Abstract
Background
Laparoscopic procedures are increasing in number and extensiveness. Many patients undergoing laparoscopic surgery have coexisting disease. Especially in patients with cardiopulmonary comorbidity, pneumoperitoneum and positioning can be deleterious. This article reviews possible pitfalls related to the combination of anesthesia, positioning of the patient, and the influence of pneumoperitoneum in the course of laparoscopic interventions.
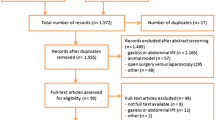
Methods
A literature search using Medline’s MESH terms was used to identify recent key articles. Cross-references from these articles were used as well.
Results
Patient positioning and pneumoperitoneum can induce hemodynamic, pulmonary, renal, splanchnic, and endocrine pathophysiological changes, which will affect the entire perioperative period of patients undergoing laparoscopic procedures.
Conclusion
Perioperative management for the estimation and reduction of risk of morbidity and mortality due to surgery and anesthesia in laparoscopic procedures must be based on knowledge of the pathophysiological disturbances induced by the combination of general anesthesia, pneumoperitoneum, and positioning of the patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Although endoscopy of the abdominal cavity was performed as early as 1911, it was not until the past few decades that laparoscopic surgery became common clinical practice [1]. Initially, the use of laparoscopic procedures was confined to small and rapid gynecological interventions such as sterilization and short diagnostic procedures. It was generally carried out in young and healthy women and often performed in a day-care setting. Recovery from anesthesia had to be rapid and with a minimum of residual effects. Therefore, laparoscopic procedures became a challenge to anesthesiologists.
New intraabdominal laparoscopic surgical techniques have since been developed and performed and are advocated for children and older patients also. In contrast to the young and healthy female, children may suffer from previously undiagnosed conditions such as congenital heart disease or an abnormal airway, whereas the older patients may have coexisting cardiac and/or pulmonary disease. Therefore, a careful preoperative evaluation and optimization of these patients should take place in order to decrease perioperative morbidity and mortality. Because these new procedures may involve extreme changes in patient position, extensive periods of intraabdominal carbon dioxide (CO2) insufflation, unexpected visceral injury, and difficulty in evaluating the amount of blood loss, anesthesia for laparoscopy can be considered a potentially high-risk procedure.
Since the early 1990s elaborate and timely laparoscopic procedures have been performed. Almost every abdominal organ now seems to be amenable to laparoscopic surgery [2–6]. All these laparoscopic procedures may induce major pathophysiological disturbances. Therefore, the anesthesiologist must choose an appropriate anesthetic management technique, apply adequate monitoring, and be aware of possible complications. In addition special attention must be given to the position of the patient on the operating table and to perioperative fluid management. Early detection and reduction of possible intraoperative problems may then be achieved. Finally, during the early postoperative period special attention must be paid to cardiovascular and pulmonary problems, postoperative nausea and vomiting, and pain management.
Preoperative evaluation
The main goal of preoperative medical assessment is the estimation and possible reduction of risk of morbidity and mortality due to surgery and anesthesia. Further aims are to increase the quality of peroperative care, to restore the patient to the desired level of function, and to obtain the patient’s informed consent for the anesthetic procedure [7]. The American Society of Anesthesiologists (ASA) classification score (Table 1) provides a simple description of the physical state and is one of the few prospective descriptions of the patient that correlates with the risks of anesthesia and surgery.
An ASA Task Force on “Practice Advisory for Preanesthesia Evaluation” recommends preoperative evaluation to include (1) readily accessible medical records, (2) patient interview, (3) a directed preanesthesia examination (Table 2, [8]), (4) preoperative tests when indicated (Table 3), and (5) other consultations when appropriate [9]. A directed preanesthetic physical examination should at least include an assessment of the airway, lungs, and heart [9].
Thus, the presence of coexisting medical disease must be identified, together with its extent and association with limiting normal daily activity in the patient. With respect to infants and children, preoperative examination must also identify previously undiagnosed conditions such as congenital heart disease [10].
All conventional complications and concerns of laparoscopy are applicable. In general pneumoperitoneum (PP) and laparoscopy are contraindicated in patients with increased cranial pressure, ventriculoperitoneal shunt, peritoneojugular shunt, hypovolemia, and congestive heart failure [11].
Intraoperative management
Anesthetic technique
Common side effects of laparoscopic procedures are irritation of the diaphragm due to the carbon dioxide insufflation for maintaining PP, significant nausea and vomiting, and referred pain in the distribution of the phrenic nerve. Although regional anesthesia has been applied successfully for laparoscopic cholecystectomy [12], general anesthesia is thought to be the technique of choice for laparoscopic procedures [13].
The combination of a generally uncomfortable position on the operating table together with a long-lasting procedure makes a state of wakefulness during laparoscopic surgery not very acceptable for patients. When regional anesthesia is combined with sedation, airway protection cannot be ensured, and respiratory depression with further induction of hypercapnia can be expected. The general anesthetic technique provides a secure airway, enables controlled mechanical ventilation with proper handling of the CO2 absorption that is induced by the PP, and facilitates management of muscle relaxation necessary to optimize the surgical view. In conclusion, general anesthesia is preferred over a regional technique for extensive laparoscopic procedures.
