Abstract
Background
Little is know about the effects of different insufflation gases on peritoneal pH during laparoscopy. However, these changes may influence the intracellular signalling system, resulting in altered cell growth or adhesiveness. The aim of this study was to determine the effects of carbon dioxide (CO2), nitrous oxide (N2O), and helium (He) on parietal and visceral peritoneal pH. The effect of different intraabdominal pressures on parietal and visceral peritoneal pH was also examined.
Methods
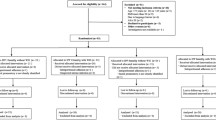
We conducted both an ambient gas study and a pressure study. For the ambient gas study, 20 pigs were divided into the following four groups: (a) CO2, (b) He, (c) N2O, and (d) abdominal wall lift (Lift) laparoscopy. Parietal and visceral peritoneal pH were measured at 15 min intervals for 180 min. For the pressure study, 15 pigs were divided into the following three groups: (a) CO2, (b) He, (c) N2O laparoscopy. Baseline values were established for parietal and visceral peritoneal pH. Intraabdominal pressure was then increased stepwise at 1-mmHg intervals to 15 mmHg. After pressure was maintained for 15 min at each setting, parietal and visceral peritoneal pH were measured.
Results
Ambient gas environment was the major determinant of parietal peritoneal pH. Carbon dioxide caused parietal peritoneal acidosis. Helium, N2O, and Lift caused alkalotic parietal peritoneal pH. Intraabdominal pressure had a minor effect on parietal peritoneal pH. At higher intraabdominal pressure (12–15 vs 5–8 mmHg), CO2 caused a slight decrease in parietal peritoneal pH, whereas N2O and He caused a slight increase in parietal peritoneal pH. Visceral peritoneal pH remained relatively unaffected during all studies.
Conclusions
Parietal peritoneal pH during laparoscopy was highly dependent on the ambient gas environment. The effect of intraabdominal pressure on parietal peritoneal pH was of minor significance. Carbon dioxide caused a slight worsening of parietal peritoneal acidosis at higher intraabdominal pressure, whereas, N2O, He, and Lift did not cause parietal peritoneal acidosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Carbon dioxide (CO2) pneumoperitoneum is known to cause systemic acidosis [8]. Recently, our research team and others showed that severe peritoneal acidosis can also occur during CO2 laparoscopy [17, 18, 20]. It was thought that either the nature of the gas itself or the untoward effects of intraabdominal pressure in causing relative ischemia of the peritoneum [16, 18] might contribute to the peritoneal acidosis. Peritoneal acidosis has been proposed as one of the mechanisms responsible for damaging the mesothelial lining of the peritoneum, thereby exposing the underlying basal lamina and providing attachment sites for spilled tumor cells [17]. Intracellular and extracellular pH are also important regulators of cell functions such as adenosine triphosphate (ATP) production, cell cycle, cell growth, and apoptosis [18]. It is therefore plausible that the increased tumor growth seen after CO2 laparoscopy in some studies [5, 7, 9] is a consequence of the peritoneal acidosis caused by CO2. In this series of experiments, we examined the relative contributions of the effects of the ambient gas environment (CO2, nitrous oxide [N2O], and helium [He]) and intraabdominal pressure on parietal and visceral peritoneal pH.
Methods
The study was divided into two parts. First, we studied the effects of different types of gases on parietal and visceral (small bowel serosa) peritoneal pH. Then we determined how increasing intraabdominal pressure affects on the pH of the peritoneum.
Ambient gas study
Twenty domestic pigs were divided into four equal groups. Three of the groups underwent laparoscopy with one of the gases (CO2, N2O, or He); the fourth group underwent laparoscopy by abdominal wall lift (Lift). All groups underwent laparoscopy for 180 min. The groups that underwent laparoscopy with gas received a continuous flow of fresh gas into the abdomen via an 11-mm port placed in the left upper quadrant. Intraabdominal pressure was maintained at 5–6 mmHg for the duration of experiment. In the group that underwent abdominal wall lift, six heavy silk sutures were inserted circumferentially on their abdominal wall to lift the anterior abdominal wall. The sutures were then attached to simple pulley systems and weights. Total weight used in lifting the abdominal wall was 5 kg. In all groups, parietal and visceral peritoneal pH was measured at 0, 5, and 15 min after the commencement of insufflation or lifting. Thereafter, the measurements were taken at 15-min intervals for 3 h.
