Abstract
Background
There are few reports on laparoscopic rectum resection demonstrating its feasibility and efficacy in patients with rectal cancer. Most patient series are small, and results must be considered preliminary and medium-term. Our large prospective conducted study aimed to assess the effectiveness of a totally laparoscopic resection for rectum carcinoma with emphasis on perioperative and long-term oncological outcomes.
Methods
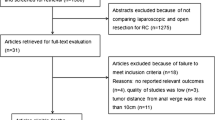
Between November 1992 and July 2003, 194 unselected patients were resected laparoscopically for rectal carcinoma. Patients with locally advanced rectum carcinoma (uT3/uT4) and no evidence of distant metastases were candidates for neoadjuvant chemoradiation. Adjuvant treatment was administered to patients with UICC stage II/III disease. All patients were followed up prospectively to evaluate complications and late outcomes. Survival probability analysis was performed using the Kaplan-Meier method. Study selection was made by Medline search using the following key words: rectal cancer, rectal neoplasms, laparoscopy, and resection. Single case reports and abstracts were excluded. When surgical series were reported more than once, only the most recent reports were considered and listed.
Results
The most common procedures were low anterior resection with total mesorectum excision in 65.5% of patients and high anterior resection in 25.3%. Average operative time was 174 min. Average number of lymph nodes removed was 25.4 and length of specimen resected was 27.6 cm. Resection was curative in 145 patients and palliative in 49 cases. UICC tumor stages were as follows: stage I: 25.2%, stage II: 27.3%, stage III: 30.4%, and stage IV: 17%. Intraoperative complications were <1% for lesions of the ureter, urinary bladder, and deferent duct. Conversion to conventional surgery was necessary in two cases (1%). The most common postoperative complication was anastomotic leakage in 13.5% of patients. There was no postoperative mortality. Follow-up evaluation ranged from 1 to 128 months with a mean of 46.1 months. The most common late complication was incisional hernia in 3.6% of patients. Port-site metastases occurred in one patient (0.5%). Tumor recurrence developed in 23 of the 145 curative resected patients (11.7% distant metastases and 4.1% local recurrence). Overall local recurrence rate was 6.7% (4.1% after curative resection and 14.3% after palliative resection). Overall survival rate was 90.6% at 1 year, 74.5% at 3 years, and 66.3% at 5 years. Overall 5-year survival rate was 76.9% after curative resection and 31.8% after palliative resection. Cancer-related survival rate was 94% at 1 year, 82.4% at 3 years, and 78.9% at 5 years. At 5 years it was 87.7% after curative resection and 48.5% after palliative resection. At 5 years, the survival rate was 100% for stage I, 94.4% for stage II, 66.6% for stage III, and 44.6% for stage IV.
Conclusions
Our results and the literature review clearly demonstrate that laparoscopic resection for rectal cancer is not associated with higher morbidity and mortality. Established oncological and surgical principles are respected and long-term outcomes are at least as good as those after open surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
One of the most controversial areas of laparoscopic colorectal surgery is that of rectal cancer. This is due to the perception that it is more challenging than colon resection in achieving radical cancer surgery within the complex anatomy of the pelvis. Furthermore, the lack of data on large patient series with longer follow-up partly accounts for surgeons’ reluctance to adopt this method in patients with rectal cancer. The purpose of this prospectively conducted study is to report the perioperative and late results, with emphasis on complications, and long-term survival in 194 patients who underwent a “totally” laparoscopic resection for rectal cancer at our department. Furthermore, published papers dealing with laparoscopic rectum resection are reviewed.
Materials and Methods
Between November 1992 and July 2003, a total of 1000 colorectal laparoscopic procedures were performed at our institution; 601 patients had a benign colorectal disease and 399 cases were resected laparoscopically for colorectal malignancy. Of these, 200 cases had a colon carcinoma and the remaining 194 had rectal cancer. The tumor was considered as primary rectal carcinoma if it was located in the lower third (0–6 cm from the anal verge), middle third (7–12 cm), or upper third of the rectum (12–18 cm) as measured by rigid rectosigmoidoscopy. All patients underwent preoperative tumor staging by contrast medium enema, rectoscopy and colonoscopy with biopsies of the tumor, endorectal ultrasonography, abdominal ultrasound, and chest x-ray.
