Abstract
Aspiration pneumonia is a potentially preventable, aggressive type of pneumonia. Little is understood on the burden in mortality from aspiration pneumonia. Our objectives were to first examine the burden of mortality from aspiration pneumonia in the United States and second investigate comorbidities associated with aspiration pneumonia to understand risk factors. We conducted a case–control study of individuals who died of aspiration pneumonia matched to those who died of other causes. We analyzed all deaths in the United States using the Multiple Cause of Death Dataset from 1999 to 2017. Cases were matched with controls based on age, sex, and race. We calculated age-adjusted mortality rates, annual percentage changes in aspiration pneumonia mortality, and matched odds ratio comparisons. We identified a total of 1,112,944 deaths related to aspiration pneumonia from 1999 to 2017 or an average of 58,576 per year (age-adjusted mortality rate, 21.85 per 100,000 population; 95% confidence interval (CI) 21.78–21.92). Aspiration pneumonia was reported as the underlying cause of death in 334,712 deaths or an average of 17,616 deaths per year (30.1% of the total aspiration pneumonia-associated deaths). Individuals 75 years old or older accounted for 76.0% of aspiration pneumonia deaths and the age adjusted rate ratio was 161.0 (CI 160.5–161.5). Neurologic, upper gastrointestinal, and pulmonary conditions as well as conditions associated with sedative substances were more often associated with aspiration pneumonia-associated deaths. Aspiration pneumonia is the underlying cause or a cofactor in tens of thousands of deaths each year in the United States. Aspiration pneumonia-associated deaths are highly prevalent with advanced age and are associated with neurologic, upper gastrointestinal and pulmonary conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aspiration pneumonia is a subclass of pneumonia brought on by inhalation of oropharyngeal or gastric secretions [1]. Comorbidities that predispose to clinically recognized aspiration pneumonia include processes that impair consciousness, cause swallowing dysfunction, or impair pulmonary clearance [2]. Diagnosis of aspiration pneumonia typically occurs following macro aspiration with involvement of characteristic anatomic locations. Aspiration pneumonia is associated with a higher mortality rate than non-aspiration pneumonia [3].
Relatively little is known about how aspiration pneumonia contributes to national mortality or how the mortality from aspiration pneumonia has changed over time in response to efforts to identify and treat dysphagia or the rise in palliative care. The Center for Disease Control and Prevention annually reports mortality from pneumonia, and in 2019 it found that pneumonia was the underlying cause for 43,881 deaths making it the eighth leading cause of death [4]. However, these figures consider all types of pneumonia. Mortality from aspiration pneumonia is not separately reported. Furthermore, aspiration pneumonia may frequently be a contributing factor to mortality but may not be reported as the underlying cause, which indicates the disease or injury which initiated the chain of events leading directly to death. The extent to which aspiration pneumonia contributes to other mortality is unknown.
In terms of previous research, most studies on aspiration pneumonia focus on incidence rates and microbiology of the infection. There are currently no other studies that analyze deaths due to aspiration pneumonia using national databases. There are several studies that analyze mortality of specific cohorts, such as Feng et al.s’ study on mortality due to aspiration pneumonia among stroke patients in Taiwan with dysphagia [5]. However, none of these studies report mortality using the volume of data from national death record databases in the manner that this study does.
We set out to examine the extent to which aspiration pneumonia contributes as a cause of death to mortality in the United States and to describe groups in which aspiration pneumonia mortality are highest. Our goals were to (1) describe the incidence of mortality due to aspiration pneumonia (2) investigate trends in deaths due to aspiration pneumonia (3) examine comorbidities associated with deaths due to aspiration pneumonia.
Methods
Data Source
We used Multiple Cause of Death data from the Center for Disease Control and Prevention (CDC) from 1999 to 2017. Briefly, this dataset includes data on all death certificates that occur within the United States. Death certificates are required by law to specify the underlying cause of death and up to 19 contributing causes of death [6]. Death certificates are compiled by vital statistics offices in each state and sent to the CDC. Multiple Cause of Death data are de-identified and publicly available. The Wayne State University Institutional Review Board determined this study was exempt from review.
Study Population and Variables
We identified individuals with aspiration pneumonia listed as the underlying cause or a contributing cause of death on their death certificate (ICD-10 J69.0). We define aspiration pneumonia-associated death as any death in which aspiration pneumonia was listed as the underlying cause or a contributing cause of death. We secondarily examined deaths in which aspiration pneumonia was listed as the underlying cause of death. We additionally examined the year, location where deaths occurred, and other causes of death. We defined deaths in the hospital as deaths that occurred inpatient, outpatient, or patients that arrived dead on arrival to the hospital.
