Abstract
The purpose of this study was to determine whether attentional resources are involved in swallowing in persons with idiopathic Parkinson’s disease, and if so, in which phase(s) of swallowing. The approach involved a dual-task, reaction time (RT) paradigm using ten participants with Parkinson’s disease. Single-task baseline measures were obtained for durations of the anticipatory phase and oropharyngeal phase of swallowing and RTs were obtained for nonword auditory stimuli. A dual-task then required participants to swallow 5 ml of water from an 8-oz. cup while listening for a target nonword presented auditorily during the anticipatory or oropharyngeal phase. Target stimuli were randomized across baseline and dual-task trials. Durations of the anticipatory and oropharyngeal phases of swallowing and RTs during baseline and dual-task trials were determined. Results showed a nonsignificant change in speed of completion for both the anticipatory phase and the oropharyngeal phase of swallowing during dual-task trials. However, there was a statistically significant increase in RT during the anticipatory phase during the dual-task condition. RT during the oropharyngeal phase remained unaffected. Given a need for additional research using more complex competing tasks, these data on attention are consistent with earlier claims of an automatic, nonresource-demanding, oropharyngeal swallowing mechanism that is preserved for persons with early-to-mid-stage Parkinson’s disease. Clinical implications of these data suggest that disruptive environmental stimuli to individuals with early-to-mid-stage Parkinson’s disease may alter feeding but have little effect on the oropharyngeal swallow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Addressed in a companion article [1] is the argument that swallowing has historically been regarded in the literature as “reflexive,” “vegetative,” and “automatic.” There are, however, aspects of swallowing, including the initiation of the oropharyngeal swallow, that suggest that it may not be as automatic as commonly believed [2–5]. Swallowing may require attentional resources that are shared with other relevant cognitive and motor behaviors. One difference between phases of swallowing (i.e., oral phase, pharyngeal phase, and esophageal phase) may be the change of demand on cognitive resources. This area of study has not been well explored, and much of what is known about attention has been addressed in neuroimaging studies that attempt to localize cortical activities rather than describe changes in behavior associated with that activity.
Numerous neuroimaging studies identify cortical activation in regions associated with attention [2, 4, 6–11]; however, we are aware of only one study that describes behaviorally the demands of cognitive tasks on swallowing, i.e., the functional changes of swallowing relative to cognitive demands [12]. This study suggested bilateral hemisphere cerebral support for swallowing and association of the left hemisphere’s motor and language systems with swallowing behavior. However, it remains unclear whether attentional resources are influential on any or all aspects of swallowing.
Leopold and Kagel [13, 14] proposed an “anticipatory phase” of ingestion, although the aforementioned phases of swallowing were also regarded as ingestion. To simplify, our work operationally defines the anticipatory phase as one adjacent, and therefore related, to swallowing that temporally precedes the oral preparatory and oral propulsive phases. The anticipatory phase involves all preparation and introduction of all nutritional materials to the oral cavity (e.g., selection of bolus size and type and placement from hand to mouth). During the oral preparatory phase of swallowing, the bolus is actively manipulated in the mouth and masticated; the oral propulsive phase moves the bolus posteriorly to the pharynx. All three of these phases require attention and effort for planning and organized movement, making them more vulnerable to interference with increased demand on attentional resources. Because these phases are a consequence of cortical and basal ganglia patterned activity, they reside outside the central pattern generator for swallowing [15]. The pharyngeal and esophageal phases of swallowing seem less likely to be subjected to attentional influences due to their non-volitionally controlled nature. The role of attention during swallowing has not been explored in patients, specifically those with neuromotor or neurocognitive disturbances.
Describing changes in behavior with increased cognitive demands is one method for exploring the role of attention in swallowing. Although it might appear that motor disorders are not related to cognitive impairment, motor control is a cognitive process. By attempting to separate motor processes from any concomitant or underlying cognitive deficit, the impact of cognitive demands on the motor system will emerge. One approach to determine the impact of attention on swallowing would be to assess swallowing in those who may have cognitive (broadly), attentional (specifically), and/or sensorimotor constraints, especially those that may affect swallowing. In the latter case, cognitive requirements of swallowing might be increased and there would be greater likelihood of seeing increased response latencies to secondary stimuli. In light of these considerations, the present investigation evaluated a possible role of attention in swallowing in individuals with Parkinson’s disease.
