Abstract
Diamond–Blackfan anemia (DBA) is an inherited red blood cell aplasia that usually presents during the first year of life. The main features of the disease are normochromic and macrocytic anemia, reticulocytopenia, and nearly absent erythroid progenitors in the bone marrow. The patients also present with growth retardation and craniofacial, upper limb, heart and urinary system congenital malformations in ~30–50 % of cases. The disease has been associated with point mutations and large deletions in ten ribosomal protein (RP) genes RPS19, RPS24, RPS17, RPL35A, RPL5, RPL11, RPS7, RPS10, RPS26, and RPL26 and GATA1 in about 60–65 % of patients. Here, we report a novel large deletion in RPL15, a gene not previously implicated to be causative in DBA. Like RPL26, RPL15 presents the distinctive feature of being required both for 60S subunit formation and for efficient cleavage of the internal transcribed spacer 1. In addition, we detected five deletions in RP genes in which mutations have been previously shown to cause DBA: one each in RPS19, RPS24, and RPS26, and two in RPS17. Pre-ribosomal RNA processing was affected in cells established from the patients bearing these deletions, suggesting a possible molecular basis for their pathological effect. These data identify RPL15 as a new gene involved in DBA and further support the presence of large deletions in RP genes in DBA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diamond–Blackfan anemia (DBA) (MIM# 105650) is an inherited rare red blood cell aplasia that usually presents during the first year of life. The main features of the disease are normochromic and macrocytic anemia, reticulocytopenia, and nearly absent erythroid progenitors in the bone marrow (Vlachos et al. 2008). These patients have growth retardation and ~30–50 % have craniofacial, upper limb, heart and urinary system congenital malformations (Ball et al. 1996; Lipton et al. 2006; Willig et al. 1999). The majority of patients have an increased mean corpuscular volume (MCV), elevated erythrocyte adenosine deaminase activity (eADA), and persistence of hemoglobin F (Glader and Backer 1988; Vlachos et al. 2008; Willig et al. 1999). However, some DBA patients do not have these laboratory findings, adding to the clinical heterogeneity of the disease. Even in the same family, symptoms can vary between affected family members, despite possessing the same genetic mutation. The incidence of DBA is estimated to be 5–7 per million live births, equally distributed between genders (Ball et al. 1996; Campagnoli et al. 2004; Willig et al. 1999). Approximately 45 % of patients are familial cases, with disease inherited mostly in an autosomal-dominant pattern; the other 55 % of patients are sporadic cases (Orfali et al. 2004).
Diamond–Blackfan anemia has been associated with heterozygous mutations in ten ribosomal protein (RP) genes; six small subunit RP genes RPS7 (MIM# 612563), RPS10 (MIM# 603632), RPS17 (MIM# 180472), RPS19 (MIM# 603474), RPS24 (MIM# 602412), and RPS26 (MIM# 603701); and four large subunit RP genes RPL5 (MIM# 612561), RPL11 (MIM# 612562), RPL35A (MIM# 180468), and RPL26 (MIM# 603704) (Cmejla et al. 2007; Doherty et al. 2010; Draptchinskaia et al. 1999; Farrar et al. 2008; Gazda et al. 2006, 2008, 2012). Mutations in these genes have been reported in ~55 % of DBA patients. Mutations in DBA result in haploinsufficiency of the protein, which causes a defect in synthesis of ribosomal subunits and in pre-rRNA maturation that can be detected in patients’ RNA (Choesmel et al. 2007, 2008; Doherty et al. 2010; Farrar et al. 2008; Flygare et al. 2007; Gazda et al. 2008, 2012; Idol et al. 2007). These findings strongly suggest that DBA is a disorder of ribosome biogenesis and/or function.
In addition, we recently reported mutations in GATA1, a transcription factor required for erythroid differentiation, in three DBA patients (Sankaran et al. 2012).
It was also shown that copy number variation in RP genes may be a cause of DBA in some patients. Previous studies have reported large deletions in RPS19, RPS26, RPS17, RPL35A, RPL11, and RPL5 detected by SNP array, quantitative PCR and multiple ligation-dependent probe amplification (MLPA) (Farrar et al. 2011; Kuramitsu et al. 2012; Quarello et al. 2012). In this current study, we aimed to investigate whether deletions or duplications of RP genes and genes potentially involved in ribosomal biogenesis exist in our cohort by performing an array-comparative genomic hybridization (aCGH) analysis on these genes for copy number variation in 87 DBA probands. We found large deletions in 6 out of 87 probands in five RP genes. Interestingly, one of the deletions was found in RPL15 (MIM# 604174), a gene not previously implicated to be causative in DBA. In addition to the RPL15 deletion, we detected five deletions in RP genes in which mutations have been previously associated to cause DBA: one each in RPS19, RPS24, and RPS26, and two in RPS17.
