for this study, we have offered laparoscopic resection as the primary approach to all patients with colorectal cancer. We have maintained a prospective database since initiating laparoscopic colorectal surgery at our center in 1992.
In this study, we reviewed the results for all the patients in whom a laparoscopic colorectal procedure was attempted for colon or rectal malignancy, with up to 10 years of clinical follow-up assessment.
Methods
Data collection
All patients undergoing colon or rectal resection for malignancy were entered prospectively into a computer database.
Preoperative assessment
A colonoscopy or barium enema was completed for all the patients. Lesions with an uncertain location were tattooed at the distal margin using carbon black dye injected submucosally. A metastatic workup included chest x-ray, carcinoembryonic antigen levels, and ultrasound or computed tomography of the abdomen. Selected rectal lesions were evaluated with endorectal ultrasound.
Patient selection
All patients were considered for laparoscopic resection as a primary approach regardless of previous surgery, obesity, or comorbidities, with the exception of patients enrolled in the COST trial [14]. We included individuals randomized to the laparoscopic arm of that study.
Surgery
All procedures were completed by one of two experienced laparoscopic surgeons (M.A. and D.B.). Mobilization was undertaken with the Harmonic Scalpel (Ethicon Endosurgery, Cincinnati, OH, USA) using a lateral to medial approach for mesenteric mobilization. Vascular supply was divided intracorporeally. Extraction incisions were either transverse muscle splitting or midline. In all cases, a wound protector was used, and the bowel was divided extracorporeally. Conversion to open surgery was considered. An incision exceeding 6 cm was created to complete some or all aspects of the operation.
Postoperative care
The patients were treated according to an established care protocol, including initiation of clear liquids orally and removal of the Foley catheter (except in cases of anterior resection and abdominoperineal resection) on the first postoperative day. The patients were placed on intermittent parenteral narcotics and oral analgesics as soon as tolerated. Patient-controlled and epidural analgesia were used early in the series.
Adjuvant therapy
Patients were evaluated by medical and radiation oncology at the discretion of the surgeon.
Follow-up evaluation
All patients were seen in a follow-up visit within 1 month of surgery to assess for postoperative complications. Regular clinical follow-up assessment was completed at 3 months, 6 months, 9 months, 1 year, and thereafter every 6 to 12 months. At clinical follow-up visits, patients’ symptoms and physical examination were assessed for any evidence of recurrence. Ultrasound or computed tomography (CT) scan of the liver was completed at 1 year and yearly thereafter for up to 5 years. Carcinoembryonic antigen levels were measured every 3 months for the first year, every 6 months for the second year, and yearly thereafter for up to 5 years. Colonoscopy was completed 1 year postoperatively and then every 3 to 5 years thereafter.
Statistical analysis
The primary outcome measure was survival. Secondary end points included disease-free survival, recurrence, site of recurrence, complications, and variables related to postoperative recovery. Nonparametric data were compared using chi-square or Fisher’s exact test. Survival data were analyzed using Kaplan–Meier curves (SPSS 11.0).
Results
A total of 231 resections were performed for adenocarcinoma of the colon or rectum. Of those resections, 93 were rectal (40.3%) and 138 were colonic (59.7%). Patient characteristics are summarized in Table 1. Eight (3.2%) of the resections were performed as emergencies. Seven (2.8%) resections were performed for cancers of the transverse colon. Only one was converted to open, with no major complications.
Of the procedures attempted laparoscopically, 27 (11.7%) were converted to open surgery. The mean operating room time was 150.1 ± 59.2 min. The sites of the tumors are summarized in Fig. 1, including 7 (2.8%) lesions in the transverse colon. The overall complication rate was 37.6%, which included 14 wound infections (6.1%), 8 significant perioperative bleeds (3.5%), 1 ureteric injury (0.4%), 1 anastomotic leak (0.4%), 19 cardiac events (8.2%), 11 prolonged ileus (4.8%), 5 cases of pneumonia (2.2%), and 8 cases of urinary retention (3.5%). The median postoperative length of stay was 6 ± 12.88 days. The median length of stay for colon resection (5 ± 14.6 days) was less than for rectal resection (7 ± 10 days). The median days to toleration of clear fluids were 2 ± 1.68 days. The last day of analgesic use was after a median of 2 ± 2.76 days. Perioperative outcomes compared favorably with those for previously published group [4] of open resections (Table 2).
Most of the patients (53.2%) had stage II disease, and 8.2% of the patients in the series underwent palliative resection for stage IV disease (Table 3). Locally advanced tumors (T3 or T4) were found in 147 patients (64%), 14 (6.1%) of which were T4 lesions. The margins were positive in three patients (1.2%). There were five perioperative deaths (2%). The median number of lymph nodes resected was 7 ± 5.5. Overall, 11.6% of the patients underwent radiation therapy (10.8% postoperatively, 0.4% preoperatively, 0.4% as a palliative measure). Chemotherapy was administered to 18.5% of the patients.
