Abstract
The purpose of this study was to test the reliability and validity of the Turkish Eating Assessment Tool (T-EAT-10) among patients with swallowing disorders. One hundred and five patients completed the T-EAT-10 and Functional Oral Intake Scale (FOIS). The internal consistency, test–retest reliability, and criterion validity of T-EAT-10 were investigated. The internal consistency was assessed using Cronbach’s alpha. Intraclass correlation coefficient (ICC) value with 95 % confidence intervals was calculated for test–retest reliability. The criterion validity of the T-EAT-10 was determined by assessing the correlation between T-EAT-10 and FOIS. All the patients in the study completed the T-EAT-10 without assistance. The mean time to complete the instrument was 1.8 ± 0.9 min. The internal consistency of the T-EAT-10 was found to be high with 0.90 Cronbach’s alpha for test and 0.91 Cronbach’s alpha for retest reproducibility. No difference between the test and retest scores of the T-EAT-10 was found (p = 0.14). A negative, moderate correlation between T-EAT-10 and FOIS was detected (r = −0.365, p < 0.001). The T-EAT-10 is a reliable and valid symptom-specific outcome tool for dysphagia in adult Turkish patients. It can be used in clinical practice and research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia is a significant and common problem seen in all age groups. It may result in critical health problems such as dehydration, malnutrition, pneumonia, and even death. Dysphagia also causes social and emotional problems [1].
Quality of life assessments and patient-based questionnaires are mostly used in clinical swallowing evaluation in recent years. Swallow Quality of Life Questionnaire, MD Anderson Dysphagia Inventory, Sydney Swallow Questionnaire, and Eating Assessment Tool (EAT-10) are the most frequently utilized questionnaires in the swallowing evaluation. The EAT-10 has some advantages over other questionnaires. It is simple, easily scorable, and applicable over a broad range of swallowing disorders. The instrument has proven useful in establishing initial dysphagia symptom severity and in monitoring treatment outcomes. Although the EAT-10 is just a symptom survey, it has been able to predict objective evidence of swallowing dysfunction [2, 3]. It was also found that the EAT-10 scale has the ability to predict aspiration risk and this supports the clinical efficacy of the scale [4]. Due to its wide applicability, the instrument has been translated to Italian, Spanish, Japanese, and Portuguese [5–8]. To the best of our knowledge, there is no dysphagia-specific and patient-centered outcome instrument in the Turkish language. The purpose of this investigation was to translate the EAT-10 to Turkish and investigate the internal consistency, test–retest reliability, and criterion validity of the Turkish version of the EAT-10 (T-EAT-10).
Materials and Methods
The study was carried out in the Swallowing Disorders Unit, Department of Physiotherapy and Rehabilitation, Hacettepe University. Written approval to use the instrument was secured, and ethical approval was obtained from Noninvasive Clinical Research Ethics Committee (Approval number: GO 13/321) of the Hacettepe University. Written and verbal informed consent was obtained from patients who participated in this study and all data were collected prospectively.
A total of 105 patients who had neurogenic dysphagia were included in the study. The inclusion criteria were willing to participate in the study, being over the age of 18, normal cognitive function (>24 points according to the Mini Mental State Examination) [9], suffering from dysphagia at least one month, and having clinically stable neurological disease. Diagnosis, age, gender, height, weight, education level, and marital and feeding statuses of the patients were also recorded.
The study consisted of 3 different phases that were (1) translation, (2) internal consistency and reliability, and (3) criterion validity.
Translation of the EAT-10
The items of the EAT-10 were first translated to Turkish by two bilingual dysphagia experts (forward translation). Two translations were examined by four dysphagia experts and converted into a single scale with a consensus (synthesis). Thirty-five patients with a mean age of 55 ± 10.4 years who reported dysphagia symptoms were included in the initial study. Their diagnoses were stroke in 24 cases, Parkinson’s disease in 7 cases, and Multiple sclerosis in 4 cases. The patients completed the first translation and discussed the wording and meaning of each item with the two dysphagia experts. Necessary adjustments in the translation were made after the consensus to develop the final version of the T-EAT-10. A native English-speaking language expert outside of the medical profession then translated the instrument to English (backward translation) and compared to the T-EAT-10 iteration. The backward translation was presented to the creator of the scale, and the translation process was completed. Every item of the T-EAT-10 was identical to the original version (Table 1).
