Abstract
This study aims to compare the effectiveness of conventional dysphagia therapy (CDT), neuromuscular electrical stimulation (NMES), and transcranial direct current stimulation (tDCS) in the treatment of post-stroke dysphagia. A single-blind randomized controlled trial was conducted with 40 acute stroke patients – 18 females and 22 males with a mean age of 65.8 ± 11.9. The subjects were grouped into 4, with 10 individuals in each. The procedures administered to groups were as follows: the first group, sham tDCS and sham NMES; the second group, tDCS and sham NMES; the third group, NMES and sham tDCS; and the fourth group, all therapy procedures. CDT was applied to all groups either as a standalone procedure or combined with one or two of the instrumental techniques. Gugging Swallowing Screen (GUSS) and Videofluoroscopic Swallowing Study (VFSS) were employed to determine the severity of dysphagia and the effectiveness of treatment modalities. Additionally, the Penetration Aspiration Scale (PAS), Functional Oral Intake Scale (FOIS), and Dysphagia Severity Rating Scale (DSRS) were administered to interpret VFSS data. Pre- and post-treatment comparisons of all groups have revealed a statistically significant difference for all parameters except for the PAS scores at International Dysphagia Diet Standardization Initiative (IDDSI)-Level 4 consistencies. However, the differences between pre- and post-treatment scores of the fourth group across all parameters were significant – GUSS (p = 0.005), FOIS (p = 0.004), DSRS (p = 0.005), PAS IDDSI-4 (p = 0.027), PAS IDDSI-0 (p = 0.004). Inter-group comparisons, on the other hand, pointed out that the difference between pre- and post-treatment GUSS, FOIS, DSRS, and PAS scores at IDDSI Level-0 consistencies was statistically significant for all groups – GUSS (p = 0,009), FOIS (p = 0,004), DSRS (p = 0,002), PAS IDDSI-0 (p = 0,049). Closer examination of treatment groups indicated that the tDCS + CDT group, the NMES + CDT group, and the group that underwent the combination of three modalities made better progress than the one that was treated with only CDT. Though not statistically significant, the NMES + CDT group achieved better improvement than the tDCS + CDT group. This study has yielded that the group in which NMES, tDCS, and CDT were applied in combination has achieved better results than all the other groups. All treatment modalities applied to accelerate the general recovery process in acute stroke patients with dysphagia were found to be effective for the treatment of post-stroke swallowing disorders. The use of instrumental treatments such as NMES and tDCS enhanced the effectiveness of the treatment and provided more significant progress. Furthermore, combining treatment modalities such as NMES and tDCS was more effective when compared to using only conventional therapy. As a result, the most effective treatment outcomes were obtained by the group receiving CDT, NMES, and tDCS in combination. Therefore, the use of combined approaches has been recommended in appropriate patients; yet the provisional results should be tested in randomized trials with more participants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Swallowing disorder is a common cause of mortality and morbidity in post-stroke patients [1, 2]. Regardless of the differences such as the duration of the disease and the location of the lesion, dysphagia is especially seen in the first three months after a stroke, which is a critical period for stroke patients [3].
Studies investigating post-stroke swallowing disorders generally expand across acute and subacute periods. Dysphagia manifests during the acute period in more than half of the patients [4].
As dysphagia persists after the stroke, patients face complications such as malnutrition, dehydration, weight loss, aspiration, and death. Such complications increase the length and cost of hospitalization. Moreover, when dysphagia is not treated, the potential problems after discharge turn into a burden for the caregiver, limit the daily-life skills of the patients, and reduce the quality of life for both [5]. Early diagnosis and treatment of dysphagia in stroke patients not only reduces the complications but also improves the functional status and accelerates the rehabilitation of swallowing. The fastest recovery happens in the first three weeks following the stroke. Thus, initiating therapy quickly and effectively without waiting for the natural recovery process will increase the rehabilitation rate of the treatment for post-stroke swallowing disorders.
Treatment of swallowing disorders aims to prevent possible complications and to ensure that the patient can safely take sufficient amounts of fluid and food during the day [6]. Depending on the cause, symptoms, and type of the swallowing disorder, different procedures are used for the treatment, which can be classified into three groups—conventional swallowing therapy, peripheral stimulation methods, and central stimulation methods.
Following the acknowledgment of the effect that neural plasticity has on the rehabilitation of post-stroke swallowing disorders, relevant treatment procedures shifted toward the neural system and the re-organization of the neural connections in the brain. Accordingly, the neuromodulator treatment modalities that enhance the brain's capacity to re-organize its neural connections have proved promising for the treatment of swallowing dysfunction. These modalities include peripheral sensorimotor stimulation like NMES and central stimulation like TMS and tDCS [7].
The use of NMES in swallowing treatment aims to facilitate the movement of the muscles involved in the swallowing function by stimulating peripheral motor neurons. The working principle of NMES is both an imitation of motor neurons that innervate the muscle fibers and an indirect stimulation creating muscle contraction via motor neurons. In doing so, the overarching aim of the procedure is to eliminate weakness in the muscles responsible for swallowing [8]. The stimulation created by the electric current leads to sufficient innervation in the peripheral nerves that trigger muscle contraction for healthy swallowing. Such innervation assists re-organization of the neural connections for the involved muscles [9]. In addition to strengthening the oropharyngeal muscles, peripheral electric stimulation also improves the conduction through afferent pathways, which enhances the oropharyngeal sensory feedback that supports cortical re-organization critical to the oropharyngeal swallowing [10,11,12]. It is well documented that NMES strengthens the contraction of Type-II muscle fibers [9, 11, 13, 14]. On the other hand, the activation of Type-I muscle fibers is achieved by conventional swallowing treatment. Thus, the integration of NMES into conventional swallowing procedures has been reported to produce better results on both types of muscle fibers, which improves the overall quality of the treatment process [9, 11, 13, 14].
NMES creates sensory and motor stimulations with the lowest amplitude that clients feel and with the amplitude that muscle contraction is observable, respectively [15]. Relevant research endeavors suggest that NMES can rehabilitate both sensory and motor functions involved in swallowing and can help clients gain better coordination during swallowing [15,16,17].
Literature is densely populated with studies examining the effectiveness of NMES. Meta-analysis research investigating articles published in the relevant body of literature until 2022 points out that use of NMES together with conventional treatment procedures is more effective than using only conventional techniques regardless of the duration after the stroke, number of sessions, and success criteria [18,19,20].
