Abstract
The generation of functional neuromuscular activity within the pre-natal gastrointestinal tract requires the coordinated development of enteric neurons and glial cells, concentric layers of smooth muscle and interstitial cells of Cajal (ICC). We investigated the genesis of these different cell types in human embryonic and fetal gut material ranging from weeks 4–14. Neural crest cells (NCC), labelled with antibodies against the neurotrophin receptor p75NTR, entered the foregut at week 4, and migrated rostrocaudally to reach the terminal hindgut by week 7. Initially, these cells were loosely distributed throughout the gut mesenchyme but later coalesced to form ganglia along a rostrocaudal gradient of maturation; the myenteric plexus developed primarily in the foregut, then in the midgut, and finally in the hindgut. The submucosal plexus formed approximately 2–3 weeks after the myenteric plexus, arising from cells that migrated centripetally through the circular muscle layer from the myenteric region. Smooth muscle differentiation, as evidenced by the expression of α-smooth muscle actin, followed NCC colonization of the gut within a few weeks. Gut smooth muscle also matured in a rostrocaudal direction, with a large band of α-smooth muscle actin being present in the oesophagus at week 8 and in the hindgut by week 11. Circular muscle developed prior to longitudinal muscle in the intestine and colon. ICC emerged from the developing gut mesenchyme at week 9 to surround and closely appose the myenteric ganglia by week 11. By week 14, the intestine was invested with neural cells, longitudinal, circular and muscularis mucosae muscle layers, and an ICC network, giving the fetal gut a mature appearance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The gastrointestinal tract is formed from a primitive gut tube that arises early in development and consists of the endoderm, which gives rise to the inner epithelial lining of the gut, and splanchnic mesoderm, which gives rise to the smooth muscle (Roberts 2000). During the development of the gastrointestinal tract, neurectoderm-derived neuronal precursors colonize the lengthening gut and become distributed in concentric plexus within the gut wall to form the enteric nervous system (ENS), the intrinsic innervation of the gastrointestinal tract. All of the neurons and glial cells of the ENS are derived from the neural crest. Neural crest cell (NCC) ablation studies (Yntema and Hammond 1954; Peters-van der Sanden et al. 1993; Burns et al. 2000), quail-chick interspecies grafting (Le Douarin and Teillet 1973, 1974; Burns and Le Douarin 2001) and other cell-tracing experiments (Epstein et al. 1994) have demonstrated that the rhombencephalic (vagal) neural crest, adjacent to somites 1–7, contributes the majority of ENS cells along the entire length of the gut. A contribution from the sacral neural crest to the post-umbilical gut has also been demonstrated in the chick and mouse (Le Douarin and Teillet 1973; Pomeranz and Gershon 1990; Pomeranz et al. 1991; Serbedzija et al. 1991; Burns and Le Douarin 1998), although the extent of the contribution and the phenotypes that arise from these cells have yet to be fully elucidated in mammals.
ENS formation requires the co-ordinated migration, proliferation, differentiation and survival of NCC within the developing gut. Numerous genes/signalling molecules have recently been shown to be involved in these processes; these include transcription factors (e.g. Phox2b, Sox10, Pax3, Mash1), components of the RET and ET-3/EDNRB signalling pathways, secreted proteins (Hedgehog, BMPs), neurotrophic factors (e.g. neurotrophin-3) and extracellular matrix (ECM) molecules (e.g. laminin) (Gershon 1998, 1999a, 1999b; Taraviras and Pachnis 1999; Ramalho-Santos et al. 2000; Manie et al. 2001; Chalazonitis et al. 2004). Mutations in genes encoding some of these signalling molecules have been documented in patients with Hirschsprung disease (HSCR), a congenital defect affecting the gut of 1 in 5,000 newborn infants (Wartiovaara et al. 1998; Amiel and Lyonnet 2001). In HSCR, the hindgut (usually the distal colon) is devoid of enteric neurons and glia, a condition that results in life-threatening intestinal obstruction and megacolon (Kapur 1999).
Much evidence has been accumulated suggesting that, in order to develop normally, migrating NCC interact with signalling cues that are encountered along their migration pathways (Le Douarin and Kalcheim 1999). It is therefore not surprising that interactions between migrating NCC and the local gut environment are essential for normal ENS development. For example, in the RET and ET-3/EDNRB pathways, the receptor components (RET, GFRα1; EDNRB) are present on migrating NCC (Pachnis et al. 1993; Nataf et al. 1996), whereas the ligands (glial-cell-derived neurotrophic factor, GDNF; ET-3) are expressed in the gut mesenchyme (Hellmich et al. 1996; Leibl et al. 1999). GDNF has been shown to promote the survival, proliferation and neuronal differentiation of ENS precursor cells in vitro (Heuckeroth et al. 1998; Gianino et al. 2003) and has also been demonstrated to be a chemoattractant for vagal NCC (Young et al. 2001; Natarajan et al. 2002). The role of ET-3 is less clear but it has been shown to affect the rate of colonization and possibly the number of vagal NCC that migrate along the gut (Barlow et al. 2003). ET-3 may also affect the environment through which NCC migrate, as increased expression of the ECM molecule, laminin, is evident within the gut of mice lacking ET-3 (Rothman et al. 1996). Alterations in laminin and collagen type IV (Parikh et al. 1992) and other molecules, including tenascin and fibronectin (Parikh et al. 1994), and nidogen (Parikh et al. 1995) have been documented in patients with HSCR, thus implicating ECM molecules in enteric neurogenesis. ECM molecules have various roles in development, including the provision of matrices for navigation during cell migration, and the promotion of neurite outgrowth, neuronal differentiation and cell survival, and are produced by the gut mesenchyme and subsequently by smooth muscle and basal lamina (Tamiolakis et al. 2002; Rauch and Schafer 2003). It is therefore important to correlate the development of NCC in the gastrointestinal tract with the development of the smooth muscle layers in order to provide a basis for further studies investigating the expression of ECM molecules during human gut development.
In addition to the NCC-derived neurons and mesenchymal smooth muscle, a third class of cell type has been shown to be involved in the mature neuromuscular function of the gut. These specialized network-forming cells, the interstitial cells of Cajal (ICC), have diverse morphologies (Burns et al. 1997) and a variety of functions in the different regions of the gut (Hirst and Ward 2003). These include the generation of gut pacemaker activity (the basis for the electrical slow waves that underlie the phasic contractions of gastrointestinal muscles; Ward et al. 1994) and the transmission of nerve signals to the smooth muscle (Burns et al. 1996; Ward et al. 2000). ICC are derived from the gut mesenchyme (Lecoin et al. 1996; Young et al. 1996) and require signalling through the kit tyrosine kinase receptor (Chabot et al. 1988) and its ligand, stem cell (steel) factor (SCF; Zsebo et al. 1990) for their development (Ward et al. 1994, 1995; Huizinga et al. 1995). ICC can be immunohistochemically labelled by using anti-kit antibodies (Burns et al. 1997) and, although such antibodies have been used to good effect to study the development of ICC in animal models (Ward and Sanders 2001), little information is available regarding the early differentiation of these cells in the human gut. Investigations have instead focused on the role of ICC in a range of clinical contexts (Kenny et al. 1998; Hagger et al. 2000; Rolle et al. 2002; Feldstein et al. 2003; Tong et al. 2004).