Materials and methods
Patients
Eighty-seven unrelated DBA probands participated in this study. The diagnosis of DBA in all probands was based on normochromic, often macrocytic anemia, reticulocytopenia, a low number or lack of erythroid precursors in bone marrow, and, in some patients, congenital malformations and elevated eADA. All these samples were previously screened by Sanger sequencing and were negative for mutations in the ten RP genes known to be mutated in DBA. Informed consent was obtained from all patients and their family members participating in the study under a protocol at Boston Children’s Hospital.
Customized aCGH
Genomic DNA was isolated from blood samples using a nucleic acid isolation system QuickGene-610L (Autogen, Holliston, MA) according to the manufacturer’s instructions. For aCGH, 136,821 unique probes complementary to RP genes and 117 genes shown to be involved in human ribosomal biogenesis or homologous to yeast pre-ribosomal factors (Supplementary Tables 1 and 2) were designed using the UCSC Genome Browser (hg18) database (http://genome.ucsc.edu/). Roche Nimblegen Incorporation (Madison, WI) manufactured the aCGH chips. These aCGH chips contained 136,821 probes, whose mean was 30 bps and median was 32 bps. The tiling design enabled us to detect deletions and duplications larger than 250 bps. Genomic DNA samples from DBA probands along with gender-matched controls were independently labeled with Cy3 and Cy5 florescent dyes, respectively, using NimbleGen CGH Arrays Protocol. Labeled test and reference DNAs were co-hybridized to NimbleGen 12X136821 (12 × 136,821 features) CGH arrays using NimbleGen Hybridization System. Following hybridization, the arrays were washed, dried and scanned using Axon GenPix 4200A Scanner. Array CGH data were extracted and analyzed using NimbleScan (Roche Nimblegen) software. We filtered this data with Microsoft Excel and the UCSC Genome Browser (hg18) database using the following criteria: the copy number variant needed to have a log2 ratio above 0.5 or below −0.5, be larger than 250 bps, and contain a protein-coding exon. Copy number variants that met these criteria were visualized using SignalMap (Roche Nimblegen). Deletions and duplications that were detected with fewer than seven probes were removed from our analysis and most likely represented artifacts of the aCGH plates. Lastly, the genomic regions of the deletions and duplications that met our criteria were compared to copy number variants published on DECIPHER (http://decipher.sanger.ac.uk/) to rule out deletions and duplications that were polymorphisms.
Multiplex PCR
To confirm the presence of the deletions in the probands, multiplex PCR (mPCR) assays were designed and performed. mPCR assays and mPCR-based approaches have been previously utilized to detect exonal deletions (Beggs et al. 1990; Ceulemans et al. 2012). Primers (Supplementary Table 3) were designed with Primer3 software (http://frodo.wi.mit.edu/cgi-bin/primer3/primer3_www.cgi) to amplify the coding exons and intron/exon boundaries of RPL15, RPS19, RPS24, RPS26, and RPS17. We compared these RP gene fragments against exons 8 or 55 of FBN1 as a control reference. We reasoned that pathogenic mutations of FBN1 leading to Marfan syndrome were unlikely to be present in DBA populations, and therefore we chose FBN1 as a control gene. In total, we designed and utilized 12 different mPCR assays (Supplementary Table 4). For each assay, DNA from three controls and the proband were used. mPCR products were run on a 1.3 % agarose gel to visualize the bands and these products were also run and analyzed on the QIAxcel system (Qiagen, Valencia, CA) to quantitate the intensity of the band. The RP intensities were normalized to the FBN1 band intensity and averaged for the proband and controls. We repeated these assays three times and ran a Student’s t test to determine if the proband’s ratio was statistically significant compared to the controls. However, we did not have an available DNA sample to complete our studies for the RPS19 mPCR assays.
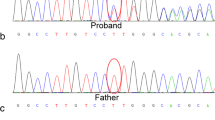
Breakpoint detection
Ultimately, to confirm the presence of the deletion in the proband, we attempted to find the exact breakpoints of these RP deletions. Using the start and end points of the deletions detected by aCGH as a guide, primers pairs were designed where the forward primer would be several hundred bases upstream of the start of the deletion and the reverse primer would be several hundred bases downstream of the end of the deletion. If a PCR product was formed from these primer pairs in only the proband and not in the control samples, it would suggest the presence of a deletion in the proband. Once a unique PCR product formed, it was treated with the reagent ExoSAP-IT (USB, Santa Clara, CA) and sequenced with an Applied Biosystems 3730 DNA Analyzer. The chromatograms were analyzed with the Sequencher 4.8 program (Gene Codes, Ann Arbor, MI).
