Abstract
Studies suggest that a functional polymorphism of the brain-derived neurotrophic factor gene (BDNF Val66Met) may mediate hippocampal-dependent cognitive functions. A few studies have reported its role in cognitive deficits in schizophrenia including its association with peripheral BDNF levels as a mediator of these cognitive deficits. We assessed 657 schizophrenic inpatients and 445 healthy controls on the repeatable battery for the assessment of neuropsychological status (RBANS), the presence of the BDNF Val66Met polymorphism and serum BDNF levels. We assessed patient psychopathology using the Positive and Negative Syndrome Scale. We showed that visuospatial/constructional abilities significantly differed by genotype but not genotype × diagnosis, and the Val allele was associated with better visuospatial/constructional performance in both schizophrenic patients and healthy controls. Attention performance showed a significant genotype by diagnosis effect. Met allele-associated attention impairment was specific to schizophrenic patients and not shown in healthy controls. In the patient group, partial correlation analysis showed a significant positive correlation between serum BDNF and the RBANS total score. Furthermore, the RBANS total score showed a statistically significant BDNF level × genotype interaction. We demonstrated an association between the BDNF Met variant and poor visuospatial/constructional performance. Furthermore, the BDNF Met variant may be specific to attentional decrements in schizophrenic patients. The association between decreased BDNF serum levels and cognitive impairment in schizophrenia is dependent on the BDNF Val66Met polymorphism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive deficits in learning, memory, attention, executive functioning, spatial working memory and cognitive processing speed are core features of schizophrenia (Sharma and Antonova 2003; Kraus and Keefe 2007). These deficits occur prior to the onset of other symptoms of schizophrenia (Lieberman et al. 2001; Dickerson et al. 2004), and generally persist during the course of the illness (Hughes et al. 2003). Indeed, cognitive impairment associated with schizophrenia is a major obstacle to rehabilitation with its severity being a predictor of poor clinical outcome (Kaneda et al. 2009; Granholm et al. 2008; Harvey et al. 2003; Harvey 2009). Although studies have defined cognitive constructs that are impaired in this disease, the pathophysiological mechanisms underlying these cognitive deficits are less clear.
BDNF is a member of the neurotrophin family of growth factors. BDNF is critical in modulating memory-associated neuroplasticity through regulating cell survival, proliferation and synaptic growth in the developing central nervous system (Poo 2001; Egan et al. 2003). More specifically, BDNF appears to play an important role in both early long-term potentiation (LTP) and late phase LTP in hippocampal neurons (Lu and Gottschalk 2000), a cellular model of learning and memory (Poo 2001). Inhibition of BDNF signaling by gene knockout or antisense RNA impairs spatial learning and memory (Guzowski et al. 2000). Also, BDNF has been prominently implicated in survival and function of midbrain dopamine neurons related to cognitive function (Altar et al. 1997). Thus, preclinical evidence suggests that BDNF activity or levels may contribute to alterations in hippocampal function and hippocampal-dependent learning and memory (Hariri et al. 2003). Indeed, previous studies indicate that a SNP (rs6265) producing a valine (Val)-to-methionine (Met) substitution in the proBDNF protein at codon 66 (Val66Met) is related to hippocampal-mediated memory performance in humans (Egan et al. 2003; Hariri et al. 2003). Consistent with this, both normal controls and schizophrenic patients with Met alleles have significant deficiencies in episodic memory (Egan et al. 2003; Hariri et al. 2003; Dempster et al. 2005). Moreover, imaging studies show that individuals with this allele exhibit abnormal hippocampal activation and reduced brain volume in regions associated with memory and attention (Szeszko et al. 2005; Bueller et al. 2006). Taken together, these findings support a role for the BDNF Val66Met polymorphism in normal hippocampal-dependent memory function in healthy controls as well as in individuals with schizophrenia.
