Abstract
Debate continues regarding an association between tracheotomy and aspiration status. The aim of this research was to perform a direct replication study to investigate further the causal relationship, if any, between tracheotomy and aspiration. Twenty-five consecutive adult hospitalized patients participated. Inclusion criteria were a pretracheotomy dysphagia evaluation, subsequent tracheotomy and tracheotomy tube placement, then a post-tracheotomy dysphagia reevaluation prior to decannulation. Twenty-two (88%) participants exhibited the same aspiration status or resolved aspiration pre- versus post-tracheotomy. Three participants exhibited new aspiration post-tracheotomy due to worsening medical conditions. Conversely, four participants exhibited resolved aspiration post-tracheotomy due to improved medical conditions. Excluding these seven participants, all nine participants who aspirated pretracheotomy also aspirated post-tracheotomy and all nine participants who did not aspirate pretracheotomy also did not aspirate post-tracheotomy (P > 0.05). No statistically significant differences were found between aspiration status and days since tracheotomy (χ 2 = 0.08, P > 0.05) or between age and aspiration status (P > 0.05). The absence of a causal relationship between tracheotomy and aspiration status was confirmed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poor methodology has led to the erroneous finding of a purported association between tracheotomy and increased incidence of aspiration, with the fundamental flaw being that no pretracheotomy aspiration data were collected [1–7]. The difficulties associated with collecting pretracheotomy data do not justify their omission, i.e., it cannot be predicted who will undergo a tracheotomy in the future, and once the decision to perform a tracheotomy has been made the patient is either too medically compromised to have a dysphagia evaluation or an endotracheal tube is present. When aspiration status was investigated appropriately, i.e., both pre- and post-tracheotomy, no causal relationship was found [8].
Many individuals who will require a tracheotomy are at increased risk for swallowing disorders, with the result being undocumented aspiration pretracheotomy due to the medical, neurologic, or surgical sequelae that necessitated a tracheotomy in the first place [9–11]. When these individuals subsequently undergo a tracheotomy, any newly documented “increased” incidence of aspiration will be incorrectly attributed to the tracheotomy [8].
Although no causal relationship was found between tracheotomy and aspiration status [8], debate continues regarding an association between tracheotomy and aspiration risk [12, 13]. Therefore, corroboration with a larger sample size via direct replication is warranted [14]. Replication provides two basic functions essential for the substantive base of any scholarly field: verification and disconfirmation, i.e., a fact is not a fact until it is replicable [14]. Specific to the current issue, a causal relationship exists when a tracheotomy is a sufficient condition for the occurrence of aspiration. That is, if the effect (aspiration) occurs before its cause (tracheotomy), a causal relationship does not exist [15]. The purpose of the current direct replication study was to confirm the lack of a causal relationship between tracheotomy and aspiration status [8] by documenting prospectively the incidence of aspiration in the same individual first pretracheotomy and then again post-tracheotomy.
Materials and Methods
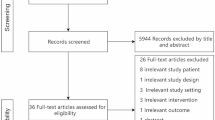
Subjects
This study was approved by the Human Investigation Committee, Yale University School of Medicine. In a prospective manner, between July 2002 and October 2008, 25 adult hospitalized patients from a large tertiary-care teaching hospital met the criteria for inclusion in this study, i.e., they underwent a pretracheotomy objective dysphagia evaluation followed by tracheotomy and tracheotomy tube placement and then a post-tracheotomy objective dysphagia evaluation prior to decannulation. Participant demographics and aspiration status are shown in Table 1.
Procedures
All participants had a fiberoptic endoscopic evaluation of swallowing (FEES) [16, 17] first pre- and then post-tracheotomy. The basic FEES protocol was followed with slight modifications [16, 17]. Briefly, each naris was examined and the scope passed through the most patent naris without administration of a topical anesthetic or vasoconstrictor to the nasal mucosa, thereby eliminating any potential adverse anesthetic reaction and assuring the endoscopist of a safe physiologic examination [18]. The base of tongue, pharynx, and larynx were viewed and swallowing was evaluated directly with food boluses of approximately 5 ml each. All patients were allowed to swallow spontaneously, i.e., without a verbal command to swallow [19]. Equipment consisted of a 3.6-mm-diameter flexible fiberoptic rhinolaryngoscope (Olympus, ENF-P3), light source (Olympus, CLK-4), camera (ELMO, MN401E), and color monitor (Magnavox, RJ4049WA01).
The first food challenge consisted of three boluses of puree consistency (yellow pudding), followed by three liquid boluses (white milk) because these colors have excellent contrast with pharyngeal and laryngeal mucosa [20]. A solid bolus (cracker) was given if the patient had adequate dentition for mastication. Aspiration was defined as the entry of material into the airway below the level of the true vocal folds [21]. No attempt was made to quantify amount of aspiration. A safe swallow was defined as no aspiration during FEES.