Here, our aim has been to examine the spatiotemporal development of the three cell types necessary for gut neuromuscular activity. We have utilized human embryos and fetal material ranging from weeks 4 to 14 of development and show that the entire length of the gut is colonized by a rostrocaudal wave of migrating NCC at week 7. Smooth muscle development also occurs as a rostrocaudal wave of maturation, with distinct circular muscle layers appearing in the foregut at week 8 and in the hindgut by week 11. ICC begin to differentiate from the gut mesenchyme at week 9 and rapidly become oriented to surround the ENS cells of the myenteric plexus.
Materials and methods
Human embryonic and fetal material
Human material was obtained from voluntary medical or surgical terminations of pregnancy (MTOP/STOP) after parental consent and ethical approval from the local committee had been obtained. Staging of embryos was carried out according to the Carnegie system by using anatomical features and foot length as guides to age. Tissue was obtained in the UK from either the Human Developmental Biology Resource (HDBR), a resource funded jointly by the Medical Research Council (MRC) and the Wellcome Trust, or from the MRC-funded Tissue Bank.
Embryos aged between 4 weeks and 6 weeks were prepared intact, whereas in older specimens aged between 7 weeks and 14 weeks, the gastrointestinal tract was dissected free from surrounding tissue, straightened and pinned out in a Sylgard-coated dish (Dow Corning). Embryos or segments of gut were chemically fixed in 4% paraformaldehyde (PFA) for 3–4 h or overnight, depending on size. They were then rinsed repeatedly in phosphate-buffered saline (PBS; 3×5 min) and prepared for wax embedding or for cryosectioning. For wax embedding, tissues were dehydrated through an ascending series of alcohol (1×5 min each), cleared in Histoclear (2×5 min) and then left overnight in molten wax at 56°C prior to embedding. For cryosectioning, samples were left overnight in 15% sucrose solution in PBS and then transferred to a solution containing 15% sucrose, 5% gelatin in PBS at 37°C. Tissues were then placed in blocks, oriented appropriately in the cooling gelatin solution and frozen in isopentane, precooled in liquid nitrogen to −60°C.
Sectioning
Transverse sections were cut from whole embryos and dissected gut segments. Sections were obtained at a thickness of 6 μm from wax blocks and 10–15 μm from frozen blocks. All sections were placed on Superfrost Plus microscope slides (BDH Laboratories). Adjacent sections were also prepared for double immunohistochemical labelling.
Immunohistochemistry
Slides were initially treated to remove supporting media. Wax sections were placed in Histoclear (National Diagnostics, Atlanta , USA; 3×5 mins) and then rehydrated through a descending series of alcohol (1×5 min each) to PBS (Oxoid, Basingstoke, UK). Frozen sections were incubated for 30 min in PBS warmed to 37°C to remove the cryoprotectant. Primary antibodies (Table 1) were applied overnight at 4°C in a humid box. Slides were then washed extensively in PBS (3×5 mins) and treated with appropriate secondary antibodies (Table 2) for 1 h at room temperature. Following further washes in PBS (3×5 mins), antibody labelling were visualized with the fluorescent markers Alexa 488 (Molecular Probes, Oregon, USA), Cy3 (Amersham Pharmacia Biotech, Buckinghamshire, UK) or with the reaction product of diaminobenzidine (DAB; Sigma, Poole, UK), as detailed in Table 2. Negative control experiments were performed by omitting the primary antibody. Following DAB staining, sections were dehydrated through an ascending series of alcohols (1×5 min each), cleared in Histoclear (2×5 mins) and mounted in DPX (Fisher Scientific, Loughbourgh, UK). Fluorescently labeled sections were mounted in Fluoromount-G (Southern Biotech, Birmingham, USA).
Images were captured on a Zeiss Axiophot microscope equipped with a Hamamatsu C4742-95 or Leica DC-500 digital camera by using Improvision Openlab (v3.11) and Leica Firecam (v1.20) software, respectively. Figures were assembled and annotated by using Adobe Photoshop 7 software (Adobe).
Results
Rostrocaudal gut colonization by p75NTR-positive neural crest cells
At week 4 of development (the earliest stage examined in this study), neural crest cells (NCC) were observed migrating away from the neural tube along stereotypical dorsoventral pathways, on each side of the embryo, lateral to the dorsal aorta (Fig. 1a). NCC were evenly scattered within the mesenchyme of the dorsal foregut (Fig. 1b) and were also apparent within the rostral midgut, where they were randomly distributed with the gut mesenchyme (Fig. 1c). Crest cells were not observed within the caudal midgut and hindgut at this stage of development (not shown). At week 5, a similar distribution pattern of NCC was observed within the dorsal aspect of the foregut, although at this stage, crest cells had begun to coalesce and form loose chains of cells (Fig. 1d). In the pre-umbilical intestine, close to the liver, NCC were present within the gut mesenchyme (Fig. 1e) and, further along the midgut, NCC encircled the gut wall (Fig. 1f), where they grouped together to form primitive ganglia (Fig. 1e, f). At week 6, numerous p75NTR-labelled NCC were observed within the stomach (Fig. 2a). These cells were present in small groups that were distributed towards the outer aspects of the gut mesenchyme, away from the submucosal region. Nerve fibres that were p75NTR-positive and derived from the vagus nerve were mainly located outside the stomach, although occasional fibres appeared to project into the stomach wall (Fig. 2a). In the midgut, NCC were present in groups of cells that were distributed in the outer layers of the gut mesenchyme at the site of the future myenteric plexus (Fig. 2b–e). Crest cells were not observed in the mesenchymal layers underlying the gut mucosa. Oblique sections through the midgut (Fig. 2b, c) revealed that the small groups of NCC were interconnected by a fine branching network of p75NTR-positive projections. The hindgut was not colonized by NCC at this stage of development (Fig. 2f). At week 7, in the oesophagus, crest cells were located external to the circular muscle layer and were organized into distinct ganglia (Fig. 3a). Enteric ganglia were also apparent within the stomach (Fig. 3b) and were distributed in the outer muscle layers. In the midgut, NCC encircled the gut, external to the circular muscle layers, and had coalesced to form primitive ganglia (Fig. 3c–e). In the hindgut, which was colonized along its entire length at this stage of development, NCC were scattered throughout the developing gut mesenchyme; an organized pattern of cells was not apparent (Fig. 3f). At week 8, in the oesophagus, p75NTR-immunopositive ganglia were present external to the circular muscle layer (Fig. 4a). In addition, smaller groups of NCC were also observed internal to the circular muscle layer, in the region corresponding to the presumptive submucosal plexus. In the stomach, p75NTR-positive ganglia and nerve fibres were apparent within the muscle layers (Fig. 4b). In the duodenum and proximal intestine, crest cells were present in tight groups located within the outer aspects of the gut wall, in the region between the developing longitudinal and circular muscle layers, corresponding to the myenteric plexus (Fig. 4c, d). These cells had coalesced to form primitive myenteric ganglia, and NCC were not observed within the presumptive submucosal region of the midgut at this stage of development. In the distal intestine, NCC were more loosely distributed throughout the gut mesenchyme and were located mainly within the developing outer muscle layers, away from the submucosa (Fig. 4e). In the hindgut, in which distinct muscle layers were not apparent, NCC were more randomly distributed throughout the gut mesenchyme; labelled cells were not present in the regions adjacent to the gut mucosa (Fig. 4f).