Parkinson’s disease (PD) is a progressive, neurological impairment of the sensorimotor system. Classically, it has been characterized by motor deficits with “the senses and intellects being uninjured” [16, p. 1]. However, in recent years it has been determined that persons with PD also have cognitive declines, which challenge the sensorimotor system even if such declines do not surface as frank dementia or the sensorimotor disturbances are not manifest. If the swallowing system in these patients were taxed by cognitive deficits, sensorimotor deficits, or both, it would seem that adding experimental demands on attention before or during swallowing might exaggerate current deficits and/or reveal additional deficits. Classic models of attention, which view attention as a limited cognitive resource, as sharable across tasks, and as differentially able to be allocated, are consistent with this prediction [17–22]. The capacity model has been used to explain reaction time (RT) effects in dual-task paradigms [17]. Capacity-sharing theory suggests that simultaneous tasks share a limited pool of available mental resources. One task requiring a great amount of mental resources will leave limited resources for the processing of a second task, and performance on that second task will be degraded, assuming the two tasks are competing for the same resources. The present study explores whether sensorimotor deficits are affected by increased demands on attention, and if so, in which phases of the swallow they occur. The findings of this study will be relevant for dysphagia treatments in individuals with either or both cognitive and motor dysfunction.
Methods
Demographics
This study was submitted for review and was approved by the Institutional Review Board of the participating institution. Participants with PD were recruited with symptoms consistent with minimal disability in the early-to-middle stages (Hoehn and Yahr stages 1, 2, and 3) of the disease [23], according to the criteria set forth by the United Kingdom Parkinson’s Disease Society’s brain bank diagnostic criteria for PD [24]. Neither dosing nor scheduling of medications was altered for the experiment. Participants verbally confirmed stability on their current medication regimen prior to administration of the experimental protocol. Participants were instructed to be in the “on” phase of their medication regimen during experimental procedures. Appointment times were scheduled to accommodate for this experimental control.
Screening
All participants had their hearing in both ears screened with pure tone stimuli through headphones at 30 dB HL for 500 Hz and 1, 2, and 4 kHz in a distraction-free room that was not sound-treated. The stimuli were presented at 85 dB SPL in free field as measured by a portable sound-level meter with an A-weighted scale at ear level and a distance of 1 m from the speakers. All sound calibration took place with continuous, prerecorded white noise normalized based on 100% peak level.
Participants were screened for cognitive impairment using COGNISTAT (The Northern California Neurobehavioral Group, Inc., 1995) [25]. Participants who scored with at least two impaired ability domains on COGNISTAT were excluded [26].
Participants were screened for depression using the Beck Depression Inventory (BDI) [27, 28] because of the known effects of reduced RTs [29] of those with this condition. Participants identified with depression were not excluded from the investigation but were considered as possible outliers a priori for statistical analyses.
Experimental Design
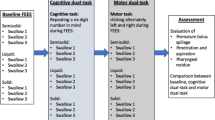
As stated in the previous article [1], this study used a within-subjects design. Auditory stimuli presented for single- and dual-task discrimination and the anticipatory and oropharyngeal phases of swallowing served as independent variables. Durations of the anticipatory and oropharyngeal phases of swallowing and RT were the dependent variables.
Procedures
Procedures are described in detail in the companion article [1]. Briefly, the testing area was split between a table setup and a floor setup. Participants were seated at a table containing a hand-lift sensor that was flush with the front edge of the table, a cup-lift sensor that was 12 in. from the front of the table and on which sat a disposable drinking cup with a cup module, and a 17-in. computer monitor approximately 18 in. from the participant. Two satellite computer speakers connected to the data computer’s audio output were placed on either side of the computer monitor at a distance of approximately 36 in. from the participant’s ear.
On the floor in front of the participant, and out of his/her view, were a foot sensor and a foot pedal used to measure RT. Each was placed in front of the participant’s dominant lower extremity. With the participant’s dominant lower extremity at a 90° flexion, the foot sensor was placed under the participant’s foot. The front edge of the foot pedal was placed 6 in. from the tip of the participant’s shoe. Both the foot sensor and the foot pedal were securely taped to the floor.
The oropharyngeal swallow was marked by surface electromyography (sEMG) using the KayPENTAX digital swallowing workstation™ (model 7100, KayPENTAX, Lincoln Park, NJ) and the Workstation’s Swallowing Signals Lab (model 7120). After the participant’s submandibular area was prepared with an alcohol swab, electrode gel was placed on the electrode surfaces of a self-adhering patch containing three electrode disks. The prepared patch then was placed over the digastric-mylohyoid-geniohyoid muscle complex.