Patients with locally advanced rectum carcinoma (uT3/uT4) and no evidence of distant metastases were candidates for neoadjuvant chemoradiation including the following schedule: 30–50 Gy radiotherapy and 5-fluouracil (5-FU) in combination with folinic acid over 5 weeks. The operation was carried out 2–3 weeks after completion of the multimodality treatment. Adjuvant treatment was administered to patients with UICC stage II/III disease and consisted of six cycles of 5-FU/folinic acid.
All patients were followed up prospectively by means of clinical examination, tumor markers (CEA, CA19-9), rectoscopy, and ultrasonography of the abdomen every 3 months for the first 2 years, every 6 months after 2 years, and then every year after 5 years in order to evaluate late complications and tumor recurrence. The survival probability analysis was performed using the Kaplan-Meier method.
Surgical technique
All operations were performed by one surgeon (E. Bärlehner). The patients were placed in a steep Trendelenburg position. We utilize five ports: four 10 mm and one 12 mm. The specimen is removed through a small (5-cm) incision in the left lower quadrant port site. The operation is performed with a harmonic scalpel (Ultracision, Ethicon Endosurgery). We begin with the mobilization of the sigmoid, descending colon, and splenic flexure on the Gerota fascia up to the mid transverse. The gonadal vessels and the left ureter are identified. The retroperitoneum is incised on the promontory, and the inferior mesenteric vessels are identified and divided. The artery is taken 1–2 cm anterior to the aorta and the vein is divided close to the pancreas. During mobilization of the mesorectum care must be taken to avoid any damage to the underlying hypogastric nerve plexus. Dissection is continued ventrally in front of the Denonvilliers’ fascia. Following that, we perform a deep or intersphincteric stapling of the rectum with a linear cutter. The rectum and sigmoid colon are extracted through a plastic wound protector in a small left lower quadrant incision. The anvil of the circular stapler is positioned in the descendens colon. The circular stapler is then inserted through the rectum and an end-to-end descendo-rectostomy is performed. The integrity of the stapled anastomosis is checked by the inspection of an intact double donut and an underwater bubble test. A drain is placed at the end of the operation in the pelvis. In cases of abdomino-perineal resection the mobilized rectum together with the whole mesorectum is retrieved through the perineal incision in the traditional fashion. The perineal wound is closed primarily and a terminal colostomy is fashioned at the left lower quadrant site.
Registry database
Clinical, surgical, and histopathological data were recorded prospectively in a registry database (PC). Data supplied for each patient included gender, age, body mass index, ASA score, tumor localization, preoperative and postoperative multimodality therapy, type of resection and anastomosis, operating time, intraoperative and postoperative complications, number of resected lymph nodes, length of removed specimen, UICC tumor stage, late complications, tumour recurrence, overall survival, cancer-related survival, and stage-specific survival. All data were analyzed by a statistician (B. Schicke) with the SPSS 11.5 software for Windows (SPSS, Chicago, IL).
Results
Patients
Patients’ baseline data are listed in Table 1. The unselected patient coort comprised 125 men and 69 women whose average age was 65 years. Of the patients, 28% were 70 years and older. The mean body mass index was 26.4 kg/m2. It was >25 kg/m2 in 102 cases. The ASA score was III–IV in >70% of the patients. Tumors were located in the upper rectum in 44 patients, the midrectum in 86 patients, and the lower rectum in 64 cases. A total of 102 patients received preoperative radiation and/or chemotherapy; 125 patients received this treatment modality postoperatively.