Development of p75NTR-immunopositive neural crest cells (NCC). a At week 4, p75NTR-labelled cells (brown) migrated away from the neural tube (nt) and were present in streams of cells (arrows) located lateral to the dorsal aorta (da). b NCC (arrows) were scattered in the dorsal aspect of the foregut mesenchyme. c In the proximal midgut, adjacent to the liver (L), NCC (arrows) were scattered across the width of the undifferentiated mesenchyme. d At week 5, NCC were present in the dorsal foregut, where they had accumulated into small groups of cells (arrows). e In the proximal midgut (prox midgut), adjacent to the liver (L) NCC (arrows) were present throughout the majority of the mesenchyme, although the ventral aspect of the developing gut was sparsely colonized (asterisk). f In the distal midgut (dist midgut), small groups of NCC encircled the gut, with the majority of cells distributed in the dorsal gut wall (arrows). Bars 200 μm (a), 100 μm (b–f)
Development of p75NTR-immunopositive NCC (stom stomach, L liver, mg midgut, hg hindgut). a At week 6, NCC (brown) were distributed with the wall of the stomach (arrows). p75NTR-immunostaining, corresponding to the vagal nerve and its branches, was also present adjacent to the stomach (arrowheads). b–e In the midgut, NCC (arrows) were present in the outer layers of the developing gut. Groups of cells (c, arrows) were interconnected by fine immunopositive fibres (c, arrowheads). Individual cell bodies could be identified within the small cell clusters (e, arrowheads). Although the midgut contained many NCC, the hindgut was free from crest cells (f). Bars 200 μm (a,b), 100 μm (d, f, 50 μm (c, e)
Development of p75NTR-immunopositive NCC. a At week 7, p75NTR immunostaining (brown) was observed in the oesophagus (eso), in cells located external to the circular muscle layer (arrows). b In the stomach (stom), labelling was apparent in groups of cells (arrows) within the muscle layers, corresponding to primitive ganglia. c, d In the duodenum (duod) and proximal intestine (prox intst), respectively, immunostained cells (arrows) encircled the gut in a ring external to the circular muscle layers. e In the distal intestine (dist intst), p75NTR-positive cells (arrows) were distributed within the developing muscle layers. f In the colon (colon), immunopositive cells (arrows) were scattered throughout the undifferentiated gut mesenchyme. Bars 100 μm (a, c, d, f), 50 μm (b, e)
Development of p75NTR-immunopositive neural crest cells. a At week 8, in the oesophagus (eso), NCC (brown) were distributed around the periphery of the gut wall (arrows), external to the circular muscle layers. Occasional immunopositive cells were also present internal to the circular muscle (arrowheads). b In the stomach (stom), groups of immunopositive cells were located towards the outer layers of the stomach wall (arrows). c In the duodenum (duod), NCC (arrows) were located within a narrow band, corresponding to the presumptive myenteric plexus. These crest cells were less tightly packed in the proximal intestine (d, prox intst, arrows), and distal intestine (e, dist intst, arrows). f In the hindgut (dist colon), NCC were scattered across the undifferentiated mesenchyme, although the presumptive submucosal region was sparsely populated. Bars 100 μm (a, c, f), 100 μm (b), 50 μm (d, e)
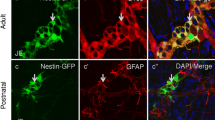
NCC were first observed in the submucosal plexus region of the oesophagus at week 8 (Fig. 4a) and in the midgut at week 11 (Fig. 5). At the latter stage of development, ganglia within the myenteric plexus of the intestine were apparent within the very outer layers of the circular muscle. Cell projections, derived from myenteric ganglia, passed through the circular muscle layer to form the primitive submucosal plexus (Fig. 5b).
Development of p75NTR-immunopositive NCC. a At week 11, in the intestine, individual NCC-containing ganglia (asterisks) were apparent within the myenteric plexus region (myp) of the small intestine. b, c Projections (arrow) from the myenteric plexus cells, traversed the circular muscle layer (cm) and interconnected with areas of immunostaining in the presumptive submucosal plexus (smp) region. Bar 50 μm
Development of gut smooth muscle layers positive for α-smooth muscle actin
At week 8 of development, a rostrocaudal gradient in the maturation of the gut smooth muscle was apparent. Anti-α-smooth muscle actin (αSMA) immunoreactivity was present in as a discrete band that encircled the oesophagus (Fig. 6a). Double-immunolabelling demonstrated p75NTR-positive ganglia external to the muscle layer, corresponding to the myenteric plexus. In the stomach, αSMA was expressed in a broad band, corresponding to the differently oriented muscle layers (Fig. 6b). In the proximal and distal intestine, αSMA immunostaining occurred as a thin band that encircled the gut and that corresponded to the circular muscle layer. This developing muscle layer was less condensed in the distal intestine (Fig. 6d) compared with the proximal intestine (Fig. 6c). Immunostaining at the level of the presumptive longitudinal muscle layer was not observed at this stage of development. In the colon, low levels of αSMA immunostaining were present within the developing gut mesenchyme and only small isolated areas of immunoreactivity were found (Fig. 6e).