Two experimental conditions were used in this study: baseline and dual-task. The baseline condition consisted of two sets of 19 trials each: (1) nonword discrimination trials and (2) swallowing trials. The dual-task condition consisted of one set of 19 trials that combined the baseline’s nonword discrimination and swallowing trials. In summary, a total of three sets of 19 trials each (i.e., 57 trials total) was completed by each participant. The initial three trials for each trial condition (i.e., baseline nonword discrimination trials, baseline swallowing trials, and dual-task) were expected to abate learning for the task [30] and were planned to be eliminated from analyses. Elimination of these nine trials left 16 trials for each condition to be analyzed for each participant. The two baseline (single-task) conditions were counterbalanced across participants; however, baseline trials were presented only prior to the dual-task trials. This order was necessary to reduce the any learning effect that might be present for the dual-task condition.
Auditory Stimuli
Auditory stimuli were created as two lists of non-words in the context of consonant–vowel–consonant (CVC), with the same lead (CV−) but different codas (–C). Each word, created by the principal investigator (PI), was phonotactically legal and monosyllabic. Each list comprised 11 distracter stimuli and one target stimulus, counterbalanced across trials and between participants.
Baseline (Single-Task) Trials
During the baseline swallow trials, each participant moved his/her hand from the hand sensor to reach for the cup containing 5 ml of water after a visual “go” cue from the computer was presented. After grasping the cup and bringing it to his/her mouth, the participant swallowed the water. During the baseline RT (nonword discrimination) trials, non-words were presented to the participants with the instruction to tap the foot pedal with their dominant foot as quickly as possible when the target word was heard, ignoring nontarget words and keeping his/her foot on the floor. The same target word was randomly presented four times during the 16 analyzed trials. Distracter words were randomly presented across the 12 remaining trials. A similar paradigm was used in prior studies [31, 32].
Dual-Task Trials
The dual task required a participant to tap the foot pedal as quickly as possible with his/her dominant foot when the target nonword was heard. Targets were presented randomly as the participant brought the cup of water to his/her mouth and swallowed the water. Four target stimuli were presented, two during the anticipatory phase of swallowing and two during the oropharyngeal phase of swallowing. These target trials were manually presented by the PI (MB) using the data computer. Presentation of the stimuli was randomized within condition and between participants.
Measures and Instrumentation
Measures consisted of time points during each of the baseline and dual-task trials. A maximum of eight additional time points were measured. These included (1) onset of the experimental trials, (2) onset of the random delay following a 3-s visual countdown, (3) onset of a green “go” signal presented on the computer monitor, (4) the participant’s hand being lifted from the hand sensor on the table (onset of the anticipatory phase), (5) the cup being lifted from its sensor, (6) the tilt circuit in the recess of the cup triggering the critical angle (i.e., the angle between the side of the cup facing the table when it was tilted immediately before 5 ml of water flowed over the rim and the table surface (completion of the anticipatory phase and onset of the oropharyngeal swallow), (7) the auditory stimulus, either target or distracter nonword, and (8) foot pedal depression. All of the aforementioned measures were electronically recorded. Offset of the sEMG signal was manually determined using the Workstation’s software.
A notebook computer (data computer), controlled by the PI, was responsible for the management of a timer, commencement cue, presentation of auditory stimuli, and real-time data acquisition for this study. Use of the Workstation with a custom interface box and the Workstation’s Swallowing Signals Lab allowed for all data presentation and acquisition. The experiment used Presentation® software ver. 0.50 (Neurobehavioral Systems, Inc., Albany, CA), programmed to allow for simultaneous experimenter-delivered stimuli, data acquisition, and voltage pulse generation captured by the Workstation. The sampling rate was 1,000 Hz for all signals.
Data Reduction
After all data were collected, the database was inspected. A total of 57 trials were completed for each participant—19 trials for each of three trial types (i.e., baseline swallowing, baseline RT, and dual-task). The first three trials were immediately removed from all analyses to control for any practice effects [30]. Box plots and stem and leaf plots were used to determine outliers. Based on group data, outliers greater than two SDs were removed from the data set for final analyses.
All trials were automatically coded as good, bad, or void based on programming code associated with each of the sensor signals and their consequent data recording. Good trials were those in which all sensors were successfully triggered and the sEMG data were successfully recorded. Bad trials were trials in which the participant made an error (i.e., did not react to a target trial, or anticipated the response to a target with an RT less than 100 ms). Voided trials were those in which at least one electronic sensor was not triggered or the sEMG signal was not recorded. No feedback was provided to the participant at any time; however, immediate feedback for the trial’s status type was presented to the PI following each trial. Bad and void trials were immediately repeated without informing the participant.
