Abstract
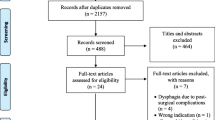
Swallowing apnea duration (SAD) and swallow-respiratory phase relationships were examined in individuals with cerebral vascular accident (CVA) and dysphagia who aspirated (n = 11) and did not aspirate (n = 15). Simultaneous videofluoroscopic and respiratory measures were recorded across 5-, 10-, 15-, and 20-ml thin and thick liquid bolus trials. These data were also compared with that previously acquired with healthy older adults (n = 20). A moderate amount of systematic missing data was evidenced in the individuals who were dysphagic and especially those who aspirated subsequently limiting inferential analyses. Only 1 of the 11 participants who aspirated and 7 of the 15 who did not aspirate completed all 16 conditions. Six of the remaining ten who aspirated had missing data subsequent to termination of trials due to aspiration risk. The remaining four and seven of the eight who did not aspirate had missing data due to poor respiratory waveforms. From the remaining data, it was found that SAD and respiratory phase relationships differed among individuals with dysphagia and CVA (i.e., those who aspirate vs. those who do not aspirate) and healthy older adults. SAD was found to be longer for those who aspirated versus those who did not for all bolus viscosities and volumes with the exception of thick-liquid 10-ml boluses. In addition, SAD from those that aspirated was twice as long as that found in healthy older adults for all conditions. Regarding respiratory phase relationships, there was a difference between the proportions of respiratory patterns in those who aspirated versus those who did not. Those who aspirated demonstrated a markedly greater percentage of swallows that interrupted inhalation. In addition, the inhale-swallow-inhale pattern occurred with a greater frequency as swallowing severity increased. Healthy older adults, those who did not aspirate, and those who aspirated used the inhale-swallow-inhale pattern 0.1%, 3.0%, and 9.0%, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Respiration cessation (i.e., swallowing apnea [SA]) is a well-recognized phenomenon that occurs during normal swallowing [1–9]. SA has been well described in the literature relative to its duration [1,5,10] and its onset and offset relative to other swallowing physiologic events (i.e., hyoid elevation, lingual bolus propulsion) [9,11,12]. Furthermore, the effect of bolus volume, viscosity, and taste on SA duration has been reported [1,5,10]. Most recently, the effects of posture such as chin tuck and recumbency on SA have been reported [13].
The respiratory phase interrupted by swallowing has been well researched [2,5–8,10,14]. Hiss et al. [5] reported that expiration was the most frequently interrupted respiratory phase with an occurrence of 62%. Although expiration is clearly the phase most frequently interrupted for swallowing, slight differences exist across the studies secondary to bolus delivery methods and recording techniques.
Initially, researchers were concerned about whether SA occurred as the result of its own neural mechanism or if it occurred obligatory to airway closure. SA has been demonstrated to occur as the result of its own neural mechanism [4,15]. In fact, SA onset and offset is an integral part of swallowing and has recently been identified to be the only single factor that explained 13% of the variability across the 11 studied swallowing onset times [16]. That is, swallowing was not found to be separated by oral and pharyngeal components as traditionally thought. One phase of swallowing can not be separated from the other because swallowing is a fluid, synergistic process; however, if one temporal factor came closest to serving as a separator of phases, it was the onset and offset of SA. Thus, SA is clearly a mechanism of swallowing that deserves investigation because it holds promise in increasing our understanding of normal and disordered swallowing.
Identifying SA and the variables (i.e., bolus volume, viscosity, taste, posture) that affect it in normal individuals is a necessary precedent in understanding SA in individuals with abnormal swallowing. If abnormal SA is identified in individuals with disordered swallowing, then SA would serve as a measurement parameter that may predict disordered swallowing and provide another physiologic variable for measurement to enhance swallowing assessments. Furthermore, SA values of disordered swallows that have been specifically correlated with aspiration events may offer insight into airway protection [5].