In addition to conventional swallowing exercises and NMES, recently Non-Invasive Brain Stimulation (NIBS) procedures have been added to the modalities employed to treat swallowing disorders. In NIBS treatment, the cortical plasticity is improved by directly stimulating the cortex. Two NIBS methods, Transcranial Direct Current Stimulation (tDCS) and Transcranial Magnetic Stimulation (TMS) are effectively used for cortical re-organization. Research results have shown that the non-involved motor cortex re-organizes itself in clients who recover from post-stroke dysphagia, but such a change is not recorded for those with persisting swallowing disorders [21, 22]. NIBS methods are acknowledged to rehabilitate clients with a hemispheric impairment by stimulating the motor cortex [23]. tDCS, one of the NIBS methods, is a non-invasive brain stimulation technique that uses direct current to enhance neural plasticity and allows the combination of swallowing maneuvers and exercises [24]. The reasons to prefer this method include ease of use, low cost, tolerability, and safety during both acute and sub-acute stages. The literature holds evidence that tDCS improves motor functions in clients with chronic stroke and that anodal tDCS applied to the pharyngeal motor cortex enhances the excitability of the pharynx [25,26,27].
The highest neurological recovery after the stroke occurs within the first three months [28, 29]. Great effort is put into action especially during this period to facilitate the treatment of post-stroke swallowing disorders. Therefore, identifying the most effective treatment options for post-stroke dysphagia in the acute and subacute stages is of clinical significance, especially for inpatient stroke rehabilitation. In addition to conventional dysphagia therapy, relevant literature indicates that the most effective therapy modalities for the treatment of post-stroke dysphagia in the acute and subacute stages are transcranial magnetic stimulation, transcranial direct current stimulation (TMS and tDCS), both of which are non-invasive brain stimulation procedures that modulate the depolarization of the cortical neurons by triggering magnetic or electric fields, and neuromuscular electric stimulation (NMES), which stimulates the muscle fibers by activating the peripheral sensory system and increases the contraction and strength of the muscles [30,31,32].
In their meta-analysis, Wang et.al (2021) conclude that non-invasive neurostimulation treatment modalities (TMS, tDCS, and NMES) are effective for the rehabilitation of post-stroke dysphagia, and this effect is substantially remarkable in the acute stage [30], which is compatible with Cheng et al. (2020) [31].
Since NMES and non-invasive brain stimulation procedures can improve motor recovery by ameliorating use-dependent plasticity impairment after stroke [33], the application of peripheral and central stimulation techniques in combination has been deemed to accelerate rehabilitation.
The literature review yields several studies in which non-invasive brain stimulation techniques and NMES are applied at the same time or separately from conventional swallowing therapy. However, the studies where non-invasive brain stimulation techniques and NMES are applied in combination are relatively fewer. Zhang et.al (2018) tested the use of rTMS—another non-invasive brain stimulation technique—with NMES and reported that the combined application of two instrumental modalities was superior [34]. For this reason, it was hypothesized that using both peripheral and central stimulation procedures together for the treatment of post-stroke dysphagia would be more effective than CDT or any adjunct therapy alone and could accelerate the recovery process in stroke patients. Besides, there is a scarcity of comprehensive studies examining the effects of therapy modalities used in swallowing disorders and the superiority of their combinations over other therapeutic approaches.
This study aims to determine the effectiveness of conventional dysphagia therapy (CDT), neuromuscular electric stimulation (NMES), and transcranial direct current stimulation (tDCS) in swallowing disorders after acute stroke, and to compare the effectiveness of each treatment modality when used in combination and isolation.
Method
Subjects
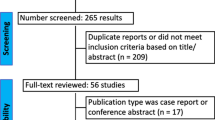
This study was conducted at Istinye University Liv Hospital Stroke Center between January 2020 and April 2021 with a sample of 40 randomly selected patients who developed a swallowing disorder after acute stroke (0–30 days).
Patients diagnosed with unilateral hemispheric stroke (ischemic or hemorrhagic) constitute the research sample. The exclusion criteria for the subjects were as follows: having typical neurological findings for brain stem stroke, lack of sitting balance for a long time, not being able to maintain an upright position with or without support, having tumors or neoplastic disease in the head-neck region and receiving radiotherapy to the neck, the presence of additional musculoskeletal diseases, having a neurological disease-other than stroke-that may cause swallowing disorder, wearing a pacemaker or ear tube, and having a previous stroke and/or epileptic seizure history. This study was approved by the Ethics Boards and Commissions of Uskudar University and conducted following the Declaration of Helsinki (Protocol Number: 99102440).
Study Design
This study was designed as a “single-blind” randomized controlled clinical trial. A pretest–posttest experimental model was applied to evaluate the effectiveness of conventional dysphagia therapy (CDT), neuromuscular electric stimulation (NMES), and transcranial direct current stimulation (tDCS) for post-stroke swallowing disorders.
24 h after the stroke, the Gugging Swallowing Screen (GUSS) was administered to the patients for bedside assessment. Patients determined to have swallowing disorder were further subjected to a Videofluoroscopic Swallowing Study (VFSS) as soon as their medical status was stable (min: 2 days max: 7 days, mean: 3.1 ± 2.5 days). The patients to be included in the study were randomly assigned into 4 groups with 10 individuals in each by using a computer-based software (Random Allocation Software 2.0), and the treatment sessions started on the same day. 10 treatment sessions were administered to each group for an hour a day, five days a week, and across two weeks. The first group received sham tDCS and sham NMES, the second group was administered tDCS treatment and sham NMES, the third group was treated with NMES and sham tDCS, and the fourth group received NMES together with tDCS treatment. All groups received Conventional Dysphagia Therapy. Accordingly, the groups were formed as follows:
-
Group 1: CDT+Sham tDCS+Sham NMES
-
Group 2: tDCS+CDT+Sham NMES
-
Group 3: NMES+CDT+Sham tDCS
-
Group 4: tDCS + NMES + CDT
Group 1
CDT was applied to the first group for an hour across 10 sessions. During the application, patients first received sham tDCS for 20 min and then sham NMES for 40 min.
Group 2
The second group received 2 mA anodal tDCS for 20 min to the pharyngeal motor cortex area on the unaffected hemisphere for 10 sessions, and then a 40-min sham NMES therapy was applied. In addition, conventional dysphagia therapy was administered.
Group 3
In the third group, sham tDCS was applied for 20 min after a 40-min NMES therapy for 10 sessions. Additionally, conventional dysphagia therapy was presented.
Group 4
2 mA Anodal tDCS was applied for 20 min to the pharyngeal motor cortex area on the unaffected hemisphere for 10 sessions, which was followed by a 40-min NMES therapy. Besides, conventional dysphagia therapy was provided.
At the end of the treatment process, the patients were re-evaluated through a videofluoroscopic swallowing study. The flowchart showing the course of action for the research is given in Fig. 1.