Statistical Analysis
Intrarater reliability for sEMG offset was calculated by selecting a random sample of 25% of the total number of sEMG tracings from each participant. A repeated-measures analysis of variance (RMANOVA) was used to determine differences between trials within participants and between conditions controlling for trials. Mauchly’s test of sphericity was used with all analyses, applying the Greenhouse–Geisser correction when applicable. Significance was set to α < 0.05 for all comparisons. Statistics were computed using SPSS v16.0 for Windows (rel. 16.0.2) (SPSS, Inc., Chicago, IL).
Results
Demographics
Ten individuals with PD participated in the study. All ten participants were Caucasian, with one Hispanic, and nine non-Hispanic. Within this sample of seven males and three females, all participants were right-handed except for one male. The average age for was 61.8 years (SD = 10.1 years, range = 45–73 years).
The motor subsets of the Unified Parkinson’s disease rating scale (UPDRS) were used to describe motoric function and stage each participant. Participants were evaluated between 30 and 45 min following their dosage of medication (i.e., during the “on” phase of their medication regimen) by a nurse practitioner. The ten participants recruited for this study ranged between stage 1 and stage 3 of the disease [23]. Individually, there was one participant who was evaluated as being in stage 1, one participant in stage 1.5, five participants in stage 2, and three participants in stage 3 (median = stage 2). Table 1 summarizes the individual scores on the UPDRS and associated Hoehn and Yahr staging for each participant. All participants reported no difficulty consuming a regular oral diet with thin liquids.
Screening Results
All participants either passed the hearing screening (n = 5) or had the sound level adjusted relative to their pure-tone average, with no less than 35 dB SL to compensate for external noises (e.g., computer fan, hall noise) (n = 5). Scores from the BDI suggested no depression in any participant. One participant presented with a mild mood disorder (score = 13) and one participant presented with borderline depression (score = 17). Composite score results from COGNISTAT were within normal limits for all participants. In sum, no participant showed evidence of a depressive, neurological, or cognitive disorder.
Data Used in Analyses
This study involved three conditions: (1) baseline (single-task) swallow, (2) baseline (single-task) RT trials to auditory stimuli, and (3) dual-task trials combining swallowing with RT trials. A total of 16 baseline swallow trials with single swallows of 5 ml of water and 16 baseline RT trials containing four randomly delivered auditory target trials among 12 distracter trials were completed. The dual-task consisted of 16 trials containing four randomly delivered auditory target trials among 12 distracter trials during which the participant completed a single 5 ml volume of water per trial.
Of the 16 possible trials during the baseline swallowing condition, 10 had complete data for each participant and were used in the final analyses. Of the four possible target trials during the baseline RT trials, three had complete data and were used in the final analyses. The dual-task condition contained four trials divided into two sets of two trials for each of the two phases of swallowing in which they were presented. Data from the dual-task condition yielded one trial from each of the two phases of swallowing, with complete data for all but one participant. Due to equipment failure, no dual-task oropharyngeal data were recorded for one participant. Data loss was due to a sensor malfunction or unreadable sEMG tracing discovered after all of the data were collected.
Baseline Data
Swallowing
The average time for the anticipatory phase of swallowing was 2,572 ms (SD = 703 ms, range = 1,463–4,426 ms). There was no significant difference between trials (F = 0.546, df = 2.633, P = 0.633) for anticipatory phase time. Participants repeated their performance consistently across trials. The average time for the oropharyngeal phase of swallowing was 2,790 ms (SD = 1,449 ms, range = 503–7,355 ms). There was no significant difference between trials (F = 0.796, df = 3.53, P = 0.523). Participants repeated their performance consistently across trials. Phase durations by trial are presented in Fig. 1.
Nonword Discrimination RT
The average RT in the target trials was 921 ms (SD = 426 ms, range = 2,190 ms). Individually, the average RT across all participants for Trial 1 was 1,071 ms (SD = 562 ms), Trial 2 was 786 ms (SD = 356), and Trial 3 was 905 ms (SD = 313). There was no significant difference between trials (F = 3.128, dF = 2, P = 0.068). Participants repeated their performance consistently across trials.
Dual-Task Data
There were two possible RT target trials for the anticipatory phase of swallowing and two possible RT target trials for the oropharyngeal phase of swallowing. From the two target trials in the anticipatory phase, only the first trial contained a full set of data for all ten participants. This was the only trial used in the final analyses. The two target trials in the oropharyngeal phase, however, contained data for just nine of the ten participants because one participant had incomplete data for both RT target trials. A choice was made prior to the analyses to use only the first RT target trial in the oropharyngeal phase because the first of the two target trials was used for anticipatory phase RT analysis. Each of these trials was inspected for outliers using descriptive statistics. No outliers were present for each set of target trials data.
