Abstract
Background
Although Roux-en-Y gastric bypass (RYGB) is an effective and widely used therapy for severe obesity, the mechanisms by which it induces weight loss are not well understood. Several studies have shown that RYGB in human patients causes a decrease in circulating levels of ghrelin, a gastric hormone that strongly stimulates food intake. Substantial variation in the effect of RYGB on serum ghrelin has been reported in different studies and among individual patients, suggesting that regulation of this hormone is complex and subject to genetic and other patient-specific factors. To control for these factors and to enable more detailed study of physiologic mechanisms, we have recently developed a clinically relevant rat model of RYGB. In this study, we used this model to examine the effect of RYGB on serum ghrelin levels.
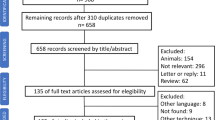
Methods
Fifteen Sprague-Dawley rats that had received a high-fat diet to induce moderate obesity underwent RYGB. The operation closely resembled the procedure in humans. Serum samples were collected 1 month before and 3 months after RYGB, and serum ghrelin levels were measured. The primary outcomes of the study were the changes in body weight, food intake, and circulating ghrelin levels after RYGB. A multiple linear regression model was developed to examine the relationship between ghrelin levels and weight change after RYGB.
Results
Three months after the procedure, RYGB-treated rats weighed 20 ± 5% less than they would have, had they not undergone the procedure. Despite the weight loss, serum ghrelin levels were 38 ± 6% lower than before surgery. There was appreciable variation in the weight loss in individual animals, and preoperative weight and pre- and postoperative ghrelin levels were the best predictors of postoperative weight loss. Thus, the animals who had the greatest weight loss were those that were heaviest before surgery. These rats had the highest preoperative and lowest postoperative ghrelin levels.
Conclusions
Using our recently developed rat model of RYGB, we found that postoperative weight loss is correlated with the magnitude of the decrease in circulating ghrelin levels. This correlation provides the strongest evidence to date that altered ghrelin signaling contributes to weight loss after this operation. The lower level of circulating ghrelin after RYGB likely blunts the appetitive drive, leading to decreased food intake in these animals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Following its introduction 50 years ago, gastrointestinal weight loss surgery was shown to induce substantial weight loss that is maintained over decades [4, 9, 18]. Among the several different weight loss operations that have been developed, Roux-en-Y gastric bypass (RYGB) is the most common and most effective procedure now performed in the United States [3, 18, 19]. After this operation, patients initially lose an average of 65–75% of their excess body weight, and most maintain this loss over the long term [19].
Despite the proven effectiveness of RYGB, however, the precise mechanisms of the resulting weight loss remain obscure. Understanding these mechanisms would provide a clearer path toward the development of effective but less invasive treatments for obesity. Historically, RYGB has been considered to induce weight loss primarily as a result of mechanical restriction and malabsorption [9]. However, recent evidence suggests that the effects of RYGB are more physiological than mechanical. Studies in human patients have shown that RYGB leads to decreased intensity of hunger, increased frequency of satiety, and an enhanced behavioral response to hunger and satiety [2, 7]. These behavioral changes themselves promote decreased food intake and consequent weight loss, in contrast to a purely anatomic model in which decreased food intake is imposed on the patient by mechanical restriction. Recent data suggest that even the decreased energy expenditure normally observed after diet-induced weight loss may be absent after RYGB and that this procedure may therefore cause a relative increase in energy expenditure [10, 21]. Thus, it appears that RYGB leads to physiological changes that differ fundamentally from the effects of restrictive diets, which often induce counterregulatory responses (increased hunger and decreased energy expenditure) that serve to promote regain of the lost weight.
To define the physiological and molecular mechanisms of RYGB-induced weight loss, we have recently developed a novel rat model of RYGB that does not interfere with long-term health and survival [20]. In this study, we examined the effect of RYGB on circulating levels of ghrelin. Ghrelin is a 28-amino acid peptide secreted primarily by the stomach and is the most potent appetite-stimulating hormone currently known [12, 13, 17]. In humans, circulating ghrelin levels increase before, and decrease immediately after, each meal, suggesting that ghrelin is a physiologically relevant regulator of food intake [7, 23]. Recent studies suggest that ghrelin also plays a significant role in the long-term regulation of body weight [17]. There is a high concentration of ghrelin receptors in orexigenic neuropeptide Y neurons in the arcuate nucleus of the hypothalamus, and ghrelin appears to stimulate food intake and promote weight gain by activating these neuronal circuits [1, 17]. Blockade of ghrelin-signaling in this region has been reported to decrease food intake, fat mass, and body weight [1].