Recent studies indicate that circulating BDNF may be a biomarker of general cognitive function in healthy adults (Yu et al. 2008). The finding that serum BDNF levels are significantly decreased in individuals with diseases associated with progressive cognitive decline, such as mild cognitive impairment (Yu et al. 2008), Alzheimer disease (Gunstad et al. 2008) and Huntington’s disease (Ciammola et al. 2007), also supports this conclusion. In fact, higher BDNF levels are associated with better neuropsychological test performance in individuals with these diseases (Yu et al. 2008). More recent studies also support the notion that circulating BDNF is a biomarker of memory and general cognitive function in healthy adults (Komulainen et al. 2008). However, none have examined this association in patients with schizophrenia. Therefore, the present study was designed to determine the interrelationships of BDNF serum levels with cognitive function and BDNF genotype in schizophrenia and healthy controls. The primary aims of this study were: (1) to examine the relationship between serum BDNF levels and cognitive function in schizophrenia and healthy controls; (2) to determine whether the Val66Met polymorphism influences cognitive function in these groups; (3) to examine whether the relationship between serum BDNF levels and/or cognitive function is dependent on the BDNF Val66Met polymorphism.
Materials and methods
Subjects
Six hundred and fifty-seven inpatients were recruited from Beijing Hui-Long-Guan Psychiatric hospital and HeBei Province Veterans Psychiatric Hospital in BaoDing city, 50 miles from Beijing. All patients met the DSM-IV diagnosis of schizophrenia, which was confirmed by two psychiatrists based on the Structured Clinical Interview for DSM-IV (SCID). Their clinical subtypes were: paranoid, 216 (32.9%); undifferentiated, 351 (53.4%); disorganized, 53 (8.1%); residual, 34 (5.2%) and others, 3 (0.4%). Patients were between 25 and 75 years old and had a mean duration of hospitalization of 9.4 ± 7.5 years. All patients had been receiving stable doses of oral antipsychotic drugs for at least 12 months.
Four hundred and forty-five control subjects (male/female = 263/182) were also recruited from the local community in Beijing. Their mean age was 44.9 ± 13.6 years (range 25–75), with a mean education of 9.7 ± 5.4 years. The mean body mass index (BMI) of the controls was 25.1 ± 4.2 kg/m2, while that of the patients was 24.7 ± 4.0 kg/m2. A research psychiatrist assessed current mental status and personal or family history of any mental disorder in controls by unstructured clinical interviews to exclude potential controls with Axis I disorders. None of them presented a personal or family history of psychiatric disorder.
We obtained a complete medical history, physical examination and laboratory tests from patients and control subjects. Any subjects with test abnormalities or medial illnesses were excluded. Neither schizophrenic patients nor control subjects suffered from drug or alcohol abuse/dependence. No schizophrenic patients took medications for treating physical diseases. All subjects were Han Chinese, and they gave written informed consent, which was approved by the Institutional Review Board of Beijing Hui-Long-Guan hospital.
Clinical measures
We assessed cognitive functioning using the repeatable battery for the assessment of neuropsychological status (RBANS, Form A) (Randolph et al. 1998). The RBANS was previously translated into Chinese by our group and its clinical validity and test–retest reliability established among controls and schizophrenic patients (Zhang et al. 2009).
Four psychiatrists who had simultaneously attended a training session in the use of the Positive and Negative Syndrome Scale (PANSS) rated patients on this scale. After training, repeated assessment showed that the interobserver correlation coefficient was maintained at >0.8 for the PANSS total score. We obtained blood samples to assess BDNF levels at the time of PANSS ratings.
Serum BDNF measurement
We measured fasting serum BDNF levels by sandwich ELISA using a commercially available kit as described in our previous report (Xiu et al. 2009). All samples were assayed by a research assistant blind to the clinical situation. Inter- and intra-assay variation coefficients were 7 and 5%, respectively.
Genotyping
The genotypes of the BDNF Val66Met polymorphisms were identified as reported in our previous study (Zhang et al. 2008). A research assistant who was blinded to the clinical status genotyped every subject twice for accuracy of genotyping.
Statistical analysis
Deviations from Hardy–Weinberg equilibrium (HWE) were assessed using the HWSIM program (Cubells et al. 1997). The BDNF Val66Met allele and genotype frequencies were compared between schizophrenic patients and healthy controls using χ2 tests. Group differences were compared using Student’s t test or one-way analysis of variance (ANOVA) for continuous variables and Chi-squared for categorical variables. Post hoc comparisons between subgroups were made using the Fisher’s least significant difference (LSD) procedure rather than the more conservative Bonferroni corrections for multiple comparisons. Correlation between variables was studied using Pearson product moment correlations.