A 100% nonblinded agreement between the endoscopist and assisting healthcare professional, e.g., physician, registered nurse, or respiratory therapist, was required to confirm aspiration status. Also, the endoscopist was blinded to results of the pretracheotomy FEES. In addition, the endoscopist who performed all FEES testing in the present study (SBL) participated in a recent investigation that reported an intrarater reliability of 100% for tracheal aspiration with FEES [20].
Statistical analysis was performed using SPSS 16.0 (SPSS Inc., Chicago, IL). Differences between duration of tracheotomy tube placement and age were analyzed with the Student’s t-test and the χ2 test was applied for nonparametric nominal data.
Results
Direct Replication Study
Table 1 shows aspiration status for all participants pre- and post-tracheotomy. Results indicated that 22 of 25 (88%) participants exhibited either the same aspiration status or resolved aspiration pre- versus post-tracheotomy. Post-tracheotomy, three participants exhibited deteriorated medical conditions which resulted in new occurrences of aspiration and four participants exhibited improved medical status which resulted in resolved aspiration (Table 2). Excluding these seven participants, all nine participants who aspirated pretracheotomy also aspirated post-tracheotomy, and all nine participants who did not aspirate pretracheotomy also did not aspirate post-tracheotomy (P > 0.05). Chi-squared analysis indicated that aspiration status was independent of tracheotomy (χ 2 = 0.08, df = 1, P > 0.05).
Examination of Table 1 reveals that the number of days post-tracheotomy was not statistically significantly different (P > 0.05) for participants who aspirated (\(\bar {X}\) = 8.8 days) versus participants who did not aspirate (\(\bar {X}\) = 9.2 days). Participants who aspirated pretracheotomy were not statistically significantly older than participants who aspirated post-tracheotomy (\(\bar {X}\) = 63.2 years, SD [standard deviation] = 10.37 versus 64.8 years, SD = 10.92, P > 0.05). Similarly, participants who did not aspirate pretracheotomy were not significantly older than participants who did not aspirate post-tracheotomy (\(\bar {X}\) = 60.6 years, SD = 9.38 versus \(\bar {X}\) = 59.3 years, SD = 8.17, P > 0.05).
In addition, there was no statistically significant difference for the number of days between pretracheotomy FEES and post-tracheotomy FEES based upon aspiration status (N = 13 nonaspirators, \(\bar {X}\) = 21.5 days, SD = 20.72, range = 6–69 days versus N = 12 aspirators, \(\bar {X}\) = 25.7 days, SD = 22.13, range = 3-86 days, P > 0.05). Finally, in order to determine when safe oral feeding could begin, four patients (Nos. 4, 6, 16, and 20) who aspirated pretracheotomy and two patients (Nos. 11 and 15) who swallowed successfully pretracheotomy but exhibited deteriorated medical conditions (see Table 2) had two to four FEES examinations post-tracheotomy. All six patients continued to aspirate during these post-tracheotomy serial FEES evaluations and were kept nil by mouth.
Combined Data from Direct Replication Study with First Leder and Ross [8] Study
Participant data from the current direct replication study (N = 25) were combined with participant data from the first study (N = 20) [8], permitting analysis of a much larger sample size, i.e., total N = 45; 26 males and 19 females; \(\bar {X}\) = 65.8 years, range = 43–84 years. This allowed for achievement of an important goal of the current direct replication study, i.e., verification of facts [14] from the original study [8]. Results of aspiration status pre- versus post-tracheotomy indicated that 41 of 45 (91%) participants exhibited either the same aspiration status or resolved aspiration pre- versus post-tracheotomy. Number of days post-tracheotomy was not significantly different (P > 0.05) for participants who aspirated (\(\bar {X}\) = 13.3 days) versus participants who did not aspirate (\(\bar {X}\) = 11.3 days). Participants who aspirated pretracheotomy were not significantly older than participants who aspirated post-tracheotomy (\(\bar {X}\) = 66.4 years, SD = 10.85 versus 67.4 years, SD = 10.66, P > 0.05). Similarly, participants who did not aspirate pretracheotomy were not significantly older than participants who did not aspirate post-tracheotomy (\(\bar {X}\) = 65.1 years, SD = 12.26 versus 63.8 years, SD = 12.21, P > 0.05)
Discussion
The results from the initial study [8], the current direct replication study, and the combined data are all in agreement regarding the finding of no causal relationship between tracheotomy and aspiration status. Specifically, since over 90% of participants exhibited the same or resolved aspiration status pre- and post-tracheotomy, the lack of a causal relationship was confirmed between tracheotomy and aspiration [8]. No statistically significant differences were found for either number of days post-tracheotomy and aspiration status or age and aspiration status.
What is of primary importance to resolution of aspiration in this population is improvement in medical condition, mental status, physical strength [22], and discontinuation of medications used to treat the critically ill, i.e., high-dose corticosteroids, neuromuscular blocking agents, and sedatives [11, 23]. In conjunction with the lack of a causal relationship between tracheotomy and aspiration, additional evidence supports the fact that the presence or absence of a tracheotomy tube is also irrelevant to swallowing success or failure [24–26]. Furthermore, research has shown that swallowing dysfunction can continue following decannulation [9] and, conversely, swallowing improvement can occur when the tracheotomy tube remains [11]. This is corroborated by the present study as four participants exhibited resolution of aspiration with the tracheotomy tube in place due to improvement in their general medical condition.