In 2002, Cummings et al. reported markedly suppressed ghrelin levels in five patients who underwent RYGB; they suggested that these low levels may have contributed to the weight-reducing effect of the procedure [7]. Since this first report, however, other investigators have found that the effect of RYGB on circulating ghrelin is highly variable, ranging from postoperative ghrelin suppression, to stable values despite massive weight loss, to increased ghrelin levels similar to those observed after diet-induced weight loss [5–8, 12]. Although the causes of these varied findings are not fully understood, they may reflect differences in the operative techniques, the characteristics of the patients included in each study, the timing of the ghrelin measurements relative to the operation and postoperative weight loss, and other factors.
Because of the numerous methodological and ethical limitations inherent in performing detailed physiologic experiments in human subjects, we sought to examine the effects of RYGB on ghrelin in our novel animal model, which closely reproduces the effects of the human procedure as closely as possible and enables the operated animals to live full, healthy lives. Studies in this model avoid some of the heterogeneity in genetic background, operative procedures, and postoperative protocols that is inherent in human studies.
Materials and methods
We used a rat model of diet-induced obesity (DIO) because it has been well studied and is considered to be closely related to most forms of human obesity [22]. To create the DIO rat model, the nutrient environment is manipulated by placing wild-type rats on highly palatable diets that are enriched in fat.
Male Sprague-Dawley rats (Harlan Sprague Dawley, Indianapolis, IN, USA) were obtained at weaning (postpartum day 21). The animals were housed individually and maintained on a 12-h light–dark cycle (lights on at 0700 h) in a facility with an ambient temperature of 19–22°C and 40–60% humidity. Sixty rats were placed on a high-fat diet (HFD) that provides 60% of total energy as fat, 20% as carbohydrate, and 20% as protein (Research Diets, New Brunswick, NJ, USA). After 16 weeks on the HFD, the 40 rats with the highest body weight gain were designated as DIO [16]. Fifteen of the DIO rats were randomly selected to undergo RYGB. The operation in rats closely resembles the human procedure. In the rodents, the stomach is transected distal to the ridge that separates the forestomach from the glandular stomach. A Roux-en-Y gastrojejunostomy is then fashioned with a 10-cm Roux limb and a biliopancreatic limb that extends 15–18 cm distal to the ligament of Treitz (Fig. 1).
Roux-en-Y gastric bypass in the rat. A Creation of the gastrojejunostomy. Intraoperative photography showing the gastric pouch (GP), the Roux limb (RL), and the side-to-end gastrojejunostomy (G-J), which is hand-sewn using a running 6-0 silk suture. B Creation of the jejunojejunal anastomosis. Intraoperative view showing the Roux limb (RL), the biliopancreatic limb (BPL), and the end-to-side jejunojejunostomy (J-J), which is also hand-sewn using a running 6-0 silk suture.
Rats were fasted for 24 h before the operation. An elevated wire rack was placed on the bottom of each cage to prevent the animals from ingesting cage bedding and excreted products during the immediate postoperative period. Blood samples were collected 1 month before and 3 months after RYGB. Blood was obtained from a tail vein. The serum was stored in a –80°C freezer until assays were performed. Serum ghrelin levels were measured using a commercially available radioimmunoassay kit (Phoenix Pharmaceuticals, Belmont, CA, USA) according to the manufacturer’s instructions. For each of the duplicate assays, 10 μL of rat serum was used.
The primary outcome examined in this study was the change in serum ghrelin levels after RYGB. A multiple linear regression model was developed to examine the relationship between ghrelin levels and weight change after RYGB. All statistical analyses were performed using the software SPSS Graduate Pack 11.0 for Windows (SPSS, Chicago, IL, USA).
All interventions were performed in compliance with and were approved by the Institutional Animal Care and Use Committee of the Massachusetts General Hospital (MGH Subcommittee on Research Animal Care).
Results
Three months after the procedure, the RYGB-treated rats weighed 20 ± 5% less than their predicted weight had they not undergone the procedure [15, 16] (Fig. 2). Unlike untreated male rats, which continue to gain weight exponentially during adult life, the weight of RYGB-treated animals remained completely stable after transient fluctuations in the early postoperative period. Three months after RYGB, their stable weight was 9 ± 3% less than their preoperative weight and 20% less than the weight of nonoperated controls. In the first several weeks after surgery, RYGB-treated rats lost ~25% of their initial body weight. Immediately thereafter, they regained half of the lost weight, suggesting that some of these early weight changes reflected the catabolic effects of the operation and subsequent recovery. Beginning at 10 weeks after the operation, there was no significant change in body weight.