Researchers have begun to investigate SA in populations known to have disordered swallowing. It has been revealed that SA is changed in disordered swallowing. However, the extent of or reason for the change is unknown at this time. Selley and colleagues [17] performed some of the original work with SA in disordered swallowing and reported that individuals with neurologic disease or insults demonstrated varying SA patterns compared with healthy normal individuals. In a group of older patients with dysphagia, a shorter swallowing apnea duration (SAD) was associated with penetration and aspiration [18]. In those with cerebral palsy, SA was demonstrated to have greater variability and duration relative to controls [19]. In patients with cerebral vascular accident (CVA), resting respiratory rate was faster with a shorter mean cycle length compared with that of normal adults [14]. Concerning the respiratory cycle surrounding SA, Leslie et al. [20] reported that individuals with CVA demonstrated statistically significant less exhale-swallow-exhale patterns compared with their age-matched control group. No difference in SAD was found between in the two groups. Although serving as an original contribution to the field on SA in CVA, generalization of the study to all individuals with stroke is limited secondary to the small number of participants and lack of differentiation in analyses between those who aspirated and those who did not aspirate.
SA and SAD as a function of CVA needs further, more comprehensive investigation. Swallowing disorders are a common sequela, ranging from 37% to 78% depending on the lesion location and severity, in those with CVA [21]. Thus, those with CVA would greatly benefit from further elucidation of physiologic breakdown in their SA. The purpose of this study was to determine the effects of bolus volume and viscosity on SAD measurements and swallow-respiratory phase relationships in individuals with CVA as measured via simultaneous videofluoroscopy and respiratory assessments. A second purpose of this study was to determine if differences in SAD and swallow-respiratory phase relationships existed between adults with CVA and normal adults.
Method
Participants
Twenty-six adults with the diagnosis of CVA served as participants. All participants had been identified as dysphagic and at risk for aspiration from the clinical swallowing evaluation, which included an oral mechanism examination and test boluses. Participants were scheduled for a videofluoroscopic swallow exam (VFSE) as part of their clinical care and provided informed consent personally or through legal guardians. They were not stratified by hemispheric lesion, severity of CVA, or time post-onset. Participants included 14 males and 12 females with a mean age of 71 years (range = 45–89 years). Some participants required supplemental oxygen via nasal cannula; however, none of the participants had a history of asthma, chronic obstructive pulmonary disease, adult respiratory distress syndrome, or concomitant neurologic disease. Twenty participants with normal swallowing served as controls for the second set of analyses. The data from normal adults were acquired from a previously reported investigation by the primary author [5] and included data from 60 adults stratified by age (i.e., young, middle-aged, and older adults). Only data from the older adults were used for comparison in the current study (i.e., age range = 60–83 years; mean = 67.0 years, standard deviation [SD] = 6.6). The older-adult data only was chosen as control data for this study because the mean age of the individuals with CVA in the current study was 71 years with only one participant under the age of 60 years.
Apparatus
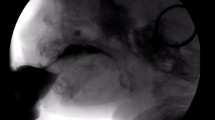
A KayPENTAX Swallowing Workstation, Model 7100 (KayPENTAX, Lincoln Park, NJ) was used to obtain concurrent VFSE and respiratory signals. The respiratory information was obtained via a 2-m nasal cannula (Hospitak, Farmingdale, NY) identical to that used to deliver supplemental oxygen. The proximal end of the nasal cannula was placed at the entrance of each nare. Of note, some participants used a nasal cannula for supplemental oxygen. However, the proximal end of the study nasal cannula was still placed at the entrance of one or both nare and respiratory waveforms were of good quality given the sensitivity of the airflow sensor transducer (i.e., 0–200 sccm and accurate sensing of low pressures of 0–2 cm H2O). The distal end of the nasal cannula was coupled to an analog-to-digital airflow sensor thermistor transducer (Honeywell Microswitch Model AWM2200V). Digital 12-bit samples were obtained with a sampling frequency of 250 Hz. The system software generated concurrent airflow waveforms as a function of time. The fluoroscopic imaging was acquired at 60 fields (30 frames) per second allowing for measurement resolution of approximately 17 ms per field. The X-ray beam was coned to image the oral cavity, pharynx, upper airway, and cervical esophagus of each patient in the lateral projection.