Swallowing
During target trials, participants demonstrated an average anticipatory phase duration of 2,597 ms (SD = 770 ms, range = 1,497–3,975 ms) and an average oropharyngeal phase duration of 2,395 ms (SD = 1,381 ms, range = 784–5,159 ms).
Non-Word Discrimination RT
The average RT for targets presented in the anticipatory phase of swallow was 1,364 ms (SD = 820 ms, range = 402–3,144 ms), and the average RT for targets presented in the oropharyngeal phase of swallowing was 1,580 ms (SD = 1,434 ms, range = 368–5,033 ms).
Comparison Between Baseline and Dual-task
Swallowing
The durations for each of the two phases of swallowing were analyzed for differences. With an average increase of 25 ms from baseline to dual-task, there was no significant difference in anticipatory phase duration (F = 0.023, df = 1, P = 0.884). Additionally, with an average decrease of 395 ms from baseline to dual-task, there was no significant difference for oropharyngeal swallow duration (F = 3.802, df = 1, P = 0.087). Figure 2 depicts the changes in swallowing phase times between baseline and dual-task trials.
Non-word Discrimination RT
RTs were analyzed for differences between baseline and the dual-task within the same phase. There was a significant increase of 443 ms in RT from baseline to dual-task during the anticipatory phase of swallowing (F = 6.898, df = 1, P = 0.028). However, there was no significant difference in the increase of 659 ms in RT from baseline to dual-task during the oropharyngeal phase of swallowing (F = 2.087, df = 1, P = 0.187). Figure 3 depicts the changes in RT between baseline and dual-task trials relative to phase of swallowing.
Discussion
As in the companion article [1], the goal of this research was to determine whether the presence of a motor impairment affects attentional resources involved in swallowing. The motor act of swallowing combined with the motor RT interference task used during this study suggests a shared pool of resources. Further dividing swallowing into the anticipatory phase and the oropharyngeal phase, we hypothesized the anticipatory phase to take a greater amount of attention due to its demand for greater attention, organization, and planning relative to the oropharyngeal phase of swallowing, which has more of an automatic nature.
The clearest evidence for attention was seen by an increase in dual-task compared to baseline RT in the secondary task during the anticipatory phase of swallowing. RTs were slowed during dual-task performance because the motor demands of swallowing were sufficiently great that additional cognitive support (i.e., attention) was required to achieve it competently during this phase. These findings are consistent with data from the physical therapy literature suggesting that motor tasks previously thought to be automatic or overlearned, such as walking, are subject to the influence of attention [33–40]. Those data indicate that the introduction of an additional task to walking (i.e., a dual-task) can affect gait, speed, and posture not only in patients with PD and Alzheimer’s disease, but also in healthy individuals—young and elderly. A similar change from baseline to dual-task in RT was not observed during the oropharyngeal phase of swallowing. Finally, both phase durations were largely invariant when comparing baseline and dual-task conditions.
Our results are consistent with the capacity-sharing model of attention in order to understand the role of attention in swallowing. This model views attention as limited, sharable across tasks, and differentially able to be allocated [17–20, 22]. The capacity model is one that has been used to explain RT effects in dual-task paradigms [17]. In greater detail, capacity-sharing theory suggests that simultaneous tasks share a limited pool of available attentional resources. If one task requires a great amount of those resources, limited resources will be available for processing in a second task. One result would be degradation in the quality of performance of the second task. As it applies to this investigation, a second result might be a delay in response to the secondary task because resource allocation is thought to affect not only performance quality but also response speed [41–43]. In our participants with PD, swallowing required a great amount of resources, thus limited resources were available for the participant’s time to respond to the nonword stimulus via foot pedal depression, suggesting that our participants with PD had subtle motoric difficulties, requiring that they allocate considerable attention to the anticipatory phase of swallowing. When an additional task was added (i.e., the dual-task RT), resources were insufficient to maintain normal response times to the secondary task, in this case response time to the auditory target.
The first explanation assumes a sufficient number of total resources. As an alternate explanation within the capacity-sharing model, participants may have had a limited amount of total resources available. During completion of the dual-task condition, the resources required overloaded the participants, even if motoric swallowing difficulties were not present. Therefore, they allocated available resources to the primary task—swallowing and secondary task performance (RT) suffered as a result. A third explanation is that both motoric and resource limitations contributed to the present pattern of results.
