Abstract
Background
Nonobese patients undergoing laparoscopic procedures present a dilemma as to the correct mode of entry into the abdominal cavity because the Veress needle (VN) technique seems to be associated with a high risk of vascular and visceral injuries. Direct trocar insertion (DTI) has been reported as an alternative to the VN for creation of the pneumoperitoneum.
Methods
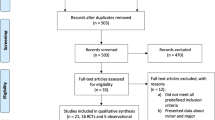
An open comparative randomized prospective study was conducted on the feasibility and safety of DTI vs the VN technique in nonobese patients of any age category referred for urgent or scheduled laparoscopic procedures. Exclusion criteria were obesity (defined as a body mass index [BMI] > 27 kg/m2), major abdominal distension, and two or more previous abdominal operations. The study endpoints were the feasibility and safety of the DTI and VN techniques. Results were evaluated on an intention-to-treat basis. Statistical analysis was carried out with the t-test for independent samples, the chi-square tests, and the Fisher’s exact tests, as appropriate. The level of significance was 0.01.
Results
Since January 2002, a total of 598 nonobese patients have been entered into the current trial; 46% (mean BMI 21.6 ± 4.4 kg/m2) were randomly allocated to DTI, whereas 54% (BMI 21.1 ± 5.3 kg/m2) were allocated to the VN techniques. Demographic features and type of procedures were similar for the two groups. DTI was feasible in 100% of patients vs 98.7% in the VN group (p = NS). Minor complications were nil in the DTI group and 5.9% in the VN group (p < 0.01). The latter group consisted of 11 cases (3.4%) of subcutaneous emphysema and eight cases (2.5%) of extraperitoneal insufflation. Major complications were nil in the DTI group and 1.3% among VN patients (p = NS). These latter cases consisted of two (0.3%) hepatic lesions managed laparoscopically; one (0.3%) misdiagnosed ileal perforation requiring reintervention, and one (0.3%) mesenteric laceration treated conservatively.
Conclusion
In thin and very thin patients of any age category with no more than one previous abdominal operation, DTI is a safe alternative to the VN technique and is associated with fewer minor complications. In terms of major complications, there is no difference between the two techniques. Either technique of access is acceptable Thin and very thin patients undergoing laparoscopy, on condition that the basic principles of laparoscopic surgery are complied with.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nonobese patients undergoing laparoscopic procedure often present a dilemma as regards the choice of the best technique for entry into the abdominal cavity. Although the Veress needle (VN) technique for establishing the pneumoperitoneum is widely used, it is associated with slow insufflation rates and potentially life-threatening complications. Although these complications mainly affect patients at the extreme ends of the weight spectrum (thin and obese) and patients who have had previous abdominal operations, they represent a major source of morbidity and mortality from laparoscopic procedures and a major reason for conversion to the open approach [11]. An incorrect VN technique may result in extraperitoneal insufflation, making the procedure more difficult and time consuming [9]; but the spectrum of VN-related complications encompasses abdominal wall injuries, as well as visceral and vascular lesions [11]. The open approach (OA) offers a good alternative to the VN technique because it is relatively safer, even if considered cumbersome by many authors. Although OA is credited with reducing the incidence of vascular and visceral complications to nil, a 0.2% incidence of complications among 10,840 open gynecologic laparoscopies and a 0.06% incidence of bowel injuries have been reported [6]. Recently, direct trocar insertion (DTI) without a pneumoperitoneum has been described as an alternative to both techniques, but it is largely confined to gynecologic procedures [6, 9]. To date, there is no evidence to prove the superiority of DTI, but it appears to be as safe as the VN and OA techniques and should be considered an integral part of the surgical armamentarium of a well-trained laparoscopic surgeon.
To assess the feasibility and safety of DTI in thin and very thin patients undergoing laparoscopic procedures, we set up an open randomized prospective trial comparing the VN technique with DTI in elective and urgent laparoscopic procedures performed at a single institution.
Materials and methods
An open comparative randomized prospective trial on the feasibility and safety of the VN vs the DTI technique in nonobese patients undergoing laparoscopic procedure was started in January 2002 at the Unità Operative di Chirurgia Generale, Ospedale Civile, Vittorio Veneto (TV), Italy. The participating surgeons (F.A., L.F.C., N.B.) were trained in both techniques. To detect a difference of 12%, with a statistical power of 80% and a significance level of <5%,230 patients were to be recruited in each treatment arm. The inclusion criteria called for nonobese pediatric and adult patients referred for urgent or scheduled laparoscopic and gynecologic procedures. No age limit was used in the current trial, because it is our policy to operate on pediatric patients by laparoscopy. Exclusion criteria were obesity, defined as a body mass index (BMI) >27 kg/m2; the presence of massive bowel distension; and a history of two or more abdominal operations. Patients were enrolled after informed consent was obtained and then randomized to one of the techniques by means of a sealed-envelope allocation system.
