Abstract
Integrin receptors mediate the interactions between cells and the extracellular matrix. They not only provide anchorage and a physical linkage to the matrix but also participate in cell signaling and the regulation of diverse cellular functions. In the epidermis of the skin, integrins are essential for tissue structure and integrity, and, under normal homeostatic conditions, the β1 subunit specifically controls the balance between proliferation and terminal differentiation. Integrin expression can also dynamically respond to changes in the cell’s environment, and integrin-mediated adhesion is required for keratinocyte migration and re-epithelialization during wound repair. Importantly, integrins participate in keratinocyte mechanotransduction and could potentially regulate cell behavior within the altered mechanical microenvironment of a wound. While the complete functions of integrin receptors in cutaneous wound healing have yet to be determined, recent evidence suggests that cell–matrix interactions are perturbed in chronic and non-healing wounds. Integrins may therefore be a potential therapeutic target for improving wound repair and tissue regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skin is the largest organ in the human body and participates in vital physiologic activities, including vitamin D synthesis and sensory perception, but its most important function is to provide a barrier from the external environment and protect against pathogens, chemicals, mechanical forces, ultraviolet light, and water loss (Nemes and Steinert 1999). The skin consists of two main layers: the dermis, which is responsible for tissue strength and elasticity, and the epidermis, which forms the barrier. The epidermis is a stratified, squamous epithelium that undergoes continuous turnover under normal homeostatic conditions (Blanpain and Fuchs 2009). Similarly, fibroblasts in the dermis synthesize and remodel the extracellular matrix (ECM) to maintain tissue mechanics (Liu and Leask 2013). Upon injury, however, cells within the skin mount a coordinated response to close the wound and repair the damaged tissue (Gurtner et al. 2008). The wound-healing process is therefore critical for restoring the skin’s protective barrier function after injury.
Cutaneous wound healing is a dynamic process of 4 overlapping phases: hemostasis, inflammation, re-epithelialization, and tissue remodeling (Martin 1997). These phases are highly organized and involve complex interactions between cells, signaling molecules and the ECM (Broughton et al. 2006). Within minutes of injury, vasoconstriction occurs, a fibrin clot is formed, there is a release of growth factors such as platelet-derived growth factor (PDGF) and epidermal growth factor (EGF), and inflammatory cells such as monocytes and neutrophils migrate to the wound site (Martin 1997; Gurtner et al. 2008). Over the next 1–3 days, epidermal keratinocytes at the wound margin migrate collectively over the wound bed to re-form the epithelial layer. This process is known as re-epithelialization and is essential for regeneration of a functional epidermis and protection against infection. Finally, fibroblasts in the dermis enter the wound and synthesize and remodel ECM proteins, such as collagen, fibronectin, and elastin, over a period of weeks to months. Fibroblast expression of α-smooth muscle actin (αSMA) also promotes contraction to aid wound closure (Desmoulière et al. 2005). Wound repair is tightly regulated by many factors, including cell–ECM interactions, growth factors and matrix metalloproteinases (MMPs) (Martin 1997; Gurtner et al. 2008). Disruption of these regulatory mechanisms at any stage can lead to chronic or non-healing wounds where inflammation persists and the barrier is compromised (Harding et al. 2002; Brem and Tomic-Canic 2007; Caskey et al. 2014). Factors such as oxygenation, infection, age, and disease state can each hinder the skin’s ability for effective wound repair (Swift et al. 2001; Edwards and Harding 2004; Brem and Tomic-Canic 2007; Bishop 2008).
Chronic wounds, including diabetic, pressure, and venous ulcers, are a major healthcare problem, which affect approximately 6.5 million people and cost over $25 billion per year in the U.S. alone (Sen et al. 2009). In addition to being an economic burden, chronic wounds significantly decrease the quality of life of patients and often lead to infection and further complications. While the underlying causes are complex and involve multiple factors, the ultimate consequence of a chronic wound is an open sore that lacks appropriate protective function and is prone to infection. Defective re-epithelialization of the epidermal layer (i.e. re-establishing barrier function) may be an important contributor to the pathogenesis of non-healing wounds. In particular, integrin-mediated adhesion to the ECM, which is essential for keratinocyte migration (Grose et al. 2002), could be a key player in re-epithelialization and overall wound healing. In this article, we will review the roles of integrin receptors in normal skin homeostasis, mechano-sensing, and repair, as well as their potential involvement in chronic wounds.
Overview of integrin receptors
Integrins are heterodimeric glycoproteins with α and β type I transmembrane subunits that are not covalently bound (Hynes 2002). Their primary function is cell adhesion to the ECM through specific binding of αβ dimers to ECM proteins, such as fibronectin, vitronectin, and collagen. To date, 26 members of the integrin family have been identified, including 18 α subunits and 8 β subunits, and these can form 24 different αβ heterodimers (Hynes 2002). The association of α and β subunits defines their recognition and binding affinity for specific peptide sequences such as the arginine-glycine-aspartic acid (RGD) motif in fibronectin (Pierschbacher and Ruoslahti 1984; Ruoslahti and Pierschbacher 1986). Integrins have a large extracellular domain for ligand binding with a shorter cytoplasmic tail, which interacts with various scaffolding proteins and signaling molecules. Crucially, the cytoplasmic tails are physically linked to cytoskeletal components including F-actin and intermediate filaments, thereby providing a mechanical connection between the ECM and the cell. Integrins mediate fundamental cell–matrix interactions, such as adhesion, polarity, and migration (Hynes 2002). Moreover, they are signaling molecules and transduce both inside out and outside in signals across the plasma membrane. Integrins regulate key processes, such as growth, survival, and differentiation.
Integrin activation, or inside–out signaling, is regulated by the binding of talin to the β subunit. Talin binding causes a conformational change in the integrin that increases the affinity of the extracellular domain for a particular ligand (Tadokoro et al. 2003). However, integrins can also bind ligands without this conformational change (Xiong et al. 2001; Adair et al. 2005). Recently, it has been proposed that kindlins can also activate integrins and/or co-activate with talin (Calderwood et al. 2013), and mutations in Kindlin-1 cause the blistering skin disease, Kindler Syndrome (Siegel et al. 2003). Talin also links integrins to the F-actin cytoskeleton and other scaffolding proteins and facilitates the initial stages of integrin clustering (Hynes 2002). Thus, talin is a central regulator of integrin function and sensing of extracellular signals.
Outside–in signaling from the ECM to the cell begins with the binding of ligands to the integrin receptors, which progressively cluster together and eventually form large signaling complexes known as focal adhesions. A key first step in this process is binding of talin to F-actin filaments and recruitment of vinculin. Vinculin is a scaffolding protein that also links integrins with F-actin filaments and further promotes integrin clustering via positive feedback from cytoskeletal tension (Humphries et al. 2007). Integrin clustering leads to the formation of nascent adhesions, which then mature into larger focal adhesions through the recruitment of adapter proteins, like paxilllin, and signaling molecules, such as focal adhesion kinase (FAK), integrin-linked kinase (ILK), and Src (Hynes 2002).
FAK transmits signals from focal adhesions into downstream pathways through phosphorylation at multiple sites, including auto-phosphorylation at Tyr397 (Mitra et al. 2005). The mitogen-activated protein kinase (MAPK) signaling cascade is among the most characterized downstream pathways of integrins and regulates proliferation and differentiation in a number of cell types (Schlaepfer et al. 1994; Zhao et al. 1998). Ligation of β1 integrins causes activation of Ras and hence increases tyrosine phosphorylation for MAPK signaling proteins ERK1/2, while disruption of binding to β1 causes a reduction in signaling (Schlaepfer et al. 1994; Schlaepfer and Hunter 1997; Zhu et al. 1999). Integrins can also induce and amplify the JAK/STAT pathway (Brizzi et al. 1999). It has also been suggested that FAK plays a role in talin recruitment (Lawson et al. 2012).
