Abstract
Background: Sacrococcygeal teratomas (SCT) are classically approached posteriorly through an inverted chevron incision. In large, external, mainly solid SCT, prior interruption of the arterial supply is warranted because of impending heart failure and life-threatening hemorrhagic diathesis. Hitherto, this has required prior laparotomy. A laparotomy is also added when the tumor extends presacrally into the pelvis. The presacral region is, however, difficult to access. A laparoscopic-assisted approach seems to offer a solution for both problems. Methods: A laparoscopic-assisted approach was used in five patients with SCT. In one neonate, it was used to interrupt the arterial blood supply only; in the other four patients, it was used to dissect the internal extension of the tumor. Results: Laparoscopic interruption of the median sacral artery proved to be simple in the neonate with a large, external, mainly solid SCT. In three of the remaining four patients with presacral extension of the tumor, good visualization and dissection of the intrapelvic portion of the tumor was obtained. In one patient, the procedure had to be converted because of a lack of working space due to extensive intraabdominal growth of the tumor. Conclusion: A laparoscopic-assisted approach seems to be ideal for SCT. It provides the opportunity to interrupt the median sacral artery before the dissection. Moreover, it enables far better access to the presacral area than the conventional surgical approach when the SCT extends presacrally into the pelvis. Such a meticulous laparoscopic dissection may improve the functional results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sacrococcygeal teratomas (SCT) have an incidence of 1:35,000 live-born babies and are therefore the most common tumors in the newborn [18]. There are two conditions in which a laparoscopic approach to SCT may offer a distinct advantage over conventional surgery: first, when the child is born with impending heart failure and/or severe coagulation disturbances [2]; second, when a more or less significant portion of the tumor extends presacrally into the pelvis or abdomen, which is the case >50% of patients [1, 9]. For these reasons, we applied a laparoscopic approach in five patients in the period from 1996 through 2002. This experience forms the basis of this report.
Patients and methods
Patients
In the period from 1996 through 2002, four children and one adolescent with SCT underwent laparoscopy at our hospital. Sex, tumor type, tumor consistency (cystic or solid), age at operation, and surgical approach are summarized in Table 1.
Surgical technique
In the neonates, the colon was washed out thoroughly before the operation. Older patients had also an antegrade bowel lavage. Prophylactic antibiotics were given after the induction of anesthesia.
Patients were placed in a supine Trendelenburg position on the operating table. The neonates and infant were placed transversely at the end of the operating table. In these patients, the surgeon stood at the head of the child with the camera operator to his left and the scrub nurse to his right. The principal monitor was at the feet of the patient. In the older patients, the surgeon stood to the right of the patient with the scrub nurse to his right. The camera operator to stood to the left of the patient, and the principal monitor was positioned at the bottom of the table.
The skin was disinfected and draped in such a way that the anus was accessible during the operation. After draping, a urine catheter was inserted for emptying of the bladder when needed.
Using an open technique, a 6-mm cannula was inserted through the inferior umbilical fold for a 5-mm 30° telescope. The pneumoperitoneum was maintained at a pressure of 8 mmHg and a flow of 5 L per min. A secondary cannula was inserted pararectally on each side at umbilical level in the smallest children and lower down in the older patients. Another secondary cannula was inserted in the epigastrium in the smallest children and further to the right and lower down in the older ones. The cannula on the left side was used for retraction; the cannulas on the right were for the working instruments. The secondary cannulas had a diameter of either 3.8 or 6 mm. The uterus was retracted anteriorly with a transabdominal wall stay suture. A Hegar dilator of appropriate size was of great help to push the rectum to the left.
Results
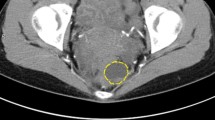
The purpose of the laparoscopic procedure in patient I, who had a large, mainly solid, type I tumor, was interruption of the median sacral artery. The positioning of a child with such a large tumor on the table was not a problem. The artery was easily accessible to the right of the rectum. The appearance of the artery was very pronounced, suggesting substantial blood flow to the tumor. The artery was dissected free and clipped twice. The procedure proved to be easy and lasted only 20 min [2].
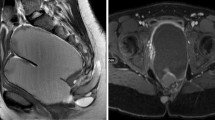
In the remaining four patients, the tumor extended deep into the presacral space. In patient 2, the tumor extended high up into the abdomen. In this patient, the laparoscopic procedure had to be converted because of inadequate working space.
In patient 3, we were able to mobilize the intrapelvic portion of the tumor right up to the coccyx, to which it was firmly adherent. The intrapelvic borders of the tumor were clearly visualized. The median sacral artery, which had a rather small diameter, was coagulated. The patient was then repositioned in a classic prone position, and the tumor was easily removed via a median sacrococcygeal approach, taking the coccyx with the specimen.