All of these possibilities are interesting to entertain, but this study was not constructed to differentiate among them. Differentiation of these scenarios should be pursued with studies designed to evaluate bidirectional trading effects because they provide the most meaningful evidence that resources are both shared between the concurrent tasks and that task demands are sufficient to demonstrate the concurrent costs. Such evidence also argues against the possibility of a third variable that is shared between the two tasks, from which other computations are derived, such as an impairment of short-term memory. The present data suggest that motoric difficulties with swallowing contributed to the results because evidence of motor difficulties in the extremities (i.e., rigidity, tremor, fine motor coordination evaluated using the UPDRS) was seen in the participants studied. Although resource limitations also may have been present, general cognitive capabilities were normal in these participants with PD, and no evidence was seen that might point to general resource limitations.
A second experimental question investigated whether there is a disparity in the demand for attention between different phases of swallowing (i.e., anticipatory versus oropharyngeal). Compared to the anticipatory phase, the commonly considered “reflexive” oropharyngeal phase was not predicted to require as much cognitive involvement, and, therefore, fewer attentional resources would be necessary. This study supports this prediction in that there was a significant difference in dual-task RTs when compared to baseline RTs in the anticipatory phase of swallowing but not in the oropharyngeal phase. Although there was a considerable time delay in dual-task RT compared to baseline RT during the oropharyngeal phase, there was also large variability in the data that resulted in statistically nonsignificant findings.
The statistical equivalence of baseline to dual-task swallowing durations in the oropharyngeal phase was unanticipated. The literature is clear that hallmark characteristics of PD include stiffness, slowness, speech disturbance, and dysphagia, even in the early stages [16, 23, 44–46], especially in cognitively demanding tasks [47, 48]. None of the participants were known to have dysphagia. They did, however, present with general motor deficits based on results of the UPDRS. Given this fact, it can be concluded that the oropharyngeal phase of swallowing was unaffected by the dual-tasks used. Considering that secondary-task RTs increased significantly in the anticipatory phase, it appears that priority was given to the process of swallowing and resources were available and utilized from the less important or perhaps irrelevant secondary task. Further support for the interference-resistant nature of swallowing was found in the previous study presented in the companion article [1]. One way to assess this in future studies would be to alter the instructions of the task so as to place different proportions of effort on each of the two tasks (i.e., swallowing and nonword discrimination) or by experimentally manipulating the difficulty of the two tasks. For now, we may draw the conclusion that swallowing is prioritized over those exogenous influences on attention offered by the task in this study.
Limitations
Data from the present investigation suggest that the “reflexive,” “vegetative,” and/or “automatic” (i.e., over-learned) nature of swallowing does appear to require cognitive (i.e., attentional) resources in individuals who have compromised motor systems, despite normal cognitive function. Conclusions about swallow’s apparent homeostasis, however, may be premature. The present task demanded enough attention to show a trade-off in resources between baseline RTs and those during the dual task in the anticipatory phase while the oropharyngeal phase remained statistically unchanged. Replication of this study with a larger sample size comparing nonimpaired controls with patients with PD will be necessary. Likewise, this task will need to be replicated in groups of individuals with motor impairments, given the supposition that shared groups of mental resources influence behaviors [17–20, 22]. This should include patients with neuromuscular impairments in the absence of cognitive dysfunction (e.g., muscular dystrophy, Guillain–Barré syndrome, multiple sclerosis). The high variability in the data may be attributed to combining participants with stage 1, stage 2, and stage 3 PD in one group and not accounting for delayed initiation of the pharyngeal swallow via instrumental examination. It is suggested that further study may consider a more homogeneous sample based on disease staging. Finally, combining the oral preparatory, oral propulsive and pharyngeal phases of swallowing appears to be an artificial grouping. This grouping was necessary because of the limitation of reliably identifying these phases separately while swallowing liquid boluses and using sEMG. Even in combination with sEMG, use of fiber-optic endoscopy will not allow for viewing the oral cavity at the same time as the pharyngeal swallow, adding nothing more to the experimental approach. Moreover, the number of trials completed in the three experimental conditions makes videofluoroscopy unfeasible. Exploration of other instrumentation and experimental controls will be necessary to parse the oral preparatory, oral propulsive and pharyngeal phases with greater detail.
Summary
The present findings suggest that attention is involved in the anticipatory phase of swallowing, at least in patients with PD. Despite large demands on attention, swallowing appears to be resilient. There may be a time or an everyday task, however, when there will be shift in attention great enough to impact swallowing physiology. Clinicians should be alerted that caution with swallowing safety should continue in patients with cognitive impairments. Likewise, patients with motor impairments, in the absence of measurable cognitive decline, should not be overlooked.