Development of αSMA-immunopositive smooth muscle layers. a At week 8, the circular muscle layer (cm) in the oesophagus (eso) was well developed and a dense band of cells was strongly immunopositive for αSMA (green). p75NTR-positive cells (red) were grouped into presumptive ganglia (arrows) external to the circular muscle. b In the stomach (stom), αSMA labelling was apparent in the developing muscle layers (cm). p75NTR-labelled cells (arrows) were scattered throughout the smooth muscle. c In the proximal intestine (prox intst), the circular muscle comprized a narrow band of αSMA-stained cells (cm, arrowhead). p75NTR-positive NCC were arranged external to the circular muscle and had coalesced to form the presumptive myenteric plexus (arrows). d In the distal intestine (dist intst), the circular muscle (cm, arrowhead) was less dense than in the proximal intestine. Some p75NTR-positive cells were grouped together as primitive ganglia (arrows) but the majority of labelled cells were scattered throughout the gut mesenchyme, external to the developing circular muscle layers. e In the colon (colon), αSMA labelling was sparse and the circular muscle layer (cm) was at an early stage of development. p75NTR-positive cells (arrows) were scattered throughout the gut mesenchyme. Bars 100 μm (b–d, 50 μm (a, e)
By week 11, αSMA immunoreactivity in the intestine occurred in broad bands corresponding to the circular and longitudinal muscle layers (Fig. 7a). The presence of enteric ganglia located between the muscle layers (i.e. the presumptive myenteric plexus) was confirmed with p75NTR double-labelling. Occasional nerve fibres penetrated the circular muscle layers and projected into the submucosal region. At week 12, the longitudinal and circular muscle layers appeared to be more condensed, with intense αSMA immunostaining present in dense bands on either side of the myenteric plexus (Fig. 7b). At this stage, double-labelling with p75NTR identified discrete ganglia within the myenteric plexus. At week 14, the gut possessed a more mature phenotype. The longitudinal muscle layer was condensed and discrete, as was the circular muscle layer (Fig. 7c). Weaker αSMA immunostaining was also observed in the muscularis mucosae, adjacent to the villi of the gut epithelium. p75NTR-positive cells were apparent within the myenteric ganglia; nerve fibres were also present within the submucosal region and within the muscularis mucosae (Fig. 7c).
Development of αSMA-immunopositive smooth muscle layers. a At week 11, αSMA staining (green) was apparent in the circular (cm) and longitudinal (Lm) muscle layers, located on either side of the p75NTR-positive (red) cells (arrows) of the presumptive myenteric plexus. Occasional areas of p75NTR immunoreactivity were also apparent in the region internal to the circular muscle layer, corresponding to the presumptive submucosal plexus (double arrowheads). b At week 12, the circular (cm) and longitudinal (Lm) muscle layers were strongly immunopositive for αSMA. Between the muscle layers, p75NTR labelling was apparent in groups of cells comprising myenteric ganglia (arrows). c At week 14, αSMA labelling was intense in the circular (cm) and longitudinal (arrowhead, Lm) muscle layers but weak in the muscularis mucosae (mm), adjacent to the villi (v). The walls of blood vessels within the submucosa were also immunopositive for αSMA (asterisks). p75NTR staining was present within ganglia of the myenteric plexus (arrows) and in nerve fibres within the submucosa (double arrowheads). Bars 50 μm (a, b), 100 μm (c)
Development of kit-positive ICC within the gastrointestinal tract
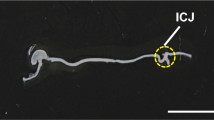
At week 9 of development, weak kit immunoreactivity was first observed within the developing muscle layer of midgut regions where the smooth muscle layers had begun to condense and differentiate, with only occasional filamentous areas of immunostaining being evident (Fig. 8a). In the hindgut at the same stage of development, immunostaining occurred across the undifferentiated mesenchyme, leaving darker unstained areas that corresponded to the regions containing neural crest-derived myenteric ganglia (Fig. 8b). By week 11, discrete kit staining was present in cells and fine projections encompassing the myenteric ganglia of the midgut (Fig. 8c). In the hindgut, where the smooth muscle was less well differentiated, kit immunoreactivity occurred across the developing muscle layer and unstained ganglia could clearly be distinguished (Fig. 8d). At week 12, when the smooth muscle was well differentiated in the midgut and hindgut, kit-positive ICC were tightly distributed around the myenteric ganglia and long thin filamentous projections interconnected the ganglia (Fig. 8e, f). By week 14, ICC were localized in tight association with the myenteric plexus cells, with discrete immunostaining being present on both aspects of the ganglia, towards the longitudinal and circular muscle layers (Fig. 8g).
Development of kit-immunopositive interstitial cells of Cajal (ICC). a At week 9, kit immunostaining (red) was present at low levels (arrows) within the developing circular muscle (cm) of the midgut. b In the hindgut, immunolabelling (arrows) was apparent within the developing muscle. Unlabelled areas, corresponding to presumptive myenteric ganglia (asterisks), were apparent. c At week 11, kit-positive ICC (arrows) were located in the midgut on either side of the presumptive myenteric ganglia (asterisks). d In the hindgut, kit staining was widespread within the developing smooth muscle layers, particularly surrounding (arrows) the presumptive myenteric ganglia (asterisks). e In the midgut at week 12, kit-positive cells (arrows) were restricted to the areas surrounding ganglia (asterisks), a pattern similar to that within the hindgut (f). g At week 14, kit-positive ICC (arrows) surrounded myenteric ganglia (asterisks) in the hindgut (cm circular muscle, Lm longitudinal muscle). Kit staining was not observed within the submucosa (sm). Bars 50 μm (a–g)
Discussion
In this study, we have analysed the spatiotemporal development of three cell types necessary for the co-ordinated neuromuscular activity of the gastrointestinal tract: (1) NCC-derived precursor cells that form the neurons and glial cells of the ENS; (2) the smooth muscle cells that form the contractile component of the gut; (3) the ICC that are involved in electrical pacemaking of the smooth muscle and in the mediation of neurotransmission between enteric nerves and gut muscle. We have utilized an antibody against the low affinity neurotrophin receptor p75NTR to label migrating NCC within the developing human gastrointestinal tract. This antibody has previously been employed extensively to label NCC in species including the amphibian Xenopus laevis (Sundqvist and Holmgren 2004), the embryonic mouse (Chalazonitis et al. 1998; Young et al. 1998a, 1999, 2003), the developing human gut (Fu et al. 2003) and other various mammals including adult human, horse, cow, sheep, pig, rabbit and rat (Esteban et al. 1998). In agreement with the recent findings of Fu et al. (2003), p75NTR-positive NCC have been found to colonize the human gut in a rostrocaudal direction from week 4 to week 7 of development, when the migration front of NCC reaches the terminal hindgut. At week 4, NCC are initially located in the dorsal aspect of the foregut and, as they migrate along the gut in the subsequent weeks, they encircle the gut and become grouped into primitive ganglia. The rostrocaudal migration of NCC along the gastrointestinal tract is similar to the pattern of colonization reported in most species to date, including fish (Shepherd et al. 2004), avians (Burns and Le Douarin 2001) and mice (Young et al. 1998a) and most recently in humans (Fu et al. 2003; Wallace and Burns 2003; Fu et al. 2004). Based on comparable labelling studies, the origin of the NCC that colonise the human gut may be attributed to the vagal neural crest. Similar findings concerning the rostrocaudal colonization of the gut by NCC have also been obtained following the investigation of RET expression in the developing human gastrointestinal tract (Attie-Bitach et al. 1998). Attie-Bitach et al. (1998) have found RET-expressing ENS precursor cells in the human foregut at 26–30 days (approximately week 4) and in the midgut and hindgut at 37–42 days (5–6 weeks), i.e. at time points similar to those described in this study.