Copy number assay
The copy number assay was carried out in duplicate using Taqman Copy Number Reference Assay RNase P (Invitrogen, Grand Island, NY) according to manufacturer protocol, using 15 ng of DNA from P5, P6, three controls, and the unaffected parents of P5. Three of the five exons of RPS17 (1, 3, and 5) were amplified. A 7300 Real Time PCR System (Applied Biosystems, Grand Island, NY) was used to perform the reaction under the following conditions: 50 °C for 2 min, 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 60 s. The sequences of the RPS17 primers used were exon 1: forward 5′-TTCGCCTGTGCTTCCTGTT-3′, reverse 5′-GGCCTCGAGCCAAAACAC-3′; exon 3: forward 5′-GGAGGAGAGAGAAAGGAGAGACAAT-3′, reverse 5′-GATTAGCCAGAAGCCCAAATATCCA-3′; and exon 5: forward 5′-TCCATTTTCTCGTTCCAGGACTTC-3′, reverse 5′-GCGTTTTGAAATTCATCCCAACTGT-3′. Data obtained using the 7300 Real Time PCR System software were then analyzed using Microsoft Excel to calculate the copy number relative to controls.
Tissue culture and knockdown of RPL15 with small interfering RNAs
HeLa cells were cultured in DMEM supplemented with 10 % fetal bovine serum and 1-mM sodium pyruvate. To knock down RPL15, 10 μl of a 100 μM siRNA solution (Eurogentec, Seraing, Belgium) was added to the cell suspension (107 cells in serum-free medium) and electro-transformation was performed with a Gene Pulser at 250 V and 950 μF in a 4-mm cuvette (Bio-Rad, Hercules, CA). Two different 21-mer siRNAs were used to knock down the expression of RPL15, siRNA rpl15-2 (5′-UGGUGUUAACCAGCUAAAGdTdT-3′) and siRNA rpl15-3 (5′- UCCAGGAGCUAUGGAGAAAdTdT-3′). Experiments on transfected cells were performed 48 h after transfection of the siRNAs. Control cells were electro-transformed with a scramble siRNA (siRNA-negative control duplex; Eurogentec). Knockdown of the RPL15 mRNA was assessed by qRT-PCR using primers 5′-ACATCCAGGAGCTATGGAGAAA-3′ and 5′-CGTAAGTTGCACCCTTAGGAAC-3′.
Analysis of pre-ribosomal RNA processing
Analysis of ribosomes on sucrose gradients and detection of pre-rRNAs by Northern blot were performed as previously described (Gazda et al. 2012; Preti et al. 2013). The probes used in the present study were 18S (5′-TTTACTTCCTCTAGATAGTCAAGTTCGACC-3′), 28S (5′-CCCGTTCCCTTGGCTGTGGTTTCGCTAGATA-3′), 5′ITS1 (5′–CCTCGCCCTCCGGGCTCCGTTAATGATC-3′), ITS1-721 (5′-GGAGCGGAGTCCGCGGTG-3′) and ITS2 (an equal amount of 5′-CTGCGAGGGAACCCCCAGCCGCGCA-3′ and 5′–GCGCGACGGCGGACGACACCGCGGCGTC-3′).
Results
Our aCGH analysis detected six deletions in RP genes in 6 out of 87 probands (Table 1). Interestingly, our analysis detected a deletion in region 23,935,136–23,937,131 of chromosome 3 in proband 1 (P1) (Fig. 1a) (all genomic coordinates are relative to hg18). This deletion contains exon 4 of RPL15. In addition to detecting the RPL15 deletion, we were able to find deletions in other probands in previously described DBA-associated RP genes, RPS19, RPS24, RPS26, and RPS17 (Cmejla et al. 2007; Doherty et al. 2010; Draptchinskaia et al. 1999; Gazda et al. 2006) (Table 1). In proband 2 (P2), we found a deletion in region 47,056,452–47,061,521 of chromosome 19. This deleted region contains exon 2 and 3 of RPS19 (Fig. 1b). In proband 3 (P3), our aCGH analysis found a deletion in region 79,463,528–79,465,261 of chromosome 10 (Fig. 1c). This deleted region corresponds to exons 1, 2, and partially 3 of RPS24. In addition, we identified a deletion in region 54,721,956–54,724,062 of chromosome 12 in proband 4 (P4) (Fig. 1d). This deleted region encompasses all four exons of RPS26. Interestingly, we found two deletions in RPS17 in our cohort: chromosome 15, 81,002,660–81,005,580 in proband 5 (P5) (Fig. 1e) and chromosome 15, 81,002,660–81,005,546 in proband 6 (P6) (Fig. 1f). These coordinates contain exons 3, 4, and 5 of RPS17.