Statistical Analysis
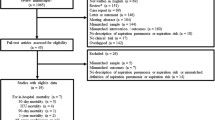
We matched cases that died of aspiration pneumonia 1:1 with controls that died of other causes based on age, sex, and race using random sampling without replacement. We compared the characteristics of individuals with aspiration pneumonia-associated death to controls. We examined comorbid risk factors including cancer, neurological conditions, conditions that impair consciousness, psychiatric conditions, and motility disorders that have been previously established to be associated with clinical aspiration pneumonia [2].
We calculated aspiration pneumonia-associated mortality ratios for each age, sex and racial/ethnic group using size and demographic data from the U.S. Census. We calculated changes in the incidence of mortality from aspiration pneumonia using version 4.9.0.0 of the Joinpoint Regression Analysis software from the National Cancer Institute [7]. Matched odds ratios were calculated by comparing the relative burden of associated comorbidities in cases and controls [8]. We performed all analysis using SPSS, version 27 [9].
Results
Burden of Aspiration Pneumonia-Associated Deaths
After analysis, we identified a total of 1,112,944 aspiration pneumonia-associated deaths from 1999 to 2017 or an average of 58,576 per year. The age-adjusted mortality rate was 21.9 per 100,000 population (95% confidence interval (CI) 21.8–21.9). There was a total of 47,728,569 deaths in the United States from 1999 to 2017, making aspiration pneumonia-associated deaths 2.3% of all deaths occurring in this time period. The majority of aspiration pneumonia-related deaths occurred in males (53.8%, Table 1). After adjusting for age, males had an odds ratio (OR) of 1.21 (CI 1.21–1.21) compared to females. In terms of race, Black (OR 0.61, CI 0.60–0.62) and Asian/Native American/Pacific Islander/Other (OR 0.18, CI 0.18–0.19) groups had lower aspiration pneumonia-associated mortality than White individuals (Table 2). Mortality rates increased with age with a crude mortality rate of 643.84 per 100,000 (CI 642.30–645.39) in individuals 85 years of age of older.
Aspiration pneumonia was the underlying cause of death in 334,712 deaths or an average of 17,616 deaths per year (30.1% of the total aspiration pneumonia-associated deaths). For deaths in which aspiration pneumonia was listed as a contributing factor but not the underlying cause, the top few underlying causes were cardiovascular disease (22.8%), dementia/Alzheimer’s (15.4%), and neoplasms (6.1%) (Table 3). Most (58.0%) aspiration pneumonia-related deaths occurred in the hospital (Table 4).
Trend in Aspiration Pneumonia Deaths Over Time
Aspiration pneumonia-associated deaths increased from 1999 to 2002 with an annual percentage change (APC) of 0.7 (CI − 1.9 to 3.4). From 2002 to 2009 deaths decreased with an APC of − 1.9 (CI − 2.8 to − 1.1), and from 2009 to 2017, deaths increased with an APC of 1.3 (CI 0.7 to 1.9) (Fig. 1A). Deaths with aspiration pneumonia listed as the underlying cause behaved similarly (Fig. 1B). From 1999 to 2001 they increased with an APC of 5.7 (CI 0.6 to 11.1). From 2001 to 2009 they decreased with an APC of − 1.6 (CI − 2.2 to − 0.9). Then from 2009 to 2017, they increased steadily with an APC of 1.8 (CI 1.3 to 2.3).
a Crude rate per 100,000 people of aspiration pneumonia-related deaths from 1999 to 2017. *Indicates that the Annual Percentage Change (APC) is significantly different from zero at the alpha = 0.05 level. b Crude rate per 100,000 people of deaths with aspiration pneumonia listed as the underlying cause from 1999 to 2017. *Indicates that the Annual Percentage Change (APC) is significantly different from zero at the alpha = 0.05 level
The locations of aspiration pneumonia-associated deaths shifted over time with increases in deaths in hospice or at home (Fig. 2). Deaths in hospice increased with an annual average percentage change (AAPC) of 36.5 (CI 29.9 to 43.4). Deaths in decedents’ homes increased with an AAPC of 3.2 (CI 2.8 to 3.7). In contrast deaths in nursing homes and long-term care decreased with an AAPC of − 2.8 (CI − 3.5 to − 2.1) and deaths in the hospital remained the same with an AAPC of − 0.1 (CI − 0.6 to 0.5).
Associated Causes of Death
Comorbid conditions that were associated with death from aspiration pneumonia included esophageal cancer, cerebrovascular disease, Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, Cerebral Palsy, hemiplegia, paraplegia, major depressive disorder, schizophrenia, sleep disorders, opioid related disorders, GERD, esophageal obstruction, esophageal diverticulum, dysphagia, chronic bronchitis, and Barrett’s esophagus (Table 5). We did not find that malignant conditions other than esophageal cancer were associated with aspiration pneumonia-associated death.
