Abstract
The purpose of this retrospective study was to compare functional dysphagia outcomes following inpatient rehabilitation for patients with brain tumors with that of patients following a stroke. Group 1 (n = 24) consisted of consecutive admissions to the brain injury program with the diagnosis of brain tumor and dysphagia. Group 2 (n = 24) consisted of matched, consecutive admissions, with the diagnosis of acute stroke and dysphagia. Group 2 was matched for age, site of lesion, and initial composite cognitive FIM score. The main outcome measures for this study included the American Speech-Language-Hearing Association (ASHA) National Outcome Measurement System (NOMS) swallowing scale, length of stay, hospital charges, and medical complications. Results showed that swallowing gains made by both groups as evaluated by the admission and discharge ASHA NOMS levels were considered to be statistically significant. The differences for length of stay, total hospital charges, and speech charges between the two groups were not considered to be statistically significant. Three patients in the brain tumor group (12.5%) demonstrated dysphagia complications of either dehydration or pneumonia during their treatment course as compared to 0% in the stroke group. This study confirms that functional dysphagia gains can be achieved for patients with brain tumors undergoing inpatient rehabilitation and that they should be afforded the same type and intensity of rehabilitation for their swallowing that is provided to patients following a stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
More than 17,000 people each year in the United States are diagnosed with a brain tumor [1]. Since the mid-1970 s, the worldwide incidence of brain tumors has increased. This increase is thought to be related to advancements in diagnosis and an increase in environmental risk factors [2]. Preoperative brain imaging and surgical improvements have reduced the mortality rate during surgery for patients with a brain tumor, and, with these improvements, patients are surviving and may require rehabilitation in order to maximize their function [3].
Brain tumors may be classified as primary or secondary. Primary brain tumors originate from brain tissue. There are several types of primary brain tumors and they may also be classified as benign and malignant [1,2,3,4]. Secondary brain tumors are tumors that represent a cancer that has spread from another part of the body to the brain. Secondary brain tumors are not the same as primary brain tumors; the cancer that metastasizes to the brain is the same disease as the original primary cancer site [1,5].
Symptoms of brain tumors are highly variable and are dependent on the location and size of the tumor. Several case studies have reported dysphagia as a primary or secondary complaint in patients with brain tumors [6,7,8]. Mukand et al. [9] conducted a study investigating the common neurologic problems in adults with brain tumors admitted for inpatient rehabilitation. In that study, they found that 26% of their patients with brain tumors also presented with dysphagia. Newton et al. [10] reported that patients with a primary brain tumor with dysphagia are likely to have impairment of swallowing that is greater than would be expected from the degree of their complaints and therefore are at risk for aspiration and nutritional compromise. Difficulty with swallowing, or dysphagia, may also occur as a secondary complication following surgery to remove the brain tumor [10]. Dysphagia may in turn lead to further complications such as pneumonia, dehydration, or malnutrition and may result in the need for a feeding tube [11,12,13,14,15,16,17,18]. Fenton et al. [19] evaluated 61 patients with tumors in the jugular foramen. They concluded that patients with brain tumors who were introduced to swallowing rehabilitation techniques prior to surgery had less postoperative morbidity. The goals of dysphagia treatment are to return the individual to safe oral feeding and to prevent any medical complications [20].
Previous research has shown that patients with brain tumors are able to make functional gains during rehabilitation [9,21,22]. An outcome study conducted by O’Dell et al. [21] evaluated the overall functional gains made by persons with a brain tumor undergoing rehabilitation. The Functional Independence Measure (FIM) was utilized and compared the gains of patients with a brain tumor with patients following a stroke. They found that gains made by both groups for their overall rehabilitation were similar. At present, no studies have been completed specifically to evaluate dysphagia treatment outcomes in patients with brain tumors.
