Abstract
Quantitative levels of harmful oral microbes present following complex surgical excisions of head and neck cancer are important since wounds are often contaminated through direct connection to the oral cavity and its flora. This possibility is especially important in irradiated patients who have decreased protective salivary function. In addition, high oral microbial levels increase and intensify oral mucositis leading to significant morbidity in patients treated with radiation therapy. One previously untested surgical teaching to decrease the bacterial inoculum present in the oral cavity is to counsel patients against consuming otherwise nutritious dairy products, as they are thought to coat the oral cavity with rate-limiting nutrients vital for bacterial growth. This risk may extend to individuals with chronic laryngeal penetration or aspiration, since salivary bacterial load might represent a lethal threat in the presence of marginal pulmonary reserve. A crossover study using six healthy adult volunteers and six patients who had previously undergone radiation therapy to an oropharyngeal primary site was performed. Saliva samples were quantitatively cultured in both groups with and without the consumption of dairy products at 1-h and 5-h intervals. Analysis of quantitative cultures demonstrated that the consumption of dairy products had no influence on bacterial levels present in previously radiated subjects and nonirradiated controls. Additionally, the consumption of dairy did not affect the composition of microbes present. Due to the lack of changes in both quantity and composition of oral bacteria seen in this study, patients would not benefit from the avoidance of dairy products.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral microbes act as a reservoir for infection in contaminated head and neck surgical wounds and may significantly increase the incidence and severity of mucositis during treatment with radiation therapy. Patients who have previously undergone treatment with radiation are at a greater risk of infection due to decreased salivary function caused by irreversible fibrosis in extraglandular blood vessels and nervous structures [1, 2]. In patients receiving radiation therapy, oral mucositis can be exacerbated by gram-negative organisms and yeast colonizing damaged mucosal surfaces leading to ulceration [3, 4]. Stopping this chain of events is important, as this condition causes some of the greatest morbidity faced by head and neck cancer patients, leading to treatment-limiting toxicity and decreased efficacy. In an attempt to minimize the risk of surgical infection, it is now standard practice for patients to have preoperative dental care, optimization of nutritional status, perioperative antibiotics, and meticulous oral hygiene regimens often involving antibiotic rinses [5]. Although further investigation is required, several studies have shown that topical antimicrobial rinses decrease the severity and incidence of oral mucositis [4, 6–12].
It is thought that consumption of dairy may increase the quantity of oral microbes by coating the oral cavity with rate-limiting nutrients. The ability of dairy to stimulate the growth of bacteria by providing appropriate amino acids, sugars, and minerals has been known since the early 1900 s, leading to its use in bacterial culture media, which continues today [13, 14]. Here, dairy supports a multitude of bacteria, including Streptococcus, Staphylococcus, and Escherichia species [14, 15]. Dental investigations involving oral cavity flora have shown that milk is able to increase Streptococcus mutans biomass on in vitro enamel slabs [16]. There has been no research on the in vivo effects of dairy on bacteria associated with surgical wounds or on the bacterial load of aspirated oropharyngeal contaminants that could irreparably destroy alveolar pulmonary function in the very patient who would benefit most from the nourishing potential of dairy products.
Methods
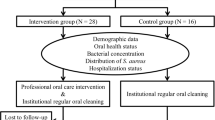
IRB approval was obtained and six healthy subjects and six subjects with a previous history of oropharyngeal squamous cell carcinoma were enrolled in the study. All individuals who had a previous diagnosis of squamous cell carcinoma had received more than 54 Gy of radiation to the primary site. The average time from completion of radiation treatment to the collection of the salivary sample was 4 years 7 months. Control of any outside influence on oral microbes was attempted by ensuring that no subject had taken antibiotics during the month before the investigation, no participant had undergone surgery in the previous 6 months, and all patients were between 50 and 65 years old. It was not possible to dictate the patients’ home medications, which could possibly influence salivary function. Subjects followed an oral hygiene regimen starting 1 week before the initial salivary samples were taken. Participants were instructed to brush their teeth morning and night with a nonantibiotic toothpaste for 2 min. Additionally, they were instructed to avoid the use of antiseptic mouthwash.
After 1 week of the prescribed oral hygiene regimen, patients awoke and ate a normal breakfast. They brushed their teeth at 7:45 am. At 8:00 am, a saliva sample was collected using the ESwab system (Copan Italia 480 CE), where a nylon flocked swab was soaked in the subject’s saliva and immediately submerged into 1 ml of Amies liquid transport medium. Two more saliva samples were collected in the same manner 1 and 5 h after the initial sample was collected. Subjects were instructed to abstain from eating after the initial salivary sample was collected until the conclusion of sample collection that day. One week later the subjects repeated the process; however, they ate two cups of Haagen Daz vanilla ice cream (Nestlé Dreyer’s Ice Cream Company, Oakland, CA, USA) immediately after the first sample was collected.
