Abstract
The purpose of this study was to evaluate the validity and the reliability of the European Portuguese version of the EAT-10 (P-EAT-10). This research was conducted in three phases: (i) cultural and linguistic adaptation; (ii) feasibility and reliability test; and (iii) validity tests. The final sample was formed by a cohort of 520 subjects. The P-EAT-10 index was compared for socio-demographic and clinic variables. It was also compared for both dysphagic and non-dysphagic groups as well as for the results of the 3Oz wst. Lastly, the P-EAT-10 scores were correlated with the EuroQol Group Portuguese EQ-5D index. The Cronbach’s α obtained for the P-EAT-10 scale was 0.952 and it remained excellent even if any item was deleted. The item-total and the intraclass correlation coefficients were very good. The P-EAT-10 mean of the non-dysphagic cohort was 0.56 and that of the dysphagic cohort was 14.26, the mean comparison between the 3Oz wst groups and the P-EAT-10 scores were significant. A significant higher perception of QoL was also found among the non-dysphagic subjects. P-EAT-10 is a valid and reliable measure that may be used to document dysphagia which makes it useful both for screening in clinical practice and in research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Swallowing is a complex function that requires coordination between both the peripheral and central nervous systems. Impaired swallowing can have many outcomes in the scope of physiological and psychosocial health. Physiologically, impaired swallowing may result in or contribute to complications such as aspiration, upper-airway obstruction, malnutrition, dehydration, and increased mortality [1, 2]. In fact, some disorders may interfere with the swallowing process and may cause dysphagia. However, dysphagia is often unrecognized and under-diagnosed by clinicians, other health care professionals and nursing home staff, and frequently goes unreported by older people and even by patients with an etiological background that may cause dysphagia [3].
Dysphagia may also cause significant social and psychological burdens and patients are more likely to be depressed and anxious at mealtimes, so avoid eating with others [2, 4]. Dysphagia is associated with high morbidity and mortality; it increases health costs and becomes more prevalent with age. Epidemiological data estimates the prevalence of dysphagia to be as high as 22 % among individuals over the age of 50 [5]. Studies have found that 13 % of patients in short-term care hospitals and up to 60 % in nursing homes have feeding difficulties [6, 7].
The research on dysphagia is relatively recent and has mainly focused on understanding the biomechanics of normal swallow and its pathophysiology. Meanwhile, other studies, have addressed assessment tools, diagnostic and intervention methods [8]. In the past few years, patient-reported symptoms and quality of life (QoL) associated to some diseases have playing an important role in guiding clinical practice. Due to the social stigma attached to drooling, coughing, and throat clearing and the effects on the simple pleasures of eating and drinking, impaired swallowing may create additional and debilitating mealtime anxieties resulting in social withdrawal that affect the person’s QoL. Many authors have reported the need for a patient-centred outcome measure that incorporates not only the physiological implications of dysphagia but also its consequence on the patient’s QoL [8–10]. These patient-centred measures may also help clinicians evaluate the effectiveness of the therapeutic planning.
Many instruments have been used to assess QoL in different groups of patients with dysphagia, notably those with head and neck cancer. Some of these instruments have subsets of questions addressing dysphagia. However, only a few tools have been specifically designed and validated to address swallowing complaints and the effects of dysphagia on QoL [11].
The Swal-QoL and the Swal-Care are outcome tools for measuring the impact of dysphagia from the patient’s perspectives. The Swal-QoL is a 44-item tool that measures 10 QoL concepts, while Swal-Care is a 15-item tool measuring the quality of care through patient satisfaction [12]. The items of Swal-QoL address desire for eating, dysphagia symptoms frequency, mental health, social concerns related to swallowing problems, food selection, fear related to eating, and the burden of dysphagia. Although Swal-QoL is currently considered to be the most comprehensive swallow-specific questionnaire, the length and time it takes to complete (about 20 min) make its use impracticable in most clinical settings. The Swal-Care items address recommendations on food, liquid, dysphagia treatment, and satisfaction with treatment.