All relevant clinical and surgical data were stored in a package database (Statistica ‘99 for Windows; StatSoft., Tulsa, OK, USA) for successive evaluation, and an intention-to-treat analysis was carried out on all patients included in the current series. The study endpoints were the feasibility of both the VN and the DTI techniques, defined as the ratio between successful to total attempts, and the incidence of VN- and DTI-related complications.
Minor complications were defined as those that did not influence the length of the postoperative hospital stay, whereas major complications were defined as those leading to death, those requiring conversion to an open procedure or reintervention, and those leading to prolongation of the hospital stay. It was agreed that unsuccessful VN and/or DTI attempts were to be converted to the OA technique and ultimately to an open operation.
The DTI technique was performed according to guidelines given elsewhere [11]. All patients are placed in the supine position with a 0° tilt. After adequate patient relaxation, a 5-mm skin incision is made at the level of the umbilicus or in the right upper quadrant (in case of laparoscopic cholecystectomy) to match the introduction of a 5-mm shielded trocar (dilating tip trocar, Endopath; Ethicon Endo-Surgery, Cincinnati, OH, USA). The abdominal wall is lifted by grasping the skin upward. Once the tip of the trocar has been inserted through the skin incision, the trocar is pulled through the fascia and the muscle layer by a continuous twisting motion with constant pressure, so that the surgeon can easily realize when the trocar has pierced the peritoneum and entered the abdominal cavity. The trocar position is verified by insertion of a 5-mm laparoscopic optic. Once visualization of the peritoneal cavity is obtained, a carbon dioxide pneumoperitoneum is insufflated at a pressure of 15 mmHg. For evaluation purposes, the trocar insertion time was defined as the interval between skin incision and introduction of the laparoscope. At the end of the procedure, the abdominal wall fascia is sutured at the level of each port site.
Values are reported as mean ± SD when appropriate. The statistical analysis was performed with the t-test for independent samples for continuously distributed values and with the chi-square test (or Fisher’s exact test when cell values < 5) for all categorical variables.
Results
Since January 2002, a total of 598 patients have been enrolled in the current trial. Forty-six percent of patients (275 of 598) were operated on with DTI, whereas 54% (323 of 598) were operated on with the VN technique. Because of an 8% post hoc deviation of patient allocation due to the sealed-envelope randomization method adopted, the level of significance was set at 0.01.
Table 1 shows the demographic characteristics of the study population. In the DTI group, the mean age was 40.2 ± 17.8 years (range, 7–76), the mean BMI was 21.6 ± 4.4 kg/m2 (range, 19.3–26.8), and the sex ratio (M:F) was 123:152. In the VN group, the mean age was 41.1 ± 15.6 years (range, 11–72, the mean BMI was 21.2 ± 5.3 kg/m2 (range, 19.5–27), and the sex ratio (M:F) was 155:168 (p = NS).
Previous abdominal procedures were reported in 41% (113 of 275) and 48% (156 of 323) of patients in the DTI and VN groups, respectively. The surgical procedures were similarly distributed. Namely, laparoscopic cholecystectomy accounted for 66% (182 of 275) and 61% (197 of 323) of cases, respectively (p = NS), in DTI and VN; appendectomy represented 23% (63 of 275) and 28% (90 of 323) of cases, respectively (p = NS); colon resections were done in 4% (11 of 275) and 5% (16 of 323), respectively (p = NS), and other procedures were performed in 7% (19 of 275) and 6% (20 of 323) of patients, respectively (Table 2). DTI was feasible in 100% of cases, and no conversion rate to OA was necessary. Duration of DTI was 123 ± 37 s. Conversely, the feasibility rate of VN was 98.7% (319 of 323), and in four cases conversion to OA was necessary because of massive extraperitoneal insufflation (p = NS) (Table 2).
Minor complications were nil in the DTI group and 5.9% (19 of 323) in the VN group (p < 0.01). The latter complications consisted of 11 cases (3.4%) of subcutaneous emphysema and eight cases (2.5%) of extraperitoneal insufflation. Major complications related to the abdominal access technique were nil in the DTI group and 1.3% among the VN patients (four of 323) (p = NS). These latter complications of two (0.3%) hepatic lesions managed laparoscopically, one (0.3%) misdiagnosed ileal perforation that required reintervention for diffuse peritonitis 10 days after the primary operation, and one (0.3%) mesenteric laceration treated conservatively. No cases of gas embolism were observed in either group. Mortality related to either technique was nil. At a mean follow-up of 11.2 ± 7.1 months, no hernia has thus far been observed at the level of DTI port site accesses.
