Abstract
This article describes the study of the characteristics of sequential swallowing of 100 ml of liquid (dyed water) in two swallowing trials, directly from a cup and through a straw, in healthy elderly individuals. The aim of the study was to determine whether differences in the swallowing pattern are influenced by the type of utensil used. The subjects were subjected to clinical assessment and fiberoptic endoscopic evaluation of swallowing. The research found that intake from the cup showed a significantly lower median as regards time to drink the total volume. The final intake volume was significantly larger from the cup. A statistically significant difference was found in the oral spillage of liquid, which was notably higher in the cup trial. Despite the presence of residue in the valleculae and pyriform sinuses, in neither trial was there penetration or aspiration of liquid. The straw has a favorable influence on the quality of the sequential swallowing of liquid in regard to bolus containment within the oral cavity, which was better with that utensil. The cup provides a higher final volume in a shorter time for intake but there is more fluid spillage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several research methods for the investigation of swallowing focus on the observation of a single bolus. Studies on sequential swallowing, in turn, have gained ground in the past few years; still, some of their findings cannot be compared because of a range of factors: the variable number of participants, the volume offered, intake instructions, tests performed for evaluation of swallowing, and the type of utensils used [1]. Studies on both sequential swallowing [2] and single swallowing [3] claim that the patterns found in single swallowing may not be replicated with sequential swallowing, especially with liquid. Considering not only that people typically ingest liquids in sequential swallows in varied, self-regulated amounts [4], but also the difficulty of taking in liquid in a way that emulates, as perfectly as possible, the natural method of swallowing, it is important to assess the deglutition of larger volumes to simulate the natural method of intake [3].
Elderly individuals without dysphagia complaints may experience greater difficulty performing sequential swallowing [5]; other subjects, on the other hand, may find it easier to perform sequential swallowing than to swallow isolated boluses because of the specific mechanical and sensomotor properties of sequential swallowing [6]. As swallows in a sequence occur during a meal, elderly individuals, however healthy, are exposed to a higher risk of airway invasion [5]. Thus, subjects at risk for aspiration must split the volume taken in into a series of single-bolus swallows [7].
In sequential swallowing, both healthy and dysphagic individuals show a few episodes of laryngeal penetration, with efficient clearance, and this is considered normal in this type of swallowing [6, 8].
The sip volume is influenced by a number of parameters such as subject age and type of utensil used. One study [9] showed that larger sip volumes were obtained in adults from the rim of the cup than the straw. It also showed that single-sip volume from a cup for elderly individuals is equivalent to that of adults from a straw. Also, the volume of one-sip swallows is larger than that taken by the subject when oriented to take sequential swallows [4, 9].
The type of utensil used influences the onset time of the swallowing events [10] and the speed [6] of swallowing, as well as the bolus acceptance/extraction [11]. The straw facilitates hydration since it minimizes oral spillage [12], and it is widely used by elderly individuals to drink liquids [13]. Some studies reported that many elderly individuals find it easier to drink through a straw [14]. With respect to pharyngolaryngeal findings, one study [15] showed that straw delivery yielded longer bolus dwell times, but there was no significant relationship between aspiration and bolus dwell time at either the valleculae or the pyriform sinuses. Other studies [2, 16] do not recommend the use of a straw for patients with respiratory diseases since it demands longer apnea, which exposes the subject to a higher risk of aspiration. One study [2] concluded that a significant number of elderly individuals experience, to some extent, airway invasion when using a straw; hence, with age, especially over 70, the ability to keep the airway protected and to perform supraglottal clearance is altered.
An integrative review [1] of scientific articles on the sequential swallowing of liquids by adult and elderly individuals did not find any consensus or evidence in the literature regarding the influence on sequential swallowing by the utensil used. That review found a small number of studies that reported on the safety of offering either healthy or dysphagic elderly individuals a straw for liquid intake.
The present research describes the characteristics of sequential swallowing of liquid through a straw and from the rim of a cup in healthy elderly individuals, based on clinical assessment and on fiberoptic endoscopic evaluation of swallowing (FEES). It aimed to check for differences in the quality of swallowing depending on the utensil used and sought to reach a better understanding of the possible interference caused by the utensil used in order to contribute to the decision regarding the use of a straw and recommending its use to elderly individuals.
Method
Participants
The present study was assessed and approved by the Research Ethics Committee of the Brazilian Air Force Gerontological Home Brigadeiro Eduardo Gomes (CEP/CGABEG). Written informed consent was provided by all volunteers. The research was carried out at the Otolaryngology Department of the Brazilian Air Force Central Hospital.