Procedure
VFSE and respiratory tracings via nasal cannula were recorded concurrently for each participant. Eight conditions were studied: 5-, 10-, 15-, and 20-ml bolus volumes across thin (i.e., 1:1 barium:water) and thick (i.e., not diluted) liquid barium (EZPaque Liquid, E-Z-EM, Inc., Lake Success, NY; 60% w/v and 41% w/w) viscosities. Two repetitions of each condition were offered to the participants starting with the smallest bolus volume and increasing in volume on thick and then thin liquid. Potentially, participants contributed 16 swallows each; however, the study protocol was terminated short of this goal if the patient demonstrated aspiration on a viscosity/volume beyond what was helpful for clinical management. For example, if a patient demonstrated only trace aspiration on the first trial of a 15-ml bolus, then the second trial of a 15-ml bolus was administered since the aspiration was only trace and sometimes patients perform better with repetitions. In contrast, if the participant demonstrated gross aspiration on the first trial of the 15-ml bolus condition, then the second 15-ml and the 20-ml trials were not administered so as not to put the patient at risk for more aspiration solely to follow the research protocol when it would not be clinically helpful to the patient. Participants were seated upright, instructed to breathe through their nose, and allowed 5 min to familiarize themselves with setting and equipment before trials began. The measured boluses were placed in 30-ml medicine cups, and the participants were instructed to swallow the amount placed in the cup when they were ready. The examiner administered the boluses and applied slight lip closure to facilitate respiration through the nasal passages for participants who were physically or cognitively unable to follow verbal instructions.
SAD and swallow-respiratory phase relationships were extracted from the airflow waveforms offline with a positive polarity indicating expiration and a negative polarity indicating inspiration. The apneic pause was defined as a flat line on the display void of positive or negative excursions in conjunction with the swallow as visualized on the videofluoroscopic imaging. SAD was measured in seconds. In addition, the phase of respiration that was interrupted by the swallow was recorded. A positive or negative polarity preceding the apneic pause was recorded as swallowing interrupting expiration or inspiration, respectively. Similarly, a positive or negative polarity succeeding the apneic pause was deemed expiration or inspiration, respectively, after the swallow. An “inspiratory spike,” which corresponded with laryngeal descent during 77% of normal adults [8], was also frequently observed in individuals with CVA and was not included in SAD measurements. That is, a brief negative polarity occurred at the end of the flat, apneic line in some of the participants. This “inspiratory spike” is an artifact of the larynx descending and the pharynx opening at the completion of the swallow creating a negative pressure or vacuum within the nasopharynx and then subsequently recorded on the waveform as a brief negative polarity. Penetration and aspiration events were also recorded. Penetration was defined as the entry of the bolus or part of the bolus into the laryngeal vestibule but not traversing the vocal folds. Material that entered the laryngeal vestibule and cleared with the swallow was also judged as penetration. Aspiration was defined as visualization of the bolus or part of the bolus below the vocal folds.
Data Analysis
One investigator measured SADs from all of the participants to eliminate any variance that may be introduced from multiple examiners measuring and recording SAD. Another investigator reexamined 16 of the 26 participants’ respiratory waveforms in an effort to provide an index of interobserver agreement. The mean SADs were 1.77 s and 1.65 s for the first and second observer, respectively. To investigate the interobserver agreement, two analyses were undertaken. First, differences in SAD means were investigated with a t test for unpaired samples. No significant difference was found between the two observers’ mean SADs [t (381) = 1.04, p = 0.30]. Second, a Pearson product-moment correlation coefficient (r) was conducted. A significant correlation (r = 0.96, p < 0.001) was found between the two observers’ SADs. The scatterplot of this data is illustrated in Figure 1. From these analyses one may conclude that interobserver agreement was good.