Volumes of 10 μl from the ESwab transport medium were inoculated and plated by the PREVI Isola system (bioMérieux, Marcy l’Etoile, France) onto Columbia agar with 5 % sheep blood, chocolate agar, MacConkey agar, anaerobic blood agar, and Sabouraud dextrose agar (Remel, Lenexa, KS, USA). Columbia blood, chocolate, and MacConkey agar were incubated at 36 °C in 5 % CO2 for 48 h. Anaerobic blood agar was incubated for 48 h at 36 °C in a Bactron IV anaerobic chamber (Shel Lab, Cornelius, OR, USA). Sabouraud dextrose agar was incubated in an aerobic chamber at 30 °C for optimal yeast growth. Colonies were counted and isolates were taken of each unique morphological type and identified using the Vitek MS (bioMérieux).
Statistical repeated-measurements analysis was performed using the PROC MIXED procedure (SAS Institute, Cary, NC, USA) to assess the change in species number over time and the difference between groups and between dairy statuses. Since the amount of organism was measured as ordinal categories of <10,000, 10,000–50,000, 50,000–100,000, and >100,000 CFU/ml for each species, a simple scale summarizing the amount of all detectable organisms was not available. Therefore, the generalized estimating equation (GEE) approach was used to model the multinomial response in a repeated-measurement setting. The interaction among groups, time, and dairy condition were examined. Further analysis of simple effects was performed to test the hypothesis of interest. The odds ratio and 95 % confidence interval were reported. It contrasted the likelihood of having higher-level CFU counts between different time points, groups, and dairy statuses. The significance level was set as <0.05, unless post hoc pairwise comparison was performed. In that case, Bonferroni correction was applied. All the statistical analyses was performed using SAS v9.2 software (SAS Institute, Cary, NC, USA).
Results
During the collection of all samples, 53 species of pathological bacteria and 4 species of pathological fungi were identified. Species were most likely to be gram positive by stain and anaerobic by growth condition (Table 1). Only two of six controls tested positive for fungus. In contrast, all six previously radiated patients tested positive for fungus.
When analyzing quantitative bacterial level changes, several results were found. No difference was seen in quantitative bacterial levels in previously irradiated subjects when they ate dairy compared to when they did not eat dairy (time by dairy interaction, p = 0.19; initial, OR 1.31, 95 % CI 0.33–5.19, p = 0.70; at 1 h, OR 0.89, 95 % CI 0.32–2.47, p = 0.83; at 5 h, OR 0.57, 95 % CI 0.12–2.63, p = 0.47). No difference was seen in the quantitative bacterial levels in nonirradiated control subjects when they ate dairy compared to when they did not eat dairy; however, nondairy-eating controls had increased odds of having a lower initial level of bacteria (time by dairy interaction, p < 0.0001; initial, OR 0.29, 95 % CI 0.10–0.83, p = 0.02; at 1 h, OR 1.14, 95 % CI 0.53–2.42, p = 0.74; at 5 h, OR 1.28, 95 % CI 0.40–4.12, p = 0.68). No difference was seen when previously irradiated patients were compared with nonirradiated patients with or without the consumption of dairy (Fig. 1) (without dairy initial, OR 0.35, 95 % CI 0.11–1.09, p = 0.07; at 1 h, OR 1.09, 95 % CI 0.41–2.93, p = 0.86; at 5 h, OR 1.19, 95 % CI 0.26–5.41, p = 0.82) (with dairy initial, OR 1.58, 95 % CI 0.41–6.05, p = 0.5; at 1 h, OR 0.86, 95 % CI 0.39–1.90, p = 0.71; at 5 h, OR 0.87, 95 % CI 0.26–2.90, p = 0.82). Only nonirradiated patients who had not consumed dairy showed increased odds of higher bacterial levels from the initial sample to hour 1 and from initial sample to hour 5 (at 1 h, OR 3.12, 95 % CI 2.26–4.31, p < 0.0001; at 5 h, OR 2.20, 95 % CI 1.42–3.40, p = 0.0004).