In addition to the rostrocaudal migration of crest cells along the gut, we have also demonstrated considerable variation in crest cell distribution in different gut regions as development progresses. For example, at week 7 (Fig. 3), although NCC have formed ganglia in the oesophagus and stomach, crest cells are distributed in the outer layers of the mesenchyme of the midgut and are scattered widely throughout the mesenchyme of the colon. Therefore, the maturation of the ENS, in terms of myenteric ganglia formation, also proceed in a rostrocaudal manner, with the myenteric plexus of the oesophagus being formed first and that of the colon approximately 3 weeks later.
The observation that NCC initially colonize the outer layers of the gut mesenchyme, thus forming the myenteric plexus, is consistent with the pattern of gut colonization previously described in laboratory mammals (Kapur et al. 1992; Gershon et al. 1993; McKeown et al. 2001) and in the small intestine of the chick (Burns and Le Douarin 1998). In these animals, the submucosal plexus forms later, following the secondary centripetal migration of crest cells from the myenteric plexus. In the present study, we have observed a similar rostrocaudal gradient of maturation of the submucosal plexus, with NCC occurring in the foregut beginning at week 8 and with well-developed submucosal ganglia in the midgut at week 11, approximately 3 weeks after the myenteric plexus has formed, a finding similar to that obtained by Fu et al. (2004). Fu et al. (2004) have reported scattered single neurons and a small submucosal plexus in the foregut and midgut at week 9; this plexus increases in size by week 12. However, submucosal ganglia have not been observed in the hindgut until week 14 (Fu et al. 2004). The centripetal pattern of gut colonization reported here, and previously in mice, is apparently attributable to the secondary migration of NCC from the myenteric plexus, inwards through the circular muscle layer. Although ligands such as GDNF and ET-3 (for the RET and EDNRB cell-cell signalling pathways, respectively) have been shown to be expressed in the gut mesenchyme (Suvanto et al. 1996; Leibl et al. 1999; Natarajan et al. 2002), their patterns of expression do not appear to coincide with this spatiotemporal migration of NCC within restricted areas of the gut mesenchyme and, therefore, do not explain the specific primary formation of the myenteric plexus followed by the formation of the submucosal plexus. However, netrins and netrin receptors, such as those that are deleted in colorectal cancer (DCC), have recently been shown to be involved in guiding this secondary migration of crest cells during the formation of the submucosal plexus (Jiang et al. 2003), since DCC crest cells appear to be attracted to areas of the gut at which netrin expression is high (i.e. in the submucosa).
NCC have been found to progress along the gut in a rostrocaudal direction, whereas the hindgut remains free from NCC until the migration front of vagal crest-derived cells has colonized the entire length of the gut by week 7. Therefore, as previously reported in the mouse (Young et al. 1998a; Kapur 2000) and the chick (Burns et al. 2000), there is no evidence for an early migration of NCC into the hindgut from a source that could be attributed to the sacral neural crest (Burns and Le Douarin 1998). The extent of the contribution of sacral NCC to the hindgut in the human embryo has yet to be determined and has not been addressed in this study.
We have demonstrated a rostrocaudal gradient of smooth muscle maturation as evidenced by the appearance of αSMA immunoreactivity. A broad band of αSMA staining is present in the circular muscle layer of the oesophagus at week 8 and in the hindgut at week 11. Although other immunohistochemical studies have also reported gradients of maturation in gut smooth muscle (Fu et al. 2004), the chronological correspondence between ultrastructural and histochemical development is poorly understood, as ultrastructural investigations have not yet confirmed the existence of such gradients (Gabella 2002). For example, a detailed ultrastructural and immunohistochemical study by Ward and Torihashi (1995) of the developing canine proximal colon has demonstrated that the increase in thickness of the tunica muscularis is attributable to an increase in number and size of smooth muscle cells, which also change their desmin and vimentin immuno-profile during the fetal period. However, because only the proximal colon has been examined, a correlation between a rostrocaudal change in smooth muscle cell morphology and expression of smooth muscle markers cannot be made.
Fu et al. (2004) have recently suggested that, in the human, the longitudinal and circular muscle layers appear at the same time and differentiate in a rostrocaudal manner between weeks 7 and weeks 9. However, we have found no αSMA immunoreactivity within the presumptive longitudinal muscle layer of the intestine or colon at week 8, whereas the circular muscle layer is αSMA-positive at these stages of development (see Fig. 6). This finding suggests that, in the mid- and hindgut, the longitudinal muscle layer “matures” (i.e. expresses αSMA) after the circular muscle layer. Such delayed maturation of the longitudinal muscle layer has been reported in the gut of the chick embryo by using the smooth muscle marker, 13F4 (Burns and Le Douarin 1998).
Expression of the tyrosine kinase receptor c-kit and its ligand, SCF, are essential for ICC development (Ward et al. 1994, 1995). During the establishment of the ICC network in the avian embryo, kit receptor is expressed in individual cells located at the outer border of the circular muscle layer, whereas its ligand, SCF, is expressed within the circular muscle layer (Lecoin et al. 1996). Other authors have shown that enteric neurons also express SCF (Torihashi et al. 1996; Young et al. 1998b), thus raising the question of whether ICC are capable of developing in the absence of SCF-expressing enteric neurons, an issue of particular relevance in a clinical context such as HSCR in which the absence of enteric neurons in one region of the bowel may have implications for the development of ICC, and subsequent gut function, in adjacent regions. The study by Wu et al. (2000) has shown that kit and its ligand are present in aganglionic gut obtained from ls/ls and c-ret−/− mice and that ICC develop in NCC-free cultures of ls/ls terminal colon, thus suggesting that enteric neurons are not required for the development of ICC. Similar findings have also been reported by Lecoin et al. (1996), following the appearance of ICC in cultured aganglionic chicken gut. Since Wu et al. (2000) have demonstrated that SCF immunoreactivity is coincident in cells with neuronal or smooth muscle markers, the kit ligand therefore seems to be provided by neurons and/or by cells in a smooth muscle lineage, which we show here to form before ICC in the human gut. This idea is further supported by investigations with Gdnf−/− mice, which lack ENS cells in the majority of the gut (Ward et al. 1999). Data from these animals suggest that the presence of neurons is not required for the formation of a mature ICC network and that the circular muscle layer, which develops before the ICC, can provide sufficient SCF for the formation of functional ICC networks. However, the developmental relationship between neurons and ICC is still contentious, particularly in humans, in which conflicting findings have recently been described (Huizinga et al. 2001; Rolle et al. 2002; Newman et al. 2003).
