Abstract
Background
An obstructing primary lung cancer is a challenging disease frequently requiring endobronchial interventional therapy. A variety of interventional modalities, including Nd:YAG laser, stenting, photodynamic therapy (PDT), and endoluminal brachytherapy, are utilized to relieve airway obstruction and bleeding. The aim of this study is to compare the effect on patient survival of bronchoscopic palliation for lung cancer utilizing one interventional modality compared to the use of combination of modalities to relieve the airway problem.
Methods
We reviewed our longitudinal experience with interventional bronchoscopy in 75 patients who underwent 176 procedures for the management of endobronchial lung cancer between 1994 and 2002. Indication for intervention was hemoptysis in 24 patients (32%) and airway obstruction in the remaining. Six patients died within 30 days from the first intervention and were excluded. Forty of the surviving 69 patients (58%) were treated with a single interventional modality (group A). In 29 patients (42%) a multimodality endoscopic treatment was utilized (group B). Single-modality treatment in group A included Nd-YAG laser in 60%, stent in 17%, brachytherapy in 20%, and PDT in 3%. A variety of combinations of the aforementioned modalities were used in group B to enhance airway patency. Patient data were compared with the Student’s t-test and chi-square test. Survival analysis and the log rank test were used to compare difference in survival between the two groups. A p-value of 0.05 was considered significant.
Results
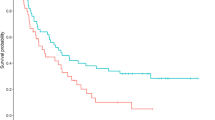
There were 46 males and 23 females, with a mean age of 67 years. The tumor was located in the trachea 9%, in the carina in 7%, and primary bronchial in 84%. Two patients had complications due to stent malposition. There was no significant difference between the two groups in relation to age, gender, tumor location, histology, and type of previous cancer therapy. There was a significant improvement in survival for the multimodality group (p = 0.04). The 1- and 3-year cumulative survival rate for groups A and B was 51.3% versus 50% and 2.3% versus 22%, respectively.
Conclusions
Improvement in survival can be seen with diligent airway surveillance after interventional bronchoscopy and liberal use of a variety of endobronchial treatment modalities for airway obstruction or bleeding. Physicians involved in the management of this difficult problem should be versed in the use of all available treatment modalities to enhance therapeutic outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Lung cancer is the most common cancer in the world and it remains the leading cause of cancer-related mortality for both sexes in the United States [17]. Thirty percent of lung cancer patients present with obstruction of the central airway (trachea, or main bronchi) manifested by symptoms of respiratory distress, bleeding, or infection [2].
The strategy and modality of treatment of primary lung cancer of the central airway depends on patient’s comorbidities, pulmonary function, previous treatment, and life expectancy [21]. Interventional bronchoscopy in association with laser [6], photodynamic therapy (PDT) [4], endobronchial radiation (brachytherapy) [18], and stenting [7] has been proven effective for symptomatic palliation of endobrochial lung cancer. These alternative treatments have been used either individually or in combination (multimodality treatment) [14].
It has been postulated that a multimodality approach is more effective than a single-modality approach for symptomatic palliation of endobrochial lung cancer [9]. However, only a few studies have compared the effectiveness of single versus multi-modality treatment [3, 10]. Randomization of patients with endobrochial lung cancer to different endoscopic treatment modalities faces multiple ethical dilemmas. In addition, little is known about the effect of single versus multimodality therapy on patient survival [11]. The purpose of this study is to report our experience and assess the impact of choice of treatment modality on patient survival.
Materials and methods
Between January 1997 and July 2002, 75 patients underwent interventional bronchoscopy with a variety of modalities in our department for symptomatic palliation of endobrochial lung cancer. Preoperative evaluation and decision making was based on a multidisciplinary approach including a pulmonologist, an oncologist, and a thoracic surgeon. Twenty-four patients (32%) presented with hemoptysis, and 51 (68%) patients with airway obstruction symptoms (cough, dyspnea, or pneumonia). All patients had biopsy-proven primary lung cancer involving the central airway, and they were not candidates for surgical resection. Non-small-cell carcinoma was the most common (81%) histologic diagnosis. Seventy-two of 75 patients (96%) had received previous treatment (radiation, chemotherapy, or surgery) for endobrochial lung cancer (Table 1). Six patients who died within 30 days after the first interventional bronchoscopy were excluded from the survival analysis. From the remaining 69 patients, 40 patients (group A) underwent interventional bronchoscopy with single-modality treatment consisting of one type of intervention (Nd:YAG laser, stent, PDT, or brachytherapy) applied without association with another type of intervention (Table 2), and 29 patients (group B) underwent a multimodality treatment consisted of a combination of endoscopic interventions in the same procedure or sequentially during the course of the follow-up (Table 3).