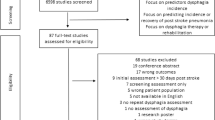
The purpose of this retrospective study was to compare the functional dysphagia treatment outcomes following inpatient rehabilitation for patients with brain tumors to patients who were status post acute stroke. The stroke group was chosen for comparison as these patients are very likely to receive dysphagia treatment during inpatient rehabilitation. The general hypothesis of this study is that patients with brain tumors will make functional swallowing gains similar to those of patients status post acute stroke undergoing inpatient rehabilitation when measurements are controlled for age, site of lesion, and initial level of cognitive functioning. Cognitive functioning was controlled for in this study because previous research has demonstrated a relationship between swallow outcomes and cognitive abilities [23,24].
Method
Subjects
Subjects were divided into two groups. Group 1 was obtained first and consisted of consecutive admissions with the diagnosis of a brain tumor and dysphagia. Group 2 subjects were consecutive acute stroke admissions (less than six weeks post onset) who were screened and, if they met the study criteria of presenting with dysphagia, they were matched to one of the subjects in group 1. Patients were matched between the two groups for age (+/−5 years), initial FIM score (+/−5 points), and hemisphere involvement (left, right, or brainstem). Matching according to these criteria was achieved for all patients with the exception of two younger brain tumor patients, aged 21 and 22 years. To compensate, these patients were matched with two slightly older stroke patients with matching FIM scores and lesion sites. The 21-year-old patient was matched to a 30 year old, and the 22 year old to a 37 year old.
Procedure
Retrospective chart reviews were completed on all patients who were admitted to the rehabilitation hospital over a 12-month period of time. This facility’s institutional review board approved this study protocol. A speech-language pathologist collected the data. A review of the medical chart included an assessment of diet and supervision level, the type of dysphagia treatment provided, amount of time dedicated to dysphagia treatment, number and type of swallowing instrumental assessments provided, dysphagia complications, length of stay, and hospital charges. Dysphagia complications were tracked for malnutrition, dehydration, and aspiration pneumonia. Site of lesion was confirmed by radiographic imaging and clinical findings reported by physicians in the medical charts.
Diet levels were classified as regular, modified (change in solid food texture and/or liquid consistency), therapeutic feedings, or NPO (nil per os). Supervision levels were classified as independent (patient consistently and independently utilized swallowing safety strategies), supervision (patient required cues or instruction 10%–25% of the time to utilize swallow safety strategies), or dependent (patient required cues or instruction 25%–100% to utilize swallow safety strategies).
Initial and discharge scores for swallowing abilities were also assigned utilizing the American Speech-Language-Hearing Association (ASHA) National Outcome Measurement System (NOMS) swallowing level scale developed by the National Center for Treatment Effectiveness in Communication Disorders. The ASHA NOMS swallowing level scale is a multidimensional tool designed to measure both the supervision level required and diet level by assigning a single number between 1 and 7. The patient’s specific diet level and level of supervision were used to assign the ASHA NOMS swallowing scale. Initial diet and supervision levels were documented within 48 hours of admission and discharge diet and supervision levels were documented within 24 hours prior to discharge. Therapists assigning the ASHA NOMS swallowing level had successfully passed the national certification test. Written permission was obtained from the American Speech-Language-Hearing Association to use this outcome measure for this project. See Figure 1 for the ASHA NOMS swallowing scale [25].
The composite initial cognitive Functional Independent Measure (FIM) scores (social interaction, memory, problem solving, comprehension, and expression) were also collected. The cognitive FIM scores are a subset of the complete FIM scale. The cognitive FIM scores range from 5 to 35 points [26]. Therapists who had successfully passed the Uniform Data Source certification test assigned the composite cognitive FIM scores within 24 hours of admission.
Types of dysphagia treatment were divided into three categories: compensatory treatment (diet modification, positioning strategies, or feeding strategies), swallowing rehabilitation/strengthening exercises, and combination of compensatory strategies and swallowing rehabilitation/strengthening exercises. Therapy time spent on dysphagia treatment (direct and indirect) was also recorded for both groups. Therapy time was categorized as 0, 15, 30, 45, and 60 minutes dedicated to dysphagia treatment. Patients typically receive a total of 60 minutes of speech and language therapy daily to address communication and feeding goal areas at this inpatient rehabilitation facility.