Discussion
Over the last decades, laparoscopy has gained widespread acceptance in common surgical practice as an effective diagnostic and therapeutic tool, with an ever-growing number of surgeons adopting this technique. Abdominal access and the creation of the pneumoperitoneum carry a risk of visceral and vascular injury [11]. In one of the first reports on laparoscopic cholecystectomy [12], Ponsky described subcutaneous and mediastinal emphysema, pneumothorax, abdominal wall bleeding, gastrointestinal perforations, solid organ and visceral injuries, avulsion of adhesions, cardiac arrhythmias, and postoperative port site hernias as complications associated with abdominal access and creation of the pneumoperitoneum. The DTI technique was first reported by Dingfelder in 1978 [5] and later described by Copeland et al. in 1983 [4], but so far it has been used mainly by gynecologists [14].
The rationale for DTI without pneumoperitoneum is based on the difficulty of grasping and lifting the abdomen distended by the gas [11] and the fact that many complications reported during laparoscopic procedures are directly related to the use of the VN [4, 5]. According to Copeland et al., the keys to a successful DTI are an adequate wall relaxation, a proper skin incision, and the use of sharp trocars [4]. The introduction of shielded trocars has encouraged some surgeons to adopt DTI [7], but no experimental or clinical study has shown the superiority of the shielded trocar over the conventional one [11].
Randomized studies comparing the VN and DTI techniques have failed to show any advantage for either method in the overall population or in selected patients [11]. The only three prospective randomized studies published so far in the international literature [1, 2, 9] collected a total of 664 patients and showed that the only major complication occurred in the group of patients that did not have a pneumoperitoneum. Nonetheless, minor complications—mainly consisting of subcutaneous emphysema—were higher in the VN group. Theoretically, open laparoscopy should reduce the incidence of VN-related vascular and visceral injuries to nil [11].
The purported advantages of the OA are avoidance of blind puncture of a solid organ or a hollow viscus, certainty of establishing a pneumoperitoneum, and a correct repair of the abdominal port site entry. Use of the OA has been generally limited to patients with previous abdominal operations, pregnant patients, children, and very thin patients, where little space exists between the abdominal wall and the spine [11]. Nonetheless, the OA, takes longer to performed and associated with difficulty maintaining the peritoneum and a definite incidence of major intraabdominal injuries [11]. The incidence of visceral injuries after OA is similar to that reported for DTI, even though there are considerably fewer reports of vascular and bowel injuries with OA than the with the VM technique [11].
To date, there is no evidence in the international literature that the VN technique for creation of the pneumoperitoneum before trocar insertion is safer than DTI, or that DTI is superior in preventing major injuries in selected and unselected patients undergoing laparoscopic procedures. However, it is commonly agreed that thin patients, pregnant women, children, and patients with previous abdominal operations are at high risk for vascular and visceral injuries with the VN technique. Therefore, DTI stands as a safe alternative to both the VN and OA techniques and should be considered an integral part of the surgical armamentarium of a well-trained laparoscopic surgeon.
To assess the risk related to the mode of entry into the abdominal cavity in a population of nonobese patients undergoing laparoscopic procedures, we carried out an open comparative randomized, prospective trial comparing DTI and the VN technique that included urgent and elective procedures performed by surgeons trained in either of the two techniques. The DTI technique adopted was the one described elsewhere by Copeland et al. [4, 11]. For a successful DTI, it was paramount to have the patient thoroughly relaxed before making the skin incision, to make an adequate incision to allow passage of the trocar tip, to use a sharp trocar, and to apply constant pressure during penetration through the abdominal wall. Compliance with these principles could be the reason for the high feasibility rate of DTI in the current experience, the lack of conversions to OA, and the lack of major complications, even in thin patients with previous abdominal operations. Currently, none of the available modes of entry into the abdominal cavity is free of complications, and solid organs and hollow viscera are also prone to trocar injury during the entire course of the laparoscopic procedure [3, 6, 8, 14]. Actually, as compared with both DTI and OA, the VN technique entails two blind steps; thus, there is a risk of small lesions caused by needle placement going undetected on further trocar placement [13], and late or delayed recognition of intraabdominal injuries adds to the morbidity and mortality rates associated with the VN technique [11].
Any laparoscopic procedure carries a definite risk of major and minor complications related to the technique for abdominal access. The incidence of these complications cannot be eliminated, given the limits of current instrumentation and the effect of the learning curve. Our experience shows that in a population of thin and very thin patients of any age category, DTI is safe, has a slightly higher feasibility rate as compared with VN technique, and is associated with fewer minor complications, such as subcutaneous emphysema and extraperitoneal insufflation. There are no differences between DTI and the technique VN in the incidence of major complications. Our results do not provide evidence of the superiority of either technique for abdominal entry in thin patients, but rather demonstrate the needed for compliance with the basic tenets of laparoscopic surgery to avoid unnecessary complications.