Pressure study
Fifteen domestic pigs were divided into three equal groups. All 15 underwent laparoscopy with gas insufflation, using either CO2, He, or N2O. Gases were insufflated into the abdomen via an 11-mm port in the left upper quadrant. The Olympus Surgical Insufflator (Olympus, Hamburg, Germany) was used for insufflation and to measure intraabdominal pressure. The intraabdominal pressure was taken inside the abdomen when the animal was at end exhalation. Intraabdominal pressures of 0–15 mmHg were achieved by adjusting the control settings on the insufflator. At any particular pressure setting, the pressure was maintained for 15 min before measurements were taken. Parietal and visceral peritoneal pH were measured at stepwise increments of 1 mmHg with a HI 1413 pH probe (Hanna Instrument, Woonsocket, RI, USA). A pH probe was inserted into the abdomen via a left lower quadrant incision.
In both studies, the animals were ventilated at a fixed tidal volume of 120 ml/kg/min. Statistical analysis was done using the two-tailed Student t-test. An independent Student t-test was used for comparisons between two groups. A paired Student t-test was used for within-group comparisons.
Results
Parietal peritoneal pH
Ambient gas study
Nitrous oxide and He resulted in alkalotic parietal peritoneal pH immediately after insufflation (N2O 7.22 → 6.59; He 7.28 → 7.64), whereas CO2 resulted in parietal peritoneal acidosis pH (7.37 → 6.59). Lift also resulted in alkalotic parietal peritoneal pH upon lifting of the abdominal wall (7.26 → 7.45) (Fig. 1).
After the initial pH changes, parietal peritoneal pH remained relatively unchanged for 3 h in all groups.
Pressure study
Carbon dioxide pneumoperitoneum resulted in parietal peritoneal acidosis. Parietal peritoneal pH dropped immediately after insufflation with CO2. Even at an intraabdominal pressure of 2 mmHg, parietal peritoneal pH had turned significantly acidotic (p < 0.01) (pH 7.41 → 6.94). It also became increasingly acidotic with increased pressure up to 15 mmHg (pH 6.94 → 6.66) (Fig. 2). When two ranges of intraabdominal pressure were compared (5–8 vs 12–15 mmHg), CO2 caused worse parietal peritoneal acidosis at the higher-pressure range (p < 0.05).
Nitrous oxide and He caused alkalotic parietal peritoneal pH as intraabdominal pressure rose from 0 to 15 mmHg (N2O pH 7.21 → 7.65; He pH 7.25 → 7.65) (Fig. 2). Both gases also caused progressively more alkalotic parietal peritoneal pH with increasing intraabdominal pressure. Again, when parietal peritoneal pH values were compared at two different ranges (5–8 vs 12–15 mmHg), they were significantly more alkalotic at higher pressure (N2O p < 0.05; He p < 0.05). The increases in parietal peritoneal pH with N2O and He were more gradual than that observed with CO2, perhaps reflecting the high solubility of CO2 (Fig. 2)
Visceral peritoneal pH
Ambient gas study
When visceral peritoneal pH was studied over time, an initial drop was seen in the CO2 group (pH 7.29 → 7.06) (Fig. 3). All other groups had an initial increase in pH (N2O pH 7.18 → 7.25; He pH 7.24 → 7.35; Lift 7.19 →7.25) (Fig. 3). Visceral peritoneal pH in all groups returned to baseline after 60 min.
Pressure study
Visceral peritoneal pH remained relatively unaffected in all groups (CO2, N2O, and He) over an intraabdominal pressure range from 0 to 15 mmHg (Fig. 4). There was no significant difference in visceral peritoneal pH between any of the groups.