Discussion
Our data suggest that the burden of aspiration pneumonia may be greater than is generally appreciated. We found that aspiration pneumonia contributes to an average of over 58,000 deaths per year in the United States. One reason why the burden of mortality may be underappreciated is that aspiration pneumonia frequently occurs as a consequence of another condition and is listed as the underlying cause of death in only 17,616 deaths per year. Underlying cause of death is defined by the World Health Organization as “the disease or injury which initiated the train of events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury.” [10]. Nonetheless, aspiration pneumonia is a significant event and may precipitate a cascade of complications ultimately leading to death, particularly in the elderly. Efforts to prevent aspiration have the potential to help those in which aspiration pneumonia was found to be the underlying cause and those in which aspiration was found to be a contributing factor.
Trend in Aspiration Pneumonia Deaths Over Time
We found that mortality from aspiration pneumonia decreased from 1999 to 2009 but then subsequently reversed course. The reasons for the increasing trend in aspiration pneumonia-associated deaths since 2009 are likely multifactorial and only partially discernable from our data. Previous research from the American Lung Association has found that the death rate from pneumonia and influenza has declined 3.8% per year from 1999 to 2013 [11]. Changing attitudes towards comfort care, defined as care meant to relieve suffering at the end of life may account for some of this trend as we observed an increase in aspiration pneumonia deaths that occurred in hospice [12]. Advanced directives regarding comfort care gained wider acceptance since 2000, and studies have shown that patients with advanced directives are less likely to receive life-sustaining treatments or die in a hospital [12, 13].
Associated Causes of Death
Previous studies have identified a robust relationship between conditions that result in swallowing dysfunction, severely impair consciousness or impair the ability to clear secretions [1, 12, 14]. However, previous research has not explored the relationship between various comorbidities and mortality from aspiration pneumonia. We found a robust and highly significant association with these conditions and mortality from aspiration pneumonia. The relationship between some conditions such as GERD, major depressive disorder, and schizophrenia with aspiration pneumonia is less well established [15]. Medical treatment of GERD with proton pump inhibitors (PPIs) and histamine receptor-2 antagonists has been reported to increase the risk of pneumonia related to aspiration of reflux contents [16]. These medications may contribute to the development of aspiration pneumonia through decreasing gastric acid, thereby reducing natural defenses against bacteria colonization [15]. In our dataset, we observed that GERD was associated with 4.5 odds of death related to aspiration pneumonia. Anti-depressant and anti-psychotic medications have also been associated with clinical aspiration pneumonia [2] and in our dataset major depressive disorder and schizophrenia were associated with a modest 1.46 and 1.62 odds of death related to aspiration pneumonia respectively.
In contrast with previous research, we did not observe an association between brain, head and neck or gastric cancer and mortality from aspiration pneumonia. Numerous studies have reported brain, head and neck, and gastric cancer to be associated with aspiration [1, 2, 14]. Specifically, a retrospective study reported that aspiration pneumonia was the cause of death in 51 out of 85 head and neck cancer patients over 12 years [17]. However, this was not the case in our results. We believe this may reflect an artifact of death certificate reporting of individuals with cancer. In death certificates of individuals with cancer, contributing factors leading to death such as aspiration pneumonia may be less likely to be reported. Indeed, cancers with the highest reported risk of aspiration (head and neck cancer, esophageal cancer and brain cancer) [2, 17], had the greatest association with aspiration pneumonia-associated mortality compared with other cancers.
Limitations
There are several limitations to consider when interpreting our data. First, our dataset was limited to information reported on death certificates. Thus, we were not able to examine health behaviors such as smoking. Second, aspiration pneumonia can be challenging to distinguish from other pneumonias leading to potential errors in reporting. For instance, in our control group we included deaths due to other pneumonias. It is possible that some of these pneumonias were secondary to aspiration but were not recorded as such. While it may appear that this could alter the results of our comparison between comorbidities of the cases and controls, it is unlikely given that out of 1,112,944 controls, only 11,854 (1.07%) were recorded as “pneumonia” (ICD10 codes J12-J18). Thus, the impact on our results, if any, is likely minimal. However, it must be acknowledged that given the retrospective nature of this study, it is not possible to ascertain the accuracy of every diagnosis of aspiration pneumonia. Nonetheless, we feel that these robust national data on cause of death from the last 20 years provide a unique perspective on mortality from aspiration pneumonia in the United States.