Rho GTPases are another group of downstream effectors of integrin-mediated adhesion and classic regulators of the actin cytoskeleton. While RhoA promotes actin polymerisation and acto-myosin contractility, Cdc42 and Rac1 control membrane protrusion and lamellipodia formation (Ridley and Hall 1992; Nobes and Hall 1995). During early stages of cell adhesion, integrin binding transiently inhibits RhoA activation in a Src- and p190GAP-dependent manner; however, at later time points RhoA activity is increased (Arthur et al. 2000). Conversely, Cdc42 and Rac1 are rapidly activated by integrin-mediated adhesion and are required for cell spreading (Clark et al. 1998). Rho GTPases reciprocally regulate focal adhesion assembly. For example, inhibition of RhoA activity blocks focal adhesion maturation via reduced cytoskeletal tension (Ridley and Hall 1992; Chrzanowska-Wodnicka and Burridge 1996).
There is significant crosstalk between integrins and growth factor signaling. Integrin receptors control intracellular signaling cascades that intersect with various receptor tyrosine kinases (RTKs). Growth factors such as epidermal growth factor (EGF), fibroblast growth factor (FGF), and keratinocyte growth factor (KGF) are ligands for RTKs that activate similar downstream targets, such as MAPK and JAK/STAT cascades. Integrins can also regulate EGF signaling by direct association with the epidermal growth factor receptor (EGFR) via interactions with Rab-coupled protein during receptor recycling (Caswell et al. 2008). Integrins cooperate with growth factors and enhance their secretion. In tumors, αvβ3 controls vascular endothelial growth factor (VEGF) production, which causes neovascularization and increased tumor growth (De et al. 2005). VEGF has also been shown to enhance adhesion and increase migration in endothelial cells through integrin αvβ3 and PI3K signaling (Byzova et al. 2000).
It is important to note that, in addition to focal adhesion interactions with F-actin, integrins also provide linkage between the ECM and the keratin cytoskeleton via hemidesmosomes, which are dense adhesive plaques present on the basal surface of epithelial cells. They consist of α6β4 integrins, along with BP230, CD151, type XVII collagen, and plectin, which bind keratin bundles to the large cytoplasmic tail of the β4 subunit (Borradori and Sonnenberg 1999). Hemidesmosomes provide stable anchorage of epithelia to the underlying basement membrane. In addition, recent evidence suggests that they participate in signaling to downstream pathways, such as MAPK and protein kinase C (PKC) (Osmanagic-Myers et al. 2006). An in depth review of hemidesmosomes can be found in the article by Walko and colleagues in this issue of Cell and Tissue Research.
Integrin expression and function in the intact epidermis
The epidermis is a stratified epithelium in which cell function is spatially and temporally defined. Keratinocytes within the basal layer attach to the basement membrane, a fibrous network consisting predominantly of laminin 332, type IV collagen, and type VII collagen (Timpl 1989), via integrin-containing hemidesmosomes (Dowling et al. 1996; DiPersio et al. 2000). The basal keratinocytes are proliferative and specifically express keratins 5 and 14 (Moll et al. 1982). Periodically, these cells withdraw from the cell cycle and undergo a program of terminal differentiation as they detach from the basement membrane and move upwards through the suprabasal layers towards the surface of the epidermis (Watt and Green 1982; Watt 1989). As cells move up through the suprabasal and granular layers, they downregulate their integrins and begin to express components of the cornified envelope, such as involucrin, filaggrin, and loricrin (Watt 1983). When keratinocytes reach the outermost layer, the stratum corneum, they become flattened and anuclear and form a cornified envelope of proteins that are highly cross-linked by transglutaminase I (Rice and Green 1977; Rice and Green 1978). Keratinocytes are eventually shed from the surface through desquamination, and the loss of terminally differentiated cells is balanced by proliferation within the basal layer in order to maintain homeostasis (Blanpain and Fuchs 2009).
Integrin expression within the epidermis is normally confined to the basal layer but may be upregulated in the suprabasal layers in inflammatory conditions, such as psoriasis and wound healing (Hertle et al. 1992). The major heterodimers expressed by keratinocytes include α2β1, α6β4, and α3β1 (Peltonen et al. 1989; Hertle et al. 1991; Adams and Watt 1991; Cavani et al. 1993). The α6β4 dimer is a hemisdesmosomal receptor that binds laminin 332 and links the ECM to the keratin cytoskeleton (Dowling et al. 1996). The β1-containing integrins, such as the collagen binding α2β1 and laminin 332 binding α3β1 receptors, are constitutively expressed and can form focal adhesion complexes that link to the F-actin cytoskeleton (Carter et al. 1991; Hertle et al. 1991). Also expressed at low levels are the αvβ5 receptors for vitronectin (Adams and Watt 1991), and, in wound-healing conditions, α9β1, α5β1, and αvβ6 are all increased (Hertle et al. 1992; Larjava et al. 1993; Cavani et al. 1993; Singh et al. 2009). The αvβ6 receptor is also elevated in squamous cell carcinoma (Thomas et al. 2001). This pattern of integrin expression varies throughout the skin, and, with increasing age, there is an overall reduction in the expression of β1 integrins (Giangreco et al. 2010). Integrins are essential for anchorage of the epidermis to the basement membrane, and loss or malfunction causes blistering skin diseases such as Kindler Syndrome (Siegel et al. 2003; White and McLean 2005) and various forms of Epidermolysis Bullosa (Georges-Labouesse et al. 1996; Pulkkinen et al. 1998; Kiritsi et al. 2013).
In addition to their function as a mechanical linker, integrins play an import role in signaling and the regulation of keratinocyte behavior. Ligation of β1 integrins by ECM proteins maintains keratinocytes in an undifferentiated state (Adams and Watt 1989; Jones and Watt 1993; Watt et al. 1993), while loss of adhesion, either in suspension culture or on micro-patterned surfaces, rapidly induces terminal differentiation (Watt et al. 1988; Adams and Watt 1989; Connelly et al. 2010). Deletion of β1 integrins in the adult mouse epidermis similarly causes epidermal thinning and reduced proliferation (Lopez-Rovira et al. 2005). Furthermore, β1 and α6 are elevated in the epidermal stem cell population and can be used to isolate stem cells either by flow cytometry or adhesion to ECM-coated surfaces (Jones and Watt 1993; Li et al. 1998). Downstream of integrins, MAPK mediates stem cell proliferation (Zhu et al. 1999), while the actin cytoskeleton and AP-1 transcription factors control terminal differentiation (Gandarillas and Watt 1995; Connelly et al. 2010). Integrin expression can also be tuned by c-Myc, a key upstream regulator of epidermal cell fate and adhesion (Frye et al. 2003). In contrast to the role of the β1 integrins, the laminin-specific subunits, α3, α6, and β4, have a milder effect on cell behavior. Loss of these integrins alone or in combination results in epidermal blistering and apoptosis, while tissue development, proliferation, and differentiation are all normal (DiPersio et al. 1997; DiPersio et al. 2000). Together, these findings indicate that the β1 integrin directly regulates cell signaling and fate within the epidermis, and that the laminin-specific receptors are important for tissue mechanics and integrity.
The role of integrins in wound healing
Acute wound healing
Integrin-mediated adhesion to the ECM plays a vital, yet complex role in cutaneous wound healing. Integrins regulate the activity of multiple cell types at each stage of healing, but are particularly important for re-epithelialization of the epidermal layer. During this phase of healing, keratinocytes at the wound margin migrate over newly deposited granulation tissue and expand in number to repair the damaged epidermis, and efficient re-epithelialization is necessary to regenerate a functional barrier and protect the wound from infection. The expression pattern and function of key integrin receptors is summarized in Table 1.