Discussion
Due to its high solubility and noncombustible properties, CO2 is the gas most commonly used for insufflation during laparoscopic procedures. Its wide use in laparoscopic surgery, and especially in oncologic procedures, began to raise concern after reports of a higher rate of tumor growth with CO2 laparoscopy [5, 7, 9]. Volz et al. have proposed that peritoneal acidosis during CO2 laparoscopy may be one of the mechanisms responsible for damaging the mesothelial lining of the peritoneum and thereby exposing the underlying basal lamina [17]. Exposed basal lamina provides good attachment sites for spilled tumor cells [2], thus promoting tumor implantation and seeding. It was also proposed that pH changes during laparoscopy may alter the electrical surface charges present on the mesothelial lining and underlying connective tissue, enabling the attachment of tumor cells [11, 17].
In a more recent study, Wildbrett et al. found that the intracellular and extracellular pH and calcium level of peritoneum were altered during laparoscopy [18]. Intracellular and extracellular pH and calcium are important regulators of many cell functions, such as cell signaling, cell apoptosis, and ATP production [18]. Griffiths et al. had also found that a low extracellular pH increased tumor cell expression of platelet-derived endothelial cell growth factor [4]. Endothelial cell growth factor is an angiogenic factor that is responsible for the growth and survival of tumor cells [15]. It is therefore not difficult to conclude that the low peritoneal pH associated with CO2 laparoscopy could be implicated in tumor metastasis. Although CO2 laparoscopy is known to be associated with peritoneal acidosis [18, 20], the effect of other insufflation gases—i.e., He and N2O—on peritoneal pH is not well understood [18]. We initially thought that the peritoneal acidosis associated with CO2 laparoscopy might be the result of intraabdominal pressures—induced ischemia [8, 16] or secondary to the hypoxic gas used for insufflation. This study, in line with others [18, 20], confirms that CO2 causes parietal peritoneal acidosis; however, the peritoneal acidosis was likely secondary to CO2 absorption rather than hypoxia-induced lactate production. Lift, N2O, and He laparoscopy did not result in parietal peritoneal acidosis. In fact, the parietal peritoneal pH turned alkalotic. Wildbrett et al. also reported that He insufflation resulted in alkalotic pH [18].
The reasons for the alkalotic peritoneal pH with N2O, He, and Lift laparoscopy are unknown. A search through the literature suggested that He and N2O are chemically and biologically inert [3, 6, 10, 12]. During the Lift procedures, air which is a combination of nitrogen, oxygen, along with a small amount of CO2 also made the peritoneum alkalotic. It is possible that the pH of the peritoneum was dependent on the amount of CO2 present. When CO2 was used for insufflation, there was an excess of CO2 gas, which displaces other gases away from the peritoneum. This causes peritoneal acidosis. On the other hand, when other gases were used for insufflation, they displaced the small amount of CO2 present in the peritoneum. Lack of CO2 created a situation where there was excess buffer, making the peritoneal pH alkalotic. Parietal peritoneal pH was therefore highly dependent on the ambient gas environment.
The contribution of intraabdominal pressure to parietal peritoneal pH was a minor one. During CO2 laparoscopy, parietal peritoneal pH turned significantly acidotic, even at low intraabdominal pressure (2 mmHg). Although a higher degree of acidosis was observed at higher pressure, the change in pH from low pressure to high pressure was only a minimal one. Most pH changes occurred initially, with the insufflation of gas at low pressure. The increased acidosis observed at higher pressure was likely to be due to the increased absorption of gas (CO2). Intraabdominal pressure (< 15 mmHg) causing relative ischemia of the peritoneum was less likely. In N2O and He laparoscopy, both gases resulted in increasingly alkalotic parietal peritoneal pH at higher pressure. If pressure caused ischemia of the peritoneum, then parietal peritoneal pH in N2O and He laparoscopy should have decreased with increased pressure. The fact that peritoneal pH rose rather than fell in N2O and He laparoscopy suggests that there was increased absorption of gases at higher pressure. In a recent study involving CO2 laparoscopy in a porcine model, blood flow in the peritoneum was found to be higher at 12 mmHg than at 4 mmHg [1]. This finding supports our contention that peritoneal acidosis during CO2 laparoscopy was not the result of peritoneal ischemia. The idea that peritoneal acidosis was secondary to the hypoxic insufflating gas was also not supported by this study, given that CO2, He, and N2O are all hypoxic gases and yet only CO2 caused peritoneal acidosis.