Assessment Procedure
Nutritional Status Assessment
The dietary patterns of the patients at the time were classified in line with the Functional Oral Intake Scale (FOIS) after the VFSS evaluation, and the food intake before and after the treatment was evaluated accordingly. The FOIS is a 7-step scale developed for the functional assessment of swallowing [35]. According to the FOIS, individuals at levels 1–3 are tube dependent while those at levels 4–7 can take total oral nutrition [36]
Swallowing Function Assessments
Clinical Assessment
The patients' clinical dysphagia assessment was completed with the GUSS, which is a standardized swallowing screening tests used especially for patients with acute stroke. Providing dietary recommendations as well as screening for the aspiration risk, the GUSS is a frequently used clinical tool [37]. On the GUSS, the patients are scored over 20 points: 0–9 severe, 10–14 moderate, and 15–19 mild dysphagia. A maximum score of 20 is considered typical swallowing [37, 38].
Instrumental Assessment
Objective assessment of swallowing before and after the treatment process was completed through VFSS, which is widely used in the assessment of swallowing disorders and is considered the gold standard [39].
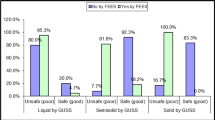
Philips DuoDiagnost 2008 fluoroscopy device was used for the VFSS assessment. The subjects were seated upright in a wheelchair at a 90° angle and 1.5 m away from the X-ray tube with their heads stabilized laterally. Continuous fluoroscopy was used for all examinations. VFSS were recorded and digitally captured at 30 frames per second. The fluoroscope was positioned for the following boundaries to be visible on the images: the lips anteriorly, the posterior pharyngeal wall posteriorly, the cervical esophagus inferiorly, and the nasopharynx superiorly. All the subjects underwent the same standard VFSS protocol through 3 swallowing trials with each of the two consistencies. E-Z-HD barium sulfate powder for suspension (98% w/w) was used as the contrast agent. In the statistical analysis, 5 ml IDDSI Level-0 for liquids and 5 ml IDDSI Level-4 for semi-solid consistencies were used as the criteria (IDDSI—International Dysphagia Diet Standardization Initiative). The footage recorded during VFSS was evaluated using the Penetration Aspiration Scale (PAS) and the Dysphagia Severity Rating Scale (DSRS). Following the administration of VFSS, the nutritional status of each subject was determined according to the FOIS results.
PAS is used to define the severity of penetration and aspiration on an 8-point clinical scale and to determine whether material entering the airway is expelled [40].
DSRS is a scale between 0 and 6 used to determine the severity of swallowing disorder and to support the instrumental findings. According to this scale, 0 and 6 indicate normal swallowing and severe dysphagia, respectively [41].
Following the treatment, the patients were re-evaluated through another videofluoroscopic swallowing study with the same standard protocol, and the video footage was recorded on a digital video file. Before and after the treatment, the footage was evaluated and scored by another Speech and Language Therapist experienced in the field and blind to the details about the subjects and therapy groups.
Treatment Procedure
Conventional Dysphagia Therapy (CDT)
For conventional dysphagia therapy, the same standard exercise program was applied to the subjects for an hour a day, five days a week, and across two weeks. The subjects who were allowed to receive oral intake were treated through compensatory methods such as diet modification and appropriate head positioning as well as through behavioral maneuvers including the Masako maneuver, and supraglottic and effortful swallowing (42,43). The Masako maneuver was practiced minimally for 10 repetitions across three sets.
The NPO subjects, on the other hand, were presented with thermal tactile stimulation to trigger the swallowing reflex, ROM exercises for the tongue, and resistant tongue base exercises [44, 45]. Repetitive swallowing exercises were facilitated with ice chips to increase salivation. The ROM exercises for the tongue were performed minimally for ten repetitions in each direction for three sets. The subjects were given a couple of minutes to rest when transitioning from one exercise to the next.
tDCS
Produced by ActiveTek Inc. and approved by Food and Drug Administration (FDA), ActivaDose® II, a battery-driven neurostimulator, was used for the tDCS therapy. Sponge electrodes covering an area of 25 cm2 with 5 × 5 cm boundaries were immersed into an isotonic solution to reduce the resistance, the scalp was cleaned by rubbing alcohol, the electrodes were fixed in their places, and the stimulation was presented at 2 mA for 20 min.
Important cortical structures related to swallowing are the insular cortex and the opercular region [48]. The insula is the most common lesion site in unilateral stroke patients with dysphagia [46]. The opercular cortex covers the top of the insula and has a recognized role in swallowing. Studies indicate that lesions of the insular cortex and the internal capsule are significantly associated with the risk of post-stroke dysphagia and acute aspiration [47]. Research also shows that the insular cortex is the main cortical area leading to aspiration after an ischemic stroke [46, 47]. These findings conclude that the insula has a key function in the regulation of both voluntary and automatic swallowing that determines the risk of aspiration.
In the current study, anodal stimulation was administered to the pharyngeal motor cortex of the unaffected hemisphere. It was hypothesized that the opercular region and the insula, both of which are critical for swallowing function and located toward the depth of the pharyngeal cortex area, would indirectly benefit from the stimulation. In line with the International EEG 10/20 system, the anodal electrodes were placed on C5 for the left hemisphere and C6 for the right one. To determine the C5-C6 areas, the distance between the two tragi was measured, and an imaginary boundary was outlined by moving toward the vertex as much as 20% of the calculated distance between the two tragi. The cathodal electrode, on the other hand, was placed onto the contralateral hemisphere within the Fp1-Fp2 regions, which are the right-left supraorbital regions.
Two types of stimulation, real and sham, were used in the study. The subjects in the real stimulation group were presented with direct electric current. In this step, the amplitude of the electric current was gradually increased to 2 mA within the first 30 s and then stabilized for 20 min. Electrode placement procedures used for real stimulation were kept the same for the sham group. Subsequently, the electric current was administered and discontinued within 30 s after the subjects felt the increase in amplitude. Both groups were also provided with conventional swallowing therapy within the same session (Fig. 2).
NMES
VitalStim® (The Chattanooga Group, Hixson, TN) and appropriate electrodes were used for Neuromuscular Electrical Stimulation. The application was performed by the researcher who had completed VitalStim® official certification program. In each session, the default Vitalstim® program (80 Hz frequency and 700 µs fixed biphasic duration) was administered for 40 min. For the electrical current to be fully transmitted and to increase surface contact of the electrodes, the neck area of the male patients where the electrodes would be placed was shaved and wiped with Uni-Patch™ Pre-TENS Skin Prep Wipes manufactured by COVIDEN™, and the electrodes were fixed with elastic bands.
Recently, several studies have investigated the effectiveness of treatment in terms of electrode placement during the NMES procedure. In a meta-analysis study, Doan et. al (2022) report that horizontal placement of electrodes leads to more effective outcomes compared to other alternatives [20]. Accordingly, the horizontal plane was chosen among alternatives in the certification program for electrode placement (Fig. 3).
