Abstract
Percutaneous endoscopic gastrostomy (PEG) is a widely used procedure for patients who cannot swallow. Athough it is mostly performed for valid indications, its use in terminally ill patients is questionable. In this study, more than 30% of patients died in hospital after PEG placement and 16% died less than 30 days after placement. Strict guidelines and oversight or PEG placement are recommended.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Percutaneous endoscopic gastrostomy (PEG) introduced in 1980 for enteral feeding [9, 16] simplified a previously complex operative procedure and deservedly achieved widespread clinical usage. In the United States alone, well over 100,000 such procedures are performed annually. Questions have been raised, however, about the ethical propriety of PEG when the burdens and risks of the procedure outweigh the benefits [5, 7, 10, 19, 20]. There is no scarcity of literature dealing with appropriate and inappropriate usage of PEG. There is, however, inadequate consideration of measures that might reduce the number of inappropriate PEGs.
This article describes PEG usage in a general hospital from the bioethical perspective and suggests measures that might be effective in offsetting such usage when the indications are ethically questionable.
Materials and methods
At an 876-bed voluntary, tertiary care teaching hospital located in a large metropolitan area, approximately 400 PEGs are performed each year. The hospital also has an active bioethics program, which encourages bioethics consultations when indicated for ethical conflicts or dilemmas. Consultation requests may be initiated by the patient, the patient’s family, or any member of the health care team (attending physicians, residents, nurses, or social workers). The consultation team consists of a doctor and nurse, who are members of the Bioethics Committee, and the social worker assigned to the case. The consultation is held with the patient, family, or surrogates with the full knowledge and participation of the patient’s attending physician.
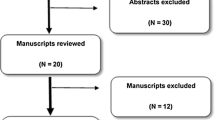
We retrospectively reviewed 503 bioethical consultations that took place between 1999 and 2002. Within this group of 503, we identified 147 patients who had PEG placement either before or during their hospitalization. This group was analyzed for demographic data, indications for PEG placement, outcomes, and timing of PEG placement relative to the request for bioethical consultation.
Results
Of the 503 bioethical consultations, 29% (147/503) involved patients who had undergone PEG during the period under study. The mean age of the patients was 74.6 years (median, 81 years). Males comprised 38% of the patients, and females represented 62%. Indications for PEG placement were varied. The majority (86%) were placed for conditions involving neurologic impairment which precluded oral intake, including stroke, head trauma, cerebral hypoxia, persistent vegetative state, and dementia. The remainder (14%), were placed for cancer or miscellaneous causes.
Outcomes
For 65% (95/147) of the patients, PEG placement was at the same admission as their bioethical consultation. Of these, 31% (29/95) died in the hospital. Their mean survival time was of 31 days. However, 16% of the patients, (15/95), died fewer than 30 days after PEG placement. Most of the bioethical consultation requests (79%) were made after PEG placement
Discussion
The number of PEGs in this institution are consistent with those reported in other published studies. The numbers are striking. One large study [11] of Medicare beneficiaries reported an incidence 0.8% among hospitalized whites 85 years or older, and 1.7% among hospitalized blacks in the same age group. As life expectancy continues to lengthen, these numbers probably will increase.
Gauderer [8], the acknowledged originator of the procedure, wrote a 20-year retrospective evaluation of the procedure, in which he stated:
“...Because of its simplicity and low complication rate, this minimally invasive procedure also lends itself to overutilization. Therefore, as percutaneous endoscopic gastrostomy enters its third decade, much of our effort in the future needs to be directed toward the ethical aspects associated with long-term enteral feeding. In addition to developing new procedures and devices, or to perfecting existing ones, we as physicians must continuously strive to demonstrate that our interventions truly benefit the patient.” (p. 882)
Many reports have described, discussed, and debated the ethical issues in PEG placement [3, 13, 18, 21]. The utility and appropriateness of the procedure for reversible or reparable conditions in which oral nutrition and hydration are impaired temporarily for prolonged periods is incontrovertible. The decision becomes more difficult in situations that involve advanced dementia, terminal malignancy, a persistent vegetative state, irreversible coma, or similar states. Clouding the decision-making process are the uncertainty of precise prognostication and prevalent multicultural attitudes toward nutrition and hydration.
There are authorative guidelines for the use of PEGs, such as those delineated in the Guidelines for the Use of Enteral Nutrition: A Medical Position Statement of the American Gastroenterological Association [2]. Among these guidelines is the constraint that PEG is justified for patients who need tube feeding more than 30 days, implying that the less interventional nasogastric tube should be used if tube feeding for a shorter time is either predictable or prognosticated.
Nevertheless, despite the extensive literature and the clear guidelines, 15% of the patients (16% in this series) who have PEG placement survive fewer than 30 days. In these cases, it may be assumed that the PEG placement was inappropriately offered or requested although, occasionally, extenuating circumstances may have been present.