The M. D. Anderson Dysphagia Inventory (MDADI) is among other measures for dysphagia and it was the first questionnaire specifically designed to assess dysphagia and QoL of patients with head and neck cancer [13]. There is also the swallowing disturbance questionnaire (SDQ), which is a self-reported 15-item questionnaire with yes/no questions on swallowing disturbances but validated only for patients with Parkinson diseases [14]. The Sydney swallow questionnaire (SSQ) is yet another measure and is specifically designed to evaluate swallowing difficulties in neuromyogenic, oropharyngeal dysphagia patients [15]. It was validated to administer to head and neck cancer patients and consists of 17 questions to assess and quantify patient-reported difficulties in the swallowing function. It specifically targets oral and pharyngeal phase impairments.
According to Rofes et al. [17], videofluoroscopy (VFS) is the gold standard for oropharyngeal (OD) diagnosis; however, it is not feasible to perform a VFS on every patient at risk of OD. The Eating Assessment Tool (EAT-10) screening method and the clinical bedside method, volume–viscosity swallow test (V–VST), detect OD with great accuracy [17].
The V–VST [16] was designed to identify clinical signs of impaired efficacy (labial seal, oral and pharyngeal residue, and piecemeal deglutition) and impaired safety of swallow (voice changes, cough, and decrease in oxygen saturation ≥3 %). It starts with nectar viscosity and increasing bolus volume, then liquid, and finally pudding viscosity, making it progressively difficult to protect patients from aspiration.
The 3Oz wst, created by de Pippo et al. [18], is a sensitive screening tool to identify patients at risk of dysphagia. Individuals are asked to drink 3 oz of water without interruption. Those who stop, cough, choke, or show a wet-hoarse vocal quality during the test or for 1 min afterwards are considered to have failed.
On the other hand, Belafsky et al. [8] developed the EAT-10, which is a shorter and more easily scored patient-centred dysphagia instrument than other measurement scales. It was designed to assess symptom severity, QoL and treatment efficacy. It can be administered to a wide range of patients with dysphagia and consists of 10 questions that take approximately 2 min to answer. A total score is obtained by adding all the answers; a score of more than three indicates a high self-perception of dysphagia. So far, the Italian [11] and Spanish [19] translations of EAT-10 have been validated but there is still no symptom-specific patient-centred outcome tool in European Portuguese. Due to the many practical advantages of EAT-10 (P-EAT-10), the aim of this study was therefore to make a cultural adaptation and to evaluate its reliability and validity. The discrepancy between the original culture and language of the measurement instrument and those of the country in which it will be implemented is a key issue. It is therefore vital not only to translate the tool but also to culturally adapt and validate it to the new context prior to its application.
The relevance of this study lies in the importance of having a short and easily scored instrument in European Portuguese to assess dysphagia and prevent its consequences.
Materials and Methods
The aim of the current research was to produce an European Portuguese version of the Eating Assessment Tool (P-EAT-10). The study was carried out in three phases: (i) the cultural and linguistic adaptation to Portuguese; (ii) a feasibility and reliability test of the version obtained in phase one; and (iii) validity tests to allow its adoption in Portugal.
Cultural and Linguistic Adaptation
We followed the translation/back translation process [20] to make the European Portuguese version of the English EAT-10. After formal permission that was granted by the author Peter C. Belafsky, we asked two Portuguese translators to independently translate EAT-10 into European Portuguese. The two versions were merged to obtain a consensus version. This was then given to a native English translator to make a translation back into English which was subsequently compared to the original version and the appropriate adjustments made.
We then asked a speech and language therapist (SLT) with extensive experience in dysphagia management to perform a clinical review of this Portuguese version of EAT-10. The SLT analyzed each item of the questionnaire, the original English terms and the translated Portuguese terms to assess the quality appropriateness of the translation. The Portuguese version was then discussed in a larger group of three additional SLT experts to ensure the quality of the translation and interpretation. The Portuguese version was then changed accordingly.
We then interviewed 10 subjects for a cognitive debriefing, during which they completed the Portuguese version of EAT-10 and discussed its comprehensiveness, length and adequacy, as well as any problems of clarity, understanding or redundancy of the items. Each question was thoroughly analyzed.
In fact, sometimes, the original versions of the instruments do not include all needed components. EAT-10 had no initial instructions so the subjects did not fully understand how to complete the questionnaire. These instructions were only added to the European Portuguese version once the original author gave authorisation.