Two stimulation types, real and sham, were administered during the NMES application, too. In real stimulation, the subjects were presented with neuromuscular electric stimulation. During the presentation, the amplitude of the current was gradually increased until the muscle contraction was observed, and then it was stabilized at the same level for 40 min.
As for the sham presentation, no electric current was administered to the subjects. The same placement procedures followed for the real stimulation were exactly repeated for this group. Subsequently, the electric current was presented and discarded within 30 s immediately after the patients felt the increase in amplitude. Both groups were also treated with conventional swallowing therapy in the same session.
Statistical Analysis
The change after the application of conventional dysphagia therapy, neuromuscular electric stimulation, and transcranial direct current stimulation was statistically analyzed through SPSS 26.0 package program. The normality distribution of the data was tested with the Shapiro–Wilk test. The statistical analysis of change across therapy groups before and after the therapy was evaluated using the Wilcoxon signed-rank test.
Kruskal Wallis test was employed to compare the effectiveness of conventional therapy, neuromuscular electric stimulation, and transcranial direct current stimulation in the treatment of post-stroke swallowing disorders. Mann Whitney U test was completed to evaluate the effect of treatment procedures across the parameters. The statistical significance criterion was set to below 0.05 p-value.
Results
Forty patients with post-stroke swallowing disorders were included in the current study—4 groups, 10 subjects in each group. 18 (45%) of the participants were female and 22 (55%) were male. Their mean age was 65.8 (± 11.9) years. As for the stroke types, 36 (90%) were diagnosed with and ischemic stroke while 4 (10%) had a hemorrhagic stroke diagnosis. As regards the lesion sites, 14 (35%) and 26 (%65) patients had lesions in the right and left hemispheres, respectively. The mean stroke severity of the participants was calculated as 10.9 (± 4.8). The descriptive characteristics of the subjects across groups are given in Table 1.
The distribution of the subjects across treatment groups was homogenous with no statistically significant difference in terms of age, gender, stroke type, lesion site, and NIHSS scores (p > 0.05). In addition, the baseline data were analyzed to figure out if the distribution of the groups was homogeneous or not before the treatment process. As a result, groups also had a homogeneous distribution across the GUSS, FOIS, DSRS, and PAS scores before the treatment started.
Pre- and Post-Treatment Results of Therapy Modalities
In this study, the effectiveness of treatment was examined for conventional swallowing therapy (CDT), neuromuscular electric stimulation (NMES), and transcranial direct current stimulation (tDCS), and the findings are presented in Table 2.
Average scores from the GUSS (p = 0.005, p = 0.005, p = 0.007, p = 0.005), FOIS (p = 0.016, p = 0.004, p = 0.004, p = 0.004), and DSRS (p = 0.007, p = 0.004, p = 0.005, p = 0.005) scales pointed to a statistically significant difference between pre- and post-treatment conditions for all groups.
Concerning treatment effectiveness, the PAS scores at IDDSI Level-4 consistencies improved after the therapy for the first group receiving conventional dysphagia therapy (CDT), the second group receiving tDCS and CDT, and the third group receiving NMES and CDT. Yet, the improvement was not statistically significant (p = 0.66, p = 0.66, p = 0.102). On the other hand, a statistically significant difference was determined between pre- and post-treatment PAS scores at IDDSI Level-4 consistencies (p = 0.027) obtained by the fourth group receiving all three treatment modalities in combination (tCDS + NMES + CDT). Regarding IDDSI Level-0 consistencies, a significant difference was found between pre- and post-treatment scores for all groups (p = 0.007, p = 0.007, p = 0.005, p = 0.004). The comparison of the scores shows that the highest difference between pre- and post-treatment scores recorded for this parameter was achieved by the group receiving all three therapy modalities (tCDS + NMES + CDT).
Comparison of Therapy Modalities Across Assessment Parameters
Kruskal Wallis test was administered to determine if treatment modalities were effective, and if so, which modality was the most effective. The results are given in Table 3.
The comparison of the treatment modalities across assessment parameters yielded a statistically significant difference for the scores obtained from the GUSS (p = 0,009), FOIS (p = 0,004), DSRS (p = 0,002), and PAS at IDDSI Level-0 consistencies (p = 0,049) in favor of the group receiving three modalities in combination (tCDS + NMES + CDT). However, the PAS scores at IDDSI Level-4 consistencies did not significantly differ across the groups (p = 0.418).
Individual Comparison of Therapy Modalities Across Assessment Parameters
To determine which treatment modality was more effective across the assessment parameters, the results were compared as shown below. Mann Whitney U test was employed to find out the difference among the parameters across the treatment modalities. The results are presented in Table 4.
Accordingly, the group in which NMES and CDT were applied together showed a greater improvement compared to the group receiving only CDT. In the GUSS (p = 0.03), FOIS (p = 0.02), and DSRS (p = 0.007) parameters, the difference between the groups was statistically significant in favor of the NMES group. There was no statistically significant difference in terms of the PAS scores at IDDSI Level-4 (p = 0.656) and Level-0 consistencies (p = 0.114).
When the group receiving only CDT was compared with the group receiving both tDCS and CDT, the latter showed greater improvement, yet this difference was statistically significant only for DSRS but not for GUSS (p = 0.117), FOIS (p = 0.69), and PAS scores and IDDSI Level-4 (p = 0.669) and Level-0 (p = 0.564) consistencies. A statistically significant difference was found in favor of the tDCS group in the DSRS parameter (p = 0.037).
The group that received all three treatment procedures together showed much greater improvement than the CDT group alone. The difference between the groups concerning GUSS (p = 0.004), FOIS (p = 0.002), DSRS (p = 0.002), and PAS scores at IDDSI Level-0 (p = 0.011) consistencies were found to be statistically significant in favor of the group that received all three modalities together. There was no statistically significant difference regarding PAS scores at IDDSI Level-4 consistencies (p = 0.350).
Likewise, no statistically significant difference was found when the NMES and tDCS groups were compared GUSS (p = 0.338), DSRS (p = 0.460), FOIS (p = 0.175), PAS IDDSI-4 (p = 0.859), PAS IDDSI-0 (p = 0.316).
The group that received all three therapies together showed greater improvement than the group that received tDCS and CDT. The difference between the groups in terms of the GUSS (p = 0.023), FOIS (p = 0.034), and DSRS (p = 0.021) parameters was statistically significant in favor of the group that received all three therapies in combination. There was no statistically significant difference concerning the PAS scores at IDDSI Level-4 and Level-0 consistencies (p = 0.144, p = 0.067).