The number and type of instrumental assessment of the swallow were also recorded. For the purpose of this study, an instrumental assessment of the swallow was referred to as either the videofluoroscopic swallow study (VFSS) or the video nasal endoscopic exam of the swallow (VEES) [27]. Patients were referred for a video nasal endoscopic swallow evaluation instead of a videofluoroscopic swallow study when a vocal pathology was suspected. The speech-language pathologists completing either the VFSS or the VEES had successfully completed the organizational competency training program. Analysis of the instrumental assessment involved only a review of the written report. The written report includes an evaluation of bolus flow for laryngeal penetration and aspiration. Additionally, if a patient presented with laryngeal penetration or aspiration, appropriate compensatory and postural strategies were introduced during the examination in order to eliminate the penetration and/or aspiration. These compensatory and postural strategies and their effectiveness were documented in the report. If the compensatory and postural strategies were not successful in eliminating the aspiration or if the laryngeal penetration was greater than trace amounts and did not clear the airway, then patients were restricted from consuming that particular consistency.
Data Analyses
To compare for group homogeneity in regards to age and initial FIM score, t-tests were completed. The McNemar test, a nonparametric test designed for comparison of nominal outcomes, was completed regarding diet level and supervision level. One way analysis of variance (ANOVA) was performed in order to determine if there was a difference in the ASHA NOMS, cognitive FIM, length of stay, and hospital charges between the two groups. Chi-squared tests were applied to test for differences in treatment types (compensatory, strengthening, both, or none) and for differences in referral type (referred for instrumental assessment vs. not referred).
Results
Subjects
A total of 38 patients over a 12-month period were admitted to the freestanding rehabilitation hospital with a diagnosis of a brain tumor. Of those 38 patients, 63% (24 patients) also were diagnosed with dysphagia. Over the same 12-month period, a total of 329 patients were admitted to the freestanding hospital with a diagnosis of a CVA. Of those 329 patients, 72.9% (240 patients) were also diagnosed with dysphagia. A subgroup of those CVA patients was matched to the brain tumor groups and was the subject of this investigation. See Table 1 for the subjects’ age, initial cognitive FIM score, and hemisphere involvement for both groups. Group 1 (the brain tumor group, n = 24) ranged in age from 21 to 90 years with a mean of 58.79 years (±17.8 years). Group 2 (the stroke group, n = 24) ranged in age from 30 to 88 years with a mean of 60.5 years (± 15.40 years). A two-sample t-test revealed that the age difference between the two groups was not statistically significant (t = 0.29, p = 0.77). Initial composite cognitive FIM scores for group 1 range was from 6 to 27 with a mean of 14.83 (±6.51) and group 2 range was from 6 to 27 with a mean of 15.46 (±5.76). A two-sample t-test revealed that the differences between the two groups for initial composite cognitive FIM scores were not statistically significant (t = 0.35, p = 0.726).
In each group, 19 patients demonstrated right hemisphere involvement, 4 patients left hemisphere involvement, and 1 patient brainstem involvement. All 24 patients in the brain tumor group had radiographic imaging confirming site of lesion, and 23/24 of the patients in the stroke group had radiographic imaging confirming site of lesion. The one subject in the stroke group who did not have radiographic imaging had his stroke/hemisphere involvement diagnosed based upon clinical findings.
In group 1, 83.3% (20/24) had primary brain tumors and 16.6% had metastatic tumors. Classification of the primary brain tumors was as follows: glioma 15% (3/20), glioblastoma 35% (7/20), astrocytoma 15% (3/20), meningioma 15% (3/20), cyst 10% (2/30), and other 10% (2/20). Twenty percent of the primary brain tumors were classified as benign and 80% were classified as malignant. For the secondary brain tumors, three of the cases were metastasis from the lungs and one from the skin. Surgery for brain tumor resection occurred in 87.5% (21/24) of the patients prior to rehabilitation. Other medical treatment with the brain tumor group that was initiated immediately prior to and during rehabilitation included radiation therapy [37.5% (9/24)] and chemotherapy [10% (2/24)]. One subject in the brain tumor group did not receive any surgery, radiation therapy, or chemotherapy. Many of the patients underwent one or more treatment modalities at a time. Additionally, two of the patients were scheduled to receive radiation therapy and one patient was to receive chemotherapy after completion of their inpatient rehabilitation. In group 2, 83.3% (20/24) of the subjects had an ischemic stroke and 16.6% (4/24) had a hemorrhagic stroke.