For the main models, analyses of covariance (ANCOVA) was constructed with BDNF genotype as the independent variable, and the cognitive scores shown by the RBANS total and 5 index scores as dependent variables, with sex, age, education, illness course, age of onset, BMI, smoking, medication type (atypical vs. typical antipsychotics) and dose (chlorpromazine equivalents) and duration of treatment as the covariates. In each model, we tested the main effect of diagnostic group, the main effect of genotype and diagnostic group × genotype interaction. The diagnostic group × genotype interaction term in the model detects the differential effects that alleles might have on cognitive scores between diagnostic groups. We first contrasted the homozygote groups (Val/Val against Met/Met). When significant differences between homozygote groups were found, we formally assessed whether heterozygotes (Val/Met) had an intermediate level using a linear regression test. Similarly, we analyzed the main effect of the BDNF genotype on serum BDNF levels using ANCOVA.
Lastly, exploratory regression analyses were used to examine whether any relationships between BDNF serum levels and cognitive function differed across BDNF genotype groups. Stepwise multiple regression analysis used RBANS total or Index scores as dependent variables with BDNF levels as the independent variable in each BDNF genotype group. Covariates in these stepwise forward entry models included age, gender, education, BMI, smoking, duration of illness, age of onset, PANSS scores and antipsychotic medication dosage, type (typical vs. atypical antipsychotics) and duration.
Results
Demographic characteristics are summarized in Table 1. A significantly greater proportion of patients were male and smokers (both p < 0.01) and older (p < 0.001) than controls.
Distributions of the BDNF genotypes were consistent with HWE in both patients and controls (both p > 0.05) (Table 1). We found no significant differences in BDNF genotype and allele distributions between patients and controls (χ2 = 2.57, df = 2, p > 0.05 and χ2 = 2.37, df = 1, p > 0.05, respectively).
Genotype effects on cognitive functioning between patients and normal controls
RBANS data were available from 575 patients and 405 healthy controls. RBANS total and index scores, and the effects of the BDNF Val66Met polymorphism on the RBANS total and index scores are summarized in Table 2.
Cognitive test scores were significantly lower in schizophrenic than control subjects on the total scores and all indexes (all p < 0.000) except for visuospatial/constructional index (p > 0.05). There were no significant genotype effects or genotype × diagnosis effects for immediate memory, language, delayed memory and total scores.
As shown in Table 2, the three genotypes significantly differed on the visuospatial/constructional index (F = 4.25, p < 0.01), and using Fisher’s LSD to control for the two potential comparisons only the Val/Val versus Met/Met difference was significant (p = 0.03). This difference in performance between Val/Val and Met/Met genotypes held within the schizophrenia (p < 0.05) and the controls (p < 0.01) based on Fisher’s LSD. Inclusion of heterozygotes produced a significant linear correlation between the number of Met-66 alleles (e.g., zero, one or two alleles) and the visuospatial/constructional index score within the controls (p < 0.01), but not the schizophrenia (p = 0.07).
Further analysis showed a significant genotype × diagnosis effect on attention (Table 2) (F = 3.15, p < 0.05). Based on Fisher’s LSD comparison, this weak interaction reflected significantly higher attention index scores in patients who were Val homozygous than those who were Met homozygous (p < 0.05), while the controls showed no differences.
Genotype effects on serum BDNF levels between patients and normal controls
Serum BDNF levels were normally distributed in both patients and controls (Kolmogorov–Smirnov one-sample test: both p > 0.05). Table 3 revealed a significant main effect of diagnostic group on BDNF levels (F = 15.2, df = 664, p < 0.001). Male patients had significantly lower BDNF levels than female patients (p < 0.01; adjusted p < 0.01). However, BDNF levels were not significantly different between men and women in controls (p > 0.05).
There was no main effect of genotype on serum BDNF levels (p > 0.05) or genotype × diagnosis effect (p > 0.05). We observed no significant differences in BDNF levels between genotypic subgroups (Val/Val, Val/Met and Met/Met) in patients or controls (both p > 0.05) (Table 3). When sex and BMI were added as covariates, there were still no significant differences in BDNF levels in genotypic subgroups in patient and control groups (both p > 0.05), suggesting that BDNF genotype did not influence serum BDNF levels in the patient or control groups.