References
Brodsky MB, McNeil MR, Martin-Harris B, Palmer CV, Grayhack JP, Abbott KV. Effects of divided attention on swallowing in healthy participants. Dysphagia. doi:10.1007/s00455-011-9367-8.
Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, Diamant NE. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999;277:G219–25.
Huckabee ML, Deecke L, Cannito MP, Gould HJ, Mayr W. Cortical control mechanisms in volitional swallowing: the Bereitschaftspotential. Brain Topogr. 2003;16:3–17.
Martin RE, Goodyear BG, Gati JS, Menon RS. Cerebral cortical representation of automatic and volitional swallowing in humans. J Neurophysiol. 2001;85:938–50.
Pouderoux P, Logemann JA, Kahrilas PJ. Pharyngeal swallowing elicited by fluid infusion: role of volition and vallecular containment. Am J Physiol. 1996;270:G347–54.
Daniels SK, Foundas AL. The role of the insular cortex in dysphagia. Dysphagia. 1997;12:146–56.
Hamdy S, Rothwell JC, Aziz Q, Thompson DG. Organization and reorganization of human swallowing motor cortex: implications for recovery after stroke. Clin Sci (Colch). 2000;99:151–7.
Hamdy S, Rothwell JC, Brooks DJ, Bailey D, Aziz Q, Thompson DG. Identification of the cerebral loci processing human swallowing with H2(15)O PET activation. J Neurophysiol. 1999;81:1917–26.
Zald DH, Pardo JV. The functional neuroanatomy of voluntary swallowing. Ann Neurol. 1999;46:281–6.
Zald DH, Pardo JV. Cortical activation induced by intraoral stimulation with water in humans. Chem Senses. 2000;25:267–75.
Groves-Wright K, Boyce S, Kelchner L. Perception of wet vocal quality in identifying penetration/aspiration during swallowing. J Speech Lang Hear Res. 2009;53:620–32.
Daniels SK, Corey DM, Barnes CL, Faucheaux NM, Priestly DH, Foundas AL. Cortical representation of swallowing: a modified dual task paradigm. Percept Mot Skills. 2002;94:1029–40.
Leopold NA, Kagel MC. Swallowing, ingestion and dysphagia: a reappraisal. Arch Phys Med Rehabil. 1983;64:371–3.
Leopold NA, Kagel MC. Dysphagia—Ingestion or deglutition? A proposed paradigm. Dysphagia. 1997;12:202–6.
Miller AJ. The search for the central swallowing pathway: the quest for clarity. Dysphagia. 1993;8:185–94.
Parkinson J. An essay on the shaking palsy. London: Whittingham and Rowland; 1817.
Kahneman D. Attention and effort. Englewood Cliffs: Prentice-Hall; 1973.
Navon D, Gopher D. On the economy of the human-processing system. Psychol Rev. 1979;86:214–55.
Navon D, Miller J. Queuing or sharing? A critical evaluation of the single-bottleneck notion. Cogn Psychol. 2002;44:193–251.
Tombu M, Jolicur P. All-or-none bottleneck versus capacity sharing accounts of the psychological refractory period phenomenon. Psychol Res. 2002;66:274–86.
Tombu M, Jolicoeur P. A central capacity sharing model of dual-task performance. J Exp Psychol Hum Percept Perform. 2003;29:3–18.
Wickens CD. The structure of attentional resources. In: Nickerson R, editor. Attention and performance VIII. Englewood Cliffs: Erlbaum; 1980. p. 239–57.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17:427–42.
Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55:181–4.
Kiernan RJ, Mueller J, Langston JW, Van Dyke C. The neurobehavioral cognitive status examination: a brief but differentiated approach to cognitive assessment. Ann Intern Med. 1987;107:481–5.
Roper BL, Bieliauskas LA, Peterson MR. Validity of the mini-mental state examination and the neurobehavioral cognitive status examination in cognitive screening. Neuropsychiatry Neuropsychol Behav Neurol. 1996;9:54–7.
Kidd D, Stewart G, Baldry J, Johnson J, Rossiter D, Petruckevitch A, Thompson AJ. The functional independence measure: a comparative validity and reliability study. Disabil Rehabil. 1995;17:10–4.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Bonin-Guillaume S, Blin O, Hasbroucq T. An additive factor analysis of the effect of depression on the reaction time of old patients. Acta Psychol. 2004;117:1–11.
Schmidt RA, Lee TD. Motor control and learning: a behavioral emphasis, 3rd ed. Champaign: Human Kinetics; 1999.