Further analysis of the composition of species present in experimental groups yielded several results. There was no difference in the number of species present between previously irradiated subjects and nonirradiated subjects (p = 0.48). However, the change in the amount of bacteria species present between those who did not eat dairy in both irradiated and nonirradiated groups and those who ate dairy was significant (time by dairy interaction: p = 0.02). In those who did not eat dairy the average number of species decreased 1.3 ± 0.4 (LS Mean ± SE) in the first hour of testing (p = 0.006) (Fig. 2). There was no significant difference in the mean number of anaerobic versus aerobic bacteria or gram-positive versus gram-negative bacteria in radiated and nonirradiated subjects with and without dairy consumption (p = 0.31, p = 0.96, p = 0.12, p = 1.00, respectively).
The low level of fungal prevalence precluded its analysis in this study.
Discussion
The human oral microbiome is immense in nature, with over 1,000 bacterial species previously identified [17]. Of these, only half can be found through traditional culture techniques. Although a great majority of oral microbes are not pathological, others have been linked to disease processes and infections. During this study, a wide range of pathological bacteria, consisting of 53 separate species, was found to be present in both irradiated and nonirradiated patients. A majority were gram positive and anaerobic in nature (Table 1). The results of our study showed no change in the quantitative levels of bacteria in both irradiated and nonirradiated patients after they ate dairy compared to when they did not eat dairy products. These results suggest that the primary factors for nutrition needed for bacterial growth come from glycoproteins previously present in the mouth and not oral intake. It also raises the question of what role casein plays in affecting bacterial growth. Casein is a protein found in many dairy products and has been shown to inhibit the adherence of bacteria when incorporated into the salivary pellicle lining the oral cavity [18, 19]. The lack of difference between irradiated and nonirradiated patients may be secondary to the similar ages of both groups. Our healthy controls were of an advanced age and may have lacked some salivary function, making the difference between them and previously irradiated subjects statistically negligible.
The consumption of dairy had no effect on the amount of bacterial species present or the composition of bacteria represented by gram stain and oxygen growth requirements, although patients who did not consume dairy had an initial decrease in the average number of species present after 1 h. It is possible that dairy consumption supported initial diversity within the microbiome, disallowing single colony expansion at the expense of other bacterial species. Importantly, by 5 h there was no significant difference between groups in the number of bacterial species present. Interestingly, and in support of our data, a previous study of 120 individuals from 12 locations around the world found no differences in salivary microbiota despite the different diets [20]. The results of this previous geographically diverse study and our results suggest that microbial composition is not strongly influenced by diet. Instead, host species may be the most important influence on the type of bacteria present.
We believe that there was the appropriate time between sample collections to assure that any bacterial trends that would arise due to the consumption of dairy were witnessed. In vitro and in vivo studies of oral organisms show that bacterial cell division occurs approximately every 1–2 h. An exponential phase of accumulation of bacteria is seen within the first 4 h, followed by a plateau in bacterial growth between 6 and 24 h [21–24]. Studies that evaluated quantitative bacteria counts after noncontinuous intervention have demonstrated that bacteria decreases, with regrowth taking place within 4 h [25]. Our study included time points up to 5 h from intervention, assuring adequate time for bacterial growth.
Two of six controls tested positive for fungus, whereas all six previously irradiated patients tested positive. Candida species are asymptomatically carried in ~50 % of all individuals, with higher levels found in patients who have poor salivary flow rates, including those with Sjögren’s syndrome or individuals with previous exposure to radiation [17, 26]. This is thought to be partly caused by decreased pH levels seen in low salivary flow conditions.
Further studies on the effects of diet on oral microbes should address the role of probiotics. The data for their use in the oral cavity is limited, but their use is growing in popularity due low cost and low side effect profiles. Current research is focused on the efforts of dentists to decrease harmful bacteria that causes caries and periodontal disease [27, 28]. Probiotics do not influence bacterial growth through direct nutritional intake of a product containing them. Instead, their presence inhibits pathogens through the phenomenon of colonization resistance [29]. Few binding sites are available for pathogenic bacteria due to the presence of nonpathogenic species. In addition, probiotic bacteria modulate oral mucosal immunity, change oral pH levels, and produce bacteriocin inhibiting the growth of other bacteria [30, 31]. Studies involving dairy, yogurt, ice cream, and cheese containing specific probiotic bacteria have shown that the bacteria have the ability to reduce levels of Streptococcus mutans and Candida albicans [32–35]. No studies have investigated the effect of probiotics on bacteria linked to surgical infections and mucositis. Our study addresses the consumption of dairy although no probiotic bacteria were present.
Conclusion
Due to the lack of quantitative changes in bacterial levels and composition seen in this study, patients would not benefit from the avoidance of dairy products in an effort to decrease inoculum present in surgical wounds or in the salivary inoculum of laryngeal aspirates.