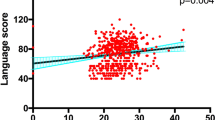
Differential effects of BDNF genotype on the relationships between BDNF serum levels and cognitive functioning
The patients showed a significant overall main effect of BDNF levels on the RBANS total score and its index scores (F = 2.59, df = 6, 411, p = 0.016). The BDNF level × genotype interaction was also statistically significant (F = 2.48, df = 6, 412, p = 0.023), indicating differences between genotypes in the relationships between BDNF levels and cognitive scores. A further partial correlation analysis showed a significant positive correlation between serum BDNF levels and the RBANS total score (r = 0.21, p < 0.03), and between BDNF levels and the immediate memory index (t = 3.22, p < 0.01). However, no significant effects of BDNF levels, BDNF genotype, gender and their interactions were found in the control group (all p > 0.05).
Regression analyses among Val homozygote patients found a significant negative association of BDNF levels with the delayed memory index (β = −0.36, t = −2.21, p = 0.04) and PANSS total score (β = −0.60, t = −3.52, p = 0.002). Among Met homozygote patients, increases in BDNF levels were significantly associated with better performance on the visuospatial/constructional index (β = 0.41, t = 2.89, p = 0.006). Among Met/Val heterozygous patients, BDNF levels were positively correlated with the attention (β = 0.59, t = 3.48, p = 0.001) and immediate memory indices (β = 0.46, t = 2.56, p = 0.013), but negatively correlated with smoking behavior (β = −0.33, t = −2.99, p = 0.004).
Discussion
Our results demonstrate that the BDNF Val66Met polymorphism may not contribute directly to the susceptibility to schizophrenia, although two previous studies reported such an association (Neves-Pereira et al. 2005; Rosa et al. 2006). Like our study, several studies did not replicate these earlier associations (Naoe et al. 2007; Varnäs et al. 2008), including studies in Han Chinese populations (Xu et al. 2007; Zhou et al. 2010; Yi et al. 2011). One possible explanation for the inconsistency is a difference in ethnic background, since we found the allele frequency distribution of Val66Met varied significantly between Chinese and Caucasian subjects. The Met allele frequency was around 50% in Chinese (Xu et al. 2007; Zhou et al. 2010; Yi et al. 2011), but around 20% in Caucasian subjects (Rosa et al. 2006; Naoe et al. 2007; Varnäs et al. 2008). In our current study, the Met allele frequency was 49.7% in control subjects, which is similar to other studies in Chinese (Xu et al. 2007; Zhou et al. 2010; Yi et al. 2011). Thus, interethnic differences in the genotype frequencies of the BDNF Val66Met polymorphism may play an important role in accounting for the inconsistent results across the different populations. Several other factors may also account for these divergent results, for example, small gene effects, heterogeneity of the schizophrenia diagnosis, and population stratification.
BDNF in human cognition and cognitive dysfunction among schizophrenia
We found significant differences in cognitive scores in nearly all of the post hoc pairwise comparisons between schizophrenics and controls except for the visuospatial/constructional index. These data replicate numerous studies indicating that patients with schizophrenia perform worse than controls on a range of cognitive tasks (Sharma and Antonova 2003; Kraus and Keefe 2007). In fact, we found that the absolute difference between the mean RBANS total scores of the two groups was more than 16 points (78.4 vs. 61.9), which is similar to a result by Dickerson et al. (2004).