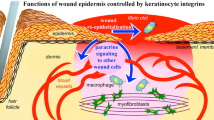
The wound bed ECM is distinctly different from the basement membrane on which keratinocytes normally adhere, and cells adapt their integrin expression profile in response to this new environment (Fig. 1a, b). While the basement membrane comprises laminin 332, collagen type IV, and collagen type VII, the ECM of the wound bed contains high levels of collagen type I, fibronectin, vitronectin, and fibrinogen (Grinnell et al. 1981; Clark et al. 1982). Correspondingly, keratinocytes begin expressing the fibronectin receptor α5β1 and upregulate the vitronectin receptor αvβ5 (Larjava et al. 1993; Cavani et al. 1993) following wounding. However, once re-epithelialization is complete, both basal and suprabasal keratinocytes switch from αvβ5 to αvβ6 expression (Clark et al. 1996). In addition, the laminin 332 receptor α3β1 increases during re-epithelialization, while α6β4-containing hemisdesmosomes are disassembled (Geuijen and Sonnenberg 2002). Once the epidermis closes, it remains hyperproliferative, and the upregulated receptors continue to be expressed in both the basal and suprabasal layers before returning to a normal expression pattern when healing is complete (Hertle et al. 1991; Juhasz et al. 1993). Thus, keratinocyte integrin expression during wound healing is spatially and temporally controlled and correlates with specific phases of tissue repair.
Schematic of integrin expression and mechano-sensing during wound healing. a α3β1 and α6β4 provide stable adhesion to the basement membrane and physically link with the actin and keratin cytoskeletons, respectively. b Following wounding, hemidesmosomes are disassembled, while α3β1, α5β1, and αvβ5 are each upregulated while migrating on newly deposited ECM. c Example of micro-patterned migration assay for studying collective epithelial migration (Costa et al. 2014). d Schematic of mechanical forces involved in collective migration of epithelia, including high ECM traction forces generated by the leader cell and intercellular tension between follower cells
Although the upregulation of fibronectin and vitronectin receptors suggests that these integrins facilitate keratinocyte migration over the wound bed, functional studies have yet to establish a definitive role. In vitro, human keratinocytes adhere to fibronectin via the α5β1 receptor and vitronectin via the αvβ5 (Adams and Watt 1991). Similarly, keratinocytes engage the α5β1 receptor to migrate on fibronectin (Clark et al. 1982; Takashima and Grinnell 1985; Kim et al. 1992), while migration on vitronectin depends on αvβ5 (Kim et al. 1994). Nevertheless, deletion of either the β5 or β6 subunits do not affect normal wound closure in mice (Huang et al. 1996; Huang et al. 2000), suggesting functional redundancy between fibronectin and vitronectin receptors in vivo. Although α5 knockout mice are not viable (Yang et al. 1993), it is likely that αvβ5 or αvβ6 would similarly compensate for deficiencies in the α5β1 in keratinocytes. Recently, studies have further identified the α9β1 receptor, which binds tenascin-C, osteopontin, and fibronectin, as a novel regulator of epidermal proliferation following wounding (Singh et al. 2009).
Like the fibronectin and vitronectin integrins, the contributions of the laminin receptors, α3β1 and α6β4, to wound healing are highly complex. The hemidesmosomal receptor α6β4 maintains stable adhesion of the epidermis to the basement membrane. While overall expression remains stable during wound healing (Larjava et al. 1993), disassembly of these adhesions facilitates keratinocyte migration (Geuijen and Sonnenberg 2002). The function of the α3β1 receptor, however, is less clear. In vitro, laminin 332 and the α3β1 receptor both inhibit keratinocyte motility (O’Toole et al. 1997; deHart et al. 2003; Margadant et al. 2009), while other reports indicate that α3β1 regulates polarization and lamellapodia formation via Rac1 and focal adhesion kinase (FAK) activation (Choma et al. 2004, 2007). In addition, α3 directs the deposition and organization of laminin-332 by keratinocytes (Hamelers et al. 2005). In vivo, however, complete knockout of α3 results in impaired re-epithelialization via altered TGF-β signaling (Reynolds et al. 2008), and conditional deletion within the epidermis only slightly accelerates wound closure (Margadant et al. 2009). The α3β1 receptor has also recently been shown to regulate angiogenesis through mitogen-regulated protein 3 (MRP3), and could further influence the overall healing process by secondary systemic effects (Mitchell et al. 2009). At this point, it is therefore unclear whether the impact of α3β1 on cutaneous wound healing is a direct consequence of altered keratinocyte migration, growth factor signaling, or both, and additional investigation is needed in this area.
In contrast to other subunits, the importance of the β1 integrin is relatively well established. Conditional deletion of the β1 subunit in the mouse epidermis prevents re-epithelialization and inhibits closure of excisional wounds (Grose et al. 2002). This response is due to impaired keratinocyte migration, rather than proliferation, and is associated with a reduction in laminin 332 in the basement membrane. It is likely that the essential role of the β1 subunit in re-epithelialization reflects its ability to bind multiple alpha subunits, including the α2, α3, α5, and α6 dimers. Loss of the α2β1 integrin, which binds fibrillar collagens, has no reported effect on re-epithelialization but increases angiogenesis following wounding (Chen et al. 2002; Grenache et al. 2007). These findings are again in contrast to the in vitro studies, in which the α2β1 receptor is required for keratinocyte adhesion and migration on type I collagen (Grenache et al. 2007), and provide another example of the discrepancies between in vitro and in vivo studies. It is worth noting that some of the differences between in vitro experiments with human cells and in vivo wounding studies in mice may reflect intrinsic differences in wound healing between the two species (Ansell et al. 2012). In mice, the skin is much looser and heals mostly by contraction, while in humans re-epithelialization plays a greater role.
Downstream effectors of integrin receptors, such as focal adhesion signaling molecules and Rho GTPases, have also been implicated in wound re-epithelialization. For example, FAK is required for keratinocyte migration in vitro, yet is dispensable for wound closure in vivo (McLean et al. 2004). In addition, integrin-linked kinase (ILK) regulates epidermal morphogenesis and promotes keratinocyte migration in vitro, and loss of ILK inhibits in vivo wound closure (Lorenz et al. 2007; Serrano et al. 2012). Rho GTPases control cytoskeletal organization and migration in many cell types, including keratinocytes. RhoA activation promotes keratinocyte contractility and migration (Jackson et al. 2011), while Rac1 is required for stable lamellapodia formation in migrating cells (Choma et al. 2004; Tscharntke et al. 2007). Furthermore, loss of Rac1 in the epidermis significantly inhibits wound closure via defects in migration and proliferation (Tscharntke et al. 2007).
Looking beyond re-epithelialization of the epidermis, integrins also regulate the activity of other cells types during wound repair. Conditional deletion of the β1 subunit in dermal fibroblasts significantly inhibits wound closure through TGF-β signaling, and involves reduced fibroblast migration, matrix production, and contractility (Liu et al. 2010). As noted above, mice lacking α2 subunits have no obvious skin abnormalities (Chen et al. 2002); however, loss of the α1 subunit increases type I collagen expression (Gardner et al. 1999). As both α1β1 and α2β1 bind collagen, these receptors could potentially compensate for each other, and it would be interesting to see the consequences of conditionally knocking out both the α1 and α2 subunits. In vitro, dermal fibroblast migration on fibronectin requires both the integrin binding motif and synergy site, specific for α5β1 (Clark et al. 2003). These findings suggest that the inhibitory effect of β1 deletion on fibroblast migration may be attributed to impaired adhesion to fibronectin and collagen. Fibroblasts can also adhere to vitronectin and fibrin through αvβ3 receptors (Gailit and Clark 1996; Gailit et al. 1997), which may support migration through the complex ECM of the wound environment. Finally, angiogenesis within the healing wound is essential for tissue regeneration and depends on integrin-mediated adhesion to the ECM (Herouy et al. 2000; Mitchell et al. 2009). Numerous studies have examined the role of integrins in angiogenesis, and these findings are reviewed in depth elsewhere (Brooks et al. 1994; Stupack and Cheresh 2004; Ramjaun and Hodivala-Dilke 2009).