Procedure performed
The most common procedure was low anterior resection with total mesorectum excision in 127 patients and colonic J-pouch in 28 cases (Table 2). A total of 49 patients had resection of the rectosigmoid junction, and 16 had abdomino-perineal resection. One patient with ulcerous colitis and rectal carcinoma received a proctocolectomy and another one a Hartmann procedure. The double stapling technique was the most common anastomosis type (90%), followed by colostomy in 9% of the cases and two hand-performed coloanal anastomoses. Average operative time was 174 min.
Histopathological results
Average number of lymph nodes removed was 25.4 (ranging from 11 to 84) and length of specimen resected was 27.6 cm (range 11–68 cm). Resection was curative in 145 patients and palliative in 49 cases. The distribution of patients according to the UICC classification was as follows: stage I: 49 patients (25.2%), stage II: 53 (27.3%), stage III: 59 (30.4%), and stage IV: 33 patients (17%).
Surgery-related complications
Intraoperative complications occurred rarely, <1% for lesions of the ureter, urinary bladder, and deferent duct. Conversion to conventional surgery was necessary in two cases (1 %). Blood transfusion was required in only two patients (Table 3).
The most common postoperative complication was the anastomotic leakage in 13.5% of the patients. The frequency of other complications such as bleeding, rectovaginal fistula, ileus, and infections was <2%. There was no postoperative mortality. A relaparoscopy was necessary in 5.1% of the patients and a laparotomy in 6.2%. Follow-up evaluation ranged from 1 to 128 months with a mean of 46.1 months. The records of 97% of the patients could be investigated prospectively.
Late complications such as anastomotic stenosis, ileus, and incontinence occurred rarely. The most common late complication was incisional hernia in 3.6% of the patients. Port site metastasis occurred in one patient (0.5%) with stage IV disease (peritoneal carcinosis) who underwent a palliative resection.
Oncological results and survival
After a mean follow-up of 46.1 (1–128) months, tumor recurrence occurred in 23 of the 145 curatively resected patients (11.7% distant metastases and 4.1% local recurrence). Overall local recurrence rate was 6.7% (4.1% after curative resection and 14.3% after palliative resection) (Table 4). Overall survival rate was 90.6% at 1 year, 74.5% at 3 years, and 66.3% at 5 years. Overall 5-year survival rate was 76.9% after curative resection and 31.8% after palliative resection (Fig. 1). Cancer-related survival rate was 94% at 1 year, 82.4% at 3 years, and 78.9% at 5 years. It was 87.7% at 5 years after curative resection and 48.5% at 5 years after palliative resection (Fig. 2). At 5 years, the survival rate was 100% for stage I, 94.4% for stage II, 66.6% for stage III, and 44.6% for stage IV (Fig. 3).
Discussion
Historically, the three major and decisive strides that have been made in the last two decades in the treatment of rectal cancer were the establishment of multimodality therapy, the introduction of total mesorecrum excision, and the application of laparoscopy. Neoadjuvant therapy made it possible for many patients with locally advanced tumors who were previously deemed unresectable to undergo potentially curative surgical resection without colostomy, preserving the anal sphincter and maintaining continence. Furthermore, it has been clearly demonstrated that adjuvant treatment has the potential of improving prognosis not only in terms of local recurrence, but also in terms of overall survival [11]. A further milestone in the outcome of rectal cancer has been the introduction of total mesorectal excision (TME). It is only historically interesting to mention that the concept of TME had already been elucidated in an impressive way by Heinrich Westhues from Erlangen, Germany, in 1934 [31]. He showed in meticulous pathologic studies that the complete en bloc removing of the tumor together with the “perirectal and retrorectal tissue” is the way to reduce pelvic recurrence, and he applied this radical procedure in 46 patients with rectum carcinoma. After a follow-up of more than 2 years, no tumor recurrence had occurred in his patient group. At that time ~50% of the patients developed local recurrence within 1 year after rectum resection. In the early 1980 s, Heald and colleagues substantiated the principles of TME [9]. With this technique, they reported a local recurrence rate of 4% at 10 years, and a disease-free survival of 80% at 5 years and 78% at 10 years after curative resection. In light of these and other results [15], TME-based operations have become the new standard technique of care for mobile rectal cancer. With the rapid application of