Internal Consistency and Reliability
One hundred and five patients with neurogenic dysphagia participated in the evaluation of both internal consistency and reliability. The data from this group were also used for the criterion validity assessment. The internal consistency and reliability of each item were measured using Cronbach’s alpha. To evaluate test–retest reliability, the T-EAT-10 was completed by the same patient on two occasions separated by a period of 48 h. The 48-h period was selected because no substantial change in the swallowing process was expected to take place within this period. The intraclass correlation coefficient (ICC) value with 95 % confidence intervals was calculated for test–retest reliability.
Criterion Validity
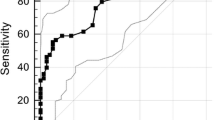
The validity of an outcome measure is the ability of an instrument to predict the functional status of a patient. The criterion validity of the T-EAT-10 was determined by assessing the correlation between T-EAT-10 and Functional oral intake scale (FOIS). FOIS is an ordinal scale that reflects the functional oral intake of patients with dysphagia. The FOIS levels are between 1 and 7. “1” means nothing by mouth, and “7” means total oral diet with no restriction. The FOIS has been shown to have adequate reliability, validity, and sensitivity to change to reflect the recommended dietary status of a patient [10]. The FOIS levels of the patients were determined based on their previous videofluoroscopic swallowing evaluation. Thus, functional oral intake levels are related to dysphagia severity of patients.
Statistical Analysis
Statistical analysis was carried out using Windows-based Statistical Package for the Social Sciences (SPSS) version 15. Arithmetical means and standard deviations (X ± SD) for quantitative variables were calculated, and all statistical tests were conducted at a 5 % significance level.
The internal consistency and reliability of each scale were measured using Cronbach’s alpha. An alpha value between 0.70 and 0.80 indicated satisfactory, between 0.8 and 0.9 indicated good, and greater than 0.9 indicated excellent consistency [11]. The intraclass correlation coefficient (ICC) value with 95 % confidence intervals was calculated to determine test–retest reliability. An ICC range between 0.60 and 0.80 indicated good and an ICC greater than 0.80 indicated excellent correlation. The Pearson product-moment coefficient was used to assess the correlation between the T-EAT-10 and FOIS to determine criterion validity. A Pearson correlation coefficient (r) less than 0.30 indicated weak, between 0.30 and 0.70 indicated moderate, and greater than 0.70 indicated strong correlation [12].
Results
One hundred and five patients (48 females and 57 males) with neurogenic dysphagia were included in the study. Their mean age was 57 ± 15.4 years. Demographic characteristics of the patients are shown in Table 2.
The mean T-EAT-10 scores of the patients and the distribution of the patients according to FOIS are shown in Table 3.
All the patients in the study completed the T-EAT-10 without any assistance. The mean time to complete the instrument was 1.8 ± 0.9 min.
The internal consistency of the T-EAT-10 was found to be high with a Cronbach’s alpha value of 0.90 for test and 0.91 for retest reproducibility. The Cronbach’s alpha values for each item in the T-EAT-10 are displayed in Table 4.
No difference was found between the test and retest scores of the T-EAT-10 (p = 0.14). A negative, moderate correlation was detected between T-EAT-10 and FOIS (r = −0.365, p < 0.001). The mean T-EAT-10 scores according to FOIS are shown in Table 5.
Discussion
The EAT-10 is a symptom-specific dysphagia instrument, which can be administered rapidly and used in a diverse range of patients. It has been shown to be a clinically useful instrument to document symptom severity and monitor disease progression and treatment efficacy. It has also been shown to predict objective evidence of swallowing dysfunction. All the Italian, Spanish, Portuguese, and Japanese versions of the EAT-10 have displayed excellent validity and reproducibility [5–8].
The current study included 105 patients with neurogenic dysphagia. All completed the T-EAT-10 without any assistance, and it was found to be a well-completed questionnaire by Turkish-speaking patients. The administration of the T-EAT-10 took <2 min. This is similar to the time required to complete the English version of the instrument [13]. Thus, the T-EAT-10 is a quick and practicable tool to use in dysphagia evaluation. The EAT-10 scores vary depending on the patient diagnosis. The mean T-EAT-10 score of the patients was 19.42 ± 11.07 in our study. Another study, which also included patients with neurogenic dysphagia, reported that the mean EAT-10 score was 23.1 ± 12.2 [14]. We performed a one-sample t test using the mean EAT-10 scores of the two studies to show if there was a similarity between the present data and prior study results of a sample from the same population. We found a statistically significant difference between EAT-10 scores (p = 0.002). This result might represent cultural or other differences in the perceptions of people of different cultures.
The internal consistency of the T-EAT-10 was high for both test and retest reproducibility of the T-EAT-10. This is consistent with the reports of other investigators evaluating the EAT-10 in other languages [5, 13]. It could be concluded that the T-EAT-10 had reliability for repeated evaluations, which means that it has a high stability over time.