Initially, 50 elderly (≥60 years) consecutive outpatients who attended the coexistence center of the Geriatric and Gerontological Unit of the hospital were recruited by the healthcare team to participate in the study. However, only individuals who did not met the exclusion criteria were included. The exclusion criteria were opposition to recording of the procedures; history of neurological disorders such as stroke, Parkinson’s disease, and Alzheimer’s disease; respiratory diseases; uncontrolled gastrointestinal disorders; former surgeries with resection of any structures of the stomatognathic system; head and neck cancer; dysphagia complaints; significant cognitive impairment; and alterations in the orofacial structure or mobility that interfere with either deglutition or suction from a straw during the filmed clinical screening. Thirty elderly (≥60 years) consecutive healthy individuals passed the exclusion criteria and were included in the study. They were unpaired for gender (24 females) and age (mean age = 72.8 ± 7 years, range = 62–87 years).
Procedures
Participants were evaluated for swallowing by both an otolaryngologist and the researcher (speech-language pathologist), as in a previous study [16]. Participants had been through a 2-h total fast when assessed. Although not standardized in FEES protocols, such orientation was meant to avoid the risk of rejection of the two 100-ml boluses of water. The assessment was filmed and the FEES was recorded on a DVD.
Each participant was seated upright. A Karl Storz flexible optical fiber for larynx examination, with a Storz halogen light source and a Swift Cam camera attached to an adaptor for a Karl Storz model 8020 endoscope, was inserted into the most patent nostril, without any topical anesthetic so as not to interfere with the pharyngolaryngeal sensitivity. The device was moved forward through the nasopharynx toward the oropharynx, while the base of the tongue, the valleculae, the pyriform sinuses, the lateral and posterior walls of the pharynx, and the vocal folds were observed both at rest and during phonation.
Swallowing was assessed with a fiberoptic laryngoscope at a high position, above the epiglottis, before and during deglutition. Only after swallowing the entire bolus was the fiberoptic laryngoscope moved forward to a lower position, just above the vocal folds, in order to check for pharyngeal residue, penetration or aspiration, as suggested in the literature [17, 18].
In agreement with other studies on sequential swallowing [14, 18, 19], we chose to use only water. Two volumes of 100 ml at room temperature, dyed with blue food dye, were offered to participants in two trials: from the rim of the cup and through a plastic straw 0.5 cm in diameter and 21 cm in length. Both volumes were offered in a 200-ml disposable plastic cup. Each participant held the cup alone or the cup with a straw and received the following instruction: “You will try to drink the whole content of the cup, without stopping.” This instruction was meant to obtain a sequential intake, as proposed in previous studies [8, 20]. No further instructions about the method of swallowing were given, which made it possible to analyze each subject’s standard swallowing behavior of such a volume as well as the potential interference of the utensil.
Following the researcher’s instruction, half of the participants first drank the water from the rim of the cup, then through the straw; whereas the other half took it first through the straw and then straight from the cup. This was done to avoid the training effect or fatigue.
Analysis of Swallowing Clinical Assessment
The quantitative aspects observed for the sequential swallowing using each utensil were total swallowed volume (the residual volume was measured with a 1-ml-scale syringe) and time to swallow the volume (measured with a stopwatch). The stopwatch was started when the water touched the participant’s lips and was stopped when the utensil was handed to the researcher, regardless of the ingested volume.
The qualitative aspects observed were efficient or delayed intake onset upon command, oral spillage of liquid, and lip sealing. In addition, the following security aspects related to the mechanism of swallowing were checked: wet voice after swallowing the total volume and cough or choke before, during, or after swallowing. Finally, whether the participant took pauses to drink the volume or swallowed it uninterrupted was also recorded.
Analysis During FEES
Both trials (cup and straw) checked whether there was effective deglutition, with total clearance of the pharynx and larynx, or there was residue in the area. The observed FEES assessment parameters were residue in the valleculae and in the pyriform sinuses (both after swallowing), laryngeal penetration before and after swallowing, aspiration before and after swallowing, and cough reflex or silent aspiration. Airway invasion during the swallow could not be determined since it is not possible to visualize the pharyngeal phase of swallowing with the FEES due the closure of pharyngolaryngeal muscles during swallowing, which leads to the whiteout effect [21]. Although some recent studies used different scales of pharyngeal residue severity [19, 22, 23], the only rating scale used in this study was the validated penetration–aspiration scale [24]. After swallowing the total volume, pharyngeal residue was classified as either present or absent so as to simplify the data since there is not a validated or widely accepted scale for residue.