advanced laparoscopy, many investigations have demonstrated benefits for laparoscopic colorectal surgery in terms of faster postoperative recovery, less pain, less morbidity and mortality, and earlier return to full activity. Furthermore, many reports have repeatedly shown the feasibility and partly the efficacy of laparoscopic rectum resection for malignancy [1, 4–8, 10, 12–14, 16, 18–22, 24, 26–30, 32, 33]. However, the effectiveness of this new method is, as yet, unclear. The main concern regarding this technique is that most trials involve only small series that are based on retrospective reviews. Only the two studies reported by Tang et al. from Singapore and Leung et al. from Hong Kong were prospective randomized [14, 27]. The trial by Tang et al. was performed in parallel with the UK Medical Research Council Conventional versus Laparoscopic-assisted Surgery in Colorectal Cancer (CLASSIC) trial. The local component of this collaboration investigated the immune stress response following open and laparoscopic resection for cancer. Thus, oncological data are not available [27]. In the study by Leung et al., 403 patients with rectosigmoid carcinoma were randomized to receive either laparoscopic assisted (n = 203) or conventional open (n = 200) resection of the tumor [14].
Nonetheless, most data reported must be considered preliminary and medium-term results at best. These reports should be interpreted and compared very carefully. Including our series, a total of 1818 patients worldwide have been reported as receiving a laparoscopic resection for rectum malignancy (Table 5). The most commonly performed operation was anterior resection in ~68% of the cases. The operative time ranged from 88 to 600 min. The reported morbidity rate was 0–55% including an anastomotic insufficiency rate of 0–27%. Conversion to open surgery varied from 0 to 50%. The postoperative mortality rate was <3% and zero in most reported series. It would seem that laparoscopic rectal surgery is associated in some series with a somewhat higher morbidity rate [2, 23, 25, 34]. The high prevalence of anastomotic breakdown is particularly worrisome, although the leak rate is comparable to that of conventional anterior resection. The overall insufficiency rate in our series was 13.5% (24/177 patients). Of these 24 patients three received rectosigmoid resection and 21 underwent low anterior resection. Only two of these 21 patients had a diverting loop ileostomy. As a matter of fact, laparoscopic low anterior resection is a very demanding operation requiring advanced surgical skills in laparoscopic colorectal surgery [17]. Nevertheless, the importance of surgical technique should be highlighted since a strong association between leakage from a colorectal anastomosis and the development of local recurrence after potentially open curative resection for rectal cancer has been recently reported [3]. No local recurrence was diagnosed after a mean follow-up of 46.1 months in our patients with anastomotic leakage. The mean survival time was 67.6 months in this subgroup of patients.
Despite acceptable postoperative data, evaluation of oncological adequacy is not only based on distal margin clearance or on the number of lymph nodes removed but also on long-term outcomes in terms of local recurrence and 5-year survival rates. The reported medium-term oncological data are altogether comparable to those after open rectum resection (Table 6). It is interesting and very important to note the very low incidence of port-site metastases. Only two cases of a total of 1818 patients who underwent laparoscopic rectum resection developed this complication (0.11%). Both patients had primary metastatic disease. Reservations must be expressed with regard to the high local recurrence rates reported by Weaver (15%) and Feliciotti (21%) [30, 6]. In the prospective randomized trial by Leung et al., laparoscopic resection did not worsen survival and disease control for patients with rectosigmoid cancer compared with open resection, and its benefits in reducing pain and allowing earlier postoperative recovery were confirmed. Conspicuous in this study is the high conversion rate (23.2%) [14]. Appropriate surgical technique together with experience in laparoscopy will ensure low incidence of morbidity rate, conversion, and local recurrence once the learning curve is passed. Our results originate from a center with extensive experience in all fields of minimally invasive surgery with more than 1100 colorectal resections performed to date and all laparoscopic rectum resections were performed by one surgeon. This reflects among other things the exceptional low abdominoperineal resection rate of 8% and the high low anterior resection rate with TME in 65.5% of the patients.