Results
Swallowing Apnea Duration
The study was designed for the 26 participants to contribute data for two liquid viscosities (i.e., thin and thick), four volumes (i.e., 5, 10, 15, and 20 ml), and two trials affording 16 trials per participant and a study total of 416 data points for analyses. However, as expected, some participants aspirated to the degree that the 16 trials could not be completed. Participants were subsequently grouped as “individuals who did not aspirate” (IWDNA; n = 15) and “individuals who aspirated” (IWA; n = 11). Only 1 of the 11 IWA and 7 of the 15 IWDNA completed all 16 conditions. Six of the remaining ten IWA had missing data due to the need to terminate the trials because of aspiration risk. The remaining four IWA and seven of the eight IWDNA had missing data due to poor respiratory waveforms. Three of the four IWA with poor respiratory waveforms were missing only three or less trials. One had 12 missing trials. Of the seven IWDNA with poor waveforms, five were missing only two or less trials, and two were missing four and six trials. One of the IWDNA was missing all of the thick liquid trials (i.e., 8) because only thin liquids were tested. Only thin liquids were tested because that was deemed what was clinically relevant to this patient’s clinical care. Thus, administration of additional thick liquid boluses and subsequent additional fluoroscopic radiation exposure to only meet the requirements of the research protocol were not warranted as written for and approved by the IRB.
For all participants both trials were averaged to reduce the amount of missing data for study analyses. In cases where a second trial was missing, the first trial that was completed was used. Averaging reduced the missing data from 30% to 20%. Table 1 presents the missing data as a function of bolus viscosity and bolus volume for both groups.
Mean SADs as a function of group, bolus viscosity, and bolus volume are presented in Table 2. Differences in SAD as a function of group, bolus viscosity, and bolus volume were not subjected to inferential analyses because of the large percentage of systematic missing data (i.e., IWA had a higher percentage of missing data because of inability to complete the trials due to aspiration risk and poor respiratory waveforms). Also, inferential analyses were not used because of the small number of data points in some cells (e.g., in some cases the number of IWA at a given bolus volume and viscosity was only four). Nevertheless, it is evident from Table 2 that mean SAD was longer for IWA for all bolus viscosities and volumes with the exception of thick liquid 10 ml boluses.
It was of interest to determine more systematically how SADs from IWA and IWDNA differed from healthy older adults. SAD and respiratory phase data from 20 healthy older adults (age range = 60–83 years; mean = 67.0, SD = 6.6) was acquired on 10-, 15-, and 20-ml boluses of thin liquids in a previous study [5]. Data from that study and for the same conditions from participants in this study are presented in Table 3. As seen in Table 3, SAD was longer in both groups of patients with CVA (i.e., IWA and IWDNA) compared with that of healthy older adults. Mean SADs for IWA was twice as long as those for healthy older adults at each bolus volume. Thus, SAD was markedly longer and more variable in individuals with CVA, regardless if they were IWA or IWDNA, than that of older healthy participants.
Respiratory Phase Relationships
Tables 4 and 5 present swallowing counts and percentages of respiratory patterns (i.e., exhale-swallow-exhale [ESE], exhale-swallow-inhale [ESI], inhale-swallow-exhale [ISE], and inhale-swallow-inhale [ISI]) as a function of group (i.e., IWA vs. IWDNA), and bolus volume (i.e., 5, 10, 15, and 20 ml) of thin and honey-thick liquids, respectively. In these presentations, available swallows from both trials were considered. Ninety of the 176 swallows and 214 of the 240 swallows were generated by the IWA and IWDNA, respectively (i.e., 11 IWA and 15 IWDNA times two viscosities, four bolus volumes, and two trials). No inferential analysis was undertaken because of the small numbers in each cell. However, as evident in Tables 4 and 5, there was a greater proportion of IWA that interrupted inhalation compared to IWDNA across all bolus volumes and viscosities with the exception of the one condition of 5 ml of thin liquid. Table 6 illustrates the respiratory pattern swallow and percentage data of IWA and IWDNA collapsed across both bolus volume and viscosity. The IWDNA had a markedly higher percentage of ESE swallows compared to IWA. That is, IWA had about twice as many swallows that interrupted inhalation as the IWDNA.
It was also of interest to examine respiratory patterns as a function of group including healthy older adults. Swallow counts and percentages of respiratory patterns as a function of group (i.e., healthy older adults, IWA, and IWDNA) collapsed across bolus volume (i.e., 10, 15, and 20 ml) are presented in Table 7 and illustrated in Figure 2. The healthy older adults generated all of their 180 swallows. That is, 20 participants contributed three trials each of 10-, 15-, and 20-ml thin liquid boluses. Again, no inferential analyses were conducted because of the small number of observations in four of the cells. However, the largest proportion of difference between the groups was found in the swallows involving inhalation. Healthy older adults used the ISE pattern 23% compared with only 7.0% and 5.0% in IWDNA and IWA, respectively. In addition, ISI increased with swallowing severity. Healthy older adults, IWDNA, and IWA used the ISI pattern 0%, 3.0%, and 9.0%, respectively.