Patient 4 had been operated on shortly after birth via a posterior sacrococcygeal approach, but she then developed a recurrent tumor presacrally. At laparoscopy, the tumor appeared to be mainly cystic, but it had a rather large feeding median sacral artery, indicating solid elements as well. The artery was ligated and severed. Mobilization of the intrapelvic part of the tumor proved to be simple, because the boundaries were well defined. The operation was completed through the posterior incision from the previous procedure.
Patient 5, the adolescent had a well-encapsulated mass in the pelvis. The tumor margins were somewhat inflamed, which made the dissection more difficult. The tumor was mobilized to a great extent, but the median sacral artery was not identified. After completion of the laparoscopic procedure, a coccygeal approach with coccygectomy was undertaken. The tumor, however, was still adherent to the anterior surface of the sacrum. It was detached bluntly, resulting in considerable bleeding. During the removal, the tumor was opened; it appeared to contain hair and sebaceous material.
All five patients did well postoperatively. None of the tumors were malignant.
Discussion
SCT can lead to hydrops in utero [8]. When this occurs before lung maturity is reached, the prognosis is very poor. Resection of the teratoma in the fetus and radiofrequency ablation have been described, but these methods have not gained popularity [6, 8, 12]. Children with large, mainly solid SCT are often born with impending heart failure and marginal coagulation equilibrium due to high vascularity of the tumor. Tumor rupture leading to fatal bleeding during delivery, even during cesarean section, has been reported [10, 17]. When the tumor is approached via a posterior sacrococcygeal incision without prior ligation of the median sacral artery, death may occur due to massive bleeding and cardiac failure [5, 15, 19]. This phenomenon is undoubtedly related to the high vascularity of the tumor and the fact that the venous drainage is interrupted before the arterial supply. This problem has been recognized for a long time, and several reports have described cases in which the arterial supply was interrupted first, either by ligation of the median sacral artery or by sling interruption of the aorta [3, 13]. The median sacral artery is apparently the main arterial supply to these tumors. In 1998, we published the first description of the laparoscopic interruption of the median sacral artery [2]. It proved to be very simple. If the hemodynamic equilibrium of the neonate is marginal, the wisest course may be to interrupt the median sacral artery laparoscopically first and to defer further dissection until a stable hemodynamic condition is reached.
A laparoscopic-assisted approach is also prudent when the SCT extends presacrally into the pelvis or even into the abdomen. This is the case tumors graded as type II, III, or IV according to the classification of Altman et al; these tumors comprise ≥50% of all SCT [1, 9]. With a sacrococcygeal approach, the presacral view is highly limited, and blind dissection may easily lead to bleeding and damage to the nerves of the anorectum and urogenital system. Nor is a classic transabdominal approach to the presacral region optimal. Although the results after traditional surgical techniques were reported to be very good for a long time, more recent follow-up studies give another picture [4, 9, 14, 16]. Fecal and urinary problems apparently occur more frequently than has been generally believed. These studies leave no doubt that the laparoscopic approach to the presacral region provides a much better view and easier access than either a sacrococcygeal or classic transabdominal approach.
Our experience with type II, III, and IV SCT so far indicates that this approach has great potential. When the tumor is mainly cystic, the visibility may be improved by transabdominal wall puncture of the cystic component. Such a procedure could have prevented the conversion in patient 2. Antenatal decompression of mainly cystic SCT by transabdominal puncture has been described as a means of enabling vaginal delivery [7, 11]. One could dispute the wisdom of this approach with respect to malignancy, but malignancy is rare in the newborn, especially when the lesion is mainly cystic. In future patients, we will pay more attention to the median sacral artery, even when the tumor is not very large. This could have prevented considerable blood loss in the patient with a type IV lesion.
The series presented here is too small to predict a better functional outcome for certain. It leaves no doubt, however, that a laparoscopic approach to the presacral area enables far better visualization of this area than either a classic transabdominal or sacrococcygeal approach. Better surgery and better results may therefore be expected.