In children, anesthesia can be induced by inhalation of volatile anesthetics as well as with intravenous techniques [10]. Because of an increased intraabdominal pressure (IAP) due to the PP, i.v. access is preferred to ensure immediate onset of medication [10]. Furthermore, it seems better to intubate children <6 years of age with a cuffed endotracheal tube (this is usually avoided in this age group because of the small diameter of the trachea) to prevent ventilation difficulties due to the IAP increase [10].
Monitoring of patients
Cardiac events are the leading cause of death during and immediately after surgical procedures [14–16]. Perioperative morbidity also is associated with pulmonary complications and moderate hypothermia [17]. However, the rate of complications directly related to anesthesia is low [18].
Although guidelines and recommendations for monitoring standards are usually defined by the national societies of anesthesia, some basic aspects should be monitored in every patient regardless of the choice of anesthetic technique, type of surgery, or condition of the individual patient [19, 20]. Table 4 gives methods for the application of these basic monitoring standards.
Advanced monitoring consists of the measurement of cardiac filling pressure, cardiac output, and mixed venous oxygen saturation. The conventional monitoring of cardiac filling pressures requires central venous cannulation. Although complications due to cannulation are infrequent, they may result in severe morbidity [21]. Since laparoscopic procedures are also performed in the elderly, often cardiovascularly disabled ASA III or IV patients, such advanced monitoring may be necessary. However, when the cardiac function is impaired the relation between central venous pressure and cardiac preload is altered and the cardiac filling pressure measurements may not be reliable [22], In such cases insertion of a pulmonary artery catheter should be considered.
Transesophageal echocardiography (TEE) is a semiinvasive method of measuring cardiac performance and ventricular filling. The use of TEE in laparoscopic procedures is recommended for early detection of gasembolism and examination of a possible patent foramen ovale (PFO) [23]. The estimation of the prevalence of PFO in postmortem studies is 25% to 35% [24]. The clinical significance increases from 5–10% at basal in vivo conditions to 18–22% after sudden release of intrathoracic pressure, a situation that might be expected during laparoscopy [25]. Although the effect of regular TEE use on outcome is unknown, when used by experienced staff the complication rate of the technique is low [26]. Therefore, its use is recommended in subsets of patients, such as those having a known cause of hemodynamic instability [19].
Fluid management
Fluid management in laparoscopic surgery can be a dilemma for the anesthesiologist. Usually, patients enter the operating room after a time of fasting, most often at least 6 h. The patients’ circulatory status is therefore relatively hypovolemic, and anesthesia, whether general or regional, further increases the fluid debt.
Depending on the positioning of the patient in combination with PP, on the one hand a restrictive fluid regimen may be advantageous whereas on the other hand vital organ perfusion requires intravenous fluid loading.
The Trendelenburg, “head-down” position in itself causes increased venous return [27]. In combination with PP, this venous return may be even further increased due to compression of the splanchnic vasculature. In cardiovascularly compromised patients these sudden hemodynamic changes may lead to congestive heart failure and/or acute myocardial infarction.
The Trendelenburg position, especially the long-lasting extreme head-down position, can raise the intracranial and intraocular pressures. Cerebral edema and retinal detachment may occur. Because of venous stagnation, cyanosis and edema in the face and neck may be expected. On the other hand hypotension can be induced when high intraabdominal pressure (IAP) is applied in combination with intermittent positive pressure ventilation (IPPV) due to compression of the inferior vena cava in combination with an elevated intrathoracic pressure. The latter is especially seen in relatively hypovolemic patients. Furthermore, high IAP may reduce renal perfusion and consequently urine production [28]. The best method for maintaining renal perfusion is the preservation of an adequate intravascular volume.
The reverse Trendelenburg, “head-up” position reduces venous return, which may lead to a fall in cardiac output and arterial pressure. If the patient has an adequate intravascular volume, PP will compensate for this decrease by increasing the venous return.
The lithotomy “legs up” position will induce “autotransfusion” by redistributing blood from the vessels of the lower extremities into the central body compartment, which thus will increase the preload of the heart. Subsequent PP will further increase venous return, the effect of which on the cardiac output (CO) will depend on the patient’s circulatory filling status.
The lateral decubitus position used for nephrectomy can cause direct compression of the inferior vena cava resulting in a decreased venous return and subsequent hypotension.
In conclusion, because of a combination of anesthesia, positioning, and PP, impressive fluid shifts may take place. Therefore, it is recommended that patients be adequately intravenously fluid loaded to maintain a normal CO. However, ASA class III and IV patients then may need advanced cardiac monitoring. It should be stressed that because of positioning and intra-thoracic pressure, central venous pressure monitoring does not reliably reflect the patient’s filling status.
Intraoperative complications
Apart from the common side effects of laparoscopy and usual reported morbidity and mortality around all surgical procedures, specific complications during laparoscopic surgery may occur. These complications are basically due to the carbon dioxide PP and/or patient positioning.
Pneumoperitoneum will induce hemodynamic, pulmonary, renal, splanchnic, and endocrine pathophysiological changes. However, most of these changes are clinically insignificant if appropriate anesthetic care is provided.