Discussion
This study examined the effects of bolus volume (i.e., 5, 10, 15, and 20 ml) and viscosity (i.e., thin and thick liquids) on SAD and SA respiratory phase relationships in 26 individuals with CVA during simultaneous videofluoroscopy and respiratory assessments. In addition, this study compared SA and SAD respiratory phase relationships of individuals post-CVA with data acquired from a previous study of 20 healthy older individuals.
The first finding of this study was the amount of missing data inherent in assessing SA in individuals who are dysphagic. Of the 11 IWA only one participant was able to complete all of the trials and only seven of the IWDNA had complete data sets. Thus inferential analyses were markedly limited even in a study with 26 participants secondary to terminated trials due to aspiration risk and/or poor respiratory waveforms sometimes found in dysphagic individuals.
Assessment of the raw data revealed that mean SAD was longer for IWA versus IWDNA across all bolus volumes and viscosities with the exception of the 10-ml thick-liquid condition. In addition, mean SAD of IWA was twice as long compared with that of healthy older individuals. Evaluation of the respiratory phase relationships revealed that IWA had a greater frequency of swallows that interrupted inhalation compared to IWDNA. Furthermore, the ISI pattern increased with increases in swallowing severity and was present in 1.0%, 3.0%, and 9.0% of swallows from healthy older adults, IWDNA, and IWA, respectively.
This study assessed SA and SAD with simultaneous respiratory and videofluoroscopic imaging of individuals with CVA who aspirated and who did not aspirate. However, the inherent problem in some cases was the need to terminate trials once the amount of aspiration an individual experienced was beyond what was clinically reasonable. Thus, one finding was the marked amount of systematic missing trials in individuals post-CVA. Systematic missing data limited our ability to use inferential analyses and restricted the evaluations to comparisons of means and percentages across groups. However, this was a notable observation within itself. That is, future investigators will appreciate the need to recruit large sample sizes in an effort to reveal true clinical trends among IWA. Also of note, there were some missing data secondary to poor respiratory tracings. This was also determined to be a systematic problem in individuals with dysphagia. That is, the respiratory breaths were sometimes too shallow or irregular to reliably measure SAD and SA respiratory phase relationships. Even though systematic missing data was an obstacle, 80% of the anticipated trials were completed and available for analyses. Thus, SA and SAD means and percentages across the targeted groups and conditions were reported.
The finding that SAD in those with CVA was longer than that of healthy older adults was consistent with those reporting delayed oropharyngeal transit time in individuals post-CVA [22–25]. However, a longer SAD in IWA and IWDNA compared to healthy older adults as found in this study conflicted with findings of Nilsson et al. [18] who reported shorter SAD in individuals with dysphagia who aspirate. One plausible explanation was that the “misdirected swallows” (p. 505) reported by Nilsson et al. included both penetration and aspiration. We did not include penetration in any of our analyses. Penetration has been demonstrated in normal healthy older adults [26] and is not indicative of dysphagia or even a misdirected swallow. Thus, by including penetration in their categorization and analyses of misdirected swallows, Nilsson et al. inadvertently included SADs of what was likely normal healthy older adult swallows. This likely resulted in shorter SADs than what would have been measured if they had assessed only SADs associated with aspiration swallows.