In terms of validity, the results showed that there was a negative, moderate correlation between the T-EAT-10 and FOIS. The mean T-EAT-10 scores stratified by FOIS indicated that all participants even in FOIS level 7 had a perception of dysphagia. The mean T-EAT-10 scores decreased through FOIS level 7. The modest correlation suggests that self-reported measures and the decision of the clinician based on instrumental swallowing evaluation provide complementary information on dysphagia. The moderate correlation may be the case because the FOIS reflects the functional oral intake status of the patients, but the T-EAT-10 represents various aspects of a patient’s feeding status. It may also be explained by the distribution of patients according to the FOIS. The number of patients at the extreme ends of the FOIS was similar and higher, but there were fewer participants in middle ranges of the FOIS.
A replication study which also investigates the normative data for the T-EAT-10 and aims to ensure the stability of the current results will be designed. The normative data should also be confirmed across categories of socioeconomic status, gender, and race. It will also be investigated whether the scale may distinguish the effect of the dysphagia severity in different patient groups and the responsiveness of the T-EAT-10 to treatment-induced changes in patients with dysphagia.
Conclusion
The data from this investigation suggest that the T-EAT-10 is a reliable and valid symptom-specific outcome instrument for dysphagia in adult Turkish patients.
References
Farri A, Accornero A, Burdese C. Social importance of dysphagia: its impact on diagnosis and therapy. Acta Otorhinolaryngol Ital. 2007;27:83–6. doi:10.1007/s00455-001-0113-5.
Plowman EK, Tabor LC, Robison R, et al. Discriminant ability of the Eating Assessment Tool-10 to detect aspiration in individuals with amyotrophic lateral sclerosis. Neurogastroenterol Motil. 2016;28:85–90. doi:10.1111/nmo.12700.
Rofes L, Arreola V, Mukherjee R, Clave P. Sensitivity and specificity of the Eating Assessment Tool and the volume-viscosity swallow test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil. 2014;26:1256–65. doi:10.1111/nmo.12382.
Cheney DM, Siddiqui MT, Litts JK, Kuhn MA, Belafsky PC. The ability of the 10-Item Eating Assessment tool (EAT-10) to predict aspiration risk in persons with dysphagia. Ann Otol Rhinol Laryngol. 2015;124:351–4. doi:10.1177/0003489414558107.
Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, Venturini C, Orlandoni P. Reliability and validity of the Italian Eating Assessment Tool. Ann Otol Rhinol Laryngol. 2013;122(11):717–24. doi:10.1177/000348941312201109.
Burgos R, Sarto B, Segurola H, et al. Translation and validation of the Spanish version of the EAT-10 (Eating Assessment Tool-10) for the screening of dysphagia. Nutr Hosp. 2012;27:2048–54. doi:10.3305/nh.2012.27.6.6100.
Wakabayashi H, Kayashita J. Translation, reliability and validity of the Japanese version of the 10-item Eating Assessment Tool (EAT-10) for the screening of dysphagia. JJSPEN. 2014;29:871–6. doi:10.11244/jjspen.29.871.
Gonçalves MIR, Remaili CB, Behlau M. Cross-cultural adaptation of the Brazilian version of the Eating Assessment Tool - EAT-10. Codas. 2013;25:601–4. doi:10.1590/S2317-17822013.05000012.
Tombaugh TN, McIntyre NJ. The mini-mental State Examination: A comprehensive review. JAGS. 1992;40:922–35. doi:10.1111/j.1532-5415.1992.tb01992.x.
Crary MA, Mann GD, Groger ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20. doi:10.1016/j.apmr.2004.11.049.
George D, Mallery P. SPSS for Windows step by step: A simple guide and reference. 4th ed. Boston: Allyn & Bacon; 2003.
Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71.
Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24. doi:10.1177/000348940811701210.
Kaspar K, Ekberg O. Identifying vulnerable patients: role of the EAT-10 and the multidisciplinary team for early intervention and comprehensive dysphagia care. Nestle Nutr Inst Workshop Ser. 2012;72:19–31. doi:10.1159/000339977.
Acknowledgments
We would like to thank the patients who participated and consented to join this study.
Funding
The authors declared that this study has received no financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Demir, N., Serel Arslan, S., İnal, Ö. et al. Reliability and Validity of the Turkish Eating Assessment Tool (T-EAT-10). Dysphagia 31, 644–649 (2016). https://doi.org/10.1007/s00455-016-9723-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9723-9