Pulmonary changes
Carbon dioxide is a highly soluble gas that is rapidly absorbed through the peritoneum into the circulation inducing hypercapnia and acidosis. During PP, the end-tidal CO2 concentrations increase progressively with time, reaching maximum value after 40 min of CO2 insufflation if ventilation is kept constant [29]. Thereafter, CO2 begins to accumulate in the body reservoir; up to 120 L CO2 can be stored. The absorption of CO2 is especially increased during prolonged surgery in combination with high IAP. Although a persistent elevation in the pCO2 is known to stimulate renal H+ secretion resulting in the addition of bicarbonate to the extracellular fluid, the renal response takes time to develop, and the net effect is that after 3 to 5 days, a new steady state is attained [30]. So, during laparoscopic procedures CO2 is almost only excreted through the lungs, and thus, hypercapnia must be decreased by compensatory hyperventilation. This hyperventilation may best be accomplished by increasing the tidal volume of ventilation in anesthetized patients. Nevertheless, respiratory acidosis and increased CO2 output last for at least up to 1 h postoperatively [31]. Carbon dioxide exhaustion is reduced when cardiopulmonary function is compromised [32].
Intraabdominal pressure plays a major role in the cause of hypercapnia as it increases the absorption and decreases the exhaustion of CO2. Elevated IAP and abdominal expansion shifts the diaphragm cephalad. This causes an increase in intrathoracic pressure; the abdominal part of the chest wall stiffens, thus restricting expansion of the lungs. During general anesthesia alone the functional residual capacity of the lung is reduced by ~20% [33]. During increased IAP the pulmonary dynamic compliance is significantly decreased up to 50%, whereas peak and plateau pressures are increased [34–36].
Ventilation perfusion mismatch and intrapulmonary shunting may become increased. In patients with a normal preoperative pulmonary function this will not lead to hypoxemia. In contrast, patients with compromised cardiopulmonary function such as emphysema or chronic obstructive pulmonary disease (COPD) will be at risk for developing hypoxemia.
To avoid hypercapnia and respiratory acidosis during PP the minute volume of ventilation should be increased, perhaps even to ~12–15 ml/kg. However, the anesthesiologist will consider the disadvantages of hypercapnia and acidosis vs the increases in inspiratory peak and plateau pressures that may induce ventilator induced lung injury (VILI). Although positive end-expiratory pressure (PEEP) improves the pulmonary gas exchange during PP [37], it should be realized that PEEP in combination with increased IAP increases the intrathoracic pressure, thus causing a reduction in CO [38]. Because of these pulmonary changes, insufflation with other gases such as argon, xenon, helium, and room air was investigated [39–44]. Although argon PP was not associated with significant changes in cardiorespiratory functions, argon embolism seemed to be more deleterious than CO2 embolism and might thus carry a higher risk in case of accidental gas embolism [39]. Helium insufflation was found to be superior in comparison to CO2 insufflation with respect to acidosis, hypercarbia, base excess changes, and influence on intracranial pressure [41, 43, 44], but was found to cause a greater impairment of hepatic blood flow [42]. Both helium and xenon were also investigated in laparoscopy because of a possible antitumor effect [40]. Further studies with these gases are still being performed.
Pulmonary complication
Pulmonary complications that may occur during laparoscopic surgery are barotrauma, pulmonary edema, atelectasis, gas embolism, subcutaneous emphysema, pneumothorax, pneumomediastinum, and pneumopericardium.
Hypoxemia may develop in patients with cardiopulmonary comorbidity such as emphysema and COPD. In most cases adequate ventilation and oxygenation will reverse hypoxemia. If not, conversion to open surgery may be required. The combination of increased mean airway pressure and decreased lung compliance is associated with barotrauma, which may result in acute pneumothorax [45]. Although pulmonary changes are of concern in infants undergoing laparoscopic surgical procedures, laparoscopy can safely be performed if proper attention is maintained during the procedure [46].
Carbon dioxide embolism is a very serious but rare complication of PP; mortality rates of up to 28% have been described [47]. The major cause of CO2 embolism is known to be misplacement of the Veress needle, either directly into a vessel or into a parenchymal organ. Carbon dioxide bubbles can enter the circulation through an opening in any injured vessel due to the raised IAP. With respect to the occurrence of gas emboli during the initial institution of PP, the Hasson technique seems safer than the Veress needle technique [48].
The intravascular presence of small amounts of CO2 frequently occurs, usually without any clinical consequence. Studies with TEE revealed 68% of asymptomatic patients to have CO2 bubbles in the right ventricle during laparoscopic cholecystectomy [49]. Since CO2 is very soluble in blood, a large amount of it must rapidly enter the circulation in order to be clinically relevant. A known risk factor is hypovolemia. If serious gas embolism is suspected during the course of laparoscopic surgery rigorous measures must be taken. Gas embolism may present as profound hypotension, cyanosis, arrhythmias, and/or asystole. A grinding murmur can be found by auscultation of the heart. End-tidal CO2 concentration suddenly increases, followed by an acute decrease due to cardiovascular collapse. Upon suspicion of embolism the following measures must be taken at once [50, 51]:
-
➣Immediate deflation of PP
-
➣Placement of the patient in a left lateral head-down position to enable the gas embolus to move into the right ventricular apex, thereby preventing its entry into the pulmonary artery
-
➣Increase of minute ventilation and administration of 100% in-tidal O2 to help eliminate CO2
-
➣Placement of a central venous catheter to enable aspiration of the gas
-
➣Cardiopulmonary resuscitation must be performed in case of asystole
-
➣Hyperbaric oxygen therapy may be used if available
Subcutaneous emphysema may be caused by gas passing through a disruption of the peritoneum into the subcutaneous tissue and into the retroperitoneal space. Its .occurrence has been estimated at 0.3–3.0% [49]. From the intraabdominal and retroperitoneal spaces, the insufflated CO2 can escape through the soft tissues around the vena cava and aorta into the mediastinum. In addition CO2 may escape into the intrapleural space through congenital defects of the diaphragm or through accidental diaphragmatic injuries. The latter has been described during laparoscopic adrenalectomy and fundoplications [52].