For the purpose of our study four different tumor locations of the central airway were considered: trachea, carina, main-stem bronchus, and peripheral (upper or lower segmental bronchi).
Technique
All procedures were performed under general anesthesia [19].
Our technique to perform interventional bronchoscopy for the management of benign and malignant airway stenoses has been previously described [16]. We have followed the safety guidelines of anesthetic management for tracheal obstruction and routinely employed jet ventilation for the management of proximal airway (tracheal) obstruction [13].
Laser resection was performed using the Nd:YAG laser (Surgical Laser Technologies, Montgomeryville, PA, USA). The Nd:YAG laser was utilized on a power setting of 30 watts/1 sec pulse duration. Long pulse duration and voltage were avoided to prevent airway perforation. We used laser for coagulation and complete manual debridement with forceps biopsy and suction tube through the rigid bronchoscopy. The flexible bronchoscopy was utilized through the rigid bronchoscopy to optimize the visualization.
Stenting was performed with the self-expanding metal stent (Ultraflex, Boston scientific, Natick, MA, USA) (Fig. 1) utilizing the same techniques previously described [7, 16]; briefly, rigid bronchoscopic control of the airway is routinely employed during the airway fluoroscopy mapping and deployment of an appropriate length and diameter endobronchial stent.
Patients who underwent photodynamic therapy (PDT) received hematoporphyrin derivative porfimer sodium (Photophrin, Axcan Pharma, Birmingham, AL), intravenously (2.0 to 5.0 mg/kg of body weight) 48 h before light irradiation (argon laser, Biomed 630) [5]. Each patient was carefully and repeatedly warned to avoid exposure to bright light, especially direct and indirect sunlight, for a period of up to 4 weeks. The patient was returned to OR for a second session of PDT and airway debridement after 48 h of the first treatment. Also, 5 days after the first PDT session a routine bronchoscopic debridement was performed.
Brachytherapy was performed with a polyethylene catheter placed 2 to 4 cm distal to the endobronchial tumor by flexible bronchoscopy. The bronchoscopy was withdrawn and the position of the catheter was radiologically confirmed (Fig. 2). High-dose remote loading (HDR brachytherapy—iridium-192) has been utilized.
We routinely aimed at restoring at least 75% of the patency of the airway at any single therapeutic session. A combination of modalities was utilized if less than an estimation of 25% of the airway was restored with any single modality.
Stenting was utilized with other endobronchial intervention when extrinsic compression or extensive residual tumor was noticed. Brachytherapy plus PDT was more utilized when peripheral extension of the obstruction was realized.
Surveillance
Most patients undergoing interventional bronchoscopy were followed with surveillance bronchoscopy 3 weeks after the first procedure. Subsequent bronchoscopy was performed based upon patient’s symptoms and roentgenographic findings.
Statistical analysis
The Student’s t-test and chi-square test were used for comparison of continuous and categorical data respectively. The ANOVA test and the Kruskal-Wallis test were used for comparison of more than two variables. Survival analysis and the log rank test were used to compare differences in survival between the two groups and between subgroups of intervention in group A. Survival curves were calculated by the Kaplan-Meier method [8]. For patients who died or were lost to follow-up, data were censored at the time of death or last documented follow-up. Survival time was defined as the time elapsed from the bronchoscopic diagnosis of endobronchial lung cancer until death or last documented follow-up. A p-value of 0.05 was considered significant.
Results
There were 75 patients (49 male and 26 female), with a median age of 68 years. A total of 176 interventional bronchoscopies were performed with an average of 2.5 ± 0.2 (range from 1 to 11) IB per patient. Laser was the most common modality used for the management of the disease in both groups (Table 4).
There was no statistical difference between the two groups in relation to age, gender, tumor location, histology, type of previous cancer treatment, or length of follow-up (Table 5).
There was a statistically significant difference (p = 0.002) in the mean number of interventional bronchoscopies per patient between group A (1.9 ± 1.2, range 1–5) and group B (3.4 ± 2.6, range 1–11). The number of surveillance bronchoscopie, however, was not significantly different between the two groups (0.77 ± 0.99 vs 0.78 ± 2.1).
The complication rate was 1.7% (3/176). A patient with a carcinoid tumor required lung resection after unsuccessful laser resection. Two patients originally treated with dilation and stenting required additional intervention for stent repositioning. Six patients died within 30 days after the initial procedure. There was no significant difference in the 30-day perioperative mortality after the first intervention between group A (5/45, 11%) and group B (1/30, 3.4%). Five out of the six patients died between the seventh and 30th postoperative day. One patient who presented with airway obstruction and symptoms of acute respiratory failure and hemoptysis died shortly after an emergency bronchoscopy. The 30-day perioperative mortality for patients of both groups who survived the first intervention and underwent additional bronchoscopic treatments was zero.