Similarly, the difference was not statistically significant between the group that received NMES treatment and the group that received three modalities together although the results for the latter were better—GUSS (p = 0.248), FOIS (p = 0.158), DSRS (p = 0.272), PAS IDDSI-4 (p = 0.170), PAS IDDSI-0 (p = 0.130).
Discussion
This study evaluated the effects of conventional dysphagia therapy (CDT), neuromuscular electric stimulation (NMES), and transcranial direct current stimulation (tDCS) procedures in the treatment of swallowing disorders following an acute stroke.
Pre- and post-treatment assessments of the subjects were carried out both clinically and instrumentally by using the GUSS scale and VFSS, respectively. The VFSS images were evaluated by using the PAS and DSRS. Following the administration of VFSS, the nutritional status was determined according to FOIS results of each subject.
Many of the techniques in conventional dysphagia therapy had been scientifically proven to be effective before they were acknowledged within the relevant body of research [48]. Since working any muscle system intensely and constantly has been documented to lead to changes in the neural innervation and patterns of movement [49, 50], functional exercises involving actual swallowing produce more long-term gains than other techniques applied within the scope of conventional dysphagia therapy. The common goal of exercises based on actual swallowing is to support neuroplasticity by re-training the neuromuscular system [48]. In the current research, effortful swallowing, the Masako exercise, and supraglottic swallowing exercises were employed as conventional dysphagia therapy. The results have indicated that the group receiving only conventional swallowing therapy recorded a statistically significant improvement between pre- and post-treatment assessments across all parameters, which is compatible with the literature. [51, 55].
NMES, the second modality in the study, has been a frequently preferred treatment procedure for dysphagia in recent years [4]. So far, many studies have investigated NMES for its efficacy in the treatment of dysphagia. While some of the studies reported positive outcomes about NMES, some indicated either negative results or no effects at all [52,53,54].
In their meta-analysis examining the studies available in the literature until December 2021, Don et al. (2022) found that adding NMES to the therapy process is superior to following conventional swallowing therapy alone regardless of the time elapsed after stroke, the number of sessions, and the outcome criteria [20]. Park et al. (2016) report that effortful swallowing exercise is effective in the treatment of post-stroke dysphagia, but this exercise is more effective when combined with NMES [55].
When the NMES modality and conventional swallowing exercises are applied together, both Type-1 and Type-2 muscle fibers are activated simultaneously [9]. In addition, NMES, as opposed to using exercises alone, leads to more and frequent swallows during the treatment session by increasing the strength and speed of the contraction of the pharyngeal muscles [9, 57]. Repetitive swallowing is considered effective for dysphagia treatment [54]. In the same vein, repetitive and task-specific movements facilitate the neural plasticity and motor recovery [33].
In the current study, NMES was applied for 40 min in addition to conventional dysphagia therapy. Analysis of pre- and post-treatment results across all parameters for the group receiving NMES and CDT has pointed to statistically significant differences. When the NMES group was compared with the one receiving only conventional dysphagia therapy, the results have shown that application of NMES and CDT in combination promoted better improvement as opposed to using only CDT. The differences between these groups across the GUSS, FOIS, and DSRS parameters were statistically significant in favor of the NMES group. Regarding the PAS scores at IDDSI Level-4 and Level-0 consistencies, the change was better for the NMES group, yet the difference was not significant. In line with the relevant body of research, the results of the current study also underline that conventional dysphagia therapy applied in combination with NMES is more effective than administering conventional dysphagia therapy in isolation.
The neuromodulator treatment techniques that help the brain re-organize its neural connections are known to facilitate the rehabilitation of disordered swallowing function [7]. These techniques include both central stimulation methods such as TMS or tDCS and peripheral methods such as NMES [7]. While NMES stimulates the peripheral sensory system, the methods such as tDCS and TMS support rehabilitation by stimulating the central system. Recent studies have concluded that central and peripheral treatments can modify the excitability of the motor representations of the swallowing muscles both on their own and in combination with other treatment modalities [7].
This study also examined the effectiveness of tDCS in the treatment of post-stroke swallowing disorders. One of the cortical stimulation methods, tDCS provides a non-invasive brain stimulation to the cerebral cortex by sending weak direct electric current via the electrodes placed on the target cortical region over the skull to modulate the brain functions for the cortical excitability and neuroplasticity [56].
Studies have shown that tDCS leads to improvement in the motor functions of patients with chronic stroke [25, 58]. Recent studies on healthy human subjects have reported that anodal tDCS applied to the pharyngeal motor cortex increases its excitability and provides support for the rehabilitation of patients with dysphagia [27]. Kumar et al. (2011) revealed that the swallowing function of patients with post-stroke dysphagia significantly improved after applying 2 mA anodal tDCS for 30 min to the non-involved hemisphere for five consecutive days [59]. Suntrup-Kruger et al. (2017) reported a significant gain in swallowing function for patients with brain injury compared to the sham-stimulated group after applying 1 mA anodal stimulation for 20 min to the pharyngeal motor cortex in the non-involved hemisphere for four consecutive days [60]. In their meta-analysis examining the studies published until 2021, He et al. (2022) reported a positive effect of tDCS on post-stroke dysphagia regardless of the time elapsed after stroke, the type of stimulation, the stimulation dose, and the preference for the hemisphere to which tDCS would be applied [61].
In this study, 2 mA anodal tDCS was applied for 20 min to the unaffected hemisphere pharyngeal motor cortex area for ten sessions. The findings could not be fully compared with the results of previous studies due to the heterogeneity of the modalities employed in those studies. However, when the group presented with conventional dysphagia therapy with unilateral anodal tDCS was compared to the group that received only conventional dysphagia therapy and sham tDCS, the post-treatment change was found numerically higher in the tDCS group, yet there was a significant difference only in the DSRS parameter between the two groups, and no statistically significant difference was found for the other parameters.
The literature suggests that NMES, which stimulates the muscle fibers and increases the muscle contractions by activating the peripheral sensory system with non-invasive brain stimulation technique, and TMS & tDCS, which modulate the cortical neurons magnetically or electrically, are very effective therapies for the treatment of post-stroke dysphagia in the acute and subacute period. Ching-Fang et al. (2018), in their meta-analysis study, examined non-invasive treatment modalities used for post-stroke dysphagia and reported that TMS, tDCS, and NMES were the most effective treatments. They also stated that NMES was more effective than tDCS treatment, but the difference was not statistically significant [32].
In this study, statistically significant changes were identified in many parameters following the comparison between the group receiving NMES and the one receiving only conventional dysphagia therapy. Yet, there was a statistically significant difference in only one parameter between the group receiving tDCS and the one provided with only conventional dysphagia therapy, which could be explained by the physiological effect of the instrumental treatments.