Another reason Nilsson et al. [18] reported shorter SADs for misdirected swallows may have been that their study included individuals with CVA but also included individuals with dysphagia from other neurologic diseases. Nonetheless, a shorter SAD intuitively seemed like that would be associated with aspiration. That is, the less time one held one’s breath (i.e., SAD), the more likely the airway was open allowing for aspiration. This reasoning is intuitive if one assumes that the cause of SA is obligatory laryngeal closure only. However, previous researchers have demonstrated that SA occurs as the result of a central process, not only an obstructive process (i.e., laryngeal closure during swallowing). Thus, SA may occur obligatory to laryngeal closure; however, neural inhibition of breathing is clearly present in SA. SA has been repeatedly found in individuals with laryngectomy [4,15] who demonstrated SA in the absence of the ability to achieve any type of laryngeal closure. An individual with CVA may have neural inhibition of respiration (i.e., SA) but still have an open glottis secondary to delayed pharyngeal and laryngeal mechanisms allowing for aspiration. Perhaps a future study of simultaneous endoscopy and respiratory assessment in individuals with CVA may elucidate this. Since endoscopy allows for direct visualization of the larynx, one may measure SA and observe aspiration outside of the “white-out” period associated with laryngeal and pharyngeal closure. However, regardless of the mechanism causing SA, we demonstrated that SAD was clearly longer in IWA compared to IWDNA and still longer relative to healthy older adults.
Another possible difference in a longer SAD as found in this study compared with that reported by Nilsson et al. [18], who found a shorter SAD associated with misdirected swallows, was that in this study the aspirator SAD was averaged across all bolus trials whether that particular trial was associated with an aspiration event or not. That is, a patient only had to aspirate once to be considered an IWA. Thus, trials that included aspiration and those that did not include aspiration on the same patient who had even only aspirated once were analyzed under the IWA group. The reason for this was the future clinical pursuit of possibly being able to use SAD to predict or distinguish IWA from IWDNA. Thus, at bedside one could use a noninvasive respiratory assessment to facilitate decisions of aspiration risk and referrals for more objective imaging swallowing assessments. Clearly, in this study SAD was longer in IWA versus IWDNA as seen in seven of eight conditions studied. However, some overlap existed across the means of IWA and IWDNA when averaged across bolus size and viscosity. Thus, it appears from this investigation that if the SAD measurement may be potentially useful in discriminating between IWA and IWDNA, clinical testing would need to occur with controlled bolus volumes and viscosities. Replication of this study with larger sample sizes is needed to support SAD as a clinical differentiator of a potential IWA who would benefit from an instrumental evaluation.
A longer SAD as found in this study was consistent with that reported by Selley et al. [17]. They reported a SAD that was twice as long in 11 individuals with CVA compared with their normal controls (i.e., 1.2 s, range = 0.4–3.4 s vs. 0.6 s, range = 0.3–1.0 s, respectively). They did not differentiate IWA from IWDNA and did not delineate how the diagnosis of dysphagia was determined. Nevertheless, a longer SAD in those with CVA was reported. In contrast, Leslie et al. [20] reported no difference in SADs of 18 individuals post-CVA and healthy older adults across 5-ml water and yogurt swallows. They had fewer participants and reported only 5-ml bolus volumes. This may account for the differences seen in their study and the current study. Thus, equivocal findings of SADs in individuals with CVA relative to healthy older adults are apparent. However, herein we used the largest number of individuals with CVA; we studied CVA not confounded with other neurologic diseases; we measured only aspirated, not penetrated, swallows, as misdirected; and, most importantly, we documented dysphagia and aspiration by using simultaneous videofluoroscopy and respiratory assessments. Thus, a longer SAD associated with increasing severity of swallowing difficulty in CVA was demonstrated with stronger methodology. However, future studies with more robust numbers of participants possibly stratified by hemispheric lesion, severity of lesion, etc., are warranted.
Of interest was the finding that IWA had longer SAD than IWDNA for seven of the eight conditions studied. Mean SADs of 1.38 vs. 1.50 s were found for IWA vs. IWDNA, respectively, on 10 ml of thick liquids. One may ask: “Why did not the IWA demonstrate a longer SAD on all eight conditions?” This may be an isolated finding and may be a manifestation of systematic missing data.