Chronic wounds
Chronic wounds, such as diabetic and venous ulcers, are a major healthcare problem, which affects approximately 6.5 million people and costs over $25 billion per year in the U.S. (Sen et al. 2009). While the underlying causes are highly complex, integrin-mediated adhesion to the ECM may play an important role. Several studies have demonstrated that both the plasma and the wound bed of diabetic patients with chronic wounds have reduced levels of fibronectin compared to healthy patients (Labat-Robert et al. 1984; Wysocki and Grinnell 1990; Herrick et al. 1992), and fibronectin molecules within the wounds of diabetic patients are more degraded (Grinnell et al. 1992; Wysocki et al. 1993). Similarly, collagen type I and type III are reduced in diabetic mouse models of impaired healing (Caskey et al. 2014). Together, these data suggest that, in chronic wounds, an inability to form a wound bed with the appropriate ECM composition may inhibit cell migration and wound closure.
Studies on the direct role of integrins in chronic wounds, however, are still in their early stages. Loss of integrin α3 results in wound-induced disruption of laminin-332 in the basement membrane and blistering in mice (Longmate et al. 2014), while α3 mutations are associated with mild blistering in human patients (Has et al. 2012). However, there is clear evidence that β6 integrins influence chronic wound development. Targeted overexpression of β6 in the mouse epidermis causes a subset of animals to develop spontaneous, non-healing wounds, consistent with elevated αvβ6 expression in human chronic wounds (Häkkinen et al. 2004). In both instances, upregulation of β6 is associated with enhanced TGF-β signaling (Häkkinen et al. 2004). Conversely, β6 deficiency further inhibits wound closure when challenged with aging or steroid treatment (AlDahlawi et al. 2006). Together, these findings suggest a multi-functional role for the β6 subunit in wound healing in which it may regulate several processes or elicit distinct cellular responses, depending on the context and level of expression. While these results provide preliminary evidence of defects in cell–ECM and integrin-mediated adhesion in chronic, non-healing wounds, additional studies are needed to understand how other integrin receptors may be involved in the pathogenesis of chronic wounds and the mechanisms involved.
Mechano-sensing and wound repair
As integrins are adhesion molecules linked to the cytoskeleton, they play a central role in sensing the physical properties of the extracellular environment. For example, the stiffness of the matrix influences cell migration, with decreasing migration speed and enhanced focal adhesion signaling observed on stiffer substrates (Pelham and Wang 1997). Elevated focal adhesion phosphorylation on stiff substrates also depends on myosin II contractility, indicating that cells mechanically sense their environment through integrins (Pelham and Wang 1997), and matrix elasticity specifically regulates the size and strength of focal adhesions (Choquet et al. 1997; Riveline et al. 2001). Furthermore, matrix mechanics can have a profound impact on cell function. For example, mesenchymal stem cells (MSCs) express tissue-specific markers for bone, muscle and brain according to the elasticity of the underlying matrix (Engler et al. 2006). Increased matrix cross-linking and tissue stiffening is also associated with tumor formation and progression (Levental et al. 2009), and matrix stiffness regulates the invasive behavior of cancer cells via Rho and ERK signaling (Paszek et al. 2005). Thus, integrin-mediated adhesion is a central component of cellular mechanotransduction.
During wound healing, the composition and structure of the ECM changes dramatically from fibrin clot formation to granulation tissue deposition and eventually to tissue remodeling. Such alterations in the ECM likely impact the biophysical and mechanical properties of the tissue and could potentially affect cell behavior. Findings from our laboratory and others indicate that keratinocytes indeed sense and respond to changes in their physical environment. Cell rounding induced by limited adhesion to the ECM promotes terminal differentiation of human keratinocytes via changes in cytoskeletal organization and activation of AP-1 transcription factors (Watt et al. 1988; Connelly et al. 2010). The degree of tethering of ECM proteins similarly affects integrin clustering, which in turn regulates keratinocyte shape and differentiation (Trappmann et al. 2011). In addition, dynamic stresses imposed by stretching activate calcium signaling in human keratinocytes (Tsutsumi et al. 2009). Recent studies also indicate that the keratin cytoskeleton has a significant influence on keratinocyte mechanics and mechanotransduction (Ramms et al. 2013; Seltmann et al. 2013; Gregor et al. 2014), suggesting that both focal adhesions and hemidesmosomes sense mechanical forces within the epidermis.
While it is clear that physical and mechanical cues regulate basic keratinocyte functions (Reichelt 2007; Evans et al. 2013), a direct effect on cell behavior during wound healing has yet to be determined. A significant challenge for these types of studies is the complexity of the wound environment and de-coupling mechanical and structural properties from other factors such as nutrient diffusion and growth factor signaling. Moreover, the dynamic nature of the wound-healing process creates an additional layer of complexity. One approach to overcoming these challenges is to engineer model in vitro systems in which the physical environment can be controlled and studied in a systematic manner. In recent years, many groups have employed micro-patterned ECM surfaces (Chen et al. 1997; McBeath et al. 2004; Thery et al. 2005; Connelly et al. 2010) or hydrogels with tuneable mechanics (Pelham and Wang 1997; Engler et al. 2006; Trappmann et al. 2011; Yang et al. 2014) to study cell–matrix interactions. This approach has recently been extended to studying wound healing and epithelial migration (Vedula et al. 2014), and several investigators have taken advantage of advances in biomaterial science to create dynamically adhesive or stimuli-responsive substrates. Examples of these strategies include selective removal of non-adhesive materials using light or electric potentials (Raghavan et al. 2010; Vignaud et al. 2012), host–guest chemistry (Boekhoven et al. 2013), light-activated de-protection of adhesive ligands (Weis et al. 2013), and click chemistry coupling reactions, such as azide-alkyne addition (Van Dongen et al. 2013). Our group has also developed a novel dynamically adhesive micro-patterned system using photo-activated, thiol-yne reactions (Costa et al. 2014). This strategy can be used to introduce new ECM-mimetic ligands in the presence of cells and activate cell migration into previously non-adhesive regions (Fig. 1c). We believe that these types of systems will be powerful research tools for studying cell migration and wound healing as they allow dynamic control over the cell’s adhesive microenvironment.
Collective cell migration is a fundamental process in which groups of cells migrate together in a coordinated fashion and which occurs in wound healing (Theveneau and Mayor 2013), development (Uriu et al. 2014) and cancer invasion (Gaggioli et al. 2007). Several recent studies have leveraged engineered in vitro systems to study the migration of simple epithelia and gain insight into the regulatory mechanisms governing collective migration. For example, following the release of MDCK cells from micro-stencils, a leader cell initiates migration and generates strong, RhoA-mediated traction forces in the direction of migration (Reffay et al. 2014). Intercellular tension at adherens junctions simultaneously maintains tissue cohesion and pulls follower cells along (Fig. 1d). Interestingly, substrate stiffness reciprocally regulates epithelial migration via myosin II contractility (Ng et al. 2012). Moreover, the response to substrate rigidity depends on the specific integrins involved. In myoepithelial cells, for instance, differences in binding kinetics between α5β1 and αvβ6 determine the level of traction force a cell can generate for a given substrate stiffness (Elosegui-Artola et al. 2014). As these receptors are upregulated in cutaneous wound healing, it is interesting to speculate whether they also play a role in mechano-sensing within normal and chronic wounds.