Pneumothorax may occur during laparoscopy because of increased mean airway pressures and should be differentiated from “capnothorax” caused by CO2 diffusion into the intrapleural space. The presence of subcutaneous emphysema should lead to the suspicion of capnothorax. End-tidal CO2 concentration increases in both subcutaneous emphysema and capnothorax. Clinically significant capnothorax should be suspected when the mean airway pressure increases and SpO2 declines. A chest x-ray then is required for diagnostic purposes. In contrast to a pneumothorax, the capnothorax generally does not require insertion of a chest drain because CO2 is rapidly reabsorbed once PP is released.
Hemodynamic changes
Cardiovascular changes occur due to a combination of anesthesia, PP, and patient positioning. Many clinical studies of laparoscopic surgical procedures have characterized the influence of the different modalities on patient hemodynamics [45, 53, 54, 55, 56, 57, 58, 59, 60]. Most studies reported increased systemic (SVR) and pulmonary vascular resistances (PVR) and a reduction of cardiac output when laparoscopy was performed with maximum IAP set at 15 mmHg or more in combination with reversed Trendelenburg position. Significant increases were also noted in mean arterial pressure (MAP), right atrial pressure (RAP), and pulmonary capillary wedge pressure (PCWP). At lower IAP the foregoing parameters change to a lesser extent. Interestingly, all measured variables usually return to preinsufflation values 30 min after the start of PP. Also, in healthy infants it was found that these same cardiovascular impairments completely reversed after peritoneal exsufflation without any clinically deleterious effect [61].
Hemodynamic changes during PP with the accompanying position of the patient are caused by a number of mechanisms. A quick rise in blood pressure, which is often seen at the start of PP, is mainly caused by an increased preload due to an increased venous return from blood compressed out of the splanchnic vasculature. Neurohumoral changes during PP may increase the SVR, which can lead to an increase in MAP. Induction of CO2-PP also may lead to an increased plasma renin activity and increased antidiuretic hormone (ADH) production, which, in combination with the influence on the sympathetic system, may induce SVR elevation [53].
Hypotension is a rare complication that may occur during laparoscopic interventions. Generally this is induced by a high IAP in combination with IPPV. It should be remembered that high IAP in combination with the reversed Trendelenburg position reduces cardiac filling even further.
Insufflating the abdomen can provoke arrhythmias. Differentiation must be made between more innocent arrhythmias due to release of catecholamines, such as sinus tachycardia and ventricular extrasystoles, and more dangerous bradyarrhythmias such as bradycardia, nodal rhythm, atrioventricular dissociation, and asystole. These latter arrhythmias are generally caused by a vagal nerve–mediated cardiovascular response due to acute stretching of the peritoneum [47]. Carbon dioxide also may induce arrhythmias as it causes irritability of the heart. Most arrhythmias respond to a reduction in IAP and increase of minute ventilation with FIO2 set at 1.0. Cardiac arrest associated with laparoscopy is caused either by a vasovagal response to rapid CO2 insufflation into the intraperitoneal cavity or by gas embolism.
Since some of the pathophysiological mechanisms underlying a number of cardiopulmonary complications are well known, preventive measures can be taken. Preoperative volume loading (10–12 ml/kg) may prevent a decrease in CO that is induced by the IAP in combination with a reversed Trendelenburg position of the patient. Invasive hemodynamic monitoring or TEE may be necessary in ASA III and IV patients. Slow CO2 insufflation will reduce gas embolism and avoids vasovagal response leading to collapse, cardiac arrest, and arrhythmias. Finally, it is recommended to apply the lowest possible IAP for each particular procedure. Extreme positioning should be avoided as it could influence cardiac function and ventilation and could cause peripheral nerve damage.
Renal physiology is influenced by PP, which may induce renal complications such as oliguria [62]. The following underlying mechanisms are considered: (1) compression of renal vasculature and parenchyma [63], (2) an increase of antidiuretic hormone release [64], (3) activation of the renin–angiotensin-aldosterone system (RAAS), and (4) a decrease of CO.
An inverse correlation exists between IAP and both renal perfusion and urine production [65–67]. Pneumoperitoneum with cool, room-temperature CO2 has been shown to decrease not only core temperature, but urine output as well [68]. Warm (body-temperature) insufflation probably causes local renal vasodilatation and may be beneficial to patients with borderline renal function [68]. In conclusion, PP especially with high IAP may impair renal function. The best method for maintaining renal perfusion is preservation of an adequate intravascular volume load, before as well as during laparoscopy, with concomitant insufflation of warmed CO2 for maintenance of PP.