In addition, it was found that the ISI pattern occurred with greater frequency as swallowing severity increased (i.e., IWA vs. IWDNA). Only 1 of 180 swallows from healthy older adults demonstrated an ISI pattern and may actually be an outlier. Thus, a swallowing respiratory phase parameter that may be predictive of dysphagia is the presence of an ISI pattern. A moderate amount of disagreement exists in the literature regarding the frequency of the respiratory phase patterns (i.e., ESE, ESI, ISE, and ISI) in healthy volunteers. One of the most plausible reasons for the differences seen across studies is the bolus delivery method. Some researchers used syringe delivery while others used premeasured bolus sizes placed in a cup that the patient self-administered. Although some of the participants with CVA were unable to self-administer their bolus trials and the examiner administered the bolus for them, we used the same delivery method for participants with CVA and healthy older adults. Thus, the finding that the ISI pattern may distinguish dysphagic CVA from healthy older adults was promising. The prevalence of ISI in individuals with CVA was also reported by Leslie et al. [20]. Again, for swallow-respiratory phase relationships and SAD measurements to hold any promise as predictors of patients at risk for aspiration, it appears that future researchers will need to control bolus volume, viscosity, and delivery method. That is, if the clinical utility of these measurements is to be achieved, a controlled bolus volume and delivery method will likely be necessary. The window of what differentiates IWA from IWDNA may be very tight at each particular bolus volume, bolus viscosity, and bolus delivery method.
One last issue is that studying SAD of individuals with CVA is more challenging than studying SAD of healthy adult volunteers. The majority of waveforms were easily measured; however, as noted in the Results section, a few of the waveforms were unanalyzable and were excluded from analyses. Even using a highly sensitive airflow thermistor transducer (i.e., 0–200 sccm and accurate sensing of low pressures of 0–2 cm H2O), some difficulties can be encountered as part of studying a compromised patient population. Individuals with CVA can have reduced tidal volumes and subsequently have shallow breathing. Furthermore, there is a possible variable of obstructed nasal passages secondary to oxygen therapy and lack of good tidal volume to clear nasal passage material. These variables, along with possible premorbid tendencies for mouth breathing, sometimes required the examiner to gently apply slight lip closure to facilitate airflow through the nasopharynx. It is true that patients will usually close their mouth as they swallow; however, to detect pre-and postswallow-respiratory phases, reliably improved nasal airflow waveforms were sometimes facilitated by reminding patients to breathe through their nose or by applying slight lip closure to patients who could not follow directions. The application of perioral stimulation could alter swallowing physiology but was needed a few times to facilitate airflow through the nasopharynx. These variables that affect SAD measurements should be appreciated by investigators who have traditionally evaluated SAD only in healthy volunteers as they plan future studies targeting a more compromised or acutely ill population.
In summary, SAD and respiratory phase relationships in individuals with CVA and dysphagia (n = 26) were investigated and compared to previously acquired data of healthy older adults (n = 20). A marked amount of systematic missing data with IWA was evidenced. In addition, poor-respiratory waveforms were a more frequent although not an insurmountable problem in individuals with CVA compared with healthy older volunteers. It was found that IWA had a longer SAD than IWDNA and SAD of these individuals with CVA was longer than that of healthy older adults. Furthermore, differences were found in respiratory phase relationships. IWA demonstrated a greater frequency of ISI than IWDNA and healthy older adults. This study provides a springboard for future larger-scale studies to further delineate whether SAD and/or swallow-respiratory phase relationships may differentiate IWA from IWDNA in individuals with CVA. Future studies may also stratify individuals with CVA by lesion location, time post-onset, and severity to determine how SAD varies as a function of CVA-related variables as well. Additional studies of SAD in CVA will potentially allow clinicians to measure SAD at bedside and then make recommendations for an instrumental swallowing evaluation with more objective data and confidence.