Feasibility and Reliability
Following the pilot project, the modified Portuguese version of EAT-10 was then tested for feasibility and reliability. In this second phase, we recruited native Portuguese speakers from hospitals and nursing homes in the Lisbon region; these men and women were all aged 18 or over and were diagnosed with or at risk of dysphagia. We also recruited a group with no morbid condition leading to dysphagia. The Mini Mental State Examination (MMSE) was performed for subjects aged 65 or more. Those who scored above the cut-off values: 22 for 0–2 years of education, 24 for 3–6 years of education and 27 for more than 6 years of education literacy, were excluded [21].
The feasibility of the P-EAT-10 was assessed by recording how long it took for respondents to complete the questionnaire as well as the difficulties they experienced in doing so. We also determined floor and ceiling effects, i.e. the percentage of answered scores of the lowest and the highest anchors of the scale, respectively. Normative data from previous studies explored the upper limit of reference interval and suggested that a final EAT-10 score of ≥3 was abnormal [8].
The reproducibility was tested by performing a 1-week test–retest with a sample of 30 subjects, 76.7 % of whom were female, with a mean age of 89.9 ± 10.1 years. Pearson correlation coefficient and intraclass correlation coefficient were computed. No clinical intervention occurred during this week. We used the whole sample to determine the internal consistency through the Cronbach’s α coefficient.
Validity
Other measurement instruments were used for the validity tests, including the Portuguese version of the self-administered generic QoL instrument EuroQoL EQ-5D [22, 23]. The EQ-5D measure has two parts: (i) a descriptive system with five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and three levels of intensity for each dimension, defining a total of 35 = 243 health states; and (ii) a visual analogue scale (VAS) designed to look like a vertical thermometer with a scale from 0, the worst imaginable health state, to 100, the best imaginable health state [24]. An econometric model permits the calculation of preference-based values (utilities) for all health states. For the Portuguese population, this EQ-5D utility index varies between −0.536 and 1.000. The negative scores correspond to health states valued as worse than death.
There were two main reasons for choosing a generic QoL measure like EQ-5D. Firstly, there is currently no other dysphagia-specific measure that has been culturally adapted and validated into European Portuguese with which a comparison could be made. In fact, this is the first study aimed at producing such a measure. On the other hand, dysphagia symptoms undoubtedly have a marked impact on patients’ QoL. Based on these two arguments, it was decided to choose EQ-5D as our “gold standard” measure and notably because it yields a utility score representing the overall impact of an individual’s health status on his/her QoL. Moreover, the use of the European Portuguese version of EQ-5D allows us to compare P-EAT-10 scores with Portuguese validated preference-based QoL scores.
We also collected socio-demographic data (age, gender, educational level, and living arrangements) and some clinical data (morbid conditions and symptoms of dysphagia) to characterize the target population.
The construct validity of the P-EAT-10 was evaluated by testing its performance with respect to the sample’s socio-demographic and clinical characteristics and the results of the 3Oz wst. Another important issue that encompasses the construct validity is the confirmation of the outcome measurement instrument’s structure. Accordingly, it was necessary to check whether the scores obtained by the P-EAT-10 maintained the unidimensionality proposed by the original author, using a principal component factor analysis. However, the suitability of this statistical techniques was first assessed by computing the Keyser–Meyer–Olkin (KMO) measure as well as Bartlett´s test of sphericity to test the null hypothesis that the correlation matrix is an identity matrix.
Finally, the criterion validity was tested by comparing EAT-10 scores with both the scores obtained by the QoL measure EQ-5D and VAS scores. Concordances between criteria were computed by correlation coefficients and χ 2 tests. Statistical tests were conducted using SPSS 21.0. Descriptive analyses, including measures of central tendency and dispersion, were also performed.
This study followed the basic ethical principles set by the Declaration of Helsinki and received prior approval from the Ethic Commissions of the institutions involved. All subjects or their representatives signed a written informed consent, and received no compensation. Data collected were used anonymously, without any reference to patients’ personal identity, which was encoded in all study documents.
Results
Cultural and Linguistic Adaptation
The cognitive debriefing involved three males and seven females, with an average age of 81.1 ± 11.4 years (median = 84, ranging from 51 to 91) and with medium to low education. A number of issues were raised during this meeting. For example, patients had some difficulty understanding what they were supposed to do with the given questionnaire. Also, some of them did not understand that 0 (no problem) and 4 (severe problem) in the response scale were two extreme anchors and that there were three others levels between. As an outcome of this cognitive debriefing, and after contact with the author, we included an introductory section telling the respondent to cross the number corresponding to what they consider the most appropriate answer to each question.