Weight loss after Roux-en-Y gastric bypass (RYGB) in Sprague-Dawley rats. Three months after the procedure, the RYGB-treated rats weighed on average 9% less than their preoperative weight and 20% less than their expected weight had they not undergone the procedure. The dashed line represents the typical growth curve of Sprague-Dawley rats on a high-fat diet; the curve reflects published data [15, 16].
Three months after the operation, plasma ghrelin levels in the RYGB-treated rats were 38 ± 6% (range, 11–76%) lower than their preoperative levels. Ghrelin levels were decreased in all but one rat (Fig. 3).
Using a linear regression model, we found that the best predictors of weight loss in individual animals were preoperative weight, time since the operation, and the preoperative and postoperative ghrelin levels. Preoperative weight and preoperative ghrelin levels were directly correlated with weight loss, whereas postoperative ghrelin and time after the operation were inversely correlated. The linear regression model that best predicts the weight loss after surgery can be summarized as follows:
In this equation, Wpre is the weight before RYGB, Wpost is the weight after RYGB, PreGhrelin and PostGhrelin are the ghrelin levels before and after RYGB, respectively, and Time is the time (in days) after RYGB.
The partial correlation coefficients that determine the relative importance of the individual predictors were –0.792 for Wpre, 0.865 for PostGhrelin, 0.892 for Time, –0.556 for PreGhrelin, and 0.767 for the variable [Wpre] x [Time] x [PreGhrelin].
The variable [Wpre] x [Time] x [PreGhrelin] represents a statistically significant, three-way interaction above and beyond the individual contributions of these three factors. Such interactions occur when the effect of one variable differs depending on the levels of one or more other variables. Here, for example, the effect of preoperative ghrelin level on postoperative weight loss is different depending on the preoperative weight and time after surgery. This interaction is expressed by the fourth variable [Wpre] x [Time] x [PreGhrelin].
To illustrate the clinical significance of this interaction variable, we plotted it against percent weight loss (Fig. 4). The values commonly examined by investigators are the mean of the variables, one SD below it, and one SD above it. All combinations of these values are used to plot the interaction among the variables, and six lines are usually sufficient to illustrate the trends. As shown in Fig. 4, the plot of the three-way interaction variable suggests that the heaviest animals with the highest preoperative and lowest postoperative ghrelin levels had the greatest weight loss after RYGB.
Predictors of weight loss after Roux-en-Y gastric bypass. Illustration of the relationships among predictors identified by linear regression analysis. The relationship between postoperative weight loss and preoperative serum ghrelin is modulated by two additional variables: preoperative weight and postoperative levels of serum ghrelin. The heaviest animals with the highest preoperative ghrelin levels and lowest postoperative serum ghrelin are predicted to have the greatest weight loss after the gastric bypass procedure (line A), whereas the lightest animals with the lowest preoperative ghrelin and highest preoperative ghrelin will have the least weight loss (line F).
Discussion
In this study using a novel rat model of RYGB recently developed in our laboratory, we found that RYGB induces substantial weight loss, followed by a long-term stable weight that is atypical for untreated animals. Three months after surgery, RYGB-treated rats weighed 20–30% less than untreated animals of comparable age and initial body weight. Thus, weight changes in this rat model are comparable to the well-described effect of RYGB in human patients [20]. In addition, we found that weight loss after operation is associated with a substantial decrease in circulating ghrelin levels. It is important to note that we examined the ghrelin levels 3 months after the operation, when the body weight of the treated rats had stabilized and no further weight change was likely to occur.
Several authors have suggested that the effect of RYGB on circulating ghrelin levels depends on the dynamic status of weight loss [5–8, 12]. In several human studies, post-RYGB ghrelin levels were decreased in patients whose weights had leveled off, whereas patients who were still losing weight had higher levels (either equal to or higher than preoperative levels). One interpretation consistent with the observed findings is that weight loss (from any cause) increases serum ghrelin levels whereas RYGB reduces them. The overall effect of RYGB on circulating ghrelin concentration in individual patients, and the size of this effect, varies depending on the patient’s genetic background and other unknown factors. In our inbred population of rats, the effect of variable genetic influences was minimized by the homogeneity of the animal population.