Visceral peritoneal pH remained relatively unchanged during laparoscopy with all three gases (CO2, N2O, He). The visceral peritoneum covering the intraabdominal organs and bowel may have a broader circulatory bed and larger-caliber vessels that enable it to clear the acid load more efficiently. It is unclear what role peritoneal pH changes plays in mesothelial lining damage after laparoscopy. Whether the use of the visceral peritoneum, with its transient and less extreme pH changes, will translate into less peritoneal damage is not known. It is, however, interesting to note that most studies of peritoneal recurrence after laparoscopic procedure have concentrated on the parietal peritoneum [7, 9, 11, 17, 18].
Despite its current widespread use for laparoscopy, CO2 is not an ideal insufflation gas. Helium and N2O have been proposed as alternatives. However, like CO2, neither of these gases is entirely harmless. Helium is insoluble in water, and in the rare event of gas embolism it has been reported to be more dangerous than CO2 [13, 14, 19]. Nevertheless, despite the theoretical risk, there are no reports in the English-language literature of gas embolism associated with He use during laparoscopy in the clinical setting (MEDLINE search from 1966 to 2004). In most studies on He gas embolism, the gas was injected directly into the circulatory system [13, 14, 19]. In fact, there have been several studies demonstrating the safe use He during laparoscopy in humans [3, 10]. Nitrous oxide may cause combustion during procedures performed with electrocautery instruments [12]. However Hunter et al. have demonstrated that there is no real risk of explosion when N2O is used during laparoscopic gastrointestinal procedures [6]. The search for the “ideal” gas is far from over. Further studies of the effects of different gases on peritoneal morphology and physiology will help guide us toward the best gas to use in the practice of laparoscopic tumor surgery.
References
SM Brundell C Tsopelas B Chatterton J Touloumtzoglou PJ Hewett (2002) ArticleTitleExperimental study of peritoneal blood flow and insufflation pressure during laparoscopy Br J Surg 89 617–622
RC Buck (1973) ArticleTitleWalker 256 tumor implantation in normal and injured peritoneum studied by electron microscopy, scanning electron microscopy, and autoradiography Cancer Res 33 3181–3188 Occurrence Handle1:STN:280:CSuD2cfnslM%3D Occurrence Handle4760534
RY Fleming TB Dougherty BW Feig (1997) ArticleTitleThe safety of helium for abdominal insufflation Surg Endosc 11 230–234 Occurrence Handle10.1007/s004649900332 Occurrence Handle1:STN:280:ByiB3snnt1I%3D Occurrence Handle9079598
L Griffiths GU Dachs R Bicknell AL Hanis IJ Stratford (1997) ArticleTitleThe influence of oxygen tension and pH on the expression of platelet-derived endothelial cell growth factor/thymidine phosphorylase in human breast tumor cells grown in vitro and in vivo Cancer Res 57 570–572 Occurrence Handle1:CAS:528:DyaK2sXht1OktLo%3D Occurrence Handle9044826
CN Gutt ZG Kim D Hollander T Bruttel M Lorenz (2001) ArticleTitleCO2 environment influences the growth of cultured human cancer cells dependent on insufflation pressure Surg Endosc 15 314–318 Occurrence Handle10.1007/s004640000321 Occurrence Handle1:STN:280:DC%2BD38%2FgvFyitw%3D%3D Occurrence Handle11344436
JG Hunter J Staheli M Oddsdottir T Trus (1995) ArticleTitleNitrous oxide pneumoperitoneum revisited: is there a risk of combustion? Surg Endosc 9 501–504 Occurrence Handle1:STN:280:ByqH3cnotFc%3D Occurrence Handle7676370
CA Jacobi R Sabat B Bohm HU Zieren HD Volk JM Muller (1997) ArticleTitlePneumoperitoneum with carbon dioxide stimulates growth of malignant colonic cells Surgery 121 72–78 Occurrence Handle10.1016/S0039-6060(97)90185-9 Occurrence Handle1:STN:280:ByiC2MvosVQ%3D Occurrence Handle9001554
TJ Knolmayer MW Bowyer JC Egan HJ Asbun (1998) ArticleTitleThe effects of pneumoperitoneum on gastric blood flow and traditional hemodynamic measurements Surg Endosc 12 115–118 Occurrence Handle10.1007/s004649900609 Occurrence Handle1:STN:280:DyaK1c7ktVemsg%3D%3D Occurrence Handle9479723
CC Nduka M Puttick P Coates L Yong D Peck A Darzi (2002) ArticleTitleIntraperitoneal hypothermia during surgery enhances postoperative tumor growth Surg Endosc 16 611–615 Occurrence Handle10.1007/s00464-001-9055-0 Occurrence Handle1:STN:280:DC%2BD383jsVertg%3D%3D Occurrence Handle11972199
TJ Neuberger CH Andrus CM Wittgen TP Wade DL Kaminski (1996) ArticleTitleProspective comparison of helium versus carbon dioxide pneumoperitoneum Gastrointest Endosc 43 38–41 Occurrence Handle1:STN:280:ByiD2MbkvFE%3D Occurrence Handle8903816
SJ Neuhaus DI Watson (2004) ArticleTitlePneumoperitoneum and peritoneal surface changes: a review Surg Endosc . .