The items of the Portuguese version of EAT-10 following the cultural and linguistic adaptation are presented in Table 1. All items are answered in a verbal rating scale with four anchors from 0 (no problem) to 4 (severe problem).
The Sample
The study sample was composed of 520 individuals, 205 of whom had symptoms of dysphagia. Table 2 presents the socio-demographic and clinical data of the sample.
As can be seen in Table 2, 72.3 % of the subjects were female. The mean age of the total sample was 78.8 ± 12.2, more than 48 % were divorced or widowed and half of them had only 5–9 years of education. More than half (53.1 %) were considered obese and the mean body mass index was 25.8 ± 4.9. Just over 60 % (60.6 %) had no symptoms of dysphagia and no medical history of neurologic or neoplastic disorder. Those with symptoms of dysphagia (205) were mainly stroke patients or those with head and neck cancer.
The distribution of EAT-10 scores and QoL scores is presented in Table 3.
We conclude that only 38.8 % had a strong perception of dysphagia, and that it affected their usual activities and their QoL. It should also be noted that the patients’ greatest difficulties are related to self-care (31.0 %) and usual activities (33.1 %). The mean perception of their QoL was generally low.
Feasibility
The mean EAT-10 completion time was 8.0 ± 2.0 min, ranging from 6:10 to 12:20 min and all items were filled in by the subjects. We assessed the floor effect of EAT-10 by analyzing the distribution of each item (Table 4).
No major floor effect was found. In fact, our sample showed a group of patients with severe problems caused by swallowing, especially going out for meals, causing pain and stress.
Reliability
Table 5 shows the results of the reliability tests performed in the Portuguese version of EAT-10. More specifically, it presents the results from the Pearson correlation coefficients (test–retest), the intraclass correlation coefficients (ICC), the item-total correlation coefficients, and the internal consistency Cronbach’s α if each item was deleted.
The Cronbach’s α obtained for the whole EAT-10 scale was excellent (0.952) and it remained so even if we deleted an item. Moreover, all items showed high item-total correlation scores and high test–retest correlation coefficients (and intraclass correlation coefficients).
Construct Validity
We assessed the construct validity of the Portuguese EAT-10 by comparing its scores to different socio-demographic variables such as gender, age, education, family status, and body mass index. Table 6 shows the sensitivity of EAT-10 index for these variables.
As we can observe, gender, education, or the body mass index do not have any influence on dysphagia impact measured by EAT-10. However, younger (40–64 years old) and married, perceived more severe problems associated to dysphagia.
For the construct validity test, we looked at the behaviour of the Portuguese version of EAT-10 when comparing individuals with and without dysphagia. The results are presented in Table 7.
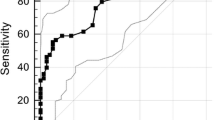
All P-EAT-10 items and its total score discriminated significantly between patients with and without dysphagia symptoms. In order to evaluate the degree to which the test measures what it is purposed the scores of the P-EAT-10 and the 3Oz wst were compared. The 3Oz wst evidenced a high and significant association with the P-EAT-10 scores. Table 8 presents the average scores of EAT-10 for each classification and the results from an ANOVA test.
A post hoc Scheffé test reveals significant differences between individuals with both cough and wet voice and those with no changes at all. Moreover, there is also a significant difference when a dummy variable is created for the 3 Oz wst (changes/no changes).
Finally, a factor analysis was performed with varimax rotation that evidenced the desirable one dimensional structure, corresponding to 70.7 % of explained variance. The corresponding KMO measure of sampling adequacy was 0.948 and the sample passed the Bartlett’s test of sphericity (p < 0.001).
Criterion Validity
Criterion validity was tested by comparing the Portuguese version of EAT-10 with the QoL scores obtained by the EQ-5D. Using the EAT-10 cutoff point mentioned earlier (isolating individuals with and without dysphagia, we created a dummy variable representing. When we compared both the EQ-5D index and VAS for each of the values of the variable, we found a significantly higher perception of QoL among the individuals without any problems, as shown in Table 9. In fact, individuals with no symptoms perceived their QoL to be better than individuals with symptoms.
. As we can see from Table 10, individuals with dysphagia assigned the two most severe levels to all dimensions of the EQ-5D descriptive system except for ‘pain/discomfort’.