One study specifically examining collective migration in human keratinocytes found that keratinocytes generate particularly high levels of intercellular tension compared to other epithelia, and that this tension maintains the integrity of the epithelial sheet when migrating over sparse ECM substrates (Vedula et al. 2014). The authors propose that epithelial bridging may aid re-epithelialization in a wound environment with limited or variable ECM adhesion. This phenomenon may also facilitate wound closure in the absence of specific integrins, and potentially explain why so few knockout models display a wound-healing phenotype. While it is clear that the physical and mechanical environment plays an important role in keratinocyte migration, more research is needed to understand the precise mechanisms involved and the impact on overall wound repair. Key areas for future investigation include defining the roles of specific integrin receptors, cytoskeletal components, and the downstream targets of mechanotransduction, as well as detailed analysis of the mechanical environment within the wound.
Conclusions
Integrin receptors in the epidermis of the skin perform complex functions required for tissue integrity, homeostasis, and repair. In the intact epidermis, the laminin 332 receptors provide anchorage to the basement membrane, while signaling through the β1 subunit controls stem cell proliferation and terminal differentiation. Integrin expression changes markedly during re-epithelialization, with upregulation of fibronectin and vitronectin receptors. The β1 integrin is essential for keratinocyte migration and overall wound closure; however, the significant redundancy between other receptors has made it difficult to determine their specific functions in vivo. Nevertheless, recent evidence suggests that integrin dysfunction, either through altered ECM composition or regulation of integrin expression, may contribute to impaired re-epithelialization in chronic wounds. Integrin receptors also play an important role in keratinocyte mechano-sensing, and the application of engineered model systems could provide new insights into how they mediate cell function within the dynamic wound-healing environment. Therapeutic interventions targeting integrin-mediated adhesion or downstream mechanotransduction pathways may therefore be a potential strategy for improving tissue repair in patients with chronic wounds.
References
Adair BD, Xiong J-P, Maddock C et al (2005) Three-dimensional EM structure of the ectodomain of integrin αVβ3 in a complex with fibronectin. J Cell Biol 168:1109–1118
Adams JC, Watt FM (1989) Fibronectin inhibits the terminal differentiation of human keratinocytes. Nature 340:307–309
Adams JC, Watt FM (1991) Expression of beta 1, beta 3, beta 4, and beta 5 integrins by human epidermal keratinocytes and non-differentiating keratinocytes. J Cell Biol 115:829–841
AlDahlawi S, Eslami A, Häkkinen L, Larjava HS (2006) The alphavbeta6 integrin plays a role in compromised epidermal wound healing. Wound Repair Regen 14:289–297. doi:10.1111/j.1743-6109.2006.00123.x
Ansell DM, Holden KA, Hardman MJ (2012) Animal models of wound repair: Are they cutting it? Exp Dermatol 21:581–585. doi:10.1111/j.1600-0625.2012.01540.x
Arthur WT, Petch LA, Burridge K (2000) Integrin engagement suppresses RhoA activity via a c-Src-dependent mechanism. Curr Biol 10:719–722
Bishop A (2008) Role of oxygen in wound healing. J Wound Care 17:399–402
Blanpain C, Fuchs E (2009) Epidermal homeostasis: a balancing act of stem cells in the skin. Nat Rev Mol Cell Biol 10:207–217. doi:10.1038/nrm2636
Boekhoven J, Rubert Pérez CM, Sur S et al (2013) Dynamic display of bioactivity through host-guest chemistry. Angew Chem Int Ed Engl. doi:10.1002/anie.201306278
Borradori L, Sonnenberg A (1999) Structure and function of hemidesmosomes: more than simple adhesion complexes. J Invest Dermatol 112:411–418. doi:10.1046/j.1523-1747.1999.00546.x
Brem H, Tomic-Canic M (2007) Cellular and molecular basis of wound healing in diabetes. J Clin Invest 117:1219–1222
Brizzi MF, Defilippi P, Rosso A et al (1999) Integrin-mediated adhesion of endothelial cells induces JAK2 and STAT5A activation: role in the control of c-fos gene expression. Mol Biol Cell 10:3463–3471
Brooks PC, Clark RA, Cheresh DA (1994) Requirement of vascular integrin alpha v beta 3 for angiogenesis. Science 264:569–571
Broughton G, Janis JE, Attinger CE (2006) The basic science of wound healing. Plast Reconstr Surg 117:12s–34s
Byzova TV, Goldman CK, Pampori N et al (2000) A mechanism for modulation of cellular responses to VEGF: activation of the integrins. Mol Cell 6:851–860
Calderwood DA, Campbell ID, Critchley DR (2013) Talins and kindlins: partners in integrin-mediated adhesion. Nat Rev Mol Cell Biol 14:503–517. doi:10.1038/nrm3624
Carter WG, Ryan MC, Gahr PJ (1991) Epiligrin, a new cell adhesion ligand for integrin alpha 3 beta 1 in epithelial basement membranes. Cell 65:599–610
Caskey RC, Zgheib C, Morris M et al (2014) Dysregulation of collagen production in diabetes following recurrent skin injury: contribution to the development of a chronic wound. Wound Repair Regen 22:515–520. doi:10.1111/wrr.12199
Caswell PT, Chan M, Lindsay AJ et al (2008) Rab-coupling protein coordinates recycling of alpha5beta1 integrin and EGFR1 to promote cell migration in 3D microenvironments. J Cell Biol 183:143–155
Cavani A, Zambruno G, Marconi A et al (1993) Distinctive integrin expression in the newly forming epidermis during wound healing in humans. J Invest Dermatol 101:600–604
Chen CS, Mrksich M, Huang S et al (1997) Geometric control of cell life and death. Science 276:1425–1428
Chen J, Diacovo TG, Grenache DG et al (2002) The alpha(2) integrin subunit-deficient mouse: a multifaceted phenotype including defects of branching morphogenesis and hemostasis. Am J Pathol 161:337–344
Choma DP, Pumiglia K, DiPersio CM (2004) Integrin alpha3beta1 directs the stabilization of a polarized lamellipodium in epithelial cells through activation of Rac1. J Cell Sci 117:3947–3959
Choma DP, Milano V, Pumiglia KM, DiPersio CM (2007) Integrin alpha3beta1-dependent activation of FAK/Src regulates Rac1-mediated keratinocyte polarization on laminin-5. J Invest Dermatol 127:31–40. doi:10.1038/sj.jid.5700505
Choquet D, Felsenfeld DP, Sheetz MP (1997) Extracellular matrix rigidity causes strengthening of integrin-cytoskeleton linkages. Cell 88:39–48
Chrzanowska-Wodnicka M, Burridge K (1996) Rho-stimulated contractility drives the formation of stress fibers and focal adhesions. J Cell Biol 133:1403–1415
Clark RA, Lanigan JM, DellaPelle P et al (1982) Fibronectin and fibrin provide a provisional matrix for epidermal cell migration during wound reepithelialization. J Invest Dermatol 79:264–269
Clark RA, Ashcroft GS, Spencer MJ et al (1996) Re-epithelialization of normal human excisional wounds is associated with a switch from alpha v beta 5 to alpha v beta 6 integrins. Br J Dermatol 135:46–51