Diet and Supervision Levels
Descriptive diet levels for each study group on admission and at discharge are represented in Table 2. Upon admission, 29% of the patients with brain tumors were eating a regular diet compared with 8% of the patients with stroke. Upon discharge, 50% of the patients in both groups were able to safely consume a regular diet. McNemar tests demonstrated that the change in the percentage of stroke patients who could eat a regular diet between admission and discharge was highly significant (p = 0.002), but the change among patients with a brain tumor was only marginally nonsignificant (p = 0.06).
Supervision level for feeding for both groups as well as composite cognitive FIM scores are represented in Table 3. At the time of discharge, 33% of the patients in the brain tumor group were independent for their feeding supervision level compared with 46% of the patients in the stroke group. McNemar tests showed that the change from admission to discharge for supervision level was significant for both patients with a brain tumor (p = 0.008) and for patients following a stroke (p = 0.002).
ASHA NOMS, Cognitive FIM Scores, Length of Stay, and Hospital Charges
The ASHA NOMS incorporates a single score between 1 and 7 that accounts for both the diet level and supervision level. The mean admission ASHA NOMS swallowing rating for the brain tumor group was 3.87 (±1.517) and for the stroke group was 3.74 (±1.356). The difference between the mean admission ASHA NOMS swallowing ratings for each group was not statistically significant (t = 0.35, p = 0.726). The mean discharge ASHA NOMS swallowing rating for both the brain tumor and the stroke group was 5.0 (brain tumor ± 1.567; stroke group ± 1.834). Gains made by both groups as evaluated by the difference in mean admission and discharge ASHA NOMS levels were statistically significant (ANOVA, brain tumor group F = 6.18, p = 0.017 and stroke control group F = 7.03, p = 0.011). The differences between the discharge composite FIM scores between the two groups were not considered to be statistically significant (t = −0.58, p = 0.568).
The average length of stay for the brain tumor group was 21.71 days (±12.03 days) and for the stroke group 28.79 days (±15.30 days). A one-way ANOVA showed that the difference in the length of stay between the two groups was not statistically significant (F = 3.18, p = 0.081). See Table 4 for hospital charges associated with the two groups. A one-way ANOVA demonstrated that the total hospital charges, speech charges alone, and average daily hospital charges between the two groups were not statistically significant.
Treatment Type and Time
Types of treatment received by the two groups are shown in Table 5 . For the brain tumor group, 71% of the patients received treatment for compensatory strategies only while 29% of the patients received treatment for both compensatory strategies and swallowing rehabilitation/strengthening exercises. In the stroke group, 50% of the patients received treatment for compensatory strategies only and 42% received treatment for both compensatory strategies and swallowing rehabilitation/strengthening exercises. A 2 × 2 chi-square was completed for treatment type after discarding the “strengthening” and “none” categories for the stroke group; the results were nonsignificant (χ2 = 1.30, df = 1, p = 0.25).
Treatment time dedicated to dysphagia treatment is given in Table 6. In both groups, the majority of patients had 30 minutes or 50% of their treatment time dedicated to dysphagia treatment. A cross tabulation and the Pearson chi-square were completed for treatment time and the results were nonsignificant (p = 0.775), indicating no dependence between treatment time and diagnosis. One patient in the stroke group received no treatment as he declined to participate in dysphagia treatment. This patient was included in this study since he met the criteria of stroke and dysphagia diagnosis and the matching criteria (consecutive admission, age, initial FIM score, and hemisphere involvement).