NMES treatment aims to eliminate the weakness in the muscles that function during swallowing, to stimulate the swallowing center in the brain through the neural networks, and to ensure the re-organization of swallowing. In this context, NMES stimulates the structures in which the movement is initiated and terminated. However, tDCS is a procedure that influences the cortical excitability and neuroplasticity by stimulating the cerebral cortex. In this sense, tDCS, unlike NMES, only stimulates the structure that initiates the act of swallowing and has no effect on the muscles that function during swallowing. Although the results of the current study revealed no clear superiority, the improvement in the NMES group was greater than in the tDCS group. This can be attributed to the fact that there was no statistically significant difference between the two groups, but there was a difference between them when compared in terms of using conventional dysphagia therapy additionally.
Several studies in the literature separately compare non-invasive brain stimulation techniques and NMES with conventional dysphagia therapy. However, there is a dearth of research in which peripheral and central treatment methods are employed together for the treatment of dysphagia. Similar to the current study, Zhang et al. (2018) employed non-invasive brain stimulation techniques, rTMS and NMES, in combination for the treatment of dysphagia, and reported that the combination was more effective than either NMES or rTMS as a standalone procedure in the treatment of post-stroke dysphagia [34]. The current study has concluded that the group receiving all three treatment modalities in combination achieved more effective results than both NMES and tDCS groups. The comparison of the outcomes of the group in which three procedures were administered in combination with those of the one in which tDCS was applied with CDT has yielded statistically significant differences across the GUSS, FOIS, and DSRS parameters. In the same vein, a similar comparison with the group in which NMES was presented with CDT has pointed to higher scores across all parameters in favor of the group receiving all three modalities, yet the difference is not statistically significant. Cross-comparison of groups within the scope of this study has shown that the greatest difference has been recorded for the subjects treated with the three modalities (tCDS + NMES + CDT). Those groups treated with the addition of either NMES or tDCS achieved the second and third better results, respectively, whereas the gains for the group in which only conventional dysphagia therapy was administered were the least. The analysis of pre- and post-treatment average PAS scores at IDDSI Level-4 consistencies has indicated that the difference was of statistical significance. Improvement was also recorded for the other groups, but pre-and post-treatment results were not significantly different. During the pre-treatment assessment, penetration and aspiration were not experienced much by the subjects at IDDSI Level-4 consistencies, and thus, the difference between pre-and post-treatment scores was not large, which can account for the lack of a statistically significant difference in favor of post-treatment scores. However, pre- and post-treatment scores for the GUSS, FOIS, DSRS, and IDDSI Level-0 consistencies across all groups were significantly different. The treatment gains achieved by the group in which three therapy modalities (tCDS + NMES + CDT) were administered in combination are better across all parameters, and it is the only group that achieved a statistically significant difference at IDDSI Level-4 consistencies. The reason why the group receiving all three therapy procedures made the greatest progress can be attributed to the integrated use of both peripheral and central stimulation methods as opposed to applying only CDT or CDT supported with one of the assistive modalities, which provides support for the hypothesis of this study. In conclusion, the results suggest that employing all three therapy methods in combination stands as the most effective treatment alternative for post-stroke dysphagia.
Limitations
There are studies in the literature showing that the effect of tDCS is directly proportional to the time elapsed after treatment [62, 63]. One of the limitations of this study is the lack of an evaluation of the long-term effects together with immediate effects, especially for the tDCS group. Future studies regarding the treatment of post-stroke swallowing disorders are advised to perform a re-evaluation for the long-term effects together with immediate effects following the tDCS therapy.
In studies evaluating therapies, the severity of the problem is acknowledged as a valid sign of the effectiveness of that therapy. During the planning stage of this research, the patients with swallowing disorders were included, but an inclusion criterion regarding the severity of the swallowing disorder was not predetermined. Therefore, another limitation of the study is the lack of predetermined inclusion criterion for the severity of the swallowing disorder. However, by the end of the research process, it was clear that all the subjects had moderate-to-severe swallowing disorders, and their distribution was homogeneous across the groups. This limitation bears no negative influence over the research results.
The number of participants in the therapy groups is another limitation of the study. The superiority of the therapy groups over each other can be demonstrated more clearly by conducting studies with more subjects.
The patients in the acute stage were included in this study to determine the effectiveness of therapy modalities in the treatment of post-stroke swallowing disorders. However, there is a spontaneous recovery effect in the acute period after stroke. Therefore, it is recommended to conduct a similar study during subacute and chronic periods to eliminate the effect of natural recovery, which will add precision to the efficacy of the procedure.
Conclusion
Early rehabilitation is essential in the treatment of swallowing disorders after acute stroke. Delaying the rehabilitation process in the first month of rapid recovery may have negative long-term effects. One of the strongest aspects of the study is selecting all cases in the acute period for active rehabilitation. In addition, administering both real and/or sham instrumental treatments to all groups is another strength of the study. Besides, this is the first-ever research effort where two non-invasive brain stimulation techniques, tDCS and NMES, were applied together for dysphagia treatment.
Research results indicate that the importance of CDT in the treatment of swallowing disorders cannot still be denied. However, when the group receiving only conventional dysphagia therapy was compared with the other groups, those assisted with instrumental treatment procedures showed greater improvement. This indicates that swallowing therapy combined with instrumental treatments such as NMES and tDCS is superior to conventional swallowing therapy alone.
The results revealed that assisting conventional swallowing therapy with instrumental treatments such as NMES and tDCS in the treatment of post-stroke swallowing disorders increases efficiency. The effectiveness of NMES therapy, frequently used in stroke-related dysphagia treatments, is a widely accepted fact. Apart from that, among the central stimulation methods, tDCS is considered an effective option in the treatment of post-stroke swallowing disorders in the acute period due to its cost-effectiveness and ease of use. Combining instrumental procedures with conventional dysphagia therapy is more effective than conventional therapy alone, but it is difficult to make a firm judgment about the superiority of peripheral or central stimulation in the treatment. Therefore, combining conventional dysphagia therapy with one of the peripheral or central stimulation techniques provides an advantage in swallowing rehabilitation. Supporting conventional dysphagia therapy with instrumental stimulation modalities in clinical settings can accelerate the recovery of swallowing function and has the potential to provide advantages in terms of time and cost.
In conclusion, the results showed that therapies were effective in each group. The use of instrumental treatments such as NMES and tDCS increased the efficiency of the treatment and provided a more significant improvement. As a result of the study, it is reasonable to conclude that the most effective treatment group is the one in which CDT, NMES, and tDCS were used in combination.
References
Meng NH, Wang TG, Lien NI. Dysphagia in patients with brainstem stroke. AM J Phys Med Rehabil. 2000;79:170–5.
Warlow CP, Dennis MS. Stroke: a practical guide to management. Oxford: Blackwell Science Ltd; 2001.
Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis Sep-Oct. 2000;10(5):380–6.
Carnaby-Mann GD. Examining the evidence on neuromuscular electrical stimulation for swallowing. Arch Otolaryngol Head Neck Surg. 2007;133:564–71.
Tan Jackson C (2005) Practical Manual of Physical Medicine and Rehabilitation: Diagnostics, Therapeutics, and Basic Problems Mosby; 2nd edition
Logemann JA. Anatomy And Physiology Of Normal Deglutition Evaluation And Treatment Of Swallowing Disorders. Austin: Pro-ed; 1998. p. 13–52.
Doeltgen SH. Huckabee M-L (2012) Swallowing neurorehabilitation: from the research laboratory to routine clinical application. Arch Phys Med Rehab. 2012;93:207–13. https://doi.org/10.1016/j.apmr.2011.08.030).
Pape, K. E., & Chipman, M. L. (2005) Electrotherapy in rehabilitation. In: J. A. Lisa, B. M. Gans, and Walsh, N. E. (Eds.), Physical medicine and rehabilitation: Principles and practice (4th ed). Philadelphia, PA: Lippincott, Williams, & Wilkins
Wijting, Y., Freed, M. (2013) Training Manual for the use of Neuromuscular Electrical Stimulation in the treatment of Dysphagia, VitalStim Certification Program, Provided by CIAO Seminars, 8–79.
Scutt P, Lee HS, Hamdy S, Bath PM. (2015) Pharyngeal electrical stimulation for treatment of poststroke dysphagia: individual patient data meta-analysis of randomized controlled trials. Stroke Res Treat. 2015;2015:429053.
Poorjavad M, Moghadam ST, Ansari NN, Daemi M. Surface electrical stimulation for treating swallowing disorders after stroke: a review of the stimulation intensity levels and the electrode placement. Stroke Res Treat. 2014. https://doi.org/10.1155/2014/918057.
Hamdy S, Rothwell JC, Aziz Q, Thompson DG. (2000) Organization and re-organization of human swallowing motor cortex: implications for recovery after stroke. Clin Sci. 2000;99(2):151–7.
Shaw GY, Sechtem PR, Searl J, Keller K, Rawi TA, Dowdy E. (2007) Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann Otol Rhinol Laryngol. 2007;116(1):36–44.
Stal P. Characterization of human oro-facial and masticatory muscles with respect to fibers types, myosins, and capillaries. Morphological, enzyme-histochemical, immune-histochemical, and biochemical investigations. Swed Dent J Suppl. 1994;98:1–55.
Shune S, Moon JB. (2012) Neuromuscular electrical stimulation in dysphagia management: clinician use and perceived barriers. Contemporary Issues in Communication Science and Disorders. 2012;39:55–68.
Carnaby-Mann GD, Crary MA. (2007) Examining the evidence on neuromuscular electrical stimulation for swallowing: a meta-analysis. Arch Otolaryngol Head Neck Surg. 2007;133(6):564–71.
Ryu JS, Kang JY, Park JY, Nam SY, Choi SH, Roh JL, et al. (2009) The effect of electrical stimulation therapy on dysphagia following treatment for head and neck cancer. Oral Oncol. 2009;45:665–8.
Yi-Wen C, Chang KH, Chen HC, Liang WM, Wang YH, Lin YN. The effects of surface neuromuscular electrical stimulation on post-stroke dysphagia: a systemic review and meta-analysis. Clin Rehab. 2016;30(1):24–35. https://doi.org/10.1177/0269215515571681.
Sun Y, Chen X, Qiao J, Song G, Xu Y, Zhang Y, Xu D, Gao W, Li Y, Xu C. (2020) Effects of transcutaneous neuromuscular electrical stimulation on swallowing disorders: a systematic review and meta-analysis. Am J Phys Med Rehab. 2020;99:701–11.
Doan TD, Ho WC, Wang LH, Chang FC, Quyn Tran TT, Chou LW. Therapeutic Effect and optimal electrode placement of transcutaneous neuromuscular electrical stimulation in patients with post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials journal. Life. 2022;2022(12):875. https://doi.org/10.3390/life12060875.
Hamdy S, Aziz Q, Rothwell JC, Power M, Singh KD, Nicholson DA, et al. Recovery of swallowing after dysphagic stroke relates to functional re-organization in the intact motor cortex. Gastroenterology. 1998;115(5):1104–12.
Hamdy S, Rothwell JC, Aziz Q, Singh KD, Thompson DG. Long-term re-organization of the human motor cortex driven by short-term sensory stimulation. Nat Neurosci. 1998;1(1):64–8.
Simons A, Hamdy S. The use of brain stimulation in dysphagia management. Dysphagia. 2017;32(2):209–15. https://doi.org/10.1007/s00455-017-9789-z.
Nitsche MA, Paulus W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology. 2001;5:1899–9101.
Hummel F, Celnik P, Giraux P, Floel A, Wu WH, Gerloff C, et al. Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke. Brain. 2005;128(pt3):490–9.
Schlaug G, Renga V, ve Nair D.,. Transcranial direct current stimulation in stroke recovery. Arch Neurol. 2008;65:1571–6.
Jefferson S, Mistry S, Singh S, Rothwell J, Hamdy S. Characterizing the application of transcranial direct current stimulation in the human pharyngeal motor cortex. Am J Physiol Gastrointest Liver Physiol. 2009;297:G1035-40.
Pedretti LW (1996) Cerebrovascular Accident. In: Occupational therapy, Practice Skills for Physical Dysfunction. 4th ed. Ed, Pedretti LW. Mosby Comp., pp: 785- 805
Dombovy ML, Sandok BA, Basford JR. rehabilitation for stroke: a review. Stroke. 1986;17:363–9.
Wang T, DongL CongX, LuoH LiW, Meng P, et al. Comparative efficacy of non-invasive neurostimulation therapies for poststroke dysphagia: a systematic review and meta-analysis. Neurophysiol Clin. 2021;51(6):493–506.
Cheng I, Sasegbon A, Hamdy S. (2020) Effects of neurostimulation on poststroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2020;24(8):1388–401.
Chiang C-F, Lin M-T, Ming-Yen Hsiao MD, Yeh Y-C, Liang Y-C, Tyng-GueyWang,. Comparative efficacy of noninvasive neurostimulation therapies for acute and subacute PosCDTroke dysphagia: a systematic review and network meta-analysis. Arch Phys Med Rehab. 2018. https://doi.org/10.1016/j.apmr.2018.09.117.
Takeuchi N, Izumi S. Rehabilitation with post-stroke motor recovery: a review with a focus on neural plasticity. Stroke Res Treat. 2013. https://doi.org/10.1155/2013/128641.