Here, we have identified kit-positive ICC in the intestine at week 9, after the colonization of the gut by NCC and following the differentiation of the circular muscle layer. Unlike these other cells, ICC do not appear to mature in a distinct rostrocaudal wave, as kit immunoreactivity is more defined in the hindgut than in the midgut at week 9. ICC rapidly mature and, by week 11, kit immunoreactivity is restricted to cells surrounding the myenteric ganglia, in a pattern that is more organized in the midgut than in the hindgut. Similar reports of ICC surrounding myenteric ganglia have been described in the human fetal small bowel (Kenny et al. 1999; Wester et al. 1999). However, Fu et al. (2004) have identified kit-positive cells within myenteric plexus at week 12; these then move to the periphery of ganglia by week 14. These authors have subsequently identified ICC preferentially located at the periphery of ganglia at week 20 (Fu et al. 2004). We have not been able to identify kit-immunopositive cells within ganglia, although we have not performed double-labelling studies with kit and neuronal markers. However, our study suggests that ICC are located on the periphery of ganglia as early as week 9 and certainly by week 11 (see Fig. 8b, c). ICC development therefore appears to lag behind that of the ENS by at least 3 weeks and slightly behind that of smooth muscle differentiation, as evidenced by αSMA immunoreactivity. A similar developmental lag for ICC has also been reported in the mouse embryo (Wu et al. 2000), as ICC forms after the gut has been colonized by neural precursors and after the development of αSMA-immunopositive muscle.
References
Amiel J, Lyonnet S (2001) Hirschsprung disease, associated syndromes, and genetics: a review. J Med Genet 38:729–739
Attie-Bitach T, Abitbol M, Gerard M, Delezoide AL, Auge J, Pelet A, Amiel J, Pachnis V, Munnich A, Lyonnet S, Vekemans M (1998) Expression of the RET proto-oncogene in human embryos. Am J Med Genet 80:481–486
Barlow A, Graaff E de, Pachnis V (2003) Enteric nervous system progenitors are coordinately controlled by the G protein-coupled receptor EDNRB and the receptor tyrosine kinase RET. Neuron 40:905–916
Burns AJ, Le Douarin NM (1998) The sacral neural crest contributes neurons and glia to the post-umbilical gut: spatiotemporal analysis of the development of the enteric nervous system. Development 125:4335–4347
Burns AJ, Le Douarin NM (2001) Enteric nervous system development: analysis of the selective developmental potentialities of vagal and sacral neural crest cells using quail-chick chimeras. Anat Rec 262:16–28
Burns AJ, Lomax AE, Torihashi S, Sanders KM, Ward SM (1996) Interstitial cells of Cajal mediate inhibitory neurotransmission in the stomach. Proc Natl Acad Sci USA 93:12008–12013
Burns AJ, Herbert TM, Ward SM, Sanders KM (1997) Interstitial cells of Cajal in the guinea-pig gastrointestinal tract as revealed by c-kit immunohistochemistry. Cell Tissue Res 290:11–20
Burns AJ, Champeval D, Le Douarin NM (2000) Sacral neural crest cells colonise aganglionic hindgut in vivo but fail to compensate for lack of enteric ganglia. Dev Biol 219:30–43
Chabot B, Stephenson DA, Chapman VM, Besmer P, Bernstein A (1988) The proto-oncogene c-kit encoding a transmembrane tyrosine kinase receptor maps to the mouse W locus. Nature 335:88–89
Chalazonitis A, Rothman TP, Chen J, Gershon MD (1998) Age-dependent differences in the effects of GDNF and NT-3 on the development of neurons and glia from neural crest-derived precursors immunoselected from the fetal rat gut: expression of GFRalpha-1 in vitro and in vivo. Dev Biol 204:385–406
Chalazonitis A, D’Autreaux F, Guha U, Pham TD, Faure C, Chen JJ, Roman D, Kan L, Rothman TP, Kessler JA, Gershon MD (2004) Bone morphogenetic protein-2 and −4 limit the number of enteric neurons but promote development of a TrkC-expressing neurotrophin-3-dependent subset. J Neurosci 24:4266–4282
Epstein ML, Mikawa T, Brown AM, McFarlin DR (1994) Mapping the origin of the avian enteric nervous system with a retroviral marker. Dev Dyn 201:236–244
Esteban I, Levanti B, Garcia-Suarez O, Germana G, Ciriaco E, Naves FJ, Vega JA (1998) A neuronal subpopulation in the mammalian enteric nervous system expresses TrkA and TrkC neurotrophin receptor-like proteins. Anat Rec 251:360–370
Feldstein AE, Miller SM, El-Youssef M, Rodeberg D, Lindor NM, Burgart LJ, Szurszewski JH, Farrugia G (2003) Chronic intestinal pseudoobstruction associated with altered interstitial cells of cajal networks. J Pediatr Gastroenterol Nutr 36:492–497
Fu M, Chi Hang Lui V, Har Sham M, Nga Yin Cheung A, Kwong Hang Tam P (2003) HOXB5 expression is spatially and temporarily regulated in human embryonic gut during neural crest cell colonization and differentiation of enteric neuroblasts. Dev Dyn 228:1–10
Fu M, Tam PK, Sham MH, Lui VC (2004) Embryonic development of the ganglion plexuses and the concentric layer structure of human gut: a topographical study. Anat Embryol (Berl) 208:33–41
Gabella G (2002) Development of visceral smooth muscle. Results Probl Cell Differ 38:1–37
Gershon MD (1998) V. Genes, lineages, and tissue interactions in the development of the enteric nervous system. Am J Physiol 275:G869–G873
Gershon MD (1999a) Endothelin and the development of the enteric nervous system. Clin Exp Pharmacol Physiol 26:985–988
Gershon MD (1999b) Lessons from genetically engineered animal models. II. Disorders of enteric neuronal development: insights from transgenic mice. Am J Physiol 277:G262–G267
Gershon MD, Chalazonitis A, Rothman TP (1993) From neural crest to bowel: development of the enteric nervous system. J Neurobiol 24:199–214
Gianino S, Grider JR, Cresswell J, Enomoto H, Heuckeroth RO (2003) GDNF availability determines enteric neuron number by controlling precursor proliferation. Development 130:2187–2198