The splanchnic circulation also may become compromised when high IAP is applied during laparoscopy. In healthy patients, increase in IAP from 10 mmHg to 15 mmHg significantly decreases blood flow, to the stomach by 54%, the jejunum by 32%, the colon by 4%, the liver by 39%, the parietal peritoneum by 60%, and the duodenum by 11%. Splanchnic blood flow decreases along with insufflation time [69]. The direct mechanical compression of the superior mesenteric artery and hepatic portal vein is the mechanism suggested in literature [69]. To prevent this possible complication, IAP should not exceed 8–10 mmHg.
Recovery period
Surgical injury induces a stress response characterised by profound endocrine-metabolic changes with hypermetabolism and catabolism, as well as an inflammatory response with activation of humoral cascade systems leading to malaise, hyperthermia, and immunosuppression [70]. Modern anesthetic and surgical care aims to reduce surgical stress responses, although the best way to modify such a natural evolutionary response is unclear [70, 71]. Various techniques are described for reduction of surgical stress responses, such as high inspired oxygen fraction postoperatively, application of peripheral nerve blocks, and prevention of hypothermia [72].
Routine postoperative care should consist of adequate monitoring of vital organ functions. This includes continuous monitoring of peripheral oxygen saturation, respiratory rate, ECG, and heart rate and rhythm. Intermittent measurements of blood pressure and urinary output are obligatory.
Advanced postoperative monitoring may be required in cardiovascularly debilitated ASA III and IV patients. If appropriate, this may include measurements of right atrial (RAP), pulmonary artery pressures (PAP), and cardiac index (CI) by means of a pulmonary artery catheter [55].
Monitoring of end-tidal CO2 is important when prolonged laparoscopic procedures are performed, when high IAP is applied, or when extensive subcutaneous emphysema is present. Since up to 120 L of CO2 can be stored in the human body during PP, prolonged postoperative mechanical ventilation may sometimes be needed until all extra CO2 has been eliminated [73]. When extensive subcutaneous emphysema is present or when either capnothorax or pneumothorax is suspected, a chest x-ray should be taken. Since prolonged PP, especially at higher IAP levels, may cause oliguria, urine output must be followed carefully, the filling status of the patient monitored, and variables of kidney function measured. This is specifically important in patients with a borderline renal function.
The gut clearly plays a role in postoperative recovery. Laparoscopy has been shown to blunt the response in serum interleukin (IL-6), with no change in gut mucosal IL-6, as compared with open laparotomy [74]. Laparoscopy causes less trauma to the peritoneal environment by decreasing the inflammatory response of the gut as compared with open laparotomy. This different response may partially explain the more rapidly restored intestinal function following laparoscopy as compared to laparotomy [74].
Postoperative nausea and vomiting (PONV) is common after laparoscopic surgery. At present, the etiological mechanism is not quite clear. Among the possible causes are mechanical pressure to gut and stomach and stretching of vagal nerve endings in the peritoneum. Carbon dioxide may induce vasodilatation of the cerebral vessels, consequently raising the intracranial pressure (ICP). A raised ICP is a well-known cause of nausea and vomiting [75]. In many centers, prophylactic administration of antiemetics is routine. The safest or least expensive drug should be used first, with multiple interventions being reserved for high-risk patients [76].
Pain after laparoscopic surgery is multifactorial and may be quite intense. Many patients require opioid analgesia [77]. A number of measures can be considered for the management of postoperative pain. Among them are local anesthetic infiltration of port sites, avoiding IAP peaks and prolonged PP with high IAP, evacuating residual gas, and using preemptive analgesia.
Early postoperative complications, which should be recognized rapidly, are intraabdominal and/or retroperitoneal hemorrhage, capnothorax, capnopericardium, and pneumothorax. When extensive subcutaneous emphysema is present and extended to the neck area, respiration must be carefully monitored.
Conclusions and recommendations
Pathophysiological changes that may occur during and after laparoscopy are hemodynamic, pulmonary, renal, splanchnic, and endocrine in nature. These changes are basically caused by CO2 pneumoperitoneum, anesthesia, and/or patient positioning. Pulmonary complications that may occur during laparoscopic surgery are barotrauma, pulmonary edema, atelectasis, gas embolism, subcutaneous emphysema, pneumothorax, pneumomediastinum, and pneumopericardium, whereas hemodynamic complications consist of changes in cardiac output, systemic and pulmonary resistance, and arrhythmias. Hypovolemia in combination with high intraabdominal pressure may lead to restrictive flow to vital organs such as kidney and the splanchnic area.
Good preassessment and anesthetic practice and adequate monitoring in combination with optimal communication between surgeon and anesthesiologist will see most patients through the extended laparoscopic procedure without complications. The elderly ASA III and IV patients, especially those with moderate to severe cardiopulmonary comorbidity, should be considered for invasive monitoring or monitoring by means of transesophageal echocardiography.
Postoperative care should be focused upon the specific complications connected with laparoscopic interventions, and the treatment of pain and PONV.