Instrumental Assessments and Dysphagia Complications
A videofluoroscopic swallow study or a video nasal endoscopic swallow evaluation was recommended and completed in 62.5% (15/24) of the patients with brain tumors and 92% (22/24) of the patients with stroke. See Tables 7 and 8 for results of the instrumental assessments for both groups. Chi-squared analysis showed the differences in the initial referral patterns to be significant (χ2 = 4.55, df = 1, p = 0.03). A followup or second instrumental assessment was recommended and completed with nine of the patients in the brain tumor group and with eight of the patients in stroke group. A second instrumental assessment was recommended when patients demonstrated aspiration or were determined to be at high risk for aspiration during their initial instrumental assessment. Overall, aspiration of liquids and/or solids was observed in seven of the patients in the brain tumor group and in eight patients in the stroke group. In the brain tumor group, all seven of the patients demonstrated aspiration in the initial instrumental assessment with no aspiration observed in the followup instrumental assessment. In the stroke group, all eight patients demonstrated aspiration in the initial instrumental assessment and two of these patients aspirated in the followup instrumental assessment.
Three patients in the brain tumor group (12.5%) developed dysphagia complications of either dehydration or pneumonia during their treatment course compared with 0% in the stroke group. None of the patients in either group presented with malnutrition.
Discussion
This study demonstrates that, with treatment, patients with brain tumors make advances in swallowing function similar to the gains achieved by patients status post acute stroke. In a previous study, O’Dell et al. [21] found that overall functional gains, as measured by the FIM, were similar in patients with brain tumors compared with those achieved in patients after stroke. The limitation of the O’Dell et al. [21] study was that the FIM does not provide specific information on dysphagia treatment outcomes. In the current study, functional gains in swallowing as measured by the ASHA NOMS were also the same between the two groups.
Even though this current research found similar gains in the area of swallowing and supervision among patients with brain tumors and patients with stroke during their inpatient rehabilitation stay, some interesting differences were also present. The difference in the length of stay between the two groups was not considered statistically significant. However, one may argue that the difference in length of stay of approximately seven days may be considered to be clinically significant, especially as the majority of the patients with a brain tumor in this current study had the malignant form and having seven fewer days in the hospital may be considered important from a quality of life standpoint.
The referral for an instrumental assessment of swallowing was another difference noted between the two groups. In the brain tumor group, only 62.5% of the patients were referred for an instrumental assessment compared with 92% of the patients in the stroke group. This difference in referral for an instrumental assessment may be attributed to a reduced recognition of dysphagia as a potential complication in the brain tumor population and/or a heightened recognition of dysphagia in the stroke group population. The differences in referral for an instrumental assessment from this study appears also to be supported by previous research completed by Newton et al. [10]. They reported that patients with a primary brain tumor and dysphagia are likely to have impairment of swallowing not in proportion to their complaints.
This current study was designed to control for cognitive ability in the two groups. It was interesting to note that both groups in this study exhibited similar gains in composite cognition FIM scores as well as in their ability to swallow and the supervision level required during oral intake. Even though the primary focus of this research project was not to evaluate the relationship between cognition and chewing/swallowing ability and supervision level, this secondary finding provides additional support to previous research showing a relationship between dysphagia treatment outcomes with chewing/swallowing and cognitive FIM scores [23,24].
In this study, 63% of patients with a brain tumor admitted to the rehabilitation hospital presented with dysphagia: a higher incidence of dysphagia than the 26% reported by Mukand et al. [9]. The difference between the two studies may simply reflect a difference in the shorter timeframe in which this current study sample was obtained as it evaluated 38 patients over 12 months compared with 51 patients over 8 years in the Mukand et al. study [9]. With a shorter timeframe, there may have been more uniformity in the diagnosis and treatment of dysphagia and/or a heightened sensitivity to the signs and symptoms of dysphagia in the admitting clinicians that accounts for the differences in the percentage of patients noted presenting with dysphagia.