Clark EA, King WG, Brugge JS et al (1998) Integrin-mediated signals regulated by members of the rho family of GTPases. J Cell Biol 142:573–586
Clark RAF, An J-Q, Greiling D et al (2003) Fibroblast migration on fibronectin requires three distinct functional domains. J Invest Dermatol 121:695–705. doi:10.1046/j.1523-1747.2003.12484.x
Connelly JT, Gautrot JE, Trappmann B et al (2010) Actin and serum response factor transduce physical cues from the microenvironment to regulate epidermal stem cell fate decisions. Nat Cell Biol 12:711–718. doi:10.1038/ncb2074
Costa P, Gautrot JE, Connelly JT (2014) Directing cell migration using micropatterned and dynamically adhesive polymer brushes. Acta Biomater. doi:10.1016/j.actbio.2014.01.029
De S, Razorenova O, McCabe NP et al (2005) VEGF-integrin interplay controls tumor growth and vascularization. Proc Natl Acad Sci U S A 102:7589–7594. doi:10.1073/pnas.0502935102
deHart GW, Healy KE, Jones JCR (2003) The role of alpha3beta1 integrin in determining the supramolecular organization of laminin-5 in the extracellular matrix of keratinocytes. Exp Cell Res 283:67–79
Desmoulière A, Chaponnier C, Gabbiani G (2005) Tissue repair, contraction, and the myofibroblast. Wound Repair Regen 13:7–12. doi:10.1111/j.1067-1927.2005.130102.x
DiPersio CM, Hodivala-Dilke KM, Jaenisch R et al (1997) alpha3beta1 Integrin is required for normal development of the epidermal basement membrane. J Cell Biol 137:729–742
DiPersio CM, Van der Neut R, Georges-Labouesse E et al (2000) alpha3beta1 and alpha6beta4 integrin receptors for laminin-5 are not essential for epidermal morphogenesis and homeostasis during skin development. J Cell Sci 113(Pt 17):3051–3062
Dowling J, Yu QC, Fuchs E (1996) Beta4 integrin is required for hemidesmosome formation, cell adhesion and cell survival. J Cell Biol 134:559–572
Edwards R, Harding KG (2004) Bacteria and wound healing. Curr Opin Infect Dis 17:91–96
Elosegui-Artola A, Bazellières E, Allen MD et al (2014) Rigidity sensing and adaptation through regulation of integrin types. Nat Mater 13:631–637. doi:10.1038/nmat3960
Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126:677–689. doi:10.1016/j.cell.2006.06.044
Evans ND, Oreffo ROC, Healy E et al (2013) Epithelial mechanobiology, skin wound healing, and the stem cell niche. J Mech Behav Biomed Mater 28:397–409. doi:10.1016/j.jmbbm.2013.04.023
Frye M, Gardner C, Li ER et al (2003) Evidence that Myc activation depletes the epidermal stem cell compartment by modulating adhesive interactions with the local microenvironment. Development 130:2793–2808
Gaggioli C, Hooper S, Hidalgo-Carcedo C et al (2007) Fibroblast-led collective invasion of carcinoma cells with differing roles for RhoGTPases in leading and following cells. Nat Cell Biol 9:1392–1400. doi:10.1038/ncb1658
Gailit J, Clark RA (1996) Studies in vitro on the role of alpha v and beta 1 integrins in the adhesion of human dermal fibroblasts to provisional matrix proteins fibronectin, vitronectin, and fibrinogen. J Invest Dermatol 106:102–108
Gailit J, Clarke C, Newman D et al (1997) Human fibroblasts bind directly to fibrinogen at RGD sites through integrin alpha(v)beta3. Exp Cell Res 232:118–126. doi:10.1006/excr.1997.3512
Gandarillas A, Watt FM (1995) Changes in expression of members of the fos and jun families and myc network during terminal differentiation of human keratinocytes. Oncogene 11:1403–1407
Gardner H, Broberg A, Pozzi A et al (1999) Absence of integrin alpha1beta1 in the mouse causes loss of feedback regulation of collagen synthesis in normal and wounded dermis. J Cell Sci 112(Pt 3):263–272
Georges-Labouesse E, Messaddeq N, Yehia G et al (1996) Absence of integrin alpha 6 leads to epidermolysis bullosa and neonatal death in mice. Nat Genet 13:370–373
Geuijen CAW, Sonnenberg A (2002) Dynamics of the alpha6beta4 integrin in keratinocytes. Mol Biol Cell 13:3845–3858. doi:10.1091/mbc.02-01-0601
Giangreco A, Goldie SJ, Failla V, et al. (2010) Human skin aging is associated with reduced expression of the stem cell markers beta1 integrin and MCSP. J Invest Dermatol 30:604–608
Gregor M, Osmanagic-Myers S, Burgstaller G et al (2014) Mechanosensing through focal adhesion-anchored intermediate filaments. FASEB J 28:715–729. doi:10.1096/fj.13-231829
Grenache DG, Zhang Z, Wells LE et al (2007) Wound healing in the alpha2beta1 integrin-deficient mouse: altered keratinocyte biology and dysregulated matrix metalloproteinase expression. J Invest Dermatol 127:455–466. doi:10.1038/sj.jid.5700611
Grinnell F, Billingham RE, Burgess L (1981) Distribution of fibronectin during wound healing in vivo. J Invest Dermatol 76:181–189
Grinnell F, Ho CH, Wysocki A (1992) Degradation of fibronectin and vitronectin in chronic wound fluid: analysis by cell blotting, immunoblotting, and cell adhesion assays. J Invest Dermatol 98:410–416
Grose R, Hutter C, Bloch W et al (2002) A crucial role of beta 1 integrins for keratinocyte migration in vitro and during cutaneous wound repair. Development 129:2303–2315
Gurtner GC, Werner S, Barrandon Y, Longaker MT (2008) Wound repair and regeneration. Nature 453:314–321. doi:10.1038/nature07039
Häkkinen L, Koivisto L, Gardner H et al (2004) Increased expression of beta6-integrin in skin leads to spontaneous development of chronic wounds. Am J Pathol 164:229–242
Hamelers IH, Olivo C, Mertens AE et al (2005) The Rac activator Tiam1 is required for (alpha)3(beta)1-mediated laminin-5 deposition, cell spreading, and cell migration. J Cell Biol 171:871–881. doi:10.1083/jcb.200509172
Harding KG, Morris HL, Patel GK (2002) Healing chronic wounds. BMJ 324:160
Has C, Spartà G, Kiritsi D et al (2012) Integrin α3 mutations with kidney, lung, and skin disease. N Engl J Med 366:1508–1514. doi:10.1056/NEJMoa1110813
Herouy Y, Mellios P, Bandemir E et al (2000) Autologous platelet-derived wound healing factor promotes angiogenesis via alphavbeta3-integrin expression in chronic wounds. Int J Mol Med 6:515–519
Herrick SE, Sloan P, McGurk M et al (1992) Sequential changes in histologic pattern and extracellular matrix deposition during the healing of chronic venous ulcers. Am J Pathol 141:1085–1095
Hertle MD, Adams JC, Watt FM (1991) Integrin expression during human epidermal development in vivo and in vitro. Development 112:193–206
Hertle MD, Kubler MD, Leigh IM, Watt FM (1992) Aberrant integrin expression during epidermal wound healing and in psoriatic epidermis. J Clin Invest 89:1892–1901. doi:10.1172/JCI115794
Huang XZ, Wu JF, Cass D et al (1996) Inactivation of the integrin beta 6 subunit gene reveals a role of epithelial integrins in regulating inflammation in the lung and skin. J Cell Biol 133:921–928
Huang X, Griffiths M, Wu J et al (2000) Normal development, wound healing, and adenovirus susceptibility in beta5-deficient mice. Mol Cell Biol 20:755–759
Humphries JD, Wang P, Streuli C et al (2007) Vinculin controls focal adhesion formation by direct interactions with talin and actin. J Cell Biol 179:1043–1057. doi:10.1083/jcb.200703036