References
Bernheim BM (1911) Organoscopy: cystoscopy of the abdominal cavity. Ann Surg 53: 764
Monson JR (1993) Advanced techniques in abdominal surgery. Br Med J 307: 1346–1350
Clinical outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350: 2050–2059
Huang MT, Lee WJ, Wang W, Wei PL, Chen RJ (2003) Hand assisted laparoscopic hepatectomy for solid tumor in the posterior portion of the right lobe: initial experience. Ann Surg 238: 674–679
Tamme C, Scheidbach H, Hampe C, Schneider C, Kockerling F (2003) Totally extraperitoneal endoscopic inguinal hernia repair. Surg Endosc 17: 190–195
Gill IS, Fergany A, Klein EA, Kaouk JH, Sung GT, Meraney AM, Savage SJ, Ulchaker JC, Novic AC (2000) Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology 56: 26–29
Garcia-Miguel FJ, Serrano-Aguilar PG, Lopez-Bastida J (2003) Preoperative assessment. Lancet 362: 1749–1757
Baxendale B, Smith G (2001) Preoperative assessment and premedication. In: Aitkenhead AR, Rowbotham DJ, Smith G, (eds) Textbook of Anesthesia Churchill Livingstone, Edinburg pp 417–428
ASA Task Force on Preanesthesia Evaluation (2003) Practice Advisory for Preanesthesia Evaluation, last amended on October 15. www.asahq.org/publicationsAndServices/practiceparam.htm
Tobias JD (2002) Anesthesia for minimally invasive surgery in children. Best Pract Res Clin Anesthesiol 2002;16(1):115–30
Joris JL (1994) Anesthetic management of laparoscopy. In: Miller RD (ed) Anesthesia Churchill Living-stone. New York, pp 2011–2029
Hanley ES (1992) Anesthesia for laparoscopic surgery. Surg Clin North Am 72:1013–1019
Whalley DG, Berrigan MJ (2000) Anesthesia for radical prostatectomy, cystectomy, nephrectomy, pheochromocytoma, and laparoscopic procedures. Anesthesiol Clin North Am 18: 899–917
Mangano DT (1989) Peri-operative cardiac morbidity — epidemiology, costs, problems, and solutions. West J Med 1994;161:87–89
Mangano DT, Browner WS, Hollenberg M, London MJ, Tubau JF, Tateo IM (1990) Association of perioperative myocardial ischemia with cardiac morbidity and mortality in men undergoing noncardiac surgery. N Engl J Med 1990;323:1781–1788
Mangano DT (1989) Anesthetics, coronary artery disease, and outcome: unresolved controversies. Anesthesiology 70: 175–178
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical wound infection and shorten hospitalization. Study of wound infection and Temperature group. N Engl J Med 334: 1209–1215
Lagasse RS (2002) Anesthesia safety: model or myth? A review of the published literature and analysis of current original data. Anesthesiology 97: 1609–1617
Buhre W, Rossaint R (2003) Perioperative management and monitoring in anesthesia. Lancet 362: 1839–1846
www.asahq.org/publicationsAndServices/standards/02.pdf#2
Bowdle TA (2002) Complications of invasive monitoring. Anesthesiol Clin North Am 20: 571–588
Buhre W, Weyland A, Schorn B, Scholz M, Kazmaier S, Hoeft A, Sonntag H (1999) Changes in central venous pressure and pulmonary capillary wedge pressure do not indicate changes in right and left heart volume in patients undergoing coronary artery bypass surgery. Eur J Anaesthesiol 16: 11–17
Hofland J, Gultuna I, Tenbrinck R (2001) Xenon anesthesia for laparoscopic cholecystectomy in a patient with Eisenmengers syndrome. Br J Anaesth 86: 882–886
Hagen PT, Scholz DG, Edwards WD (1984) Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 59: 17–20
Lechat P, Mas JL, Lascault G, Loron P, Theard M, Klimezac M, Drobinski G, Thomas D, Grosgogeat Y (1988) Prevalence of patent foramen ovale in patients with stroke. N Engl J Med 1988; 318: 1148–1152
Spahn DR, Schmid S, Carrel T, Pasch T, Schmid ER (1995) Hypopharynx perforation by a transesophageal echocardiography probe. Anesthesiology 82: 581–583
Barker L (2002) Positioning on the operating table. Update Anaesth 15: 1–6.02
Wedgewood J, Doyle E (2001) Anesthesia and laparoscopic surgery in children. Paediatr Anaesth 11: 391–399
Baraka A, Jabbour S, Hammoud R, Aouad M, Najjar F, Khoury G, Sibai A (1994) End-tidal carbon dioxide tension during laparoscopic cholecystectomy: Correlation with baseline value prior to carbon dioxide insufflation. Anaesthesia 49: 304–306
Rose BD, Post TW (2001) Respiratory acidosis. In: Rose BD, Post TW (eds) Clinical physiology of acid-base and electrolyte disorders. McGraw Hill, New York, pp 647–672
Kazama T, Ikeda K, Kato T, Kikura M (1996) Caroon dioxide output in laparoscopic cholecystectomy. Br J Anaesth 76: 530–535