Ribosomal protein gene deletions detected by aCGH. Visual images of entire RP genes containing a deletion detected by aCGH analysis were made using Nimblegen’s SignalMap v1.9 software. a RPL15 deletion in P1, b RPS19 deletion in P2, c RPS24 deletion in P3, d RPS26 deletion in P4, e RPS17 deletion in P5, f RPS17 deletion in P6
We validated the deletions we found by performing mPCR assays and showed that the band intensities of PCR products of deleted exons are reduced in the probands (Table 2). For P1, we assessed all four exons of RPL15 and found only the amount of PCR product of exon 4 is significantly decreased, while the ratios of the remaining exons are similar to our controls. For P3, we tested five exons of RPS24 and showed that the amount of PCR product is mildly reduced for exon 1, significantly reduced for exons 2 and 3, and not reduced for the remaining exons when compared to the controls. For P4, we examined all four exons of RPS26 and found the amounts of PCR product for all four exons to be significantly decreased. For P5 and P6, we investigated all five exons of RPS17. For P5, we detected that the amounts of PCR product for exons 1, 2, 4, and 5 were significantly reduced, while mildly reduced for exon 3 when compared to controls. For P6, we found that the band intensities of PCR products of exons 2, 3, and 5 are significantly reduced, while those of exons 1 and 4 are mildly reduced compared to controls. Subsequently, we performed mPCRs on the deleted genes on available family members of the probands to determine if their RP gene deletion was inherited from a parent or was a sporadic deletion. For P1, P2, P3, P4, and P5, all family members’ ratios appeared to be more similar to the controls than to their affected related proband (Table 3 and Supplementary Table 5). These results indicate that probands P3, P4, and P5 have de novo deletions, as their parents’ DNA analysis did not show deletions of the RPS24, RPS26 and RPS17 genes, respectively. DNA from both parents was not available for probands P1, P2 and P6.
Ultimately, to confirm the presence of the deletion in the proband, we attempted to find the exact breakpoints of these RP deletions. Using the PCR method, we were able to find the exact breakpoints of the RPL15, RPS24, and RPS26 deletion (Table 4). For P1, the RPL15 deletion was 2,393 bps in size and encompassed the region 23,935,161–23,937,553 on chromosome 3. For P3, the RPS24 deletion was 5,134 bps in size and spanned the region 79,460,166–79,465,299 on chromosome 10. For P4, the RPS26 deletion was 20,456 bps in size and located in region 54,711,095–54,731,551 on chromosome 12. Interestingly, by finding the exact breakpoints, we showed that all three deletions were larger than those found by aCGH. The RPL15 deletion was larger by 397 bps, RPS24 by 3,401 bps, and RPS26 by 18,349 bps (Tables 1, 4).
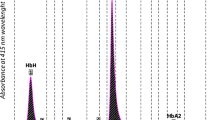
Since mPCR of all five exons of RPS17 in probands P5 and P6 showed reduction compared to control samples (by aCGH only exons 3, 4, and 5 were deleted), and because there are four functional copies of RPS17, we performed a copy number assay on exons 1, 3, and 5 of this gene on DNA samples from P5, P6, three control samples and the unaffected parents of P5. The copy number assay revealed a 50 % reduction of RPS17 DNA in both probands compared to control samples and samples from the parents of P5 (Fig. 2). These results indicate the deletion of two out of four copies of RPS17 in both probands, P5 and P6.
RPS17 copy number measured by copy number assay. Copy number at exons 1, 3, and 5 of RPS17 was measured after normalization to RNase P in three control individuals, parents of P5, and in both DBA probands P5 and P6. Probands P5 and P6 showed ~50 % reduced copy number at exons 1, 3, and 5 of RPS17 as compared to three control individuals and unaffected parents of P5
Interestingly, the proband P1 (RPL15 deletion) was diagnosed with anemia at birth, responded to corticosteroid treatment and for the last 6 years has been in remission. She had a ventricular septal defect and triphalangeal thumbs. The proband P5 (RPS17 deletion) required red blood cell transfusions 2–3 times a year between age 6 weeks and 6 years, then entered remission. This proband was also diagnosed with developmental delay. Other probands were either steroid-dependent [P2 (RPS19 deletion) and P3 (RPS24 deletion)] or transfusion-dependent [P4 (RPS26 deletion) and P6 (RPS17 deletion)]. Proband P2 has a webbed neck.