Conclusion
Patients with brain tumors should be afforded the same type and intensity of rehabilitation for their swallowing that is provided to patients following a stroke since similar gains in function can be demonstrated during inpatient rehabilitation. Functional dysphagia gains as measured by the ASHA NOMS swallowing level scale were made by patients with brain tumors undergoing inpatient rehabilitation and were similar to those made by patients status post acute stroke matched by age, site of lesion, and admission composite cognitive FIM score. It is important for the rehabilitation team to recognize the presence of dysphagia in patients with brain tumors and the potential for functional rehabilitation of the swallow during inpatient rehabilitation. Future research should focus on comparing long-term dysphagia outcomes in these patient populations.
References
National Cancer Institute: What you need to know about brain tumors. NIH Publication No. 95-1558, September 28, 1998
FG Davis BJ McCarthy (2000) ArticleTitleEpidemiology of brain tumors. Curr Opin Neurol 13 635–640 Occurrence Handle1:STN:280:DC%2BD3M7jtVyltA%3D%3D Occurrence Handle11148662
WL Lanier (2001) ArticleTitleBrain tumor resection in the awake patient. Mayo Clin Proc 76 670–672 Occurrence Handle1:STN:280:DC%2BD3MzptVGnug%3D%3D Occurrence Handle11444397
EC Holland (2001) ArticleTitleBrain tumor animal models: importance and progress. Curr Opin Oncol 13 143–147 Occurrence Handle1:STN:280:DC%2BD3Mzot12muw%3D%3D Occurrence Handle11307055
TY Poussaint (2001) ArticleTitleMagnetic resonance imaging of pediatric brain tumors. State of the art. Top Magn Reson Imaging 12 411–433 Occurrence Handle1:STN:280:DC%2BD3MnpvV2jsw%3D%3D Occurrence Handle11744878
Y Frank SB Schwartz NE Epstein HR Bereford (1989) ArticleTitleChronic dysphagia, vomiting and gastroesophageal reflux as manifestation of a brain stem glioma: a case report. Pediatr Neurosci 15 265–268 Occurrence Handle1:STN:280:By6B3cvlvVQ%3D Occurrence Handle2488955
A Straube TN Witt (1990) ArticleTitleOculo-bulbar myastenic symptoms as the sole sign of tumor involving or compressing the brain stem. J Neurol 237 369–371 Occurrence Handle1:STN:280:By6C3MnjsF0%3D Occurrence Handle2277271
M Hensel K Haake S Vogel W Flugel D Krausch WJ Kox (1997) ArticleTitleManagement of swallowing disorders and chronic aspiration by glottic closure procedure. J Neurosurg Anesthesiol 9 273–276 Occurrence Handle1:STN:280:ByiA1czmtVQ%3D Occurrence Handle9239592
JA Mukand DD Blackinton MG Crincoli JJ Lee BB Santos (2001) ArticleTitleIncidence of neurologic deficits and rehabilitation of patients with brain tumors. Am J Phys Med Rehabil 80 346–350 Occurrence Handle1:STN:280:DC%2BD3M3kvFGmtw%3D%3D Occurrence Handle11327556
HB Newton C Newton D Pearl T Davidson (1994) ArticleTitleSwallowing assessment in primary brain tumor patients with dysphagia. Neurology 44 1927–1932 Occurrence Handle1:STN:280:ByqD383itFY%3D Occurrence Handle7936249
MF Brin D Younger (1988) ArticleTitleNeurologic disorders and aspiration. Otolaryngol Clin North Am 21 692–699
JA Logemann BR Pauloski AW Rademaker LA Colangelo (1997) ArticleTitleSpeech and swallowing rehabilitation for head and neck cancer patients. Oncology 11 651–664 Occurrence Handle1:STN:280:ByiA3czks1w%3D Occurrence Handle9159792
DH Barer (1989) ArticleTitleThe natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry 52 236–241 Occurrence Handle1:STN:280:BiaC1MbgtVw%3D Occurrence Handle2564884