Hsieh CH (2003) Laparoscopic cholecystectomy for patients with chronic obstructive pulmonary disease. J Laparoendosc Adv Surg Tech A 13:5–9
Wahba RW (1991) Perioperative functional residual capacity. Can J Anaesth 38:384–400
Hirvonen EA, Nuutinen LS, Kauko M (1995) Ventilator effects, blood gas changes and oxygen consumption during laparoscopic hysterectomy. Anesth Analg 80: 961–966
Bardoczky GI, Engelman E, Levarlet M, Simon P (1993) Ventilator effects of pneumoperitoneum monitored with continuous spirometry. Anesthesia 48: 309–311
Rauh R, Hemmerling TM, Rist M, Jacobi KE (2001) Influence of pneumoperitoneum and patient positioning on respiratory system compliance. J Clin Anesth 13: 361–365
Loeckinger A, Kleinsasser A, Hoermann C, Gassner M, Keller C, Lindner KH (2000) Inert gas exchange during pneumoperitoneum at incremental values of positive end-expiratory pressure. Anesth Analg 90: 466–471
Luz CM, Polarz H, Bohrer H, Hundt G, Dorsam J, Martin E (1994) Hemodynamic and respiratory effects of pneumoperitoneum and PEEP during laparoscopic pelvic lymphadenectomy in dogs. Surg Endosc 8: 25–27
Mann C, Boccara G, Grevy V, Navarro F, Fabre J, Colson P (1995) Argon pneumoperitoneum is more dangerous than CO2 pneumoperitoneum during venous gasembolism. Anesth Analg 85: 1367–1371
Dähn S, Schwalbach P, Wöhleke F, Benner A, Kuntz C (2003) Influence of different gases used for laparoscopy (helium, carbon dioxide, room air, xenon) on tumor volume, proliferation, and apoptosis. Surg Endosc 17: 1653–1657
Hazebroek EJ, Haitsma JJ, Lachmann B, Steverberg FW, de Bruin RW, Bouvy ND (2002) Impact of carbon dioxide and helium insufflation on cardio-respiratory function during prolonged pneumoperitoneum in an experimental rat model. Surg Endosc 16: 1073–1078
Sala-Blanch X, Fontanals J, Martinez-Palli G, Taura P, Delgado S, Bosch J, Lacy AM, Visa J (1998) Effects of carbon dioxide vs helium pneumoperitoneum on hepatic blood flow. Surg Endosc 12: 1121–1125
Schöb OM, Allen DC, Benzel E, Curet MJ, Adams MS, Baldwin NG, Largiader F, Zucker KA (1996) A comparison of the pathophysiologic effects of carbon dioxide, nitrous oxide, and helium pneumoperitoneum on intracranial pressure. Am J Surg 172: 248–253
Brackman M, Finelli FC, Light T, Llorente O, McGill K, Kirkpatrick J (2003) Helium pneumoperitoneum amelio-rates hypercarbia and acidosis associated with carbon dioxide insufflation during laparoscopic gastric bypass in pigs. Obes Surg 13: 768–771
Koivusalo AM, Lindgren L (2000) Effects of carbon dioxide pneumoperitoneum for laparoscopic cholecystectomy. Acta Anesthesiol Scand 44: 834–841
Bannister CF, Brosius KK, Wulkan M (2003) The effect of insufflation pressure on pulmonary mechanics in infants during laparoscopic surgical procedures. Paediatr Anaesth 13: 785–789
Magrina JF 2002 Complications of laparoscopic Surgery. Clin Obset Gynecol 45:469–480
Bonjer HJ, Hazebroek EJ, Kazemier G, Giuffrida MC, Meijer WS, Lange JF (1997) Open versus closed establishment of pneumoperitoneum in laparoscopic surgery. Br J Surg 84: 599–602
Derouin M, Couture P, Boudreault D, Girard D, Gravel D (1996) Detection of gas embolism by transesophageal echocardiography during laparoscopic cholecystectomy. Anesth Analg 82: 119–124
Haroun-Bizri S, El Rassi T (2001) Successful resuscitation after catastrophic carbon dioxide embolism during laparoscopic cholecystectomy. Eur J Anesthesiol 18: 118–121
Archer DP, Pash MP, MacRae ME (2001) Successful management of venous air embolism with inotropic support. Can J Anaesth 48: 204–208
Del Pizzo JJ, Jacobs SC, Bishoff JT, Kavoussi LR, Jarrett TW (2003) Pleural injury during laparoscopic renal surgery: early recognition and management. J Urol 169: 41–47
O’Leary E, Hubbard K, Tormey W, Cunningham AJ (1996) Laparoscopic cholecystectomy: haemodynamic and neuroendocrine responses after pneumoperitoneum and changes in position. Br J Anaesth 76: 640–644
Odeberg S, Ljungqvist O, Svenberg T, Gannedahl P, Bäckdahl M, vonRosen A, Sollevi A (1994) Haemodynamic effects of pneumoperitoneum and the influence of posture during anesthesia for laparoscopic surgery. Acta Anesthesiol Scand 38: 276–283
Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, Buchler MW (2004) Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg 21: 95–105
Harris SN, Ballantyne GH, Luther MA, Perrino AC Jr (1996) Alterations of cardiovascular performance during laparoscopic colectomy: a combined hemodynamic and echocardiographic analysis. Anesth Analg 83: 482–487