We found that Met allele carriers, regardless of whether they were healthy controls or patients with schizophrenia, consistently performed worse than their Val homozygous counterparts on the visuospatial/constructional index. Moreover, we found a significant linear correlation between the number of Met66 alleles and the visuospatial/constructional index score in both patients and controls. The underlying mechanisms that are responsible for the Met66 allele’s influence on this cognitive measure are unknown. However, studies have shown that the BDNF Val66Met polymorphism is related to hippocampal-mediated memory performance in humans (Egan et al. 2003; Hariri et al. 2003). Hippocampal neurons that are transfected with the Met variant of BDNF show less depolarization-induced BDNF secretion (Chen et al. 2004). The Met variant results in inefficient trafficking of BDNF to secretory granules, reduced activity-dependent BDNF release and poorer hippocampal-mediated memory (Egan et al. 2003). Overall, Met allele carriers, regardless of whether they are controls or patients with schizophrenia, or unaffected siblings demonstrate poorer episodic memory than their respective Val-homozygous counterparts (Egan et al. 2003; Dempster et al. 2005). The patients who are Met allele carriers have lower hippocampal function while performing a declarative memory task as assessed with functional MRI blood oxygenation level responses (Hariri et al. 2003). These Met allele patients also have reduced hippocampal and prefrontal gray matter (Szeszko et al. 2005; Bueller et al. 2006). Ho et al. (2007) found the BDNF 66Met variant correlates with reduced gray matter volumes within temporal and occipital lobes, brain regions known to participate in verbal memory and visuospatial abilities in both normal controls and patients with schizophrenia. The convergence of these cognitive and brain morphology findings suggests that the BDNF Val66Met polymorphism influences specific aspects of human cognition. Our current study also indicated the association between the BDNF Met-66 variant and poor visuospatial/constructional performance, but this genotype status did not appear to impact total cognitive function, or affect language, immediate and delayed memory performances.
Visuospatial performance is subserved by large scale-distributed neuronal networks. Object perception involves the ventral occipito-temporal, whereas processing spatial information involves the dorsal occipito-parietal pathway. Therefore, brain regions that mediate visuospatial abilities include the secondary visual cortices, inferior temporal regions, and the parietal heteromodal association cortices (Ho et al. 2007). Patients with schizophrenia and healthy controls who carry the Met allele have smaller temporal and occipital lobar GM volumes than their respective Val-homozygous counterparts, and those patients with the BDNF Met-66 allele are significantly more impaired in visuospatial abilities than patients who are Val homozygous (Ho et al. 2007).
The BDNF 66Met variant also may have a specific role in attentional dysfunction among schizophrenics. Unlike controls, patients with schizophrenia who carry the Met allele consistently performed worse than their Val-homozygous counterparts on attentional performance. In our current studies this common SNP showed different effects on cognitive function in patients with schizophrenia than in healthy controls. However, the mechanisms by which the BDNF Val66Met variant affects attention are not well understood. Hence, the differential effects of the BDNF Val66Met genotype on attention in patients with schizophrenia and healthy controls deserve further investigation.
Our cognitive index test findings about the differences between schizophrenia and controls across the three BDNF Val66Met genotypes remained significant in key comparisons between the two homozygous genotypes using Fisher’s LSD for group comparisons. However, the heterozygous genotype did not differ from either homozygous group among the schizophrenia, suggesting that the effects of the BDNF Val66Met genotype on some aspects of cognitive function may be moderate. Moreover, the genotype by diagnosis interaction on attention was difficult to evaluate especially without modest sample size. Therefore, our results should be interpreted with caution.
Previous studies reported associations of the Met allele with deficits in memory functions (Egan et al. 2003; Hariri et al. 2003; Dempster et al. 2005; Ho et al. 2007), but we found associations with visuospatial and attention more than memory. These other aspects of neuropsychological functioning are clearly not independent of memory and cultural aspects of learning. One possible explanation for discrepant association findings between Met allele with cognitive functioning is differences in population genetic structure between patient samples. For example, a recent population-based genetic study showed that the derived Met allele of the Val66Met polymorphism increased in frequency from 0.55 to 19.9% and 43.6% frequency in Sub-Saharan Africa, Europe and Asia, respectively (Petryshen et al. 2010). Furthermore, this study examined haplotypes comprising 12 BDNF SNPs and observed considerable haplotype diversity among global populations (Petryshen et al. 2010), suggesting substantial population diversity at the BDNF locus. Thus, interethnic differences in the genotype frequencies of the BDNF gene Val66Met polymorphism may play an important role that may account for the inconsistent results between Met allele with cognitive functioning seen in different samples from the different populations. On the other hand, quantitative and molecular genetic studies have established that there are additive genetic contributions to different aspects of cognitive ability, especially general intelligence, which involves several genes of small effects that interact to express the different aspects of cognition (Deary et al. 2010). However, whether some cognition-related candidate genes are related to different aspects of cognition in different population is still unclear. Hence, whether this discrepancy may be related to the interethnic differences in the allelic frequencies of the BDNF gene polymorphisms between different populations or complex genetic mechanisms related to different aspects of cognition deserve further investigations.