Follow-up evaluation
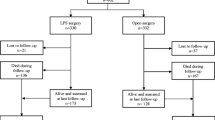
The patients were followed up for a period ranging from 6 to 131.5 months (Fig. 2). A total of 51 patients (22.1%) had recurrence before death, including 14 (6.1%) local and 37 (16%) distant recurrences. Only two patients had wound recurrences (0.8%), and both of these patients had widespread peritoneal recurrence at the time of diagnosis. Overall survival was 65.3% at 60 months and 60.3% at 120 months. The disease-free survival rate was 58% at 60 months and 56% at 120 months. Stage-specific survival is shown in Fig. 3. The results from our series were compared with those from a large database of open colorectal resections, and no statistically significant difference in long-term cancer outcomes was observed (Tables 4 and 5). Port-site recurrence in this series was 0.8%.
Discussion
Randomized clinical trials have shown the application of laparoscopic techniques for colon malignancy to be safe. It seems likely that the availability of these data will greatly expand the application of these techniques to colon malignancy in multiple centers. Surgeons may begin to present this as their preferred surgical approach for colorectal malignancy.
The application of these techniques to rectal malignancy and lesions of the transverse colon has not been addressed in the randomized trials [14, 20]. Both rectal cancer [3, 5, 9, 18] and transverse colon malignancy [9, 16] have been treated successfully, as reported in case series. Our data suggest that the outcome should not be different from that reported by the COST study [20].
The learning curve for laparoscopic colectomy is reported to require 20 to 40 cases [2, 24], but the specific types of resections in these suggested learning curves have not been delineated. The aforementioned areas can be difficult to approach laparoscopically and may require additional experience to approach with comfort. Our own experience includes 93 rectal resections and 6 resections of transverse colon malignancies.
Many of the large series published to date have significant conversion rates [6, 20]. This probably relates in part to the differing levels of experience of the surgeons in each of these studies. Certainly, conversion rates are seen to decrease as more experience is gained [2, 24]. Furthermore, study protocols have been designed to mandate conversion with a relatively low threshold [20]. Although this is important for safe evaluation of the technique, as the surgeon’s laparoscopic experience increases, the conversion rate likely will decrease, enhancing the short-term benefits of attempts to perform resection laparoscopically. Caution must be used, however, to ensure that oncologic principles are not sacrificed for the sake of completing the procedure laparoscopically. Our experience shows an overall conversion rate of 11.7%, including 30 patients enrolled in the randomized trial.
Early in the experience laparoscopic surgery, there was concern about its ability to achieve adequate margins with the loss of tactile feedback. A combination of preoperative tattooing and intraoperative endoscopy was used in our center to compensate for the decrease in tactile information. In our series, only three resections (1.2%) had pathologically positive margins.
The number of lymph nodes harvested has been used as a surrogate marker for adequacy of oncologic resection. Although there are many factors that determine the number of lymph nodes identified in a specimen, the presence of adequate numbers in the specimen has significant implications for staging. Our median number of lymph nodes resected [22] (n = 18) compares favorably with other large series that had no standardized pathologic evaluation for laparoscopic [6, 16] or open [12] resections. Higher numbers of lymph nodes have been reported in trials with standardized pathologic examination [20]. Our lower numbers of nodes are likely related to diligence of pathologic evaluation because the node numbers in the open group from our institution are equivalent.
The attractiveness of the laparoscopic approach is based largely on short-term outcomes. Hospital stay, return of bowel function, and narcotic use in our experience are comparable with those of other large published series [6, 10, 14, 20, 25]. These results also compare favorably with a previously published meta-analysis [1]. Also, short-term outcomes continue to show advantages over the data on open surgery in our institution. Most of the complications over the 10-year series have been minor, with low rates of surgery-specific, major complications, including leak (0.4%), postoperative bleed (0.4%), and ureteric injury (0.4%). The low leak rates likely reflect attention to operative principles: minimal handling of the bowel, avoidance of tension, care to ensure a good blood supply, evaluation of all left-sided anastomoses with endoscopy and insufflation, and selective use of loop ileostomy for low rectal cancers.
Although patients and surgeons may be attracted to the short-term advantages of the laparoscopic approach, these must not be pursued at the expense of decreased oncologic outcomes. Our center has applied laparoscopic techniques to all the different types of colon and rectal resections. With a relatively low conversion rate of 11.7%, which includes locally advanced lesions, our cancer outcomes, including overall survival and disease-free survival, compare favorably with those of a large national cancer database from the United States [11] with a median follow-up period of 26 ± 32.6 months. Furthermore, it seems that the concern about port-site recurrences [14, 16, 20, 22] is slowly coming to rest. Our own experience has involved two port-site recurrences (0.8%).
Regarding rectal cancer, our local recurrence rates with laparoscopic resection are 9% at 36 months, with 11.6% of patients undergoing pre- or postoperative radiation therapy. These are comparable with previously published laparoscopic results [5, 15], and with the outcomes for open resection for total mesorectal excision [13, 17, 19]. This series had a relatively low rate of neoadjuvant therapy and a relatively high rate of locally advanced disease, including T4 disease (6.6% of rectal cases).
Conclusion
Laparoscopic techniques can be applied to a wide range of colorectal malignancies without sacrificing oncologic results during a long-term follow-up period.