In our experience with this technique, the rates of local recurrence, distant metastases, and patient survival are comparable with those established by the larger series of patients with rectal carcinoma. Laparoscopic rectum resection allows accurate magnification and identification of all fine and important anatomic structures in the narrow pelvis, e.g., the hypogastric nerves, and the “holy planes.” Dissection under laparoscopic view allows minimal blood loss and avoids tumor cell seeds in the pelvis. Of course, laparoscopic surgery is technically more demanding than the open approach, and the learning curve is somewhat protracted. Nevertheless, what is laparoscopically difficult may also be technically arduous with the conventional counterpart.
Conclusion
Rectum surgery has not reached a plateau beyond which it will not progress. Laparoscopic resection for rectal malignancy might be the next step in the evolution of modern rectal cancer surgery. Our results and the literature review clearly demonstrate that laparoscopic resection for rectal carcinoma is not associated with a higher morbidity or mortality. Established oncological and surgical principles are respected, and the few reported data on long-term outcomes seem to equal to those after open surgery. The fundamental feasibility and efficacy of this method have been proven. Now it should be examined to what extent these favorable results can be reproduced in the setting of a multicenter Phase 3 study. Nonetheless, at the present time, laparoscopic rectum resection for cancer cannot be yet recommended for routine use.
References
M Anthuber A Fuerst F Elser R Berger KW Jauch (2003) ArticleTitleOutcome of laparoscopic surgery for rectal cancer in 101 patients Dis Colon Rectum 46 1047–1053 Occurrence Handle10.1007/s10350-004-7279-5 Occurrence Handle12907898
E Bärlehner Decker Th Anders St B Heukrodt (2001) ArticleTitleLaparoskopische Chirurgie des Rektumkarzinoms. Onkologische Radikalität und Spätergebnisse Zentralbl Chir 126 302–306 Occurrence Handle10.1055/s-2001-14745 Occurrence Handle11370393
SW Bell KG Walker MJFX Rickard G Sinclair OF Dent PH Chapuis EL Bokey (2003) ArticleTitleAnastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence Br J Surg 90 1261–1266 Occurrence Handle10.1002/bjs.4219 Occurrence Handle14515297
JCC Chen JB Chen HM Wang (2002) ArticleTitleLaparoscopic coloanal anstomosis for low rectal cancer J Soc Laparoendosc Surg 6 345
A Darzi C Lewis N Menzies-Gow PJ Guillou JRT Monson (1995) ArticleTitleLaparoscopic abdominoperineal excision of the rectum Surg Endosc 9 414–417 Occurrence Handle7660266
F Feliciotti M Guerrieri AM Paganini A Sanctis ParticleDe R Campanacci S Perretta G D’Ambrosio G Lezoche E Lezoche (2003) ArticleTitleLong-term results of laparoscopic vs open resections for rectal cancer for 124 unselected patients Surg Endosc 17 1530–1535 Occurrence Handle10.1007/s00464-002-8874-y Occurrence Handle12874687
JW Fleshman SD Wexner M Anvari JF LaTulippe EH Birnbaum IJ Kodner TE Read JJ Nogueras EG Weiss (1999) ArticleTitleLaparoscopic vs. open abdominoperineal resection for cancer Dis Colon Rectum 42 930–939 Occurrence Handle10411441
JE Hartley BJ Mehigan AE Qureshi GS Duthie PWRL Lee JRT Monson (2001) ArticleTitleTotal mesorectal excision: Assessment of the laparoscopic approach Dis Colon Rectum 44 315–321 Occurrence Handle11289275