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110:673–687
Jackson B, Peyrollier K, Pedersen E et al (2011) RhoA is dispensable for skin development, but crucial for contraction and directed migration of keratinocytes. Mol Biol Cell 22:593–605. doi:10.1091/mbc.E09-10-0859
Jones PH, Watt FM (1993) Separation of human epidermal stem cells from transit amplifying cells on the basis of differences in integrin function and expression. Cell 73:713–724
Juhasz I, Murphy GF, Yan HC et al (1993) Regulation of extracellular matrix proteins and integrin cell substratum adhesion receptors on epithelium during cutaneous human wound healing in vivo. Am J Pathol 143:1458–1469
Kim JP, Zhang K, Chen JD et al (1992) Mechanism of human keratinocyte migration on fibronectin: unique roles of RGD site and integrins. J Cell Physiol 151:443–450. doi:10.1002/jcp.1041510303
Kim JP, Zhang K, Chen JD et al (1994) Vitronectin-driven human keratinocyte locomotion is mediated by the alpha v beta 5 integrin receptor. J Biol Chem 269:26926–26932
Kiritsi D, Has C, Bruckner-Tuderman L (2013) Laminin 332 in junctional epidermolysis bullosa. Cell Adh Migr 7:135–141
Labat-Robert J, Leutenegger M, Llopis G et al (1984) Plasma and tissue fibronectin in diabetes. Clin Physiol Biochem 2:39–48
Larjava H, Salo T, Haapasalmi K et al (1993) Expression of integrins and basement membrane components by wound keratinocytes. J Clin Invest 92:1425–1435. doi:10.1172/JCI116719
Lawson C, Lim S-T, Uryu S et al (2012) FAK promotes recruitment of talin to nascent adhesions to control cell motility. J Cell Biol 196:223–232. doi:10.1083/jcb.201108078
Levental KR, Yu H, Kass L et al (2009) Matrix Crosslinking Forces Tumor Progression by Enhancing Integrin Signaling. Cell 139:891–906
Li A, Simmons PJ, Kaur P (1998) Identification and isolation of candidate human keratinocyte stem cells based on cell surface phenotype. Proc Natl Acad Sci U S A 95:3902–3907
Liu S, Leask A (2013) Integrin β1 is required for dermal homeostasis. J Invest Dermatol 133:899–906. doi:10.1038/jid.2012.438
Liu S, Xu S, Blumbach K et al (2010) Expression of integrin beta1 by fibroblasts is required for tissue repair in vivo. J Cell Sci 123:3674–3682. doi:10.1242/jcs.070672
Longmate WM, Monichan R, Chu M-L et al (2014) Reduced fibulin-2 contributes to loss of basement membrane integrity and skin blistering in mice lacking integrin α3β1 in the epidermis. J Invest Dermatol 134:1609–1617. doi:10.1038/jid.2014.10
Lopez-Rovira T, Silva-Vargas V, Watt FM (2005) Different consequences of beta1 integrin deletion in neonatal and adult mouse epidermis reveal a context-dependent role of integrins in regulating proliferation, differentiation, and intercellular communication. J Invest Dermatol 125:1215–1227
Lorenz K, Grashoff C, Torka R et al (2007) Integrin-linked kinase is required for epidermal and hair follicle morphogenesis. J Cell Biol 177:501–513. doi:10.1083/jcb.200608125
Margadant C, Raymond K, Kreft M et al (2009) Integrin alpha3beta1 inhibits directional migration and wound re-epithelialization in the skin. J Cell Sci 122:278–288. doi:10.1242/jcs.029108
Martin P (1997) Wound healing–aiming for perfect skin regeneration. Science 276:75–81
McBeath R, Pirone DM, Nelson CM et al (2004) Cell shape, cytoskeletal tension, and RhoA regulate stem cell lineage commitment. Dev Cell 6:483–495
McLean GW, Komiyama NH, Serrels B et al (2004) Specific deletion of focal adhesion kinase suppresses tumor formation and blocks malignant progression. Genes Dev 18:2998–3003. doi:10.1101/gad.316304
Mitchell K, Szekeres C, Milano V et al (2009) Alpha3beta1 integrin in epidermis promotes wound angiogenesis and keratinocyte-to-endothelial-cell crosstalk through the induction of MRP3. J Cell Sci 122:1778–1787. doi:10.1242/jcs.040956
Mitra SK, Hanson DA, Schlaepfer DD (2005) Focal adhesion kinase: in command and control of cell motility. Nat Rev Mol Cell Biol 6:56–68. doi:10.1038/nrm1549
Moll R, Franke WW, Schiller DL et al (1982) The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell 31:11–24
Nemes Z, Steinert PM (1999) Bricks and mortar of the epidermal barrier. Exp Mol Med 31:5–19. doi:10.1038/emm.1999.2
Ng MR, Besser A, Danuser G, Brugge JS (2012) Substrate stiffness regulates cadherin-dependent collective migration through myosin-II contractility. J Cell Biol 199:545–563. doi:10.1083/jcb.201207148
Nobes CD, Hall A (1995) Rho, rac, and cdc42 GTPases regulate the assembly of multimolecular focal complexes associated with actin stress fibers, lamellipodia, and filopodia. Cell 81:53–62
O’Toole EA, Marinkovich MP, Hoeffler WK et al (1997) Laminin-5 inhibits human keratinocyte migration. Exp Cell Res 233:330–339. doi:10.1006/excr.1997.3586
Osmanagic-Myers S, Gregor M, Walko G et al (2006) Plectin-controlled keratin cytoarchitecture affects MAP kinases involved in cellular stress response and migration. J Cell Biol 174:557–568. doi:10.1083/jcb.200605172
Paszek MJ, Zahir N, Johnson KR et al (2005) Tensional homeostasis and the malignant phenotype. Cancer Cell 8:241–254. doi:10.1016/j.ccr.2005.08.010
Pelham RJ, Wang Y (1997) Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc Natl Acad Sci U S A 94:13661–13665
Peltonen J, Larjava H, Jaakkola S et al (1989) Localization of integrin receptors for fibronectin, collagen, and laminin in human skin. Variable expression in basal and squamous cell carcinomas. J Clin Invest 84:1916–1923. doi:10.1172/JCI114379
Pierschbacher MD, Ruoslahti E (1984) Cell attachment activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature 309:30–33
Pulkkinen L, Rouan F, Bruckner-Tuderman L et al (1998) Novel ITGB4 Mutations in Lethal and Nonlethal Variants of Epidermolysis Bullosa with Pyloric Atresia: Missense versus Nonsense. Am J Hum Genet 63:1376–1387
Raghavan S, Desai RA, Kwon Y et al (2010) Micropatterned dynamically adhesive substrates for cell migration. Langmuir 26:17733–17738. doi:10.1021/la102955m
Ramjaun AR, Hodivala-Dilke K (2009) The role of cell adhesion pathways in angiogenesis. Int J Biochem Cell Biol 41:521–530. doi:10.1016/j.biocel.2008.05.030
Ramms L, Fabris G, Windoffer R et al (2013) Keratins as the main component for the mechanical integrity of keratinocytes. Proc Natl Acad Sci U S A 110:18513–18518. doi:10.1073/pnas.1313491110
Reffay M, Parrini MC, Cochet-Escartin O et al (2014) Interplay of RhoA and mechanical forces in collective cell migration driven by leader cells. Nat Cell Biol 16:217–223. doi:10.1038/ncb2917
Reichelt J (2007) Mechanotransduction of keratinocytes in culture and in the epidermis. Eur J Cell Biol 86:807–816. doi:10.1016/j.ejcb.2007.06.004
Reynolds LE, Conti FJ, Silva R et al (2008) alpha3beta1 integrin-controlled Smad7 regulates reepithelialization during wound healing in mice. J Clin Invest 118:965–974. doi:10.1172/JCI33538