Conclusions
This direct replication study confirmed previous findings [8], i.e., there is no causal relationship between tracheotomy and the presence of a tracheotomy tube and aspiration status. In addition, no statistically significant differences were found for age, number of days between pre- and post-tracheotomy FEES evaluations, and number of days post-tracheotomy based on aspiration status.
References
Betts RH. Post-tracheostomy aspiration. N Engl J Med. 1965;273:155.
Feldman SA, Deal CW, Urguhart W. Disturbance of swallowing after tracheostomy. Lancet. 1966;1:954–5. doi:10.1016/S0140-6736(66)90951-2.
Bonanno PC. Swallowing dysfunction after tracheostomy. Ann Surg. 1971;174:29–33. doi:10.1097/00000658-197107010-00005.
Cameron JL, Reynolds J, Zuidema GD. Aspiration in patients with tracheostomies. Surg Gynecol Obstet. 1973;136:68–70.
Elpern EH, Jacobs ER, Bone RC. Incidence of aspiration in tracheally intubated adults. Heart Lung. 1987;16:527–31.
Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994;105:563–6. doi:10.1378/chest.105.2.563.
Nash M. Swallowing problems in the tracheotomized patient. Otolaryngol Clin North Am. 1988;21:701–9.
Leder SB, Ross DA. Investigation of the causal relationship between tracheotomy and aspiration in the acute care setting. Laryngoscope. 2000;110:641–4. doi:10.1097/00005537-200004000-00019.
DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990;18:1328–30. doi:10.1097/00003246-199012000-00004.
Pannunzio TG. Aspiration of oral feedings in patients with tracheostomies. AACN Clin Issues. 1996;7:560–9. doi:10.1097/00044067-199611000-00010.
Tolep K, Getch CL, Criner GJ. Swallowing dysfunction in patients receiving prolonged mechanical ventilation. Chest. 1996;109:167–72. doi:10.1378/chest.109.1.167.
Hammond CAS, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia. Chest. 2006;129:154S–68S. doi:10.1378/chest.129.1_suppl.154S.
Shama L, Connor NP, Ciucci MR, McCulloch TM. Surgical treatment of dysphagia. Phys Med Rehabil Clin N Am. 2008;19:817–35. doi:10.1016/j.pmr.2008.05.009.
Muma JR. The need for replication. J Speech Hear Res. 1993;36:927–30.
Heise DR. Causal analysis. New York: Wiley & Sons; 1975.
Langmore SE, Schatz MA, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216–9. doi:10.1007/BF02414429.
Langmore SE, Schatz MA, Olsen N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100:678–81.
Leder SB, Ross DA, Briskin KB, Sasaki CT. A prospective, double-blind, randomized study on the use of topical anesthetic, vasoconstrictor, and placebo during transnasal flexible fiberoptic endoscopy. J Speech Hear Res. 1997;40:1352–7.
Daniels SK, Schroeder MF, DeGeorge PC, Corey DM, Rosenbek JC. Effects of verbal cue on bolus flow during swallowing. J Speech Lang Hear Res. 2007;16:120–47.
Leder SB, Acton LM, Lisitano HL, Murray JT. Fiberoptic endoscopic evaluation of swallowing with and without blue-dyed food. Dysphagia. 2005;20:157–62. doi:10.1007/s00455-005-0009-x.
Logemann JA. Evaluation and treatment of swallowing disorders, 2nd edn. Austin, TX: Pro-Ed; 1998.
Leder SB. Serial fiberoptic endoscopic swallowing evaluations in the management of patients with dysphagia. Arch Phys Med Rehabil. 1998;79:1264–9. doi:10.1016/S0003-9993(98)90273-8.
Ashley J, Duggan M, Sutcliffe N. Speech, language, and swallowing disorders in the older adult. Clin Geriatr Med. 2006;22:291–310. doi:10.1016/j.cger.2005.12.008.
Donzelli J, Brady S, Wesling M, Theisen M. Effects of removal of the tracheotomy tube on swallowing during the fiberoptic endoscopic exam of the swallow (FEES). Dysphagia. 2005;20:283–9. doi:10.1007/s00455-005-0027-8.
Leder SB, Joe JK, Ross DA, Coelho DH, Mendes J. Presence of a tracheotomy tube and aspiration status in early, postsurgical head and neck cancer patients. Head Neck. 2005;27:757–61. doi:10.1002/hed.20239.
Sharma OP, Oswanski MF, Singer D, Buckley B, Courtright B, Raj SS, et al. Swallowing disorders in trauma patients: impact of tracheostomy. Am Surg. 2007;73:1117–21.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leder, S.B., Ross, D.A. Confirmation of No Causal Relationship Between Tracheotomy and Aspiration Status: A Direct Replication Study. Dysphagia 25, 35–39 (2010). https://doi.org/10.1007/s00455-009-9226-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-009-9226-z