To carry out a categorical analysis with respect to age, using mean age, subjects were placed in one of two groups: GA, ≤72 years of age, and GB, >72 years of age.
Some subjects took pauses during the sequential swallowing of the assigned volume, with either the cup or the straw. Participants were then regrouped based on the presence or absence of pauses with each utensil in order to check whether those pauses interfered with the clinical assessment and FEES findings. These new groups were GC, cup without pauses; GD, cup with pauses; GE, straw without pauses; and GF, straw with pauses.
The exam was interrupted in case of evident signs of aspiration, e.g., excessive liquid in the valleculae, in the pyriform sinuses, in the vestibule, or in the glottic portion, without clearance of the stasis content after three important swallowing movements, coughing, or choking.
Statistical Analysis
The descriptive analysis was based on the following summary measures: frequency (n) and percentage (%) for qualitative data, and median, minimum, and maximum for quantitative data.
The nonparametric McNemar test and the Wilcoxon signed-rank test were used to check whether there were significant findings on the FEES and clinical assessment variables for the consumption from the cup versus with the straw. Fisher’s exact test was used to verify the effect on some variables of pauses that occurred during intake. The Mann–Whitney test was used to compare the time of intake of the two age groups, as well as the presence or absence of pauses during the intake.
Statistical analyses was performed using SAS ver. 6.11 (SAS Institute, Inc., Cary, NC). The adopted significance for the application of the statistical tests was 5 % (0.05).
Results
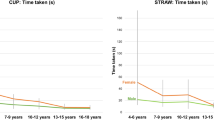
Frequency (n) and percentage (%) of clinical assessment and FEES variables, with a statistical analysis (p value), are given in Tables 1 and 2, respectively, categorized according to the utensil (cup or straw). Time of intake [in seconds (s)] and swallowed volume [in milliliters (ml)] are expressed as the median (minimum–maximum). No statistically significant differences were found in the clinical assessment in regard to the intake method (with or without pauses), efficiency of intake onset, lip sealing, and the presence of cough. Statistically significant differences were observed for oral spillage, time of intake, and total volume, according to the utensil. Data showed a greater occurrence of oral spillage with the cup (p = 0.002), a longer time of intake with the straw (p = 0.0001), and a larger total volume taken in with the cup (p = 0.020).
Of the 11 participants that had oral spillage with the cup, 45.5 % had drunk first from the rim of the cup and 54.5 % from the straw, which shows that the order of the utensil used was not relevant for this item.
Results in Table 2 show that there are no statistically significant differences between the two utensils. Penetration or aspiration was observed with neither utensil. On the other hand, post-swallowing residue in the valleculae and the pyriform sinuses was observed with both utensils. However, as the percentage of residue in the valleculae (≥60 %) was higher than in the pyriform sinuses (<20 %), we present only the data regarding the influence of pauses on the residue in the valleculae according to utensil.
Time of intake according to age [GA, ≤72 years (n = 16), and GB, >72 years (n = 14)] is given in Table 3. Statistically significant difference between ages was found only with the straw.
With respect to the effect of pauses on the variables in the clinical assessment (oral spillage and time of intake) and FEES (post-swallowing residues in valleculae), the results show that there were no statistically significant differences in GC [cup without pauses (n = 25)] and GD [cup with pauses (n = 5)] (Table 4) and GE [straw without pauses (n = 20)] (Table 5) with respect to the variables studied. However, GF [straw with pauses (n = 10)] (Table 5) showed a statistically significant difference with longer time of intake.
Discussion
No significant differences in total intake volume were found between the utensils. Those participants who did not swallow the entire volume did so for both the cup and the straw, meaning that the type of utensil did not influence the total intake volume. None of the studies reviewed reported a similar finding; therefore, it is not possible to establish a comparison.
Even though subjects were instructed to swallow the entire volume without stopping, those who paused were not excluded from the analysis, as done in previous studies [20, 25]. Similarly, another study [26] did not exclude subjects who had failed to complete the test, and total intake volume was calculated based on the volume left in the beaker. This procedure differs from that of one study [7] that excluded from the analysis those subjects who failed to strictly follow the instructions. On the other hand, other studies [4, 26] did not state whether subjects who had paused during intake were excluded from the analysis.