The heaviest animals with the highest preoperative and lowest postoperative ghrelin levels had the greatest weight loss after RYGB. Thus, the magnitude of the decrease in circulating ghrelin levels predicts postoperative weight loss. This finding suggests that ghrelin signaling is directly involved in the physiological effects of RYGB and provides further support for the hypothesis that weight loss results more from the physiological effects of this operation than from mechanical effects. Although it has often been assumed that food intake after RYGB is reduced because of physical restriction of the gastric reservoir, these observations support the conclusions from human studies that the decrease in food intake likely results from diminished hunger, in part as a consequence of lower levels of circulating ghrelin, leading to diminished stimulation of orexigenic neurons in the arcuate nucleus [2, 7, 9].
Because ghrelin represents only one means of communication between the gastrointestinal (GI) tract and central nervous system (CNS), a reduced ghrelin level is unlikely to be the sole mechanism by which RYGB induces weight loss. Communication between the GI tract and the CNS is complex, and several other signaling molecules and pathways are likely to be involved in RYGB-induced weight loss. Because weight loss after purely restrictive procedures, such as adjustable gastric banding (AGB) and vertical banded gastroplasty (VBG), is associated with elevated circulating ghrelin levels, non–ghrelin-related mechanisms must be invoked to explain their effects [11, 14]. Because RYGB includes a gastric restrictive component, it is likely that one or more of the mechanisms used by AGB and VBG contribute to weight loss after RYGB as well. The availability of this rat model should facilitate the identification of these additional pathways.
In conclusion, we have developed a novel rat model for RYGB and have begun to explore the mechanisms by which RYGB induces weight loss. Despite the known differences between humans and rats in gastrointestinal anatomy and food intake patterns, the similar responses of body weight and ghrelin levels to RYGB in the two species suggests strong conservation of the relevant weight regulatory mechanisms. These observations support usefulness of this animal model for exploring the physiological mechanisms of weight loss after RYGB in more detail.
Using the rat RYGB model, we have shown that RYGB is associated with a decrease in circulating ghrelin levels, the magnitude of which predicts postoperative weight loss. The close relationship between postoperative decrease in ghrelin levels and weight loss provides the strongest evidence to date that altered ghrelin signaling contributes to gastric bypass–induced weight loss. It is virtually certain that other weight regulatory pathways are also affected by this operation, and this rat model provides a valuable tool for their discovery and characterization.
References
A Asakawa A Inui T Kaga H Yuzuriha T Nagata N Ueno S Makino et al. (2001) ArticleTitleGhrelin is an appetite-stimulatory signal from stomach with structural resemblance to motilin Gastroenterology 120 637–345 Occurrence Handle10.1053/gast.2001.22158
CW Baker LM Kaplan (2003) ArticleTitleThe impact of gastric surgery on hunger, satiety and non-hunger–related desire to eat Obes Res 11 A109–A110
BM Balsiger FP Kennedy HS Abu-Lebdeh M Collazo-Clavell MD Jensen T O’Brien DD Hensrud et al. (2000) ArticleTitleProspective evaluation of Roux-en-Y gastric bypass as primary operation for medically complicated obesity Mayo Clin Proc 75 673–680 Occurrence Handle10907381
RE Brolin (2002) ArticleTitleBariatric surgery and long-term control of morbid obesity JAMA 288 2793–2796 Occurrence Handle10.1001/jama.288.22.2793 Occurrence Handle12472304
PM Copeland P Davis LM Kaplan (2003) ArticleTitleWeight loss after gastric bypass is associated with decreased plasma gastric inhibitory polypeptide without a significant change in circulating ghrelin Obes Res 11 A17–A18
DE Cummings JQ Purnell RS Frayo K Schmidova BE Wisse DS Weigle (2001) ArticleTitleA preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans Diabetes 50 1714–1719 Occurrence Handle11473029