GG Neuman G Sidebotham E Negoianu J Bernstein AF Kopman RG Hicks ST West et al. (1993) ArticleTitleLaparoscopy explosion hazards with nitrous oxide Anesthesiology 78 875–879 Occurrence Handle1:STN:280:ByyB2Mnjt1w%3D Occurrence Handle8489060
MW Roberts KA Mathiesen HS Ho BM Wolfe (1997) ArticleTitleCardiopulmonary responses to intravenous infusion of soluble and relatively insoluble gases Surg Endosc 11 341–346 Occurrence Handle10.1007/s004649900359 Occurrence Handle1:STN:280:ByiB2M%2FntVE%3D Occurrence Handle9094273
B Rudston-Brown PN Draper B Warriner KR Walley PT Phang (1997) ArticleTitleVenous gas embolism—a comparison of carbon dioxide and helium in pigs Can J Anaesth 44 1102–1107 Occurrence Handle1:STN:280:DyaK1c%2FhtFCmtA%3D%3D Occurrence Handle9350372
D Shweild A Itin D Soffer E Keshet (1992) ArticleTitleVascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis Nature 359 843–845 Occurrence Handle10.1038/359843a0 Occurrence Handle1279431
P Taura A Lopez AM Lacy T Anglada J Beltran L Fernandez-Cruz E Targarona et al. (1998) ArticleTitleProlonged pneumoperitoneum at 15 mmHg causes lactic acidosis Surg Endosc 12 198–201 Occurrence Handle10.1007/s004649900633 Occurrence Handle1:STN:280:DyaK1c7mvFGltg%3D%3D Occurrence Handle9502694
J Volz S Koster Z Spacek N Paweletz (1999) ArticleTitleCharacteristic alterations of the peritoneum after carbon dioxide pneumoperitoneum Surg Endosc 13 611–614 Occurrence Handle10.1007/s004649901052 Occurrence Handle1:STN:280:DyaK1M3nvVGnug%3D%3D Occurrence Handle10347302
P Wildbrett A Oh D Naundorf T Volk CA Jacobi (2003) ArticleTitleImpact of laparoscopic gases on peritoneal microenvironment and essential parameters of cell function Surg Endosc 17 78–82 Occurrence Handle10.1007/s00464-002-9015-3 Occurrence Handle1:STN:280:DC%2BD3s%2FmtFKjuw%3D%3D Occurrence Handle12360379
JS Wolf SuffixJr S Carrier ML Stoller (1994) ArticleTitleGas embolism: helium is more lethal than carbon dioxide J Laparoendosc Surg 4 173–177 Occurrence Handle7919504
YT Wong PC Shah DH Birkett DM Brams (2004) ArticleTitleCarbon dioxide pneumoperitoneum causes severe peritoneal acidosis unaltered by heating, humidification, or bicarbonate in a porcine model Surg Endosc . .
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, Y.T., Shah, P.C., Birkett, D.H. et al. Peritoneal pH during laparoscopy is dependent on ambient gas environment: helium and nitrous oxide do not cause peritoneal acidosis. Surg Endosc 19, 60–64 (2005). https://doi.org/10.1007/s00464-003-9291-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-9291-6