HM Finestone LS Greene–Finestone ES Wilson RW Teasell (1995) ArticleTitleMalnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil 76 973–976
MA Holas KL Depippo MJ Reding (1994) ArticleTitleAspiration and relative risk of medical complications following stroke. Arch Neurol 51 1051–1053 Occurrence Handle1:STN:280:ByqD3s7ntVw%3D Occurrence Handle7945003
ER Johnson SW McKenzie A Sievers (1993) ArticleTitleAspiration pneumonia in stroke. Arch Phys Med Rehabil 74 973–976 Occurrence Handle1:STN:280:ByyA1Mzkt1A%3D Occurrence Handle8379846
D Kidd J Lawson R Nesbitt J MacMahon (1995) ArticleTitleThe natural history and clinical consequences of aspiration in acute stroke. QJM 88 409–413 Occurrence Handle1:STN:280:ByqA2snislw%3D Occurrence Handle7648232
PB Terry SD Fuller (1989) ArticleTitlePulmonary consequences of aspiration. Dysphagia 3 179–183 Occurrence Handle1:STN:280:By%2BA3MrpsFQ%3D Occurrence Handle2639773
JE Fenton H Brake A Shirazi MS Mendelsohn M Atlas PA Fagan (1996) ArticleTitleThe management of dysphagia in jugular foramen surgery. J Laryngol Otol 110 144–147 Occurrence Handle1:STN:280:BymA3cnit10%3D Occurrence Handle8729498
SE Langmore (1995) ArticleTitleEfficacy of behavioral treatment for oropharyngeal dysphagia. Dysphagia 10 259–262 Occurrence Handle1:STN:280:BymD3Mbks10%3D Occurrence Handle7493507
M O’Dell K Barr D Spanier R Warnick (1998) ArticleTitleFunctional outcome of inpatient rehabilitation in persons with brain tumors. Arch Phys Med Rehabil 79 1530–1534 Occurrence Handle1:STN:280:DyaK1M%2FnslWisg%3D%3D Occurrence Handle9862294
M Huang D Cifu L Keyser–Marcus (1998) ArticleTitleFunctional outcomes after brain tumor and acute stroke: a comparative analysis. Arch Phys Med Rehabil 79 1386–1390 Occurrence Handle1:STN:280:DyaK1M%2FjslKlsg%3D%3D Occurrence Handle9821898
A Halper L Cherney K Cichowski M Zhang (1999) ArticleTitleDysphagia after head trauma: The effects of cognitive-communicative impairments on functional outcomes. J Head Trauma 14 489–496
C Smith–Hammond RD Horner L Gonzalez–Rothi M Kuchiblatla C Schaver X Kerner (2001) ArticleTitleEffect of cognitive impairment on outcomes among stroke patients with and without dysphagia. Poster presented at the 9th Annual Meeting of the Dysphagia Research Society, October 26–28, 2000, Savannah, GA. Dysphagia 16 152
InstitutionalAuthorNameAmerican Speech-Language Hearing Association National Outcomes Measurements System (NOMS) (1998) Adult Speech-Language Pathology Training Manual. ASHA Rockville MD
RC Fiedler CV Granger (1996) The functional independence measure: a measurement of disability and medical rehabilitation. N Chino JL Melvin (Eds) Functional Evaluation of Stroke Patients. Springer-Verlag Tokyo 75–92
InstitutionalAuthorNameAmerican Speech-Language Hearing Association (1992) ArticleTitleAd hoc committee on advances in clinical practice, instrumental diagnostic procedures for swallowing. ASHA 34 IssueIDSuppl 7 25–33
Acknowledgements
The authors would like to acknowledge Barbara Kremmer, Ph.D., for her statistical support in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
The Dr. Ralph and Marian Falk Medical Research Foundation supported this work. Work completed at Marianjoy Rehabilitation Hospital, Wheaton, Illinois
Rights and permissions
About this article
Cite this article
Wesling, M., Brady, S., Jensen, M. et al. Dysphagia Outcomes in Patients with Brain Tumors Undergoing Inpatient Rehabilitation . Dysphagia 18, 203–210 (2003). https://doi.org/10.1007/s00455-002-0098-8
Issue Date:
DOI: https://doi.org/10.1007/s00455-002-0098-8