References
L Borgatta L Gruss D Barad (1990) ArticleTitleDirect trocar insertion vs. Veress needle use for laparoscopic sterilization J Reprod Med 35 891–894 Occurrence Handle1:STN:280:DyaK3M%2FjvFSrsQ%3D%3D Occurrence Handle2146389
JW Byron G Markenson K Miyazawa (1993) ArticleTitleA randomized comparison of Veress needle and direct trocar insertion for laparoscopy Surg Gynecol Obstet 177 259–262 Occurrence Handle1:STN:280:DyaK3szmt1Sgug%3D%3D Occurrence Handle8356499
M Catarci M Carlini P Gentileschi E Santoro (2001) ArticleTitleMajor and minor injuries during the creation of pneumoperitoneum: a multicenter study on 12,919 cases Surg Endosc 15 566–569 Occurrence Handle1:STN:280:DC%2BD3MrksV2nsw%3D%3D Occurrence Handle10.1007/s004640000381 Occurrence Handle11591941
C Copeland R Wing JF Huka (1983) ArticleTitleDirect trocar insertion at laparoscopy: an evaluation Obstet Gynecol 62 665–669
JR Dingfelder (1978) ArticleTitleDirect laparoscope trocar insertion without prior pneumoperitoneum J Reprod Med 21 45–47 Occurrence Handle1:STN:280:DyaE1M%2FgslelsQ%3D%3D Occurrence Handle151144
MT Jacobson J Osias R Bizhang M Tsang S Lata M Helmy C Nezhat et al. (2002) ArticleTitleThe direct trocar technique: an alternative approach to abdominal entry for laparoscopy JSLS 6 169–174 Occurrence Handle12113423 Occurrence Handle3043410
JC Jarrett Suffix2nd (1990) ArticleTitleLaparoscopy: direct trocar insertion without pneumoperitoneum Obstet Gynecol 75 725–727 Occurrence Handle2138267
D Molloy PD Kaloo M Cooper TV Nguyen (2002) ArticleTitleLaparoscopic entry: a literature review and analysis of technique and complications of primary port entry Aust N Z J Obstet Gynaecol 42 246–254 Occurrence Handle10.1111/j.0004-8666.2002.00246.x Occurrence Handle12230057
FR Nezhat SL Silfen D Evans C Nezhat (1991) ArticleTitleComparison of direct insertion of disposable and standard reusable laparoscopic trocars and previous pneumoperitoneum with Veress needle Obstet Gynecol 78 148–150 Occurrence Handle1:STN:280:DyaK3M3mtFehtQ%3D%3D Occurrence Handle1828549
AJ Penfield (1985) ArticleTitleHow to prevent complications of open laparoscopy J Reprod Med 30 660–663 Occurrence Handle1:STN:280:DyaL28%2FjslWjsw%3D%3D Occurrence Handle2932552
PA Philips FA Amaral (2001) ArticleTitleAbdominal access complications in laparoscopic surgery J Am Coll Surg 192 525–536 Occurrence Handle1:STN:280:DC%2BD3M3ivFSrsg%3D%3D Occurrence Handle10.1016/S1072-7515(01)00768-2 Occurrence Handle11294410
JL Ponsky (1991) ArticleTitleComplications of laparoscopic cholecystectomy Am J Surg 161 393–395 Occurrence Handle1:STN:280:DyaK3M7lvVSqsQ%3D%3D Occurrence Handle10.1016/0002-9610(91)90605-D Occurrence Handle1825765
M Schafer M Lauper L Krahenbuhl (2001) ArticleTitleTrocar and Veress needle injuries during laparoscopy Surg Endosc 15 275–280 Occurrence Handle1:STN:280:DC%2BD38%2FgvFyjtQ%3D%3D Occurrence Handle10.1007/s004640000337 Occurrence Handle11344428
MA Yerdel K Karayalcin A Koyuncu B Akin C Koksoy AG Turkcapar N Erverdi et al. (1999) ArticleTitleDirect trocar insertion versus Veress needle insertion in laparoscopic cholecystectomy Am J Surg 177 247–249 Occurrence Handle1:STN:280:DyaK1M3jsFaksg%3D%3D Occurrence Handle10.1016/S0002-9610(99)00020-3 Occurrence Handle10219864
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agresta, F., De Simone, P., Ciardo, L.F. et al. Direct trocar insertion vs veress needle in nonobese patients undergoing laparoscopic procedures: a randomized prospective single-center study. Surg Endosc 18, 1778–1781 (2004). https://doi.org/10.1007/s00464-004-9010-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-9010-y