There were no differences between the utensils with respect to intake method, i.e., with pauses or continuous swallowing of the whole volume. This seems to corroborate the findings in the literature, which state that the presence of pauses in sequential swallowing in elderly individuals is expected, confirming the variable nature of this type of deglutition. This was discussed in one study [27] regardless of the utensil, and pointed to in another study [25] with both those utensils.
Bolus containment within the oral cavity was more effective with the straw, in agreement with a previous study [28] in which the straw was an adaptive device to decrease labial leakage. Oral spillage of liquid was observed solely during intake from the cup, with a statistically significant difference when compared to the straw. This finding agrees with that of a previous study [12], which reported that the straw not only promotes increased muscle activity compared to the maximal voluntary lip sealing pressure, but it also decreases oral spillage in subjects with reduced lip muscle strength. Besides, swallowing from the rim of the cup demands accurate control to keep the lips in contact with the utensil [29], whereas the straw has the liquid go straight to the rear of the oral cavity [14], which might explain the difference between both utensils concerning oral spillage observed in the present study.
Median time of intake of the total volume from the cup was 12 s, which corresponds to 8.3 ml/s for the 100-ml volume. This rate was lower than the 13.6 ml/s found for elderly subjects with the water swallowing test [25], and the minimum average volume per swallow of 10.6 ml/s in elderly individuals found in another study [26]. This difference in intake can be explained by the different instructions given: in the aforementioned studies, subjects were supposed to swallow the whole volume as quickly as possible.
Median time of intake of the total volume with the straw was 17 s, which was significantly longer compared to the cup. With respect to time of intake from the straw, we extrapolated the data obtained in an earlier study [4] and found that subjects would swallow the 100-ml volume in about 9 s, a shorter time than that found in our research. However, that study was performed with young subjects and with the straws of different length than those used in our study, though they had the same diameter. Thus, it would only be possible to compare the time of intake from a straw in the present study to that found in other studies if the utensil had the same dimensions.
The total intake volume from the cup was larger than that through the straw, which is a finding different from the literature [9], which showed no difference between the utensils for elderly individuals. The total intake volumes for young adults in the aforementioned study, however, are comparable to those of the present study, as both groups swallowed a larger volume from the cup. However, it must be said that the studies used a different volume to analyze: the earlier study [9] used sip volume and the present study used total volume. Still, the total intake volume variation with the cup was less frequent than with the straw, in agreement with a previous study [4] that showed great variability in the biomechanics of sequential swallowing with the straw.
Participants showed residue in the valleculae and in the pyriform sinuses after deglutition with both utensils. That is in agreement with an earlier study [22] which also noted that the utensil does not influence the presence of pharyngeal residue. The present research confirms studies that observed pharyngeal residue in an elderly group with no dysphagia complaints [19, 30, 31].
While some studies found that healthy elderly adults have instances of penetration and aspiration during assessment [2, 32], or a thin trace of penetration with immediate expulsion [6], neither laryngeal penetration nor aspiration after a series of swallows was observed with either utensil. All of our subjects scored 1 in the P-A scale, in agreement with previous studies which found that the mean score in subjects with deficits in oral and pharyngeal phases did not exceed 2 [8], and 96 % of individuals scored 1 [27]. Although a few studies have reported some degree of invasion of the lower airway despite the lower positioning of the content at the beginning of the pharyngeal phase of swallowing [33], whereas other studies have described the absence of tracheal aspiration in sequential swallowing [4], the present research could not determine airway invasion because of the limitation of FEES. The absence of penetration and aspiration in this study can also be attributed to the whiteout effect [21], which may have caused underestimation of these phenomena. The lack of influence of the utensil on penetration or aspiration agrees with one former study [32] and disagrees with another [22], which demonstrates that there is no consensus regarding the influence of the utensil in airway invasion.
This research used water as the trial liquid for a number of reasons. Not only can the volume and taste of liquid alter the temporal characteristics of a swallow [9], it can also be assumed that 100 ml of milk, for example, could produce sequential swallows that would differ from those of water. Besides, the use of various types of milk have been reported in the literature: yogurt [23], refrigerated [19, 32], and skim [34]. Some studies have shown that there is more residue, penetration, or aspiration with milk than with water [18, 19, 23], since milk reflects light from the endoscope better than water [19, 34]. Others did not find any difference between the liquids [32]. The use of water as a thin liquid can underestimate residue and aspiration [19].