References
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short term outcomes after laparoscopic resection of colorectal cancer. Br J Surg 91: 1111–1114
Bennett C, Stryker S, Rosario FM, Adams J, Beart R (1997) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1,194 laparoscopic-assisted colectomies. Arch Surg 132: 41–45
Bretangol F, Lelong B, Luarent C, Moutardier V, Rullier A, Monges G, Delpero JR, Rullier E (2005) The oncological safety of laparoscopic total mesorectal excision with sphincter preservation for rectal carcinoma. Surg Endosc 19: 892–896
Feliciotti F, Paganini AM, Guerreri M, Sanctis A, Campagnacci R, Lezoche E (2002) Results of laparoscopic vs open resections for colon cancer in patients with a minimum follow-up of 3 years. Surg Endosc 16: 1158–1161
Fleshman J, Wexner SD, Anvari M, La Tulippe JF, Birnbaum EH, Kodner IJ, Read TE, Nogueras J, Weiss EG (1999) Laparoscopic vs. open abdominoperineal resection for cancer. Dis Colon Rectum 42: 930–939
Hoffman GC, Baker JW, Fitchett CW, Vansant JH (1994) Laparoscopic-assisted colectomy: initial experience. Ann Surg 219: 732–743
Hong D, Lewis M, Tabet J, Anvari M (2002) Prospective comparison of laparoscopic versus open resection for benign colorectal disease. Surg Laparosc Endosc Percutan Tech 12: 238–242
Hong D, Tabet H, Anvari M (2001) Laparoscopic vs open resection for colorectal adenocarcinoma. Dis Colon Rectum 44: 10–18
Ichihara T, Takada M, Fukumoto S, Kuroda T (2004) Lymphadenectomy along the middle colic artery in laparoscopic resection of transverse colon. Hepatogastroenterology 51: 454–456
Jacob BP, Salky B (2005) Laparoscopic colectomy for colon cancer: an 11-year retrospective review with 5 year survival rates. Surg Endosc 19: 643–649
Jessup JM, McGinnis LS, Steele GD, Menck HR, Winchester DP (1996) The National Cancer Data Base report on colon cancer. Cancer 78: 918–926
Johnson PM, Malatjalian D, Porter GA (2002) Adequacy of nodal harvest in colorectal cancer: a consecutive cohort study. J Gastrointest Surg 6: 883–890
Kapiteilijn E, Putter H, van de Velde CJH (2002) Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in the Netherlands. Br J Surg 89: 1142–1149
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique J, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of nonmetastatic colon cancer: a randomized trial. Lancet 359: 2224–2229
Leroy J, Jamali L, Forbes L, Smith M, Rubino F, Mutter D, Marescaux J (2004) Laparoscopic total mesorectal excision (TME) for rectal cancer surgery. Surg Endosc 18: 281–289
Lujan HJ, Plasencia G, Jacobs M, Viamonte M, Hartmann RF (2002) Long-term survival after laparoscopic colon resection for cancer: complete five-year follow-up. Dis Colon Rectum 45: 491–501
Martling AL, Holm T, Rutqvist LE, Moral BJ, Heald RJ, Cedermark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the county of Stockholm. Stockholm Colorectal Study Group, Basingstoke Bowel Cancer Research Project. Lancet 356: 93–96
Morino M, Parini U, Giraudo G, Salval M, Brachet Contul R, Garrone C (2003) Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg 237: 335–342
Murty M, Enker WE, Martz J (2000) Current status of total mesorectal excision and autonomic nerve preservation in rectal cancer. Semin Surg Oncol 19: 321–328
Nelson H, Sargent DJ, Wieand H, Fleshman J, Anvari M, Stryker J, Beart RW, Hellinger M, Flanagan R, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350: 2050–2059
Phillips EH, Franklin M, Carroll B, Fallas MJ, Ramos R, Rosenthal D (1992) Laparoscopic colectomy. Ann Surg 216: 703–707
Schiedeck THK, Schwandner O, Baca I, Baehrlehner E, Konradt J, Kockerling F, Kuthe A, Buerk C, Herold A, Bruch HP (2000) Laparoscopic surgery for the cure of colorectal cancer: results of a German five-year study. Dis Colon Rectum 43: 1–8
Schlachta CM, Mamazza J, Gregoire R, Burpee S, Poulin E (2003) Could laparoscopic colon and rectal surgery become the standard of care? A review and experience with 750 procedures. Can J Surg 46: 432–440
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44: 217–222
Wexner SD, Reissman P, Pfeifer J, Bernstein M, Geron N (1996) Laparoscopic colorectal surgery: analysis of 140 cases. Surg Endosc 10: 133–136
Acknowledgment
The authors acknowledge the assistance of Catherine Gill Pottruff in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) meeting, Hollywood FL, USA, 12–16 April 2005
Rights and permissions
About this article
Cite this article
Sample, C.B., Watson, M., Okrainec, A. et al. Long-term outcomes of laparoscopic surgery for colorectal cancer. Surg Endosc 20, 30–34 (2006). https://doi.org/10.1007/s00464-005-0253-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0253-z