The pathogenic effect of mutations in RP genes has been associated with defects in pre-ribosomal RNA processing (Choesmel et al. 2007, 2008; Doherty et al. 2010; Farrar et al. 2008; Flygare et al. 2007; Gazda et al. 2012; Idol et al. 2007). Hence, we have previously shown that loss of function of RPS17, RPS19, RPS24, or RPS26 affects maturation of the 18S rRNA (Choesmel et al. 2007, 2008; Doherty et al. 2010; Gregory et al. 2007; O’Donohue et al. 2010). These four proteins are essential for the formation of the small ribosomal subunit. Likewise, all RPs linked to DBA so far are strictly required for synthesis of one subunit or the other. To assess whether this was also true for RPL15, we knocked down RPL15 in HeLa cells and fractionated the cytoplasmic ribosomes on a sucrose gradient. In parallel, we analyzed the pre-rRNAs by Northern blot. RPL15knockdown induced a drop in free 60S subunits and appearance of half-mers in the polysome profile, a phenotype characteristic of defective 60S subunit production (Fig. 3b). This loss of 60S subunits was associated with decreased levels of 32S and 12S pre-rRNAs, the precursors to the 5.8S and 28S rRNAs (Fig. 3c, central panel). In addition, we observed accumulation of the 41S, 30S and 18S-E pre-rRNAs relative to the 21S pre-rRNA, suggesting a defect in internal transcribed spacer 1 (ITS1) cleavage at site 2 (Fig. 3c, left panel). Moreover, two species migrating above the 30S and the 32S pre-rRNA were detected with probes ITS1-721 and ITS2 (Fig. 3c, middle and right panel). We previously observed these precursors upon depletion of RPL26, whose mutation was recently detected in a DBA patient (Gazda et al. 2012), and identified them as the 36S and 36S-C pre-rRNAs (Fig. 3a), the latter being an exonucleolytic processing product of the former (Preti et al. 2013).
Analysis of pre-rRNA processing in cells derived from DBA patients. a Schematic representation of the human pre-rRNA primary transcript and its maturation intermediates. The endonucleolytic cleavage sites are indicated by arrowheads. The colored bars show the positions of the probes used in this work. The main precursors detected in the rest of the figure are schematized. b Polysome analysis on sucrose gradient shows decreased levels of free 60S subunits upon knockdown of RPL15, induced here with two different siRNAs. Half-mers are concomitantly detected in the polysomes (arrows), consistent with a defect in 60S subunit synthesis. Reduction of the RPL15 mRNA level was more efficient with the with the rpl15-2 siRNA (13 % of the level observed with the scramble siRNA) than with the rpl15-3 siRNA (40 %), as assessed by qRT-PCR, c Northern blot analysis of pre-rRNA processing in RPL15-depleted cells with the 5′ITS1, ITS2 and ITS1-721 probes. The ITS2 and ITS1-721 probes reveal the accumulation of 36S and 36S-C pre-rRNAs. The mature 18S and 28S rRNAs were detected with specific probes. d Pre-rRNA processing in LCL cells established from DBA patients was analyzed with the same probes as in c. A faint band corresponding to the 36S-C pre-rRNA is detected with the ITS1-721 probe in the RPL15 +/mut cells (P1), while 36S pre-rRNA is detected in the RPS17 +/mut sample (P5) (arrowheads). This is best seen on the intensity profiles of the upper part of the lanes shown on the left panel. The experiment was reproduced twice with similar results. e The Northern blot signals with the 5′ITS1 and ITS2 probes were measured by phosphorimaging, quantified using MultiGauge software and normalized to the 18S rRNA. For each species, the value of the mean of the two control samples was arbitrarily set to 1
We next analyzed RNA from lymphoblastoid cell lines (LCL) established from the DBA patients harboring the large deletions mentioned above. RNA from the patient with the RPL15 deletion (P1) showed a pre-rRNA pattern close to control cells, including for the 32S and 12S precursors (Fig. 3d, e). The 41S and the 21S pre-rRNAs were slightly more abundant, suggesting a delay in ITS1 cleavage at site 2, while more 18S-E pre-rRNA was detected, a pattern consistent with RPL15 knockdown in HeLa cells. But most interestingly, we observed the weak but reproducible presence of a band migrating at the same position as the 36S-C precursors, as shown on the profile of the pattern observed with the ITS1-721 probe (Fig. 3d, right). These data strongly suggest that RPL15 depletion affects pre-rRNA processing in the patient cells. RNA from the patients mutated in RPS17 (P5) and RPS26 (P4) showed higher levels of 21S and 18S-E pre-rRNA, which matches the pattern observed upon knockdown of these proteins (Fig. 3d, e). In contrast, the deletion in RPS24 resulted in higher levels of 30S pre-rRNA (Fig. 3d, e), as expected for i-RPSs (Choesmel et al. 2008; O’Donohue et al. 2010). Therefore, these results support a direct impact of the four deletions on pre-rRNA processing and provide a molecular basis for their pathological effect.