Discussion
Dysphagia is a difficulty in swallowing and the EAT-10 is a self-administered outcome measure for the subjective assessment of dysphagia patients with a vast array of clinical diagnoses. As dysphagia is a symptom, not a disease, it is essential that the clinician is able to document the severity of a patient’s self-perception of the disability caused by a swallowing problem. Although other dysphagia inventories were developed and validated before the EAT-10, none of these are in widespread clinical use.
EAT-10 revealed excellent internal consistency, test–retest reproducibility and criterion-based validity. It has been used to document initial severity of dysphagia and to monitor response to treatment in persons with a wide range of swallowing disorders. Its validity and reliability have been demonstrated in large cohorts of patients with a wide variety of causes for dysphagia. Higher EAT-10 scores indicate higher self-perception of dysphagia while normative data suggest that a score equal to or >3 is considered abnormal. The absence of specific domains precludes the stratification of subset disability into social, emotional, and functional categories. This limitation is, however, overcome by the test’s simplicity, the easiness of administration and scoring, and its utility in patients with a wide range of dysphagia causes.
In this study, the psychometric properties of the European P-EAT-10 were studied in a group of 315 patients with dysphagia symptoms and in a control group of 205 subjects without symptoms. All questionnaires were filled in completely suggesting that everyone understood the questions well and felt comfortable answering them. Therefore, P-EAT-10 can be considered an instrument that is easily self-administrated and requires about 8 min to complete. However, the population selected for this study only included cognitively able patients and subjects.
The internal consistency of the P-EAT-10 proved to be high (α = 0.952), though slightly lower than the one reported by its authors. The results are higher than both the Italian [11] and the Spanish version; the former obtained Cronbach’s alpha values of 0.90 and 0.93, and the latter a Cronbach’s α coefficient of 0.87 [19].
As for reliability, the scores obtained in the test–retest analysis for both the patient and control groups confirm the high stability and reproducibility of the P-EAT-10 over time. In fact, ICC scores ranged from 0.921 to 1.000 and the test–retest Pearson correlation coefficients for both patient and control groups ranged from 0.934 to 1.000, higher than those reported by the authors of the original version.
Similarly to the original study, patients with symptoms scored higher than those with no symptoms. P-EAT-10 can therefore be considered a sensitive tool to discriminate between patients with and without swallowing disorders. Moreover, a significant relation between P-EAT-10 scores and the 3Oz wst was found, which indicates that the test measures the intended construct.
In conclusion, P-EAT-10 is a reliable and valid self-administered, symptom-specific outcome tool for dysphagia in adult Portuguese patients. The normative data from a large cohort of patients without dysphagia, including a large number of old patients, suggest that a score of 3 or more is abnormal. The application of P-EAT-10 in Portuguese patients with dysphagia is therefore recommended in everyday clinical practice as well as in epidemiological and outcome research. Lastly, while this study represents a validation of the original English EAT-10 in another language, the optimal results of internal consistency, test–retest reliability and clinical validity seem promising and could allow for transcultural research in swallowing disorders. The results obtained provide distinct and complimentary information on dysphagia. The difficulty of using instrumental swallowing assessment was one of the main limitations of the present study. Other limitation was the reduced number of head and neck cancer patients presented in the sample.
Future research is necessary to replicate these findings in a diverse sample of persons with a variety of causes of dysphagia. EAT-10 data across age groups, as well from various categories of socioeconomic status, gender and race should be evaluated in order to produce normative valid data for both young and elderly populations. A comparison of EAT-10 scores obtained before and after medical and surgical dysphagia therapy in larger cohorts will also help clarify the role of the EAT-10 in the documentation and evaluation of treatment outcomes.
References
Nogueira D, Reis E. Swallowing disorders in nursing home residents: how can the problem be explained? Clin Interv Aging. 2013;8:221–7.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46. doi:10.1007/s00455-001-0113-5.
Steele CM, Greenwood C, Ens I, Robertson C, Seidman-Carlson R. Mealtime difficulties in a home for the aged: not just dysphagia. Dysphagia. 1997;12(1):43–50 discussion 1.
Wilkins T, Gillies RA, Thomas AM, Wagner PJ. The prevalence of dysphagia in primary care patients: a HamesNet Research Network study. J Am Board Fam Med. 2007;20(2):144–50. doi:10.3122/jabfm.2007.02.060045.