Illustrative cases
Terminal hepatorenal syndrome
A 63 year-old woman had a long history of severe diabetes and cirrhosis of the liver with multiple serious complications, including chronic renal failure requiring renal dialysis. After 5 years of dialysis, progressive jaundice, developed resulting finally in a full-blown hepatorenal syndrome. During 4 weeks in the hospital, the patient’s clinical status worsened markedly. A PEG was placed 6 days before she died.
Cerebro-vascular accident, advanced dementia
A 58-year-old African American man with advanced dementia was admitted after a grand mal seizure attributable to a cerebrovascular accident. He experienced multiple organ system (renal, respiratory, cerebral) failure. Because his mental status precluded oral feeding, the family insisted on placement of a PEG. He died 10 days after PEG placement.
Severe cerebral trauma in an aged woman
An 89-year-old woman severely impaired in an auto accident had multiple fractures (ribs, pelvis, scapula), and a large subdural hematoma. Acute respiratory distress syndrome, renal failure, and pneumonia subsequently developed. The patient had expressed before the accident that she had no desire for life support if she could not live independently. A PEG was by placed 2 weeks before her death caused by overwhelming sepsis.
None of these cases had the benefit of bioethics consultation, which would have allowed a full discussion of the burdens and benefits of the procedure, as well as the goals of the intervention.
What corrective measures might reduce the inappropriate placement of PEGs? First, we advocate education. All physicians who recommend or place PEGs should be familiar with the published guidelines of the American Gastroenterological Association for PEG placement. These are explicit in stating that “gastrostomy tubes are justified for patients who need tube feeding for more than 30 days.” A technical review by the same organization [2] expands the indications to include, for example, “untreatable bowel obstruction due to cancer, or expressed patient preference over nasogastric intubation, even when death is imminent.” Also recommended is the involvement of hospital ethics committees when the indications are debatable, as well as education promoted in conferences, seminars, and suggested readings.
The education of patients and families on the burdens compared with the benefits of artificial nutrition and hydration (ANH) via PEG also is indicated. Informed consent should, but frequently does not, include the discussion of the complications in placement [4], and the risk of aspiration [4], as well as a frank description of the benefits as compared with the burdens [1,6, 12, 15, 17]. All too frequently, the option of a PEG is offered and eagerly accepted by surrogates who are not familiar with, or will not accept, the alternative of withholding ANH, fearing the consequences of unbearable thirst and hunger. These are not problematic when ANH is withheld or withdrawn. Both physicians and families should be aware of this alternative for patients facing imminent death or for patients with advanced dementia who have lost their ability to swallow and whose quality of life is severely compromised. In such cases, ANH may serve only to prolong the dying process, which may not be a desirable option.
Second, we advocate more frequent use of bioethics consultation when the indications are doubtful or debatable. Ethical dilemmas are optimally discussed in a group setting where in concerns are addressed, options are considered, and the burdens versus the benefits of a treatment are carefully considered. In our series, 79% of the bioethics consultations were requested at some time after PEG placement. In most instances, the consultation would have been more helpful before the procedure was performed, with the choices clearly defined. We have encountered instances in which PEG placement was being considered, or had already been performed despite an Advance Directive stating that it was against the patient’s wishes. In other cases of predictably near or imminent death, the PEG provided no benefit and arguably increased the burden of a prolonged dying process. As a general rule, bioethics consultation should always be requested when PEG is being considered for patients in a persistent vegetative state. The ethical dilemmas involved seriously require discussion.
Finally, we recommend that there be a periodic departmental audit (by the gastroenterology or surgery department) or peer review of PEG placement cases. Currently, to our knowledge, no such audit exists in our hospital or any others. Audit and peer review would bring to light repeat offenders responsible for inappropriate placement, and would facilitate the institution of corrective measures. The PEG placement procedure poses sufficient ethical dilemmas for it to be worthy of more intensive oversight.
Conclusions
Percutaneous endoscopic gastrostomy has been a remarkably successful method of enteral feeding, one that is highly preferable to previous surgical procedures. Its placement is ethically and medically appropriate in most cases for which it is used. However, a residue of cases remains in which placement of a PEG is either debatable or inappropriate. To reduce this latter category to a minimum, we recommend a more effective education program, periodic audit and peer review, and increased usage of bioethics consultations.