Giebler RM, Walz MK, Peitgen K, Scherer RU (1996) Hemodynamic changes after retroperitoneal CO2 insufflation for posterior retroperitoneoscopic adrenalectomy. Anesth Analg 82: 827–831
Gannedahl P, Odeberg S, Brodin LA, Sollevi A (1996) Effects of posture and pneumoperitoneum during anesthesia on the indices of left ventricular filling. Acta Anesthesiol Scand 40: 160–166
Fujise K, Shingu K, Matsumoto S, Nagata A, Mikami O, Matsuda T (1998) The effects of the lateral position on cardiopulmonary function during laparoscopic urological surgery. Anesth Analg 87: 925–930
Fahy BG, Hasnain JU, Flowers JL, Plotkin JS, Odonkor P, Furguson MK (1999) Transesophageal echocardio-graphic detection of gas embolism and cardiac valvular dysfunction during laparoscopic nephrectomy. Anesth Analg 88: 500–504
Gueugniaud PY, Abisseror M, Moussa M, Godard J, Foussat C, Petit P, Dodat H (1998) The hemodynamic effects of pneumoperitoneum during laparoscopic surgery in healthy infants: assessment by continuous esophageal aortic blood flow echo-doppler. Anesth Analg 86: 290–293
Nguyen NT, Perez RV, Fleming N, Rivers R, Wolfe BM (2002) Effect of prolonged pneumoperitoneum on intraoperative urine output during laparoscopic gastric bypass. J Am Coll Surg 195: 476–483
Chiu AW, Azadzoi KM, Hatzichristou DG, Siroky MB, Krane RJ, Babayan RK (1994) Effects of intra-abdominal pressure on renal tissue perfusion during laparoscopy. J Endourol 8: 99–103
Hazebroek EJ, de Vos tot Nederveen Cappel R, Gommers D, van Gelder T, Weimar W, Steyerberg EW, Bonjer HJ, Ijzermans JH (2002) Antidiuretic hormone release during laparoscopic donor nephrectomy. Arch Surg 137: 600–604
Koivusalo AM, Kellokumpu I, Scheinin M, Tikkanen I, Halme L, Lindgren L (1996) Randomized comparison of the neuroendocrine response to laparoscopic cholecystectomy using either conventional or abdominal wall lift technique. Br J Surg 83: 1532–1536
Koivusalo AM, Kellokumpu I, Ristkari S, Lindgren L (1997) Splanchnic and renal deterioration during and after laparoscopic cholecystectomy: A comparison of carbon dioxide pneumoperitoneum and the abdominal wall lift method. Anesth Analg 85: 886–891
Koivusalo AM, Scheinin M, Tikkanen I, Yli-Suomu T, Ristkari S, Laakso J, Lindgren L (1998) Effects of esmolol on haemodynamic response to CO2 pneu-moperitoneum for laparoscopic surgery. Acta Anesthesiol Scand 42: 510–517
Backlund M, Kellokumpu I, Scheinin T, von Smitten K, Tikkanen I, Lindgren L (1998) Effect of temperature of insufflated CO2 during and after prolonged laparoscopic surgery. Surg Endosc 12: 1126–1130
Schilling MK, Redaelli C, Krahenbuhl L, Signer C, Buchler MW (1997) Splanchnic microcirculatory changes during CO2 laparoscopy. J Am Coll Surg 185: 423
Wilmore DW (2002) From Cuthbertson to fast-track surgery: 70 years of progress in reducing stress in surgical patients. Ann Surg 236: 643–648
Buunen M, Gholghesaei M, Veldkamp R, Meijer DW, Bonjer HJ, Bouvy ND (2004) Stress responsetolaparoscopic surgery. A review. Surg Endosc 18: 1022–1028
Kehlet H, Dahl JB (2003) Anesthesia, surgery, and challenges in postoperative recovery. Lancet 362: 1921–1928
Schulte-Steinberg H, Meyer G, Forst H (1996) Are high risk patients candidates for minimally invasive surgery with CO2 pneumoperitoneum? Viewpoint from anesthesiology. Chirurg 67: 72–76
Tung PH, Wang Q, Ogle CK, Smith CD (1998) Minimal increase in gut-mucosal interleukin-6 during laparoscopy. Surg Endosc 12: 409–411
Andrews PL (1992) Physiology in nausea and vomiting. Br J Anaesth 69(Suppl 1): 2S–19S
Apfel CC, Korttilla K, Abdalla M, Kerger H, Turan A, Vedder I, Zemak C, Danner K, Jokela R, Pocock SJ, Trenkler S, Kredel M, Biedler A, Sessler DI, Roewer N, for the IMPACT Investigators (2004) factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med 350: 2441–2451
Mouton W, Bessell J, Otten KT, Maddern GJ (1999) Pain after laparoscopy. Surg Endosc 13: 445–448
Acknowledgment
The authors thank W. Bemelman, MD, PhD, endoscopic surgeon, for critically reviewing the manuscript and for his valuable comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Henny, C., Hofland, J. Laparoscopic surgery: Pitfalls due to anesthesia, positioning, and pneumoperitoneum. Surg Endosc 19, 1163–1171 (2005). https://doi.org/10.1007/s00464-004-2250-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-2250-z