There was a significant improvement in survival in favor of group B (p = 0.04). The 1- and 3-year cumulative survival rate for groups A and B was 51.3% vs 50% and 2.3% vs 22%, respectively (Fig. 3). The type of modality used among patients of group (single-modality group) had no impact on survival (Fig. 4).
Discussion
Only 20% of patients with lung cancer are candidates for surgical resection with a 5-year survival rate of <30%. Thus, the majority of patients with lung cancer will eventually require palliative treatment [15].
Obstruction of the central airway is frequently encountered in patients with inoperable lung cancer. It may be caused by an intraluminal tumor growth, extrinsic compression (Fig. 5), or weakness of the bronchial wall.
A variety of bronchoscopic techniques are now available for the management of malignant obstruction of the central airway. When the initial goal is tumor debulking (intraluminal tumor growth), laser therapy (Nd-YAG, CO2, argon), electrocautery, cryotherapy, photodynamic therapy, or brachytherapy are the alternatives [1]. Stenting is often preferred for patients with central airway obstruction due to extrinsic compression, weakness of the bronchial wall, or a combination of the above [20]. Because of the progression of the disease, complementary use of these modalities is often required in order to achieve adequate airway patency.
Systematic algorithms have been proposed for the management of airway obstruction; however, the decision as to which modality will be used is often based on individual preference. Interventional bronchoscopy with single-modality treatment is often used because of limited exposure to other modalities, personal bias, or unavailability of specialized equipment [11, 21].
Presently, there is no randomized trial to compare the outcomes (survival, cost, quality of life) of each modality of treatment because of the ethical dilemma created by such life-threatening conditions. Survival benefit from interventional bronchoscopy is difficult to demonstrate because of the lack of randomized trials [12].
An increased of > 4 months in the overall survival was reported after laser treatment when a complete recanalization of the airway occurred [12]. Successful treatment with total recanalization of the airway is observed more frequently when the tumor obstructs a large airway (trachea, main bronchi) (Fig. 6).
Applying a strategy of combination in different modalities of interventional bronchoscopy, simultaneously (laser and stenting, for example) or planned sequentially (laser/stenting/brachytherapy), may improve long-term airway patency. The favorable results in group B (multimodality) reinforce that a clinical approach of periodic bronchoscopic surveillance and intervention may improve survival among patients with bleeding or obstructive malignant airway lesions.
Conclusions
The management of endobronchial lung cancer is a difficult problem. Interventional bronchoscopy with a multimodality approach may improve airway patency and survival. Physicians treating such patients should recognize the limitation of singlemodality therapy and become skilled in utilizing alternative complementary treatment approaches, in order to achieve optimal disease palliation.
References
TV Boxen M Muller B Vemmans P Postmus T Sutedja (1999) ArticleTitleNd Yag laser vs bronchoscopic electrocautery for palliation of symptomatic airway obstruction. A cost effectiveness study. Chest 116 1108–1112 Occurrence Handle10.1378/chest.116.4.1108
S Cavalieri F Venuta P Foccoli C Toninelli B Face ParticleLa (1996) ArticleTitleEndoscopic treatment of malignant airway obstructions in 2,008 patients. Chest 110 1536–1542 Occurrence Handle10.1378/chest.110.6.1536
A Chella MC Ambrogi A Ribechini et al. (2000) ArticleTitleCombined Nd-YAG laser/HDR brachytherapy versus Nd-YAG laser only in malignant central airway involvement: a prospective randomized study. Lung Cancer 27 169–175 Occurrence Handle1:STN:280:DC%2BD3c7msFWmuw%3D%3D Occurrence Handle10.1016/S0169-5002(99)00102-6
DA Cortese JH Kinsey (1982) ArticleTitleEndoscopic management of lung cancer with hematoporphyrin derivative phototherapy. Mayo Clin Proc 57 . Occurrence Handle7109683