No correlation was found between age and time of intake from the cup, which differs from one study which reported that the amount sipped from the rim of the cup decreases and the time of intake increases with age [3]. With the straw, however, there were statistically significant differences between GA and GB, possibly indicating that time of intake with this utensil increases with age. The reviewed literature did not show any similar data; however, one study [29] observed that ingestion of liquid, either from a cup or through a straw, was better in subjects >70 years old than in those between 60 and 69 years old, contrasting with what was found and described here.
Correlation of pauses with the variables in clinical assessment (oral spillage and time of intake) and FEES (post-swallowing residue in valleculae) showed that the presence of pauses with the cup did not interfere with the time of intake or with oral spillage (observed only with the cup). The reviewed literature did not show any similar data about oral spillage of liquid. The presence of pauses with the straw, on the other hand, increased the time of intake, in agreement with two earlier studies. One study [25] found more pauses during sequential swallowing from the straw than from the cup, and another [20] advocated that pauses to breathe between sequential swallows from a straw probably increase total time of swallowing.
In analyzing the correlation of pauses with the cup and the straw with post-swallowing residue in the valleculae, this study agrees with an earlier study [22] that also found pharyngeal retention, though in single swallows, without influence of the utensil.
This study suffers from a few possible limitations. There was the lack of gender parity, which limited our ability to check the effect of this variable. Another was the use of only one type of thin liquid. And the main limitation was the impossibility of doing a blinded interpretation due to the time constraints of the daily schedule of other staff otolaryngologists, which led to a nonblinded analysis during the exams, even though it is well known that multiple raters reduce the effect of random rating errors [23]. This study would benefit in terms of reliability if data could be analyzed by multiple raters.
Conclusion
The main characteristics of sequential swallowing of liquids in elderly healthy individuals that we found were the presence of lip sealing with the utensil, intake with and without pauses, and residue in the valleculae and pyriform sinuses without penetration and/or aspiration of liquid regardless of the utensil.
The cup provides a larger total volume in a shorter time of intake, yet it causes oral spillage of liquid. The straw seems to influence favorably the quality of sequential swallowing with respect to bolus containment within the oral cavity, which was better with that utensil.
Considering the increasing number of elderly people becoming more dependent, which includes needing help with feeding, the present findings agree with the recommendation to healthy elderly individuals of using a straw, as use of this utensil showed a lower occurrence of oral spillage and therefore is a benefit to the oral phase of swallowing. Further research with a larger number of participants, including dysphagic subjects, is needed to investigate whether similar behavior is found with those utensils.
References
Veiga HP, Bianchini EM. Characteristics of sequential swallowing of liquids in young and elderly adults: an integrative review. J Soc Bras Fonoaudiol. 2012;24(4):401–8. doi:10.1590/S2179-64912012000400019.
Daniels SK, Corey DM, Hadskey LD, Legendre C, Priestly DH, Rosenbek JC, et al. Mechanism of sequential swallowing during straw drinking in healthy young and older adults. J Speech Lang Hear Res. 2004;47:33–45.
Bennett JW, Van Lieshout PH, Pelletier CA, Steele CM. Sip-sizing behaviors in natural drinking conditions compared to instructed experimental conditions. Dysphagia. 2009;24(2):152–8.
Daniels SK, Foundas AL. Swallowing physiology of sequential straw drinking. Dysphagia. 2001;16(3):176–82.
Robbins J, Coyle J, Rosenbek J, Roecker E, Wood J. Differentiation of normal and abnormal airway protection during swallowing using the penetration–aspiration scale. Dysphagia. 1999;14(4):228–32.
Chi-Fishman G, Sonies B. Motor strategy in rapid sequential swallowing: new insights. J Speech Lang Hear Res. 2000;43:1481–92.
Preiksaitis HG, Mills CA. Coordination of breathing and swallowing: effects of bolus consistency and presentation in normal adults. J Appl Physiol. 1996;81(4):1707–14.
Murguia M, Corey DM, Daniels S. Comparison of sequential swallowing in patients with acute stroke and healthy adults. Arch Phys Med Rehabil. 2009;90:1860–5.
Lawless HT, Bender S, Oman C, Pelletier C. Gender, age, vessel size, cup vs. straw sipping, and sequence effects on sip volume. Dysphagia. 2003;18(3):196–202.
Martin-Harris B, Brodsky MB, Michel Y, Lee FS, Walters B. Delayed initiation of the pharyngeal swallow: normal variability in adult swallows. J Speech Lang Hear Res. 2007;50:585–94.
Steele CM, Van Lieshout PH. Influence of bolus consistency on lingual behaviors in sequential swallowing. Dysphagia. 2004;19(3):192–206.