Decreased serum BDNF levels and cognitive impairment: relationship to BDNF Val66Met genotype
We showed decreased serum levels of BDNF in patients with a chronic form of schizophrenia, which replicates our previous studies (Xiu et al. 2009; Zhang et al. 2008) and is consistent with others (Rizos et al. 2008) but not all (Vinogradov et al. 2009). Numerous factors may have contributed to these differences, such as the clinical status of patients, the subtypes of schizophrenic patients recruited, and the type, dosage and length of administration of antipsychotic drugs (Rizos et al. 2008).
Only one recent study has shown that serum BDNF levels were increased in chronic schizophrenic patients after cognitive training, and BDNF levels were correlated with cognitive performance (Vinogradov et al. 2009). In our present study, BDNF was associated with cognition in schizophrenics but not in healthy controls, suggesting that the effects of serum BDNF on cognitive function differ between patients with schizophrenia and healthy control. Furthermore, the BDNF Val66Met polymorphism affects the correlation between BDNF levels and different aspects of cognitive function in schizophrenic patients.
We found higher serum BDNF levels associated with better cognitive function in schizophrenia, which is consistent with two recent studies in healthy older adults showing higher serum BDNF levels associated with better neuropsychological function (Gunstad et al. 2008; Komulainen et al. 2008). The exact mechanisms responsible for these findings are unknown. One possible explanation is the neuroprotective effects of BDNF. BDNF plays a key role in modulating synaptic transmission and plasticity (Shimizu et al. 2003), and has been hypothesized to be an important factor in the induction of LTP, a persistent strengthening of synapses associated with learning and memory (Lu et al. 2008). Preclinical studies show that LTP is impaired in mice lacking the BDNF gene (Tyler et al. 2002), and LTP can be restored with adenovirus-mediated transfection of these mutant mouse CA1 cells with the BDNF gene. Taken together, these results support a mechanism linking cognitive function and BDNF levels.
Yet, it is noteworthy that the source of circulating BDNF remains unknown. Although BDNF is highly concentrated in the nervous system, it is also present in peripheral blood with high concentrations in serum (Radka et al. 1996). A recent study found a significant correlation between BDNF levels in plasma and cerebrospinal fluid (CSF) of unmedicated schizophrenic patients (Pillai et al. 2010). Accordingly, if low peripheral BDNF levels reflect low levels in the brain, this could affect cognitive function in patients with schizophrenia. Indeed, we showed that increased BDNF serum levels were correlated with better performance on visuospatial/constructional ability for the Met/Met genotype, as well with better performance on attention and immediate memory abilities for the Met/Val heterozygous. In contrast, increased BDNF serum levels were associated with poor delayed memory performance for the Val/Val genotype. The clinical significance of these divergent serum BDNF–cognitive function relationships across BDNF genotypes in schizophrenia remains unclear. Further studies are needed to determine the association of peripheral BDNF levels and cognitive function in patients with schizophrenia and possibly other psychiatric disorders or subtypes of schizophrenia (Lencz et al. 2009).
Like many others, we found that the serum BDNF levels were lower among the schizophrenic patients, but were not related to the val66met genotype. For example, the Val66Met polymorphism was unrelated to the concentration of BDNF in whole blood in a healthy European sample (n = 78) (Trajkovska et al. 2007) and was also unrelated to plasma or serum concentrations of BDNF in several healthy Asian samples (Yu et al. 2008). However, a recent healthy European sample (n = 114) showed an association between the Val66Met genotype and serum BDNF concentrations, such that individuals with the Met allele had higher BDNF levels (Lang et al. 2009). Interestingly, other variants rather than the Val66Met variant in the BDNF gene might regulate the level of serum BDNF, as identified in a recent Italian community-based sample (n = 2,054) (Terracciano et al. 2011). The BDNF Val66Met polymorphism may indeed have an association with serum BDNF levels only among some ethnic groups, with Asians not having this association. Moreover, the Met variant has been hypothesized to decrease the activity dependent but not the constitutive BDNF secretion, which our studies assess (Tramontina et al. 2007). Finally, we are assessing serum, not brain BDNF levels, although Klein et al. (2011) recently reported that blood and plasma BDNF levels reflect brain-tissue BDNF levels.