DE Cummings DS Weigle RS Frayo PA Breen MK Ma EP Dellinger JQ Purnell (2002) ArticleTitleHuman plasma ghrelin levels after diet-induced weight loss and gastric bypass surgery N Engl J Med 346 1623–1630 Occurrence Handle10.1056/NEJMoa012908 Occurrence Handle12023994
M Faraj PJ Havel S Phelis D Blank AD Sniderman K Cianflone (2003) ArticleTitlePlasma acylation–stimulating protein, adiponectin, leptin, and ghrelin before and after weight loss induced by gastric bypass surgery in morbidly obese subjects J Clin Endocrinol Metab 88 1594–1602 Occurrence Handle10.1210/jc.2002-021309 Occurrence Handle12679444
BL Fisher P Schauer (2002) ArticleTitleMedical and surgical options in the treatment of severe obesity Am J Surg 184 9S–16S Occurrence Handle10.1016/S0002-9610(02)01173-X Occurrence Handle12527344
L Flancbaum PS Choban LR Bradley JC Burge (1997) ArticleTitleChanges in measured resting energy expenditure after Roux-en-Y gastric bypass for clinically severe obesity Surgery 122 943–949 Occurrence Handle10.1016/S0039-6060(97)90336-6 Occurrence Handle9369895
U Hanusch-Enserer G Brabant M Roden (2003) ArticleTitleGhrelin concentrations in morbidly obese patients after adjustable gastric banding N Engl J Med 348 2159–2160 Occurrence Handle10.1056/NEJM200305223482125
C Holdstock BE Engstrom M Ohrvall L Lind M Sundborn FA Karlsson (2003) ArticleTitleGhrelin and adipose tissue regulatory peptides: effect of gastric bypass surgery in obese humans J Clin Endocrinol Metab 88 3177–3183 Occurrence Handle10.1210/jc.2002-021734 Occurrence Handle12843162
M Kojima H Hosoda Y Date M Nakazato H Matsuo K Kangawa (1999) ArticleTitleGhrelin is a growth hormone–releasing acylated peptide from stomach Nature 402 656–660 Occurrence Handle10.1038/45230 Occurrence Handle10604470
F Leonetti G Silecchia G Iacobellis MC Ribaudo A Zappaterreno C Tiberti CV Iannucci et al. (2003) ArticleTitleDifferent plasma ghrelin levels after laparoscopic gastric bypass and adjustable gastric banding in morbid obese subjects J Clin Endocrinol Metab 88 4227–4231 Occurrence Handle10.1210/jc.2003-030133 Occurrence Handle12970291
BE Levin RE Keesey (1998) ArticleTitleDefense of differing body weight set points in diet-induced obese and resistant rats Am J Physiol 274 R412–R419 Occurrence Handle9486299
BE Levin AA Dunn-Meynell B Balkan RE Keesey (1997) ArticleTitleSelective breeding for diet-induced obesity and resistance in Sprague-Dawley rats Am J Physiol 273 R725–R730 Occurrence Handle9277561
M Nakazato N Murakami Y Date M Kojima H Matsuo K Kangawa S Matsukura (2001) ArticleTitleA role for ghrelin in the central regulation of feeding Nature 409 194–198 Occurrence Handle10.1038/35051587 Occurrence Handle11196643
WJ Pories MS Swanson KG MacDonald SB Long PG Morris BM Brown HA Barakat et al. (1995) ArticleTitleWho would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus Ann Surg 222 339–352 Occurrence Handle7677463
PR Schauer S Ikramuddin W Gourash R Ramanathan J Luketich (2000) ArticleTitleOutcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity Ann Surg 232 515–529 Occurrence Handle10.1097/00000658-200010000-00007 Occurrence Handle10998650
N Stylopoulos J Pettit DW Rattner LM Kaplan (2003) ArticleTitleLong-term weight loss after gastric bypass surgery in rats is proportional to the degree of excess body weight Obes Res 11 A20
N Stylopoulos SM Maithel DB Jones DW Rattner LM Kaplan (2004) ArticleTitleIncreased energy expenditure accounts for a substantial-portion of the weight loss after Roux-en-Y gastric bypass in rats Gastroenterology 126 A90 Occurrence Handle10.1053/j.gastro.2003.10.014
M Tschop ML Heiman (2001) ArticleTitleRodent obesity models: an overview Exp Clin Endocrinol Diabetes 109 307–319 Occurrence Handle10.1055/s-2001-17297 Occurrence Handle11571668
M Tschöp R Wawarta RL Riepl S Friedrich M Bidlingmaier R Landgraf C Folwaczny (2001) ArticleTitlePost-prandial decrease of circulating human ghrelin levels J Endocrinol Invest 24 RC19–RC21 Occurrence Handle11434675
Acknowledgments
This work was supported by grants DK99010, DK43351, and DK46200 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stylopoulos, N., Davis, P., Pettit, J.D. et al. Changes in serum ghrelin predict weight loss after Roux-en-Y gastric bypass in rats. Surg Endosc 19, 942–946 (2005). https://doi.org/10.1007/s00464-004-8825-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8825-x