Discussion
We found six deletions of RP genes in six probands from our aCGH analysis of RP genes in our cohort of 87 DBA patients. In contrast, we did not find any copy number variations in the 117 genes related to ribosomal biogenesis that we screened. In total, 7 % of our cohort of 87 probands without known RP point mutations contained RP deletions in RPL15, RPS19, RPS24, RPS26, and RPS17. Since ~50 % of DBA probands have point mutations in RP genes, large deletions in our cohort are present in ~3.5 % of all DBA patients. This percentage is lower than previously published reports (Farrar et al. 2011; Kuramitsu et al. 2012; Quarello et al. 2012). Strikingly, we found a deletion in the RPL15 gene for the first time in a DBA patient. The RPL15 gene is 3,694 bps long and located on chromosome 3. RPL15 is known to have many alternatively spliced transcripts, but the gene typically consists of four exons varying in size. The largest of these alternative transcripts is 2,600 bps long and encodes a 204-amino-acid-long RPL15 protein, a component of the large ribosomal subunit. Usually, the start codon is in exon 2, and the stop codon is in exon 4. The RPL15 deletion we detected includes intron 3 and exon 4. As a result, any transcript of this RPL15 variant, despite how it is alternatively spliced, would not have a stop codon. In addition, the largest alternatively spliced RPL15 transcript’s exon 4 is 1,600 bps long and encodes 102 amino acids of the RPL15 protein. Without exon 4, the RPL15 transcript is significantly smaller than the wild type RPL15 transcript; therefore, this RPL15 transcript is most likely prematurely degraded and the RPL15 deletion is DBA causal in P1.
Depletion of RPL15 affects pre-rRNA processing in a fashion similar to knockdown of RPL26: both proteins are required early in the 60S subunit synthesis pathway, and both are necessary for efficient cleavage of the ITS1 at site 2. Accumulation of the 36S and 36S-C precursors has only been reported for a small subset of proteins so far, which suggests that the two proteins are functionally related. They are both located at close positions in the 60S subunit where they make contact with both the 28S and the 5.8S rRNAs (Supplementary Fig. 1). They are likely to associate with large 90S pre-ribosomal particles before cleavage of the ITS1. Interestingly, ITS1 processing is affected in most DBA patients bearing a mutation in a RP gene, since it also involves RPS19, RPS26, RPS10 and RPS17. It is therefore tempting to speculate that a pathological mechanism is linked to this pre-rRNA maturation step in DBA, the mechanism of which remains to be defined.
The other deletions we detected occur in genes previously associated with DBA: RPS19, RPS24, RPS26, and RPS17. However, previous studies have found deletions in all of these RP genes except for RPS24 (Farrar et al. 2011; Kuramitsu et al. 2012; Quarello et al. 2012). Here, we show large-scale deletions can also occur in RPS24. Interestingly, we detected two large-scale deletions in RPS17. Previous studies have also found large deletions in RPS17 in 10 patients out of 150 studied without RP gene point mutations (7 %) (Farrar et al. 2011; Kuramitsu et al. 2012; Quarello et al. 2012). However, there have only been three point mutations described in RPS17 (Cmejla et al. 2007; Gazda et al. 2008; Song et al. 2010). Large-scale deletions occur often on chromosome 15, where two copies of the RPS17 gene are situated.
Our data reinforces the presence of large-scale RP deletions in DBA patients. However, about 35–40 % of DBA patients are still negative for RP mutations, both on the nucleotide and copy number level. We believe there are still genes yet to be discovered that are mutated in DBA patients. Recently, we identified GATA1 mutations in two DBA families (Sankaran et al. 2012). GATA1 is an important transcription factor required for erythroid differentiation. Hence, other genes, such as those encoding transcription factors needed for erythroid differentiation, may be mutated in DBA patients and could elucidate the disease mechanisms behind DBA.
Our current study found six deletions in six DBA probands. This study further supports the need to screen copy number variation in RP genes in DBA patients who are negative for RP gene point mutations. Although many of the RP deletions found before this study have been in DBA-associated RP genes, we believe other RP genes may be deleted in DBA patients as seen by our detection of the RPL15 deletion. Because of this finding, we propose a total examination of all 80 RP genes for copy number changes in DBA patients.