Rice RH, Green H (1977) The cornified envelope of terminally differentiated human epidermal keratinocytes consists of cross-linked protein. Cell 11:417–422
Rice RH, Green H (1978) Relation of protein synthesis and transglutaminase activity to formation of the cross-linked envelope during terminal differentiation of the cultured human epidermal keratinocyte. J Cell Biol 76:705–711
Ridley AJ, Hall A (1992) The small GTP-binding protein rho regulates the assembly of focal adhesions and actin stress fibers in response to growth factors. Cell 70:389–399
Riveline D, Zamir E, Balaban NQ et al (2001) Focal contacts as mechanosensors: externally applied local mechanical force induces growth of focal contacts by an mDia1-dependent and ROCK-independent mechanism. J Cell Biol 153:1175–1186
Ruoslahti E, Pierschbacher MD (1986) Arg-Gly-Asp: a versatile cell recognition signal. Cell 44:517–518
Schlaepfer DD, Hunter T (1997) Focal adhesion kinase overexpression enhances ras-dependent integrin signaling to ERK2/mitogen-activated protein kinase through interactions with and activation of c-Src. J Biol Chem 272:13189–13195
Schlaepfer DD, Hanks SK, Hunter T, Van der Geer P (1994) Integrin-mediated signal transduction linked to Ras pathway by GRB2 binding to focal adhesion kinase. Nature 372:786–791
Seltmann K, Fritsch AW, Käs JA, Magin TM (2013) Keratins significantly contribute to cell stiffness and impact invasive behavior. Proc Natl Acad Sci U S A 110:18507–18512. doi:10.1073/pnas.1310493110
Sen CK, Gordillo GM, Roy S et al (2009) Human Skin Wounds: A Major and Snowballing Threat to Public Health and the Economy. Wound Repair Regen 17:763–771. doi:10.1111/j.1524-475X.2009.00543.x
Serrano I, Díez-Marqués ML, Rodríguez-Puyol M et al (2012) Integrin-linked kinase (ILK) modulates wound healing through regulation of hepatocyte growth factor (HGF). Exp Cell Res 318:2470–2481. doi:10.1016/j.yexcr.2012.08.001
Siegel DH, Ashton GH, Penagos HG et al (2003) Loss of kindlin-1, a human homolog of the Caenorhabditis elegans actin-extracellular-matrix linker protein UNC-112, causes Kindler syndrome. Am J Hum Genet 73:174–187
Singh P, Chen C, Pal-Ghosh S et al (2009) Loss of integrin alpha9beta1 results in defects in proliferation, causing poor re-epithelialization during cutaneous wound healing. J Invest Dermatol 129:217–228. doi:10.1038/jid.2008.201
Stupack DG, Cheresh DA (2004) Integrins and angiogenesis. Curr Top Dev Biol 64:207–238. doi:10.1016/S0070-2153(04)64009-9
Swift ME, Burns AL, Gray KL, DiPietro LA (2001) Age-related alterations in the inflammatory response to dermal injury. J Invest Dermatol 117:1027–1035
Tadokoro S, Shattil SJ, Eto K et al (2003) Talin Binding to Integrin ß Tails: A Final Common Step in Integrin Activation. Science 302:103–106
Takashima A, Grinnell F (1985) Fibronectin-mediated keratinocyte migration and initiation of fibronectin receptor function in vitro. J Invest Dermatol 85:304–308
Thery M, Racine V, Pepin A et al (2005) The extracellular matrix guides the orientation of the cell division axis. Nat Cell Biol 7:947–953
Theveneau E, Mayor R (2013) Collective cell migration of epithelial and mesenchymal cells. Cell Mol Life Sci. doi:10.1007/s00018-012-1251-7
Thomas GJ, Lewis MP, Whawell SA et al (2001) Expression of the alphavbeta6 integrin promotes migration and invasion in squamous carcinoma cells. J Invest Dermatol 117:67–73. doi:10.1046/j.0022-202x.2001.01379.x
Timpl R (1989) Structure and biological activity of basement membrane proteins. Eur J Biochem 180:487–502
Trappmann B, Gautrot JE, Connelly JT et al (2011) Extracellular-matrix tethering regulates stem-cell fate. Nat Mater 11:642–649. doi:10.1038/nmat3339
Tscharntke M, Pofahl R, Chrostek-Grashoff A et al (2007) Impaired epidermal wound healing in vivo upon inhibition or deletion of Rac1. J Cell Sci 120:1480–1490. doi:10.1242/jcs.03426
Tsutsumi M, Inoue K, Denda S et al (2009) Mechanical-stimulation-evoked calcium waves in proliferating and differentiated human keratinocytes. Cell Tissue Res 338:99–106. doi:10.1007/s00441-009-0848-0
Uriu K, Morelli LG, Oates AC (2014) Interplay between intercellular signaling and cell movement in development. Semin Cell Dev Biol. doi:10.1016/j.semcdb.2014.05.011
Van Dongen SFM, Maiuri P, Marie E et al (2013) Triggering cell adhesion, migration or shape change with a dynamic surface coating. Adv Mater Weinheim 25:1687–1691. doi:10.1002/adma.201204474
Vedula SRK, Hirata H, Nai MH et al (2014) Epithelial bridges maintain tissue integrity during collective cell migration. Nat Mater 13:87–96. doi:10.1038/nmat3814
Vignaud T, Galland R, Tseng Q et al (2012) Reprogramming cell shape with laser nano-patterning. J Cell Sci 125:2134–2140. doi:10.1242/jcs.104901
Watt FM (1983) Involucrin and Other Markers of Keratinocyte Terminal Differentiation. J Investig Dermatol 81:100s–103s
Watt FM (1989) Terminal differentiation of epidermal keratinocytes. Curr Opin Cell Biol 1:1107–1115
Watt FM, Green H (1982) Stratification and terminal differentiation of cultured epidermal cells. Nature 295:434–436
Watt FM, Jordan PW, O’Neill CH (1988) Cell shape controls terminal differentiation of human epidermal keratinocytes. Proc Natl Acad Sci U S A 85:5576–5580
Watt FM, Kubler MD, Hotchin NA et al (1993) Regulation of keratinocyte terminal differentiation by integrin-extracellular matrix interactions. J Cell Sci 106(Pt 1):175–182
Weis S, Lee TT, Del Campo A, García AJ (2013) Dynamic cell-adhesive microenvironments and their effect on myogenic differentiation. Acta Biomater 9:8059–8066. doi:10.1016/j.actbio.2013.06.019
White SJ, McLean WH (2005) Kindler surprise: mutations in a novel actin-associated protein cause Kindler syndrome. J Dermatol Sci 38:169–175
Wysocki AB, Grinnell F (1990) Fibronectin profiles in normal and chronic wound fluid. Lab Invest 63:825–831
Wysocki AB, Staiano-Coico L, Grinnell F (1993) Wound fluid from chronic leg ulcers contains elevated levels of metalloproteinases MMP-2 and MMP-9. J Invest Dermatol 101:64–68
Xiong J-P, Stehle T, Diefenbach B et al (2001) Crystal structure of the extracellular segment of integrin αVβ3. Science 294:339–345
Yang JT, Rayburn H, Hynes RO (1993) Embryonic mesodermal defects in alpha 5 integrin-deficient mice. Development 119:1093–1105
Yang C, Tibbitt MW, Basta L, Anseth KS (2014) Mechanical memory and dosing influence stem cell fate. Nat Mater 13:645–652. doi:10.1038/nmat3889
Zhao JH, Reiske H, Guan JL (1998) Regulation of the cell cycle by focal adhesion kinase. J Cell Biol 143:1997–2008
Zhu AJ, Haase I, Watt FM (1999) Signaling via beta1 integrins and mitogen-activated protein kinase determines human epidermal stem cell fate in vitro. Proc Natl Acad Sci U S A 96:6728–6733
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kenny, F.N., Connelly, J.T. Integrin-mediated adhesion and mechano-sensing in cutaneous wound healing. Cell Tissue Res 360, 571–582 (2015). https://doi.org/10.1007/s00441-014-2064-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-014-2064-9