Implications
Aspiration pneumonia is a significant contributor to mortality in the United States both as a contributing factor and the underlying cause of death. While not all mortality from aspiration pneumonia is preventable, many deaths could potentially be avoided with speech therapy and dietary modification in at risk populations [18,19,20]. Early recognition of individuals with dysphagia at risk of aspiration is critical. Though it is challenging to identify patients at risk of silent aspiration, completing procedures such as the modified barium swallow study (MBSS) and fiberoptic endoscopic evaluation of swallowing (FEES) as a standard of care in high-risk patients would greatly accelerate prevention efforts. Our data provide a profile of the age groups and comorbidities most associated with aspiration pneumonia to help guide these efforts.
Conclusion
While a robust literature describes the burden of clinically diagnosed aspiration pneumonia [2, 14, 21], little previous research has focused on the burden of aspiration pneumonia-associated mortality. We believe the burden of morality from aspiration pneumonia may be underappreciated. We observed that aspiration pneumonia contributes to over 57,000 deaths each year in the United States. Multidisciplinary efforts to identify patients at risk of aspiration and prevent subsequent aspiration pneumonia have a substantial opportunity to save lives.
References
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med United States. 2001;344:665–71.
Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med United States. 2019;380:651–63.
Rodriguez AE, Restrepo MI. New perspectives in aspiration community acquired pneumonia. Expert Rev Clin Pharmacol England. 2019;12:991–1002.
Centers for Disease Control and Prevention. FastStats: pneumonia [Internet]. National Center for Health Statistics. 2021 [cited 2021 Mar 26]. Available from: https://www.cdc.gov/nchs/fastats/pneumonia.htm.
Feng M-C, Lin Y-C, Chang Y-H, Chen C-H, Chiang H-C, Huang L-C, et al. The mortality and the risk of aspiration pneumonia related with dysphagia in stroke patients. J Stroke Cerebrovasc Dis. 2019;28:1381–7.
Centers for Disease Control and Prevention. U.S. Standard Certificate of Death: Centers for Disease Control and Prevention [Internet]. Centers for Disease Control and Prevention; 2003 [cited 2021 Mar 27]. Available from: https://www.cdc.gov/nchs/data/dvs/death11-03final-acc.pdf.
Joinpoint Regression Program, Version 4.8.0.1 - April 2020; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute.
Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care United States. 2005;18:367–72.
IBM. SPSS. Armonk: IBM; 2021.
Centers for Disease Control and Prevention. Underlying cause of death 1999–2019 [Internet]. 2021 [cited 2021 Apr 2]. Available from: https://wonder.cdc.gov/wonder/help/ucd.html.
American Lung Association. Trends in pneumonia and influenza morbidity and mortality [Internet]. 2015 [cited 2021 Apr 2]. Available from: https://www.lung.org/getmedia/98f088b5-3fd7-4c43-a490-ba8f4747bd4d/pi-trend-report.pdf.pdf.
Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc United States. 2007;55:189–94.
Manu ER, Mody L, McNamara SE, Vitale CA. Advance directives and care received by older nursing home residents. Am J Hosp Palliat Care. 2017;34:105–10.
Manabe T, Teramoto S, Tamiya N, Okochi J, Hizawa N. Risk factors for aspiration pneumonia in older adults. PLoS ONE. 2015;10:e0140060.
DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care United States. 2015;30:40–8.
Hsu W-T, Lai C-C, Wang Y-H, Tseng P-H, Wang K, Wang C-Y, et al. Risk of pneumonia in patients with gastroesophageal reflux disease: a population-based cohort study. PLoS ONE. 2017;12:e0183808.
Madan R, Kairo AK, Sharma A, Roy S, Singh S, Singh L, et al. Aspiration pneumonia related deaths in head and neck cancer patients: a retrospective analysis of risk factors from a tertiary care centre in North India. J Laryngol Otol England. 2015;129:710–4.
Carnaby G, Hankey GJ, Pizzi J. Behavioural intervention for dysphagia in acute stroke: a randomised controlled trial. Lancet Neurol England. 2006;5:31–7.
Foley N, Teasell R, Salter K, Kruger E, Martino R. Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age Ageing England. 2008;37:258–64.
Momosaki R. Rehabilitative management for aspiration pneumonia in elderly patients. J Gen Fam Med. 2017;18:12–5.
Wu C-P, Chen Y-W, Wang M-J, Pinelis E. National trends in admission for aspiration pneumonia in the United States, 2002–2012. Ann Am Thorac Soc United States. 2017;14:874–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupte, T., Knack, A. & Cramer, J.D. Mortality from Aspiration Pneumonia: Incidence, Trends, and Risk Factors. Dysphagia 37, 1493–1500 (2022). https://doi.org/10.1007/s00455-022-10412-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10412-w