Murray KA, Larson CR, Logemann JA. Electromyographic response of the labial muscles during normal liquid swallows using a spoon, a straw, and a cup. Dysphagia. 1998;13(3):160–6.
Hammond CAS, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1):154S–68S.
Cichero J, Halley S. Variations of the normal swallow. In: Cichero J, Murdoch B, editors. Dysphagia: foundation, theory and practice. Chichester: Wiley; 2006. p. 47–57.
Butler SG, Maslan J, Stuart A, Leng X, Wilhelm E, Rees C, Williamson J, Kritchevsky SB. Factors influencing bolus dwell times in healthy older adults assessed endoscopically. Laryngoscope. 2011;121(12):2526–34.
Martin BJ, Logemann JA, Shaker R, Dodds WJ. Coordination between respiration and swallowing: respiratory phase relationships and temporal integration. J Appl Physiol. 1994;76(2):714–23.
Seidl RO, Nusser-Müller-Busch R, Westhofen M, Ernst A. Oropharyngeal findings of endoscopic examination in swallowing disorders of neurological origin. Eur Arch Otorhinolaryngol. 2008;265(8):963–70.
Butler SG, Stuart A, Leng X, Wilhelm E, Rees C, Williamson J, Kritchevsky SB. The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol A Biol Sci Med Sci. 2011;66A(4):452–8.
Butler SG, Stuart A, Kemp S. Flexible endoscopic evaluation of swallowing in healthy young and older adults. Ann Otol Rhinol Laryngol. 2009;118(2):99–106.
Lederle A, Hoit JD, Barkmeier-Kraemer J. Effects of sequential swallowing on drive to breathe in young, healthy adults. Dysphagia. 2012;27(2):221–7.
Nacci A, Ursino F, La Vela R, Matteucci F, Mallardi V, Fattori B. Fiberoptic endoscopic evaluation of swallowing (FEES): proposal for informed consent. Acta Otorhinolaryngol Ital. 2008;28(4):206–11.
Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia. 2001;16(2):119–22.
Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006;31(5):425–32.
Rosenbek JC, Robbins J, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11(2):93–8.
Hirst LJ, Ford GA, Gibson GJ, Wilson JA. Swallow-induced alterations in breathing in normal older people. Dysphagia. 2002;17(2):152–61.
Hughes TA, Wiles CM. Clinical measurement of swallowing in health and in neurogenic dysphagia. QJM. 1996;89(2):109–16.
Dozier TS, Brodsky MB, Michel Y, Walters BC, Martin-Harris B. Coordination of swallowing and respiration in normal sequential cup swallows. Laryngoscope. 2006;116:1489–93.
Ashley J, Duggan M, Sutcliffe N. Speech, language and swallowing disorders in the older adult. Clin Geriatr Med. 2006;22(2):291–310.
Fucile S, Wright PM, Chan I, Yee S, Langlais ME, Gisel EG. Functional oral-motor skills: do they change with age? Dysphagia. 1998;13(4):195–201.
Yoshikawa M, Yoshida M, Nagasaki T, Tanimoto K, Tsuga K, Akagawa Y. Influence of aging and denture use on liquid swallowing in healthy dentulous and edentulous older people. J Am Geriatr Soc. 2006;54(3):444–9.
Humbert IA, Fitzgerald ME, McLaren DG, Johnson S, Porcaro KK, Hind J, Robbins J. Neurophysiology of swallowing: effects of age and bolus type. Neuroimage. 2009;44(3):982–91.
Butler SG, Stuart A, Markley L, Rees C. Penetration and aspiration in healthy older adults as assessed during endoscopic evaluation of swallowing. Ann Otol Rhinol Laryngol. 2009;118(3):190–8.
Stephen JR, Taves DH, Smith RC, Martin RE. Bolus location at the initiation of the pharyngeal stage of swallowing in healthy older adults. Dysphagia. 2005;20(4):266–72.
Leder SB, Acton LM, Lisitano HL, Murray JT. Fiberoptic endoscopic evaluation of swallowing (FEES) with and without blue-dyed food. Dysphagia. 2005;20(2):157–62.
Conflict of interest
The authors claim no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veiga, H.P., Fonseca, H.V. & Bianchini, E.M.G. Sequential Swallowing of Liquid in Elderly Adults: Cup or Straw?. Dysphagia 29, 249–255 (2014). https://doi.org/10.1007/s00455-013-9503-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9503-8