DA Cortese JH Kinsey (1984) ArticleTitleHematopophyrin derivate phototherapy in the treatment of bronchogenic carcinoma. Chest 86 8–13 Occurrence Handle1:STN:280:DyaL2c3jsFWgsA%3D%3D Occurrence Handle10.1378/chest.86.1.8
JF Dumon S Shapshay J. Bourcereau S Cavaliere B. Meric N Garbi J Beamis (1984) ArticleTitlePrinciples for safety in appplication of neodymium-YAG laser in bronchology. Chest 86 163–168 Occurrence Handle1:STN:280:DyaL2c3mtVOgug%3D%3D Occurrence Handle10.1378/chest.86.2.163
P Goldstraw G Ladas (1996) Endobronchial stenting. U Sigwart (Eds) Endoluminal stenting WB Saunders Philadelphia
EL Kaplan Meier (1958) ArticleTitleNonparametric estimation from incomplete observations. J Am Statist Assoc 53 457–481 Occurrence Handle10.1080/01621459.1958.10501452
A Katayama T Konishi M Hiraishi K Mafune M Makuuchi (1998) ArticleTitleA combination of laser therapy, radiation therapy, and stent placement for the palliation of complete malignant bronchial obstruction. Surg Endosc 12 1419–1423 Occurrence Handle1:STN:280:DyaK1M%2FktVWhtA%3D%3D Occurrence Handle10.1007/s004649900872
BP Khanavcar P Stern W Albert JA Nakhosteen (1991) ArticleTitleComplications associated with brachytharapy—alone or with laser—in lung cancer. Chest 99 1062–1065 Occurrence Handle10.1378/chest.99.5.1062
P Lee E Kupeli A Mehta (2002) ArticleTitleTherapeutic bronchoscopy in lung cancer. Clin Chest Med 23 241–256 Occurrence Handle10.1016/S0272-5231(03)00075-3
HN Macha KO Becker HP Kemmer (1994) ArticleTitlePattern of failure and survival in endobronchial laser resection. Chest 105 1668–1672 Occurrence Handle1:STN:280:DyaK2c3msFGhsA%3D%3D Occurrence Handle10.1378/chest.105.6.1668
MJ Magee M Klain PF Ferson RJ Keenan RJ. Landreneau (1994) ArticleTitleNasotracheal jet ventilation for rigid endoscopy. Ann Thorac Surg 57 1031–1032 Occurrence Handle1:STN:280:DyaK2c3hvFyrtA%3D%3D Occurrence Handle10.1016/0003-4975(94)90236-4
DJ Mathisen HC Grillo (1989) ArticleTitleEndoscopic relief of malignant airway obstruction. Ann Thorac Surg 48 469–475 Occurrence Handle1:STN:280:DyaK3c%2FisFGjsg%3D%3D Occurrence Handle10.1016/S0003-4975(10)66842-7
CF Mountain (1997) ArticleTitleRevision in the international system for staging lung cancer. . 111 1710–1717 Occurrence Handle1:STN:280:DyaK2szjtVOguw%3D%3D Occurrence Handle9187198
JR Sonett RJ Keenan PF Ferson BP Griffith RD Landreneau (1995) ArticleTitleEndobronchial management of benign, malignant, and lung transplantation airway stenoses. Ann Thorac Surg 59 1417–1422 Occurrence Handle1:STN:280:DyaK2M3ovFOlsg%3D%3D Occurrence Handle10.1016/0003-4975(95)00216-8
A Steptoe J Wardle W Cui et al. (2002) ArticleTitleAn international comparison of tobacco smoking, beliefs and risk awareness in university students from 23 countries. Addiction 97 1561–1571 Occurrence Handle10.1046/j.1360-0443.2002.00269.x
AG Villanueva TCM Lo JF Beamis SuffixJr (1995) ArticleTitleEndobronchial brachytherapy. Clin Chest Med 16 445–454 Occurrence Handle1:STN:280:DyaK28%2FoslCmtQ%3D%3D Occurrence Handle8521699
RS Wilson (1987) Anesthetic management for tracheal reconstruction. HC Grillo H Eschapasse (Eds) International trends in general thoracic surgery, vol 2, Major challenges. WB Saunders Philadelphia 3–12
DE Wood (2001) ArticleTitleAirway stenting. Chest Surg Clin North Am 11 841–861 Occurrence Handle1:STN:280:DC%2BD38%2FlsFaisg%3D%3D
DE Wood (2002) ArticleTitleManagement of malignant tracheobronchial obstruction. Surg Clin N Am 82 612–642 Occurrence Handle10.1016/S0039-6109(02)00025-7
Acknowledgments
The following members of the Division of General Thoracic Surgery of the Allegheny General Hospital helped in collection of data and should be acknowledged: Susan Bartley, RN; Robin Macherey, RN; and Tibetha Santucci, RN.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santos, R.S., Raftopoulos, Y., Keenan, R.J. et al. Bronchoscopic palliation of primary lung cancer: Single or multimodality therapy?. Surg Endosc 18, 931–936 (2004). https://doi.org/10.1007/s00464-003-9202-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-9202-x