RJ Heald BJ Moran RDH Ryall R Sexton JK MacFarlane (1998) ArticleTitleRectal cancer. The Basingstoke experience of total mesorectum excision Arch Surg 133 894–899 Occurrence Handle10.1001/archsurg.133.8.894 Occurrence Handle9711965
AJN Iroatulam F Agachan O Alabaz EG Weiss JJ Nogueras SD Wexner (1998) ArticleTitleLaparoscopic abdominoperineal resection for anorectal cancer Am Surg 64 12–18 Occurrence Handle9457031
E Kapiteijn CJ van-de-Velde (2002) ArticleTitleThe role of total mesorectal excision in the management of rectal cancer Surg Clin North Am 82 995–1007 Occurrence Handle10.1016/S0039-6109(02)00040-3 Occurrence Handle12507205
SW Larach MC Salomon PR Williamson E Goldstein (1993) ArticleTitleLaparoscopic assisted abdominoperineal resection Surg Laparosc Endosc 3 115–118 Occurrence Handle8269230
J Leroy F Jamali L Forbes M Smith F Rubino D Mutter J Marescaux (2003) ArticleTitleLaparoscopic total mesorectal excision (TME) for rectal cancer surgery Surg Endosc 18 281–289 Occurrence Handle14691716
KL Leung SPY Kwok SCV Lam JFY Lee RYC Yiu SSM Ng PBS Lai WY Lau (2004) ArticleTitleLaparoscopic resection of rectosigmoid carcinoma: prospective randomised trial Lancet 363 1187–1192 Occurrence Handle10.1016/S0140-6736(04)15947-3 Occurrence Handle15081650
AL Martling T Holm LE Rutqvist BJ Moran RJ Heald B Cedermark InstitutionalAuthorNameStockholm Colorectal Cancer Study Group InstitutionalAuthorNameBasingstoke Bowel Cancer Research Project (2000) ArticleTitleEffect of surgical training programme on outcome of rectal cancer in the county of Stockholm Lancet 356 93–96 Occurrence Handle10.1016/S0140-6736(00)02469-7 Occurrence Handle10963244
M Morino U Parini G Giraudo M Salval RB Conral C Garrone (2003) ArticleTitleLaparoscopic total mesorectal excision. A consecutive series of 100 patients Ann Surg 237 335–342 Occurrence Handle10.1097/00000658-200303000-00006 Occurrence Handle12616116
M Pera S Delgado JC García-Valdecasas M Pera A Castells JM Piqué E Bombuy AM Lacy (2002) ArticleTitleThe management of leaking rectal anastomoses by minimally invasive techniques Surg Endosc 16 603–606 Occurrence Handle10.1007/s00464-001-9097-3 Occurrence Handle11972197
A Pietrabissa C Moretto A Carobbi U Boggi F Ghilli F Mosca (2002) ArticleTitleHand-assisted laparoscopic low anterior resection. Initial experience with a new procedure Surg Endosc 16 431–435 Occurrence Handle10.1007/s00464-001-9084-8 Occurrence Handle11928022
EC Poulin CM Schlachta R Grégoire P Seshadri MO Cadeddu J Mamazza (2002) ArticleTitleLocal recurrence and survival after laparoscopic mesorectal resection for rectal adenocarcinoma Surg Endosc 16 989–995 Occurrence Handle10.1007/s004640080182 Occurrence Handle12163970
JR Ramos RH Petrosemolo EA Valory FC Polania R Pecanha (1997) ArticleTitleAbdominoperineal resection: laparoscopic versus conventional Surg Laparosc Endosc 7 148–152 Occurrence Handle10.1097/00019509-199704000-00017 Occurrence Handle9109247
JA Reis Neto FA Quilici F Cordeiro JA Reis SuffixJr O Kagohara J Simoes Neto (2002) ArticleTitleLaparoscopic total mesorectal excision J Soc Laparoendosc Surg 6 163–167
R Rullier A Sa Cunha P Couderc A Rullier R Gontier J Saric (2003) ArticleTitleLaparoscopic intersphincteric resection with coloplasty and coloanal anastomosis for mid and low rectal cancer Br J Surg 90 445–451 Occurrence Handle10.1002/bjs.4052 Occurrence Handle12673746