References
Rode M, Smid L, Budihna M, Gassperssic D, Soba E. The influence of pilocarpine and biperiden on pH value and calcium, phosphate, and bicarbonate concentrations in saliva during and after radiotherapy for head and neck cancer. Oral Surg Oral med Oral Pathol Oral Radiol Endod. 2001;92(5):509–14. doi:10.1067/moe.2001.115984.
Hannig M, Dounis E, Henning T, Apitz N, Stosser L. Does irradiation affect the protein composition of saliva? Clin Oral Invest. 2006;10(1):61–5. doi:10.1007/s00784-005-0026-z.
Naidu MU, Ramana GV, Rani PU, Mohan IK, Suman A, Roy P. Chemotherapy-induced and/or radiation therapy-induced oral mucositis-complicating the treatment of cancer. Neoplasia. 2004;6(5):423–31. doi:10.1593/neo.04169.
Donnelly JP, Bellm LA, Epstein JB, Sonis ST, Symonds RP. Antimicrobial therapy to prevent or treat oral mucositis. Lancet Infect Dis. 2003;3(7):405–12.
Kirchner JC, Edberg SC, Sasaki CT. The use of topical oral antibiotics in head and neck prophylaxis: is it justified? Laryngoscope. 1988;98(1):26–9. doi:10.1288/00005537-198801000-00007.
McGaw WT, Belch A. Oral complications of acute leukemia: prophylactic impact of a chlorhexidine mouth rinse regimen. Oral Surg Oral Med Oral Pathol. 1985;60(3):275–80.
Ferretti GA, Ash RC, Brown AT, Largent BM, Kaplan A, Lillich TT. Chlorhexidine for prophylaxis against oral infections and associated complications in patients receiving bone marrow transplants. J Am Dent Assoc. 1987;114(4):461–7.
Ferretti GA, Raybould TP, Brown AT, Macdonald JS, Greenwood M, Maruyama Y, Geil J, Lillich TT, Ash RC. Chlorhexidine prophylaxis for chemotherapy- and radiotherapy-induced stomatitis: a randomized double-blind trial. Oral Surg Oral Med Oral Pathol. 1990;69(3):331–8.
Symonds RP, McIlroy P, Khorrami J, Paul J, Pyper E, Alcock SR, McCallum I, Speekenbrink AB, McMurray A, Lindemann E, Thomas M. The reduction of radiation mucositis by selective decontamination antibiotic pastilles: a placebo-controlled double-blind trial. Br J Cancer. 1996;74(2):312–7.
Adamietz IA, Rahn R, Bottcher HD, Schafer V, Reimer K, Fleischer W. Prophylaxis with povidone-iodine against induction of oral mucositis by radiochemotherapy. Support Care Cancer. 1998;6(4):373–7.
Rahn R, Adamietz IA, Boettcher HD, Schaefer V, Reimer K, Fleischer W. Povidone-iodine to prevent mucositis in patients during antineoplastic radiochemotherapy. Dermatology. 1997;195(Suppl 2):57–61.
Matthews RH, Ercal N. Prevention of mucositis in irradiated head and neck cancer patients. J Exp Ther Oncol. 1996;1(2):135–8.
Nelson FE. The effect of the new standard milk agar on the plate count of dairy products. J Bacteriol. 1940;39(3):263–72.
O’Brien KL, Bronsdon MA, Dagan R, Yagupsky P, Janco J, Elliott J, Whitney CG, Yang YH, Robinson LG, Schwartz B, Carlone GM. Evaluation of a medium (STGG) for transport and optimal recovery of Streptococcus pneumoniae from nasopharyngeal secretions collected during field studies. J Clin Microbiol. 2001;39(3):1021–4. doi:10.1128/JCM.39.3.1021-1024.2001.
Fang W, Shi M, Huang L, Shao Q, Chen J. Growth of lactobacilli, Staphylococcus aureus and Escherichia coli in normal and mastitic milk and whey. Vet Microbiol. 1993;37(1–2):115–25.
Munoz-Sandoval C, Munoz-Cifuentes MJ, Giacaman RA, Ccahuana-Vasquez RA, Cury JA. Effect of bovine milk on Streptococcus mutans biofilm cariogenic properties and enamel and dentin demineralization. Pediatr Dent. 2012;34(7):e197–201.
Wade WG. The oral microbiome in health and disease. Pharmacol Res. 2013;69(1):137–43. doi:10.1016/j.phrs.2012.11.006.