In conclusion, we have provided new evidence to support the association between the BDNF 66Met variant and poor visuospatial/constructional performance in both patients with schizophrenia and healthy controls, suggesting a specific role of the BDNF 66Met variant in some aspects of poor cognitive function. The present study indicates that peripheral BDNF levels may be a biomarker of general cognitive function in schizophrenia. The association between decreased serum BDNF levels and the degree of cognitive impairment in schizophrenic patients appears to be dependent on the presence of BDNF Val66Met polymorphism.
References
Altar CA, Cai N, Bliven T, Juhasz M, Conner JM, Acheson AL, Lindsay RM, Wiegand SJ (1997) Anterograde transport of brain-derived neurotrophic factor and its role in the brain. Nature 389(6653):856–860
Bueller JA, Aftab M, Sen S, Gomez-Hassan D, Burmeister M, Zubieta JK (2006) BDNF Val66Met allele is associated with reduced hippocampal volume in healthy subjects. Biol Psychiatry 59(9):812–815
Chen ZY, Patel PD, Sant G, Meng CX, Teng KK, Hempstead BL, Lee FS (2004) Variant brain-derived neurotrophic factor (BDNF) (Met66) alters the intracellular trafficking and activity-dependent secretion of wild-type BDNF in neurosecretory cells and cortical neurons. J Neurosci 24(18):4401–4411
Ciammola A, Sassone J, Cannella M, Calza S, Poletti B, Frati L, Squitieri F, Silani V (2007) Low brain-derived neurotrophic factor (BDNF) levels in serum of Huntington’s disease patients. Am J Med Genet B Neuropsychiatr Genet 144B(4):574–577
Cubells JF, Kobayashi K, Nagatsu T, Kidd KK, Kidd JR, Calafell F, Kranzler HR, Ichinose H, Gelernter J (1997) Population genetics of a functional variant of the dopamine beta-hydroxylase gene (DBH). Am J Med Genet 74(4):374–379
Deary IJ, Penke L, Johnson W (2010) The neuroscience of human intelligence differences. Nat Rev Neurosci 11(3):201–211
Dempster E, Toulopoulou T, McDonald C, Bramon E, Walshe M, Filbey F, Wickham H, Sham PC, Murray RM, Collier DA (2005) Association between BDNF val66 met genotype and episodic memory. Am J Med Genet B Neuropsychiatr Genet 134B(1):73–75
Dickerson F, Boronow JJ, Stallings C, Origoni AE, Cole SK, Yolken RH (2004) Cognitive functioning in schizophrenia and bipolar disorder: comparison of performance on the repeatable battery for the assessment of neuropsychological status. Psychiatry Res 129(1):45–53
Egan MF, Kojima M, Callicott JH, Goldberg TE, Kolachana BS, Bertolino A, Zaitsev E, Gold B, Goldman D, Dean M, Lu B, Weinberger DR (2003) The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell 112:257–269
Granholm E, McQuaid JR, Link PC, Fish S, Patterson T, Jeste DV (2008) Neuropsychological predictors of functional outcome in cognitive behavioral social skills training for older people with schizophrenia. Schizophr Res 100(1–3):133–143
Gunstad J, Benitez A, Smith J, Glickman E, Spitznagel MB, Alexander T, Juvancic-Heltzel J, Murray L (2008) Serum brain-derived neurotrophic factor is associated with cognitive function in healthy older adults. J Geriatr Psychiatry Neurol 21(3):166–170
Guzowski JF, Lyford GL, Stevenson GD, Houston FP, McGaugh JL, Worley PF, Barnes C (2000) Inhibition of activity-dependent arc protein expression in the rat hippocampus impairs the maintenance of long-term potentiation and the consolidation of long-term memory. J Neurosci 20(11):3993–4001