Hagger R, Finlayson C, Kahn F, De Oliveira R, Chimelli L, Kumar D (2000) A deficiency of interstitial cells of Cajal in Chagasic megacolon. J Auton Nerv Syst 80:108–111
Hellmich HL, Kos L, Cho ES, Mahon KA, Zimmer A (1996) Embryonic expression of glial cell-line derived neurotrophic factor (GDNF) suggests multiple developmental roles in neural differentiation and epithelial-mesenchymal interactions. Mech Dev 54:95–105
Heuckeroth RO, Lampe PA, Johnson EM, Milbrandt J (1998) Neurturin and GDNF promote proliferation and survival of enteric neuron and glial progenitors in vitro. Dev Biol 200:116–129
Hirst GD, Ward SM (2003) Interstitial cells: involvement in rhythmicity and neural control of gut smooth muscle. J Physiol (Lond) 550:337–346
Huizinga JD, Thuneberg L, Kluppel M, Malysz J, Mikkelsen HB, Bernstein A (1995) W/kit gene required for interstitial cells of Cajal and for intestinal pacemaker activity. Nature 373:347–349
Huizinga JD, Berezin I, Sircar K, Hewlett B, Donnelly G, Bercik P, Ross C, Algoufi T, Fitzgerald P, Der T, Riddell RH, Collins SM, Jacobson K (2001) Development of interstitial cells of Cajal in a full-term infant without an enteric nervous system. Gastroenterology 120:561–567
Jiang Y, Liu MT, Gershon MD (2003) Netrins and DCC in the guidance of migrating neural crest-derived cells in the developing bowel and pancreas. Dev Biol 258:364–384
Kapur RP (1999) Hirschsprung disease and other enteric dysganglionoses. Crit Rev Clin Lab Sci 36:225–273
Kapur RP (2000) Colonization of the murine hindgut by sacral crest-derived neural precursors: experimental support for an evolutionarily conserved model. Dev Biol 227:146–155
Kapur RP, Yost C, Palmiter RD (1992) A transgenic model for studying development of the enteric nervous system in normal and aganglionic mice. Development 116:167–175
Kenny SE, Connell MG, Rintala RJ, Vaillant C, Edgar DH, Lloyd DA (1998) Abnormal colonic interstitial cells of Cajal in children with anorectal malformations. J Pediatr Surg 33:130–132
Kenny SE, Connell G, Woodward MN, Lloyd DA, Gosden CM, Edgar DH, Vaillant C (1999) Ontogeny of interstitial cells of Cajal in the human intestine. J Pediatr Surg 34:1241–1247
Le Douarin NM, Kalcheim C (1999) The neural crest. Cambridge University Press, Cambridge
Le Douarin NM, Teillet MA (1973) The migration of neural crest cells to the wall of the digestive tract in avian embryo. J Embryol Exp Morphol 30:31–48
Le Douarin NM, Teillet MA (1974) Experimental analysis of the migration and differentiation of neuroblasts of the autonomic nervous system and of neurectodermal mesenchymal derivatives, using a biological cell marking technique. Dev Biol 41:162–184
Lecoin L, Gabella G, Le Douarin N (1996) Origin of the c-kit-positive interstitial cells in the avian bowel. Development 122:725–733
Leibl MA, Ota T, Woodward MN, Kenny SE, Lloyd DA, Vaillant CR, Edgar DH (1999) Expression of endothelin 3 by mesenchymal cells of embryonic mouse caecum. Gut 44:246–252
Manie S, Santoro M, Fusco A, Billaud M (2001) The RET receptor: function in development and dysfunction in congenital malformation. Trends Genet 17:580–589
McKeown SJ, Chow CW, Young HM (2001) Development of the submucous plexus in the large intestine of the mouse. Cell Tissue Res 303:301–305
Nataf V, Lecoin L, Eichmann A, Le Douarin NM (1996) Endothelin-B receptor is expressed by neural crest cells in the avian embryo. Proc Natl Acad Sci USA 93:9645–9650
Natarajan D, Marcos-Gutierrez C, Pachnis V, Graaff E de (2002) Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development 129:5151–5160
Newman CJ, Laurini RN, Lesbros Y, Reinberg O, Meyrat BJ (2003) Interstitial cells of Cajal are normally distributed in both ganglionated and aganglionic bowel in Hirschsprung’s disease. Pediatr Surg Int 19:662–668
Pachnis V, Mankoo B, Costantini F (1993) Expression of the c-ret proto-oncogene during mouse embryogenesis. Development 119:1005–1017
Parikh DH, Tam PK, Van Velzen D, Edgar D (1992) Abnormalities in the distribution of laminin and collagen type IV in Hirschsprung’s disease. Gastroenterology 102:1236–1241
Parikh DH, Tam PK, Van Velzen D, Edgar D (1994) The extracellular matrix components, tenascin and fibronectin, in Hirschsprung’s disease: an immunohistochemical study. J Pediatr Surg 29:1302–1306
Parikh DH, Leibl M, Tam PK, Edgar D (1995) Abnormal expression and distribution of nidogen in Hirschsprung’s disease. J Pediatr Surg 30:1687–1693
Peters-van der Sanden MJ, Kirby ML, Gittenberger-de Groot A, Tibboel D, Mulder MP, Meijers C (1993) Ablation of various regions within the avian vagal neural crest has differential effects on ganglion formation in the fore-, mid- and hindgut. Dev Dyn 196:183–194
Pomeranz HD, Gershon MD (1990) Colonization of the avian hindgut by cells derived from the sacral neural crest. Dev Biol 137:378–394
Pomeranz HD, Rothman TP, Gershon MD (1991) Colonization of the post-umbilical bowel by cells derived from the sacral neural crest: direct tracing of cell migration using an intercalating probe and a replication-deficient retrovirus. Development 111:647–655
Ramalho-Santos M, Melton DA, McMahon AP (2000) Hedgehog signals regulate multiple aspects of gastrointestinal development. Development 127:2763–2772
Rauch U, Schafer KH (2003) The extracellular matrix and its role in cell migration and development of the enteric nervous system. Eur J Pediatr Surg 13:158–162
Roberts DJ (2000) Molecular mechanisms of development of the gastrointestinal tract. Dev Dyn 219:109–120
Rolle U, Piotrowska AP, Nemeth L, Puri P (2002) Altered distribution of interstitial cells of Cajal in Hirschsprung disease. Arch Pathol Lab Med 126:928–933