References
Ball SE, McGuckin CP, Jenkins G, Gordon-Smith EC (1996) Diamond–Blackfan anaemia in the UK: analysis of 80 cases from a 20-year birth cohort. Br J Haematol 94:645–653
Beggs AH, Koenig M, Boyce FM, Kunkel LM (1990) Detection of 98% of DMD/BMD gene deletions by polymerase chain reaction. Hum Genet 86:45–48
Campagnoli MF, Garelli E, Quarello P, Carando A, Sv SV, Nobili B, Dl DL, Pecile V, Zecca M, Dufour C, Ramenghi U, Dianzan I (2004) Molecular basis of Diamond–Blackfan anemia: new findings from the Italian registry and a review of the literature. Haematologica 89:480–489
Ceulemans S, van der Ven K, Del-Favero J (2012) Targeted screening and validation of copy number variations. Methods Mol Biol 838:311–328
Choesmel V, Bacqueville D, Rouquette J, Noaillac-Depeyre J, Fribourg S, Cretien A, Leblanc T, Tchernia G, Da Costa L, Gleizes PE (2007) Impaired ribosome biogenesis in Diamond–Blackfan anemia. Blood 109:1275–1283
Choesmel V, Fribourg S, Aguissa-Toure AH, Pinaud N, Legrand P, Gazda HT, Gleizes PE (2008) Mutation of ribosomal protein RPS24 in Diamond–Blackfan anemia results in a ribosome biogenesis disorder. Hum Mol Genet 17:1253–1263
Cmejla R, Cmejlova J, Handrkova H, Petrak J, Pospisilova D (2007) Ribosomal protein S17 gene (RPS17) is mutated in Diamond–Blackfan anemia. Hum Mutat 28:1178–1182
Doherty L, Sheen MR, Vlachos A, Choesmel V, O’Donohue MF, Clinton C, Schneider HE, Sieff CA, Newburger PE, Ball SE, Niewiadomska E, Matysiak M, Glader B, Arceci RJ, Farrar JE, Atsidaftos E, Lipton JM, Gleizes PE, Gazda HT (2010) Ribosomal protein genes RPS10 and RPS26 are commonly mutated in Diamond–Blackfan anemia. Am J Hum Genet 86:222–228
Draptchinskaia N, Gustavsson P, Andersson B, Pettersson M, Willig TN, Dianzani I, Ball S, Tchernia G, Klar J, Matsson H, Tentler D, Mohandas N, Carlsson B, Dahl N (1999) The gene encoding ribosomal protein S19 is mutated in Diamond–Blackfan anaemia. Nat Genet 21:169–175
Farrar JE, Nater M, Caywood E, McDevitt MA, Kowalski J, Takemoto CM, Talbot CC Jr, Meltzer P, Esposito D, Beggs AH, Schneider HE, Grabowska A, Ball SE, Niewiadomska E, Sieff CA, Vlachos A, Atsidaftos E, Ellis SR, Lipton JM, Gazda HT, Arceci RJ (2008) Abnormalities of the large ribosomal subunit protein, Rpl35a, in Diamond–Blackfan anemia. Blood 112:1582–1592
Farrar JE, Vlachos A, Atsidaftos E, Carlson-Donohoe H, Markello TC, Arceci RJ, Ellis SR, Lipton JM, Bodine DM (2011) Ribosomal protein gene deletions in Diamond–Blackfan anemia. Blood 118:6943–6951
Flygare J, Aspesi A, Bailey JC, Miyake K, Caffrey JM, Karlsson S, Ellis SR (2007) Human RPS19, the gene mutated in Diamond–Blackfan anemia, encodes a ribosomal protein required for the maturation of 40S ribosomal subunits. Blood 109:980–986
Gazda HT, Grabowska A, Merida-Long LB, Latawiec E, Schneider HE, Lipton JM, Vlachos A, Atsidaftos E, Ball SE, Orfali KA, Niewiadomska E, Da Costa L, Tchernia G, Niemeyer C, Meerpohl JJ, Stahl J, Schratt G, Glader B, Backer K, Wong C, Nathan DG, Beggs AH, Sieff CA (2006) Ribosomal protein S24 gene is mutated in Diamond–Blackfan anemia. Am J Hum Genet 79:1110–1118
Gazda HT, Sheen MR, Vlachos A, Choesmel V, O’Donohue MF, Schneider H, Darras N, Hasman C, Sieff CA, Newburger PE, Ball SE, Niewiadomska E, Matysiak M, Zaucha JM, Glader B, Niemeyer C, Meerpohl JJ, Atsidaftos E, Lipton JM, Gleizes PE, Beggs AH (2008) Ribosomal protein L5 and L11 mutations are associated with cleft palate and abnormal thumbs in Diamond–Blackfan anemia patients. Am J Hum Genet 83:769–780
Gazda HT, Preti M, Sheen MR, O’Donohue MF, Vlachos A, Davies SM, Kattamis A, Doherty L, Landowski M, Buros C, Ghazvinian R, Sieff CA, Newburger PE, Niewiadomska E, Matysiak M, Glader B, Atsidaftos E, Lipton JM, Gleizes PE, Beggs AH (2012) Frameshift mutation in p53 regulator RPL26 is associated with multiple physical abnormalities and a specific pre-ribosomal RNA processing defect in Diamond–Blackfan anemia. Hum Mutat 33:1037–1044