Schupbach P, Neeser JR, Golliard M, Rouvet M, Guggenheim B. Incorporation of case in oglycomacropeptide and case in ophosphopeptide into the salivary pellicle inhibits adherence of mutans streptococci. J Dent Res. 1996;75(10):1779–88.
Aimutis WR. Bioactive properties of milk proteins with particular focus on anticariogenesis. J Nutr. 2004;134(4):989S–95S.
Nasidze I, Li J, Quinque D, Tang K, Stoneking M. Global diversity in the human salivary microbiome. Genome Res. 2009;19(4):636–43. doi:10.1101/gr.084616.108.
Brusca MI, Irastorza RM, Cattoni DI, Ozu M, Chara O. Mechanisms of interaction between Candida albicans and Streptococcus mutans: an experimental and mathematical modelling study. Acta Odontol Scand. 2013;71(3–4):416–23. doi:10.3109/00016357.2012.690530.
Nyvad B, Kilian M. Microbiology of the early colonization of human enamel and root surfaces in vivo. Scand J Dent Res. 1987;95(5):369–80.
Dawes C. Estimates, from salivary analyses, of the turnover time of the oral mucosal epithelium in humans and the number of bacteria in an edentulous mouth. Arch Oral Biol. 2003;48(5):329–36.
Li YH, Bowden GH. Characteristics of accumulation of oral gram-positive bacteria on mucin-conditioned glass surfaces in a model system. Oral Microbiol Immunol. 1994;9(1):1–11.
Balbuena L, Stambaugh KI, Ramirez SG, Yeager C. Effects of topical oral antiseptic rinses on bacterial counts of saliva in healthy human subjects. Otolaryngol Head Neck Surg. 1998;118(5):625–9.
Karbach J, Walter C, Al-Nawas B. Evaluation of saliva flow rates, Candida colonization and susceptibility of Candida strains after head and neck radiation. Clin Oral Invest. 2012;16(4):1305–12. doi:10.1007/s00784-011-0612-1.
Bosch M, Nart J, Audivert S, Bonachera MA, Alemany AS, Fuentes MC, Cune J. Isolation and characterization of probiotic strains for improving oral health. Arch Oral Biol. 2012;57(5):539–49. doi:10.1016/j.archoralbio.2011.10.006.
Bowden GH. Does assessment of microbial composition of plaque/saliva allow for diagnosis of disease activity of individuals? Community Dent Oral Epidemiol. 1997;25(1):76–81.
Vollaard EJ, Clasener HA. Colonization resistance. Antimicrob Agents Chemother. 1994;38(3):409–14.
Wescombe PA, Heng NC, Burton JP, Chilcott CN, Tagg JR. Streptococcal bacteriocins and the case for Streptococcus salivarius as model oral probiotics. Futur Microbiol. 2009;4(7):819–35. doi:10.2217/fmb.09.61.
Meurman JH. Probiotics: do they have a role in oral medicine and dentistry? Eur J Oral Sci. 2005;113(3):188–96. doi:10.1111/j.1600-0722.2005.00191.x.
Nase L, Hatakka K, Savilahti E, Saxelin M, Ponka A, Poussa T, Korpela R, Meurman JH. Effect of long-term consumption of a probiotic bacterium, Lactobacillus rhamnosus GG, in milk on dental caries and caries risk in children. Caries Res. 2001;35(6):412–20.
Ahola AJ, Yli-Knuuttila H, Suomalainen T, Poussa T, Ahlstrom A, Meurman JH, Korpela R. Short-term consumption of probiotic-containing cheese and its effect on dental caries risk factors. Arch Oral Biol. 2002;47(11):799–804.
Caglar E, Kuscu OO, Selvi Kuvvetli S, Kavaloglu Cildir S, Sandalli N, Twetman S. Short-term effect of ice-cream containing Bifidobacterium lactis Bb-12 on the number of salivary mutans streptococci and lactobacilli. Acta Odontol Scand. 2008;66(3):154–8. doi:10.1080/00016350802089467.
Hatakka K, Ahola AJ, Yli-Knuuttila H, Richardson M, Poussa T, Meurman JH, Korpela R. Probiotics reduce the prevalence of oral candida in the elderly–a randomized controlled trial. J Dent Res. 2007;86(2):125–30.
Acknowledgments
This work was supported in part by the Virginia Wright Fund and the Charles W. Oshe Endowment.
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schutt, C.A., Neubauer, P., Paskhover, B. et al. The Impact of Dairy Consumption on Salivary Inoculum. Dysphagia 29, 277–282 (2014). https://doi.org/10.1007/s00455-013-9508-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9508-3