References
Butler SG, Postma GN, Fischer E: Effects of viscosity, taste, and bolus volume on swallowing apnea duration of normal adults. Otolaryngol Head Neck Surg 131:860–863, 2004
Hirst LJ, Ford GA, Gibson GJ, Wilson JA: Swallow-induced alterations in breathing in normal older people. Dysphagia 17:152–156, 2002
Hiss SG, Strauss M, Treole K, Stuart A, Boutilier S: Effects of age, gender, bolus volume, bolus viscosity, and gustation on swallowing apnea onset relative to lingual bolus propulsion onset in normal adults. J Speech Lang Hear Res 47:572–583, 2004
Hiss SG, Strauss M, Treole K, Stuart A, Boutilier S: Swallowing apnea as a function of airway closure. Dysphagia 18:293–300, 2003
Hiss SG, Treole K, Stuart A: Effects of age, gender, bolus volume, and trial on swallowing apnea duration and swallow/respiratory phase relationships of normal adults. Dysphagia 16:128–135, 2001
Klahn MS, Perlman AL: Temporal and durational patterns associating respiration and swallowing. Dysphagia 14:131–138, 1999
Martin-Harris B, Brodsky MB, Michel Y, Ford CL, Walters B, Heffner J: Breathing and swallowing dynamics across the adult lifespan. Arch Otolaryngol Head Neck Surg 131:762–770, 2005
Martin-Harris B, Brodsky MB, Price CC, Michel Y, Walters B: Temporal coordination of pharyngeal and laryngeal dynamics with breathing during swallowing: single liquid swallows. J Appl Physiol 94:1735–1743, 2003
Perlman AL, He X, Barkmeier J, VanLeer E: Bolus location associated with videofluoroscopic and respirodeglutometric events. J Speech Lang Hear Res 48:21–33, 2005
Martin BJ, Logemann JA, Shaker R, Dodds WJ: Coordination between respiration and swallowing: respiratory phase relationships and temporal integration. J Appl Physiol 76:714–723, 1994
Selley WG, Ellis RE, Flack FC, Bayliss CR, Pearce VR: The synchronization of respiration and swallow sounds with videofluoroscopy during swallowing. Dysphagia 9:162–167, 1994
Gross RD, Attwood CW Jr, Grayhack JP, Shairman S: Lung volume effects on pharyngeal swallowing physiology. J Appl Physiol 95:2211–2217, 2003
Ayuse T, Ayuse T, Ishitobi S, Kurata S, Sakamoto E, Okayasu I, Oi K: Effect of reclining and chin-tuck position on the coordination between respiration and swallowing. J Oral Rehabil 33:402–408, 2006
Leslie P, Drinnan MJ, Ford GA, Wilson JA: Swallow respiratory patterns and aging: presbyphagia or dysphagia? J Gerontol A Biol Sci Med Sci 60:391–395, 2005
Charbonneau I, Lund JP, McFarland DH: Persistence of respiratory-swallowing coordination after laryngectomy. J Speech Lang Hear Res 48:34–44, 2005
Martin-Harris B, Michel Y, Castell DO: Physiologic model of oropharyngeal swallowing revisited. Otolaryngol Head Neck Surg 133:234–240, 2005
Selley WG, Flack FC, Ellis RE, Brooks WA: Respiratory patterns associated with swallowing: Part 2. Neurologically impaired dysphagic patients. Age Ageing 18:173–176, 1989
Nilsson H, Ekberg O, Bulow M, Hindfelt B: Assessment of respiration during video fluoroscopy of dysphagic patients. Acad Radiol 4:503–507, 1997
Rempel G, Moussavi Z: The effect of viscosity on the breath-swallow pattern of young people with cerebral palsy. Dysphagia 20:108–112, 2005
Leslie P, Drinnan MJ, Ford GA, Wilson JA: Swallow respiration patterns in dysphagic patients following acute stroke. Dysphagia 17:202–207, 2002
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R: Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36:2756–2763, 2005
Mann G, Hankey GJ: Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia 16:208–215, 2001
Mann G, Hankey GJ, Cameron D: Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 30:744–748, 1999
Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL: Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res 37:1041–1059, 1994
Veis SL, Logemann JA: Swallowing disorders in persons with cerebrovascular accident. Arch Phys Med Rehabil 66:372–375, 1985
Hind JA, Nicosia MA, Roecker EB, Carnes ML, Robbins J: Comparison of effortful and noneffortful swallows in healthy middle-aged and older adults. Arch Phys Med Rehabil 82:1661–1665, 2001
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Butler, S.G., Stuart, A., Pressman, H. et al. Preliminary Investigation of Swallowing Apnea Duration and Swallow/Respiratory Phase Relationships in Individuals with Cerebral Vascular Accident. Dysphagia 22, 215–224 (2007). https://doi.org/10.1007/s00455-007-9077-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-007-9077-4