H Scheidbach C Schneider E Baerlehner J Konradt F Koeckerling (2001) ArticleTitleLaparoscopic anterior resection for rectal carcinoma Surg Oncol Clin North Am 10 599–609
H Scheidbach C Schneider J Konradt E Bärlehner L Köhler Wittekind Ch F Köckerling (2002) ArticleTitleLaparoscopic abdominoperineal resection and anterior resection with curative intent for carcinoma of the rectum Surg Endosc 16 7–13 Occurrence Handle10.1007/s00464-001-8314-4 Occurrence Handle11961595
H Scheidbach C Schneider O Hugel H Scheuerlein E Bärlehner J Konradt C Wittekind F Köckerling (2003) ArticleTitleOncological quality and preliminary long-term results in laparoscopic colorectal surgery Surg Endosc 17 903–910 Occurrence Handle10.1007/s00464-002-8966-8 Occurrence Handle12632133
O Schwandner THK Schiedeck C Killaitis HP Bruch (1999) ArticleTitleA case-control study comparing laparoscopic versus open surgery for rectosigmoidal and rectal cancer Int J Colorectal Dis 14 158–163 Occurrence Handle10.1007/s003840050203 Occurrence Handle10460907
CL Tang KW Eu BC Tai JGS Soh D Machin F Seow-Choen (2001) ArticleTitleRandomized clinical trial of the effect of open versus laparoscopically assisted colectomy on systemic immunity in patients with colorectal cancer Br J Surg 88 801–807 Occurrence Handle10.1046/j.1365-2168.2001.01781.x Occurrence Handle11412248
WWC Tsang CC Chung MKW Li (2003) ArticleTitleProspective evaluation of laparoscopic total mesorectal excision with colonic J-pouch reconstruction for mid and low rectal cancers Br J Surg 90 867–871 Occurrence Handle10.1002/bjs.4105 Occurrence Handle12854115
I Uyama A Sugioka H Matsui J Fujita Y Komori T Hanai A Hasumi (2001) ArticleTitleLaparoscopic lateral node dissection with autonomic nerve preservation for advanced lower rectal cancer J Am Coll Surg 193 579–584 Occurrence Handle10.1016/S1072-7515(01)01042-0 Occurrence Handle11708519
DW Weaver SR Eachempati (2000) ArticleTitleLaparoscopically assisted transsacral resection of rectal cancer with primary anastomosis. A preliminary review Surg Endosc 14 703–707 Occurrence Handle10.1007/s004640020085 Occurrence Handle10954813
H Westhues (1934) Die pathologisch-anatomischen Grundlagen der Chirurgie des Rektumkarzinoms G Thieme Leipzig
S Yamamoto M Watanabe H Hasegawa M Kitajima (2002) ArticleTitleProspective evaluation of laparoscopic surgery for rectosigmoid and rectal carcinoma Dis Colon Rectum 45 1648–1654 Occurrence Handle10.1007/s10350-004-7253-2 Occurrence Handle12473889
ZG Zhou Z Wang YY Yu Y Shu Z Cheng L Li WZ Lei TC Wang (2003) ArticleTitleLaparoscopic total mesorectal excision of low rectal with preservation of anal sphincter: a report of 82 cases World J Gastroenterol 9 1477–1481 Occurrence Handle12854145
O Zmora SD Wexner (2001) ArticleTitlePart I. Laparoscopic surgery for colon and rectal cancer Curr Probl Cancer 25 286–309 Occurrence Handle10.1067/mcn.2001.117697 Occurrence Handle11568735
Acknowledgment
We are indebted to Prof. Peter Hohenberger (University of Mannheim) for his invaluable assistance in reviewing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bärlehner, E., Benhidjeb, T., Anders, S. et al. Laparoscopic resection for rectal cancer: Outcomes in 194 patients and review of the literature. Surg Endosc 19, 757–766 (2005). https://doi.org/10.1007/s00464-004-9134-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-9134-0