References
RP Altman JG Randolf JR Lilly (1974) ArticleTitleSacrococcygeal teratoma: American Academy of Pediatrics Surgical Section Survey—1973. J Pediatr Surg 9 389–398 Occurrence Handle4843993
NMA Bax DC van der Zee (1998) ArticleTitleLaparoscopic clipping of the median sacral artery in huge sacrococcygeal teratomas. Surg Endosc 12 882–883 Occurrence Handle10.1007/s004649900735 Occurrence Handle1:STN:280:DyaK1c3mslegsA%3D%3D Occurrence Handle9602012
JFR Bentley (1968) Coccygeal teratoma (sacrococcygeal tumour). C Rob R Smith (Eds) Operative surgery: pediatric surgery; vol V, pt 2. 2nd ed. Butterworths London 824–829
TM Boemers JD van Gool TP de Jong KM Bax (1994) ArticleTitleLower urinary tract dysfunction in children with benign sacrococcygeal teratoma. J Urol 151 174–176 Occurrence Handle1:STN:280:ByuD2snkvFI%3D Occurrence Handle8254808
SJ Bond MR Harrison KG Schmidt NH Silverman AW Flake RN Slomick RL Anderson SL Warsof DC Dyson (1990) ArticleTitleDeath due to high output cardiac failure in fetal sacrococcygeal teratoma. J Pediatr Surg 25 1287–1291 Occurrence Handle1:STN:280:By6C2c%2Fjs1I%3D Occurrence Handle2286911
T Chiba CT Albanese RW Jennings RA Filly JA Farrell MR Harrison (2000) ArticleTitleIn utero repair of rectal atresia after complete resection of a sacrococcygeal teratoma. Fetal Diagn Ther 15 187–190 Occurrence Handle10.1159/000021003 Occurrence Handle1:STN:280:DC%2BD3c3ksFantA%3D%3D Occurrence Handle10782007
AM Garcia WM III Morgan JP Bruner (1998) ArticleTitleIn utero decompression of a cystic grade IV sacrococcygeal teratoma. Fetal Diagn Ther 13 305–308 Occurrence Handle10.1159/000020859 Occurrence Handle1:STN:280:DyaK1M%2Fjt1yksQ%3D%3D Occurrence Handle9813425
JL Graf CT Albanese RW Jennings JA Farrell MR Harrison (2000) ArticleTitleSuccessful fetal sacrococcygeal teratoma resection in a hydropic fetus. J Pediatr Surg 35 1489–1491 Occurrence Handle10.1053/jpsu.2000.16420 Occurrence Handle1:STN:280:DC%2BD3crgt1Oitg%3D%3D Occurrence Handle11051157
P Havranek H Hedlund A Rubenson D Guth M Husberg T Frykberg LT Larsson (1992) ArticleTitleSacrococcygeal teratoma in Sweden between 1987 and 1989: long-term functional results. J Pediatr Surg 7 916–918
T Hoehn MF Krause C Wilhelm U Lattermann KD Rueckauer (1999) ArticleTitleFatal rupture of a sacrococcygeal teratoma during delivery. J Perinatol 19 596–598 Occurrence Handle10.1038/sj.jp.7200232 Occurrence Handle1:STN:280:DC%2BD3c7htVWhsQ%3D%3D Occurrence Handle10645528
S Kay S Khalife JM Laberge K Shaw L Morin H Flageole (1999) ArticleTitlePrenatal percutaneous needle drainage of cystic sacrococcygeal teratomas. J Pediatr Surg 34 1148–1151 Occurrence Handle1:STN:280:DyaK1MzmvFaitw%3D%3D Occurrence Handle10442611
YH Lam MH Tang TW Shek (2002) ArticleTitleThermocoagulation of fetal sacrococcygeal teratoma. Prenat Diagn 22 99–101 Occurrence Handle10.1002/pd.230 Occurrence Handle11857611
H Lindahl (1988) ArticleTitleGiant sacrococcygeal teratoma: a method of simple intraoperative control of hemorrhage. J Pediatr Surg 23 1068–1069 Occurrence Handle1:STN:280:BiaB3MnktVY%3D Occurrence Handle3244094
PS Malone L Spitz EM Kiely RJ Brereton PG Duffy PG Ransley (1990) ArticleTitleThe functional sequelae of sacrococcygeal teratomas. J Pediatr Surg 25 679–680 Occurrence Handle1:STN:280:By%2BB1Mvgs1c%3D Occurrence Handle2359006
JJ Murphy GK Blair GC Fraser (1992) ArticleTitleCoagulopathy associated with large SCT. J Pediatr Surg 27 1308–1310 Occurrence Handle1:STN:280:ByyD38%2FgtVI%3D Occurrence Handle1403511
R Rintala P Lahdenne H Lindahl M Siimes M Heikinheimo (1993) ArticleTitleAnorectal function in adults operated for benign sacrococcygeal teratoma. J Pediatr Surg 28 1165–1167 Occurrence Handle1:STN:280:ByuC2c7mslQ%3D Occurrence Handle8308684
W Serlo (1984) ArticleTitleTotal rupture of giant sacrococcygeal teratoma. Z Kindechir 39 405–406 Occurrence Handle1:STN:280:BiqC3MjlvVA%3D
MA Skinner (1997) Germ cell tumors. KT Oldham PM Colombani RP Foglia (Eds) Surgery of infants and children. Lippincott-Raven Philadelphia 653–662
D Teitelbaum S Teich S Cassidy M Karp D Cooney G Besner (1994) ArticleTitleHighly vascularized sacrococcygeal teratoma: description of this atypical variant and its operative management. J Pediatr Surg 29 98–101 Occurrence Handle1:STN:280:ByuC28rpsVE%3D Occurrence Handle8120774
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bax, N., van der Zee, D. The laparoscopic approach to sacrococcygeal teratomas . Surg Endosc 18, 128–130 (2004). https://doi.org/10.1007/s00464-003-9093-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-9093-x