Zhang M, Tao T, Zhang BZ, Zhu X, Fan WG, Pu LJ, Chu L, Yue SW. Effectiveness of neuromuscular electrical stimulation on patients with dysphagia with medullary infarction. Arch Phys Med Rehab. 2016;97(3):355–62. https://doi.org/10.1177/0300060518807340.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20.
Belafsky PC, Kuhn MA. The Clinician’s Guide to Swallowing Fluoroscopy. New York: Springer; 2014. https://doi.org/10.1007/978-1-4939-1109-7.
Trapl M, Enderle P, Nowotny M, Teuschl Y, Matz K, Dachenhausen A, Brainin M. Dysphagia bedside screening for acute-stroke patients: the gugging swallowing screen. Stroke. 2007;38(11):2948–52. https://doi.org/10.1161/STROKEAHA.107.483933.
Warnecke T, Im S, Kaiser C, Hamacher C, Oelenberg S, Dziewas R. Aspiration and dysphagia screening in acute stroke - the gugging swallowing screen revisited. Eur J Neurol. 2017;24(4):594–601. https://doi.org/10.1111/ene.13251.
Rugiu M. Role of videofluoroscopy in the evaluation of neurologic dysphagia. Acta Otorhinolaryngol Ital. 2007;27(6):306.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Waxman MJ, Durfee D, Moore M. Nutritional aspects and swallowing function of patients with Parkinson’s disease. Nutr Clin Prat. 1990;5:196–9.
Carnaby G, Hankey GJ, Pizzi J. Behavioural intervention for dysphagia in acute stroke: a randomized controlled trial. Lancet Neurol. 2006;5:31–7.
DePippo K, Holas M, Reding M, Mandel F, Lesser M. Dysphagia therapy following stroke A controlled trial. Neurology. 1994;44:1655.
de Lama LG, Lazarus C, Logemann JA. Impact of thermal stimulation on the triggering of the swallowing re ex. Dysphagia. 1986;1:73–7.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Amer Geriatr Soc. 2005;53:1483–9.
Daniels SK, Foundas AL. Lesion localization in acute stroke patients with risk of aspiration. J Neuroimaging. 1999;9(2):91–8.
Riecker A, Gastl R, Kühnlein P, Kassubek J, Prosiegel M. Dysphagia due to unilateral infarction in the vascular territory of the anterior insula. Dysphagia. 2009;24:114–8.
Langmore SE, Pisegna JM. Efficacy of exercises to rehabilitate dysphagia: a critique of the literature. Int J Speech Lang Pathol. 2015;17(3):222–9. https://doi.org/10.3109/17549507.2015.1024171.
Robbins J, Butler SG, Daniels SK, Gross RD, Langmore S, Lazarus CL, Martinn-Harris B, McCabe D, Musson N, Rosenbek JC. Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. J Speech Lang Hear Res. 2008;51:S276-300.
Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51:S225-39.
Beyon H. (2016) Effect of the Masako maneuver and neuromuscular electrical stimulation on the improvement of swallowing function in patients with dysphagia caused by stroke. J Phys Ther Sci. 2016;28:2069–71.
Blumenfeld L, Hahn Y, Lepage A, Leonard R, Belafsky PC. Transcutaneous electrical stimulation versus traditional dysphagia therapy: a nonconcurrent cohort study. Otolaryngol Head Neck Surg. 2006;135:754–7.
Suiter DM, Leder SB, Ruark JL. Effects of neuromuscular electrical stimulation on submental muscle activity. Dysphagia. 2006;21:56–60.
Lim KB, Lee HJ, Lim SS. Choi YI (2009) Neuromuscular electrical and thermal-tactile stimulation for dysphagia caused by stroke: a randomized controlled trial. J Rehabil Med. 2009;41(3):174–8. https://doi.org/10.2340/16501977-0317.
Park JS, Oh DH, Hwang NK, Lee JH. (2016) Effects of neuromuscular electrical stimulation combined with effortful swallowing on post-stroke oropharyngeal dysphagia: a randomized controlled trial. J Oral Rehabil. 2016;43:426–34.
Boes AD, Kelly MS, Trapp NT, Stern AP, Press DZ, Pascual-Leone A. Noninvasive brain stimulation: challenges and opportunities for a new clinical specialty. J Neuropsychiatry Clin Neurosci. 2018;30(3):173–9.
Wakabayashi H, Matsushima M, Momosaki R. The effects of resistance training of swallowing muscles on dysphagia in older people: a cluster, randomized, controlled trial. Nutrition. 2018;48:111–6.
Schlaug G, Renga V, Nair D. Transcranial direct current stimulation in stroke recovery. Arch Neurol. 2008;65:1571–6. https://doi.org/10.1001/archneur.65.12.1571.
Kumar S, Wagner CW, Frayne C, Zhu L, Selim M, Feng W, et al. Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke. 2011;42(4):1035–40. https://doi.org/10.1161/STROKEAHA.110.602128.
Suntrup-Kruger S, Ringmaier C, Muhle P, Wollbrink A, Kemmling A, Honning U, Claus I, Warnecke T, Teismann I, Pantev C. Randomized trial of transcranial DC stimulation for post-stroke dysphagia. Ann Neurol. 2017. https://doi.org/10.1002/ana.25151.
He K, Wu L, Huang Y, Chen Q, Qiu B, Liang K, Ma R. Efficacy and safety of transcranial direct current stimulation on post-stroke dysphagia: a systematic review and meta-analysis. J Clin Med. 2022;11(9):2297. https://doi.org/10.3390/jcm11092297.
Yang EJ, Baek SR, Shin J, Lim JY, Jang HJ, Kim YK, et al. Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci. 2012;30(4):303–11. https://doi.org/10.3233/RNN-2012-110213.
Cheng I, Sasegbon A, Hamdy S. Effects of neurostimulation on PosCDTroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2021;24(8):1388–401. https://doi.org/10.1111/ner.13327.
Author information
Authors and Affiliations
Contributions
This study was designed by SB and YK. YK acted as a consultant and monitored the research process. Data collection, analysis, and interpretation were completed by SB who also drafted the article. YK and ND critically read the article and helped revise it for the final draft. The final version of the article was approved by all the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest concerning this research.
Ethical Approval
All procedures performed in studies involving human participants met the ethical standards of the institutional research committee (IRC:99102440/2020–04) and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all the individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bengisu, S., Demir, N. & Krespi, Y. Effectiveness of Conventional Dysphagia Therapy (CDT), Neuromuscular Electrical Stimulation (NMES), and Transcranial Direct Current Stimulation (tDCS) in Acute Post-Stroke Dysphagia: A Comparative Evaluation. Dysphagia 39, 77–91 (2024). https://doi.org/10.1007/s00455-023-10595-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10595-w