Hollerbach S, Fitzpatrick D, Shine G, Kamath MV, Upton AR, Tougas G. Cognitive evoked potentials to anticipated oesophageal stimulus in humans: quantitative assessment of the cognitive aspects of visceral perception. Neurogastroenterol Motil. 1999;11:37–46.
Schneider W, Shiffrin RM. Controlled and automatic human information processing: I. Detection, search, and attention. Psychol Rev. 1977;84:1–66.
Camicioli R, Howieson D, Lehman S, Kaye J. Talking while walking: the effect of a dual task in aging and Alzheimer’s disease. Neurology. 1997;48:955–8.
Hausdorff JM, Yogev G, Springer S, Simon ES, Giladi N. Walking is more like catching than tapping: gait in the elderly as a complex cognitive task. Exp Brain Res. 2005;164:541–8.
Bair N, Bobek MB, Hoffman-Hogg L, Mion LC, Slomka J, Arroliga AC. Introduction of sedative, analgesic, and neuromuscular blocking agent guidelines in a medical intensive care unit: physician and nurse adherence. Crit Care Med. 2000;28:707–13.
O’Shea S, Morris ME, Iansek R. Dual task interference during gait in people with Parkinson disease: effects of motor versus cognitive secondary tasks. Phys Ther. 2002;82:888–97.
Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:122632.
Verghese J, Buschke H, Viola L, Katz M, Hall C, Kuslansky G, Lipton R. Validity of divided attention tasks in predicting falls in older individuals: a preliminary study (see comment). J Am Geriatr Soc. 2002;50:1572–6.
Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002;16:1–14.
Yogev G, Giladi N, Peretz C, Springer S, Simon ES, Hausdorff JM. Dual tasking, gait rhythmicity, and Parkinson’s disease: Which aspects of gait are attention demanding? (References). Eur J Neurosci. 2005;22:1248–56.
Cohen MD. Are we doing enough to minimize fluoroscopic radiation exposure in children? Pediatr Radiol. 2007;37:1020–4.
McLean D, Smart R, Collins L, Varas J. Thyroid dose measurements for staff involved in modified barium swallow exams. Health Phys. 2006;90:38–41.
American Speech-Language-Hearing Association. Guidelines for speech-language pathologists performing videofluoroscopic swallowing studies (Guidelines). ASHA; 2004 (Suppl 24). p. 77–92.
Goldman WP, Baty JD, Buckles VD, Sahrmann S, Morris JC. Cognitive and motor functioning in Parkinson disease: subjects with and without questionable dementia. Arch Neurol. 1998;55:674–80.
Jahanshahi M, Marsden CD. Parkinson’s disease: a self-help guide. New York: Demos Medical Publishing, Inc.; 2000.
Mir P, Matsunaga K, Gilio F, Quinn NP, Siebner HR, Rothwell JC. Dopaminergic drugs restore facilitatory premotor-motor interactions in Parkinson disease. Neurology. 2005;64:1906–12.
Fern-Pollak L, Whone AL, Brooks DJ, Mehta MA. Cognitive and motor effects of dopaminergic medication withdrawal in Parkinson’s disease. Neuropsychologia. 2004;42:1917–26.
Wylie SA, Stout JC, Bashore TR. Activation of conflicting responses in Parkinson’s disease: evidence for degrading and facilitating effects on response time. Neuropsychologia. 2005;43:1033–43.
Fahn S, Elton RL. The UPDRS Development Committee. Unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne D, Goldstein M, editors. Recent developments in Parkinson’s disease. Florham Park: Macmillan Healthcare Information; 1987. p. 153–63.
Martínez-Martín P, Gil-Nagel A, Gracia LM, Gómez JB, Martínez-Sarriés J, Bermejo F. Unified Parkinson’s disease rating scale characteristics and structure. The Cooperative Multicentric Group. Mov Disord. 1994;9:76–83.
Acknowledgments
The authors thank the Mark and Evelyn Trammell Trust, Atlanta, Georgia; the Evelyn Trammell Institute for Voice and Swallowing in the Department of Otolaryngology-Head and Neck Surgery, Medical University of South Carolina, Charleston, South Carolina; and the Trident Parkinson’s Support Group for their support. The authors also thank Neil Szuminsky and Pete Arvenitis for their dedication, ingenuity, and technical expertise that lead to the design and creation of the hardware and programming necessary for this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brodsky, M.B., Abbott, K.V., McNeil, M.R. et al. Effects of Divided Attention on Swallowing in Persons with Idiopathic Parkinson’s Disease. Dysphagia 27, 390–400 (2012). https://doi.org/10.1007/s00455-011-9381-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-011-9381-x