Rothman TP, Chen J, Howard MJ, Costantini F, Schuchardt A, Pachnis V, Gershon MD (1996) Increased expression of laminin-1 and collagen (IV) subunits in the aganglionic bowel of ls/ls, but not c-ret −/− mice. Dev Biol 178:498–513
Serbedzija GN, Burgan S, Fraser SE, Bronner-Fraser M (1991) Vital dye labelling demonstrates a sacral neural crest contribution to the enteric nervous system of chick and mouse embryos. Development 111:857–866
Shepherd IT, Pietsch J, Elworthy S, Kelsh RN, Raible DW (2004) Roles for GFRalpha1 receptors in zebrafish enteric nervous system development. Development 131:241–249
Sundqvist M, Holmgren S (2004) Neurotrophin receptors and enteric neuronal development during metamorphosis in the amphibian Xenopus laevis. Cell Tissue Res 316:45–54
Suvanto P, Hiltunen JO, Arumae U, Moshnyakov M, Sariola H, Sainio K, Saarma M (1996) Localization of glial cell line-derived neurotrophic factor (GDNF) mRNA in embryonic rat by in situ hybridization. Eur J Neurosci 8:816–822
Tamiolakis D, Papadopoulos N, Hatzimichael A, Lambropoulou M, Tolparidou I, Vavetsis S, Kotini A, Anninos F, Simopoulos C (2002) A quantitative study of collagen production by human smooth muscle cells during intestinal morphogenesis. Clin Exp Obstet Gynecol 29:135–139
Taraviras S, Pachnis V (1999) Development of the mammalian enteric nervous system. Curr Opin Genet Dev 9:321–327
Tong WD, Liu BH, Zhang LY, Zhang SB, Lei Y (2004) Decreased interstitial cells of Cajal in the sigmoid colon of patients with slow transit constipation. Int J Colorectal Dis 19:467–473
Torihashi S, Yoshida H, Nishikawa S, Kunisada T, Sanders KM (1996) Enteric neurons express Steel factor-lacZ transgene in the murine gastrointestinal tract. Brain Res 738:323–328
Wallace AS, Burns AJ (2003) Spatiotemporal migration of neural crest cells within the human gastrointestinal tract. Neurogastroent Motil 15:201
Ward SM, Sanders KM (2001) Physiology and pathophysiology of the interstitial cell of Cajal: from bench to bedside. I. Functional development and plasticity of interstitial cells of Cajal networks. Am J Physiol Gastrointest Liver Physiol 281:G602–G611
Ward SM, Torihashi S (1995) Morphological changes during ontogeny of the canine proximal colon. Cell Tissue Res 282:93–108
Ward SM, Burns AJ, Torihashi S, Sanders KM (1994) Mutation of the proto-oncogene c-kit blocks development of interstitial cells and electrical rhythmicity in murine intestine. J Physiol (Lond) 480:91–97
Ward SM, Burns AJ, Torihashi S, Harney SC, Sanders KM (1995) Impaired development of interstitial cells and intestinal electrical rhythmicity in steel mutants. Am J Physiol 269:C1577–C1585
Ward SM, Ordog T, Bayguinov JR, Horowitz B, Epperson A, Shen L, Westphal H, Sanders KM (1999) Development of interstitial cells of Cajal and pacemaking in mice lacking enteric nerves. Gastroenterology 117:584–594
Ward SM, Beckett EA, Wang X, Baker F, Khoyi M, Sanders KM (2000) Interstitial cells of Cajal mediate cholinergic neurotransmission from enteric motor neurons. J Neurosci 20:1393–1403
Wartiovaara K, Salo M, Sariola H (1998) Hirschsprung’s disease genes and the development of the enteric nervous system. Ann Med 30:66–74
Wester T, Eriksson L, Olsson Y, Olsen L (1999) Interstitial cells of Cajal in the human fetal small bowel as shown by c-kit immunohistochemistry. Gut 44:65–71
Wu JJ, Rothman TP, Gershon MD (2000) Development of the interstitial cell of Cajal: origin, kit dependence and neuronal and nonneuronal sources of kit ligand. J Neurosci Res 59:384–401
Yntema CL, Hammond WS (1954) The origin of intrinsic ganglia of trunk viscera from vagal neural crest in the chick embryo. J Comp Neurol 101:515–541
Young HM, Ciampoli D, Southwell BR, Newgreen DF (1996) Origin of interstitial cells of Cajal in the mouse intestine. Dev Biol 180:97–107
Young HM, Hearn CJ, Ciampoli D, Southwell BR, Brunet JF, Newgreen DF (1998a) A single rostrocaudal colonization of the rodent intestine by enteric neuron precursors is revealed by the expression of Phox2b, Ret, and p75 and by explants grown under the kidney capsule or in organ culture. Dev Biol 202:67–84
Young HM, Torihashi S, Ciampoli D, Sanders KM (1998b) Identification of neurons that express stem cell factor in the mouse small intestine. Gastroenterology 115:898–908
Young HM, Ciampoli D, Hsuan J, Canty AJ (1999) Expression of Ret-, p75(NTR)-, Phox2a-, Phox2b-, and tyrosine hydroxylase-immunoreactivity by undifferentiated neural crest-derived cells and different classes of enteric neurons in the embryonic mouse gut. Dev Dyn 216:137–152
Young HM, Hearn CJ, Farlie PG, Canty AJ, Thomas PQ, Newgreen DF (2001) GDNF is a chemoattractant for enteric neural cells. Dev Biol 229:503–516
Young HM, Bergner AJ, Muller T (2003) Acquisition of neuronal and glial markers by neural crest-derived cells in the mouse intestine. J Comp Neurol 456:1–11
Zsebo KM, Williams DA, Geissler EN, Broudy VC, Martin FH, Atkins HL, Hsu RY, Birkett NC, Okino KH, Murdock DC, et al (1990) Stem cell factor is encoded at the Sl locus of the mouse and is the ligand for the c-kit tyrosine kinase receptor. Cell 63:213–224
Acknowledgements
We thank the joint Medical Research Council/Wellcome Trust-funded Human Developmental Biology Resource (HDBR) for provision of human embryonic and fetal material.
Author information
Authors and Affiliations
Corresponding author
Additional information
A.S.W. is funded by a PhD studentship awarded to A.J.B. by the Child Health Research Appeal Trust.
Rights and permissions
About this article
Cite this article
Wallace, A.S., Burns, A.J. Development of the enteric nervous system, smooth muscle and interstitial cells of Cajal in the human gastrointestinal tract. Cell Tissue Res 319, 367–382 (2005). https://doi.org/10.1007/s00441-004-1023-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-004-1023-2