Glader BE, Backer K (1988) Elevated red cell adenosine deaminase activity: a marker of disordered erythropoiesis in Diamond–Blackfan anaemia and other haematologic diseases. Br J Haematol 68:165–168
Gregory LA, Aguissa-Toure AH, Pinaud N, Legrand P, Gleizes PE, Fribourg S (2007) Molecular basis of Diamond–Blackfan anemia: structure and function analysis of RPS19. Nucleic Acids Res 35:5913–5921
Idol RA, Robledo S, Du HY, Crimmins DL, Wilson DB, Ladenson JH, Bessler M, Mason PJ (2007) Cells depleted for RPS19, a protein associated with Diamond Blackfan anemia, show defects in 18S ribosomal RNA synthesis and small ribosomal subunit production. Blood Cells Mol Dis 39:35–43
Kuramitsu M, Sato-Otsubo A, Morio T, Takagi M, Toki T, Terui K, Wang R, Kanno H, Ohga S, Ohara A, Kojima S, Kitoh T, Goi K, Kudo K, Matsubayashi T, Mizue N, Ozeki M, Masumi A, Momose H, Takizawa K, Mizukami T, Yamaguchi K, Ogawa S, Ito E, Hamaguchi I (2012) Extensive gene deletions in Japanese patients with Diamond–Blackfan anemia. Blood 119:2376–2384
Lipton JM, Atsidaftos E, Zyskind I, Vlachos A (2006) Improving clinical care and elucidating the pathophysiology of Diamond Blackfan anemia: an update from the Diamond Blackfan anemia registry. Pediatr Blood Cancer 46:558–564
O’Donohue MF, Choesmel V, Faubladier M, Fichant G, Gleizes PE (2010) Functional dichotomy of ribosomal proteins during the synthesis of mammalian 40S ribosomal subunits. J Cell Biol 190:853–866
Orfali KA, Ohene-Abuakwa Y, Ball SE (2004) Diamond Blackfan anaemia in the UK: clinical and genetic heterogeneity. Br J Haematol 125:243–252
Preti M, O’Donohue MF, Montel-Lehry N, Bortolin-Cavaille ML, Choesmel V, Gleizes PE (2013) Gradual processing of the ITS1 from the nucleolus to the cytoplasm during synthesis of the human 18S rRNA. Nucleic Acids Res 41:4709–4723
Quarello P, Garelli E, Brusco A, Carando A, Mancini C, Pappi P, Vinti L, Svahn J, Dianzani I, Ramenghi U (2012) High frequency of ribosomal protein gene deletions in Italian Diamond Blackfan anemia patients detected by multiplex ligation-dependent probe amplification (MLPA) assay. Haematologica 97:1813–1817
Sankaran VG, Ghazvinian R, Do R, Thiru P, Vergilio JA, Beggs AH, Sieff CA, Orkin SH, Nathan DG, Lander ES, Gazda HT (2012) Exome sequencing identifies GATA1 mutations resulting in Diamond–Blackfan anemia. J Clin Invest 122:2439–2443
Song MJ, Yoo EH, Lee KO, Kim GN, Kim HJ, Kim SY, Kim SH (2010) A novel initiation codon mutation in the ribosomal protein S17 gene (RPS17) in a patient with Diamond–Blackfan anemia. Pediatr Blood Cancer 54:629–631
Vlachos A, Ball S, Dahl N, Alter BP, Sheth S, Ramenghi U, Meerpohl J, Karlsson S, Liu JM, Leblanc T, Paley C, Kang EM, Leder EJ, Atsidaftos E, Shimamura A, Bessler M, Glader B, Lipton JM (2008) Diagnosing and treating Diamond Blackfan anaemia: results of an international clinical consensus conference. Br J Haematol 142:859–876
Willig TN, Niemeyer CM, Leblanc T, Tiemann C, Robert A, Budde J, Lambiliotte A, Kohne E, Souillet G, Eber S, Stephan JL, Girot R, Bordigoni P, Cornu G, Blanche S, Guillard JM, Mohandas N, Tchernia G (1999) Identification of new prognosis factors from the clinical and epidemiologic analysis of a registry of 229 Diamond–Blackfan anemia patients. DBA group of Societe d’Hematologie et d’Immunologie Pediatrique (SHIP), Gesellshaft fur Padiatrische Onkologie und Hamatologie (GPOH), and the European Society for Pediatric Hematology and Immunology (ESPHI). Pediatr Res 46:553–561
Acknowledgments
We wish to thank the patients and their families for participating in the study. This work was supported by the following Grants: NIH Grants R01 HL107558 and K02 HL111156, a Grant from the DBA Foundation (to H.T.G.), and a Grant from the Agence Nationale de la Recherche (RIBOCRASH) (to P.E.G.).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Landowski, M., O’Donohue, MF., Buros, C. et al. Novel deletion of RPL15 identified by array-comparative genomic hybridization in Diamond–Blackfan anemia. Hum Genet 132, 1265–1274 (2013). https://doi.org/10.1007/s00439-013-1326-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-013-1326-z