Bloem BR, Lagaay AM, van Beek W, Haan J, Roos RA, Wintzen AR. Prevalence of subjective dysphagia in community residents aged over 87. BMJ. 1990;300(6726):721–2.
Siebens H, Trupe E, Siebens A, Cook F, Anshen S, Hanauer R, et al. Correlates and consequences of eating dependency in institutionalized elderly. J Am Geriatr Soc. 1986;34(3):192–8.
Lindgren S, Janzon L. Prevalence of swallowing complaints and clinical findings among 50-79-year-old men and women in an urban population. Dysphagia. 1991;6(4):187–92.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919–24.
Leow LP, Huckabee ML, Anderson T, Beckert L. The impact of dysphagia on quality of life in ageing and Parkinson’s disease as measured by the swallowing quality of life (SWAL-QOL) questionnaire. Dysphagia. 2010;25(3):216–20. doi:10.1007/s00455-009-9245-9.
Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of life–a population-based study. Aliment Pharmacol Ther. 2008;27(10):971–9. doi:10.1111/j.1365-2036.2008.03664.x.
Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, et al. Reliability and validity of the Italian Eating Assessment Tool. Ann Otol Rhinol Laryngol. 2013;122(11):717–24.
McHorney CA, Bricker DE, Robbins J, Kramer AE, Rosenbek JC, Chignell KA. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: II. Item reduction and preliminary scaling. Dysphagia. 2000;15(3):122–33.
Carlsson S, Ryden A, Rudberg I, Bove M, Bergquist H, Finizia C. Validation of the Swedish M. D. Anderson Dysphagia Inventory (MDADI) in patients with head and neck cancer and neurologic swallowing disturbances. Dysphagia. 2012;27(3):361–9. doi:10.1007/s00455-011-9375-8.
Manor Y, Giladi N, Cohen A, Fliss DM, Cohen JT. Validation of a swallowing disturbance questionnaire for detecting dysphagia in patients with Parkinson’s disease. Mov Disord. 2007;22(13):1917–21. doi:10.1002/mds.21625.
Dwivedi RC, St Rose S, Roe JW, Khan AS, Pepper C, Nutting CM, et al. Validation of the Sydney Swallow Questionnaire (SSQ) in a cohort of head and neck cancer patients. Oral Oncol. 2010;46(4):e10–4. doi:10.1016/j.oraloncology.2010.02.004.
Rofes L, Arreola V, Clave P. The volume-viscosity swallow test for clinical screening of dysphagia and aspiration. Nestle Nutr Inst Workshop Ser. 2012;72:33–42. doi:10.1159/000339979.
Rofes L, Arreola V, Mukherjee R, Clave P. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil. 2014;26(9):1256–65. doi:10.1111/nmo.12382.
DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol. 1992;49(12):1259–61.
Burgos R, Sarto B, Segurola H, Romagosa A, Puiggros C, Vazquez C, et al. Translation and validation of the Spanish version of the EAT-10 (Eating Assessment Tool-10) for the screening of dysphagia. Nutr Hosp. 2012;27(6):2048–54. doi:10.3305/nh.2012.27.6.6100.
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for translation and cultural adaptation. Value Health. 2005;8(2):94–104. doi:10.1111/j.1524-4733.2005.04054.x.
Morgado J, Rocha CS, Maruta C, Guerreiro M, Martins IP. Cut-off scores in MMSE: a moving target? Eur J Neurol. 2010;17(5):692–5. doi:10.1111/j.1468-1331.2009.02907.x.
Ferreira LN, Ferreira PL, Pereira LN, Oppe M. The valuation of the EQ-5D in Portugal. Quality Life Res. 2014;23(2):413–23. doi:10.1007/s11136-013-0448-z.
Ferreira LN, Ferreira PL, Pereira LN, Oppe M. EQ-5D Portuguese population norms. Qual Life Res. 2014;23(2):425–30. doi:10.1007/s11136-013-0488-4.
R. R, F. C, A. S. Introduction. In EQ-5D value sets – inventory, comparative review and user guide. 2007.
Conflict of interest
Authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nogueira, D.S., Ferreira, P.L., Reis, E.A. et al. Measuring Outcomes for Dysphagia: Validity and Reliability of the European Portuguese Eating Assessment Tool (P-EAT-10). Dysphagia 30, 511–520 (2015). https://doi.org/10.1007/s00455-015-9630-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9630-5