References
InstitutionalAuthorNameAckerman TF (1996) ArticleTitleThe moral implications of medical uncertainty: tube feeding demented patients (editorials) J Am Geriatr Soc 44 1265–1267
AGA guideline: Enteral nutrition (1994) UpToDate Online 10.3. Retrieved at http://www.uptodate.com, Access Date: February 13, 2003
F Angus R Burakoff (2003) ArticleTitleThe percutaneous endoscopic gastrostomy tube: medical and ethical issues in placement Am J Gastroenterol 98 272–277 Occurrence Handle12591040
AS Brett JC Rosenberg (2001) ArticleTitleThe adequacy of informed consent for placement of gastrostomy tubes Arch Intern Med 161 745–748 Occurrence Handle10.1001/archinte.161.5.745 Occurrence Handle1:STN:280:DC%2BD3M3jsFGjtA%3D%3D Occurrence Handle11231709
CM Callahan KM Haag NN Buchanan R Nisi (1999) ArticleTitleDecision making for percutaneous endoscopic gastrostomy among older adults in a community setting J Am Geriat Soc 47 1105–1109 Occurrence Handle1:STN:280:DyaK1Mvht1Smtw%3D%3D Occurrence Handle10484254
AM Easson DB Hinshaw DL Johnson (2002) ArticleTitleThe role of tube feeding and total parenteral nutrition in advanced illness J Am Coll Surg 194 225–228 Occurrence Handle10.1016/S1072-7515(01)01154-1 Occurrence Handle11848638
TE Finucane C Christmas K Travis (1999) ArticleTitleTube feeding in patients with advanced dementia: a review of the evidence (special communication) JAMA 282 1365–1370 Occurrence Handle10.1001/jama.282.14.1365 Occurrence Handle1:STN:280:DyaK1MvlsVejug%3D%3D Occurrence Handle10527184
M Gauderer (1999) ArticleTitleTwenty years of percutaneous endoscopic gastrostomy: origin and evolution of a concept and its expanded applications (editorials) Gastrointest Endosc 50 IssueID6 882
MWL Gauderer JL Ponsky RJ Izant SuffixJr (1980) ArticleTitleGastrostomy without laparotomy: a percutaneous endoscopic technique J Pediatr Surg 15 872–875 Occurrence Handle1:STN:280:Bi6C3Mbks1Y%3D Occurrence Handle6780678
MR Gillick (2000) ArticleTitleRethinking the role of tube feeding in patients with advanced dementia (sounding board) N Engl J Med 342 206–210 Occurrence Handle10.1056/NEJM200001203420312 Occurrence Handle1:STN:280:DC%2BD3c%2Fpt1eluw%3D%3D Occurrence Handle10639550
MD Grant MA Rudberg JA Brody (1998) ArticleTitleGastrostomy placement and mortality among hospitalized medicare beneficiaries (original contributions) JAMA 279 1973–1976 Occurrence Handle10.1001/jama.279.24.1973 Occurrence Handle1:STN:280:DyaK1czgs1Sitg%3D%3D Occurrence Handle9643861
DE Larson DD Burton KW Schroeder EP DiMagno (1987) ArticleTitlePercutaneous endoscopic gastrostomy: indications, success, complications, and mortality in 314 consecutive patients Gastroenterology 93 48–52 Occurrence Handle1:STN:280:BiiB3MbntlI%3D Occurrence Handle3108063
SB Mackie (2001) ArticleTitlePEGs and ethics (features) Gastroenterol Nurs 24 138–142 Occurrence Handle10.1097/00001610-200105000-00007 Occurrence Handle1:STN:280:DC%2BD387hsV2ruw%3D%3D Occurrence Handle11847863
PE Marik (2001) ArticleTitleAspiration pneumonitis and aspiration pneumonia N Engl J Med 344 665–671 Occurrence Handle10.1056/NEJM200103013440908 Occurrence Handle1:STN:280:DC%2BD3M7ltVWmsg%3D%3D Occurrence Handle11228282
SL Mitchell FM Lawson (1999) ArticleTitleDecision making for long-term tube feeding in cognitively impaired elderly people (evidence) Can Med Assoc J 160 1705–1709 Occurrence Handle1:STN:280:DyaK1MzjvVyhsg%3D%3D
JL Ponsky MWL Gauderer (1981) ArticleTitlePercutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy Gastrointest Endosc 27 9–11 Occurrence Handle1:STN:280:Bi6C28rksV0%3D Occurrence Handle6783471
SG Post (1995) The moral challenge of Alzheimer disease: ethical issues from diagnosis to dying John Hopkins University Press Baltimore, MD
L Rabeneck LB McCullough NP Wray (1997) ArticleTitleEthically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement Lancet 349 496–498 Occurrence Handle10.1016/S0140-6736(96)07369-2 Occurrence Handle1:STN:280:ByiC1M3pvF0%3D Occurrence Handle9040591
L Rabeneck NP Wray NJ Petersen (1996) ArticleTitleLong-term outcomes of patients receiving percutaneous endoscopic gastrostomy tubes J Gen Intern Med 11 287–293 Occurrence Handle1:STN:280:BymA3sfmsF0%3D Occurrence Handle8725977
GMA Rosendaal ParticleVan MJ Verhoef TD Kinsella (1999) ArticleTitleHow are decisions made about the use of percutaneous endoscopic gastrostomy for long-term nutritional support? Am J Gastroenterol 94 3225–3228 Occurrence Handle10.1111/j.1572-0241.1999.01522.x Occurrence Handle10566719
HC Wolfsen RA Kozarek (1992) ArticleTitlePercutaneous endoscopic gastrostomy: ethical considerations Gastrointest Endosc Clin North Am 2 259–271
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morgenstern, L., Laquer, M. & Treyzon, L. Ethical challenges of percutaneous endoscopic gastrostomy. Surg Endosc 19, 398–400 (2005). https://doi.org/10.1007/s00464-004-8109-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8109-5