Hariri AR, Goldberg TE, Mattay VS, Kolachana BS, Callicott JH, Egan MF, Weinberger DR (2003) Brain-derived neurotrophic factor val66met polymorphism affects human memory-related hippocampal activity and predicts memory performance. J Neurosci 23(17):6690–6694
Harvey PD (2009) Pharmacological cognitive enhancement in schizophrenia. Neuropsychol Rev 19:324–335
Harvey PD, Geyer MA, Robbins TW, Krystal JH (2003) Cognition in schizophrenia: from basic science to clinical treatment. Psychopharmacology 169:213–214
Ho BC, Andreasen NC, Dawson JD, Wassink TH (2007) Association between brain-derived neurotrophic factor Val66Met gene polymorphism and progressive brain volume changes in schizophrenia. Am J Psychiatry 164(12):1890–1899
Hughes C, Kumari V, Soni W, Das M, Binneman B, Drozd S, O’Neil S, Mathew V, Sharma T (2003) Longitudinal study of symptoms and cognitive function in chronic schizophrenia. Schizophr Res 59(2–3):137–146
Kaneda Y, Jayathilak K, Meltzer HY (2009) Determinants of work outcome in schizophrenia and schizoaffective disorder: role of cognitive function. Psychiatry Res 169(2):178–179
Klein AB, Williamson R, Santini MA, Clemmensen C, Ettrup A, Rios M, Knudsen GM, Aznar S (2011) Blood BDNF concentrations reflect brain-tissue BDNF levels across species. Int J Neuropsychopharmacol 14(3):347–353
Komulainen P, Pedersen M, Hänninen T, Bruunsgaard H, Lakka TA, Kivipelto M, Hassinen M, Rauramaa TH, Pedersen BK, Rauramaa R (2008) BDNF is a novel marker of cognitive function in ageing women: the DR’s EXTRA Study. Neurobiol Learn Mem 90(4):596–603
Kraus MS, Keefe RS (2007) Cognition as an outcome measure in schizophrenia. Br J Psychiatry 50:46–51
Lang UE, Hellweg R, Sander T, Gallinat J (2009) The Met allele of the BDNF Val66Met polymorphism is associated with increased BDNF serum concentrations. Mol Psychiatry 14(2):120–122
Lencz T, Lipsky RH, DeRosse P, Burdick KE, Kane JM, Malhotra AK (2009) Molecular differentiation of schizoaffective disorder from schizophrenia using BDNF haplotypes. Br J Psychiatry 194(4):313–318
Lieberman JA, Perkins D, Belger A, Chakos M, Jarskog F, Boteva K, Gilmore J (2001) The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry 50(11):884–897
Lu B, Gottschalk W (2000) Modulation of hippocampal synaptic transmission and plasticity by neurotrophins. Prog Brain Res 128:231–241
Lu Y, Christian K, Lu B (2008) BDNF: a key regulator for protein synthesis-dependent LTP and long-term memory? Neurobiol Learn Mem 89(3):312–323
Naoe Y, Shinkai T, Hori H, Fukunaka Y, Utsunomiya K, Sakata S, Matsumoto C, Shimizu K, Hwang R, Ohmori O, Nakamura J (2007) No association between the brain-derived neurotrophic factor (BDNF) Val66Met polymorphism and schizophrenia in Asian populations: evidence from a case-control study and meta-analysis. Neurosci Lett 415(2):108–112
Neves-Pereira M, Cheung JK, Pasdar A, Zhang F, Breen G, Yates P, Sinclair M, Crombie C, Walker N, St Clair DM (2005) BDNF gene is a risk factor for schizophrenia in a Scottish population. Mol Psychiatry 10(2):208–212
Petryshen TL, Sabeti PC, Aldinger KA, Fry B, Fan JB, Schaffner SF, Waggoner SG, Tahl AR, Sklar P (2010) Population genetic study of the brain-derived neurotrophic factor (BDNF) gene. Mol Psychiatry 15(8):810–815
Pillai A, Kale A, Joshi S, Naphade N, Raju MS, Nasrallah H, Mahadik SP (2010) Decreased BDNF levels in CSF of drug-naive first-episode psychotic subjects: correlation with plasma BDNF and psychopathology. Int J Neuropsychopharmacol 13(4):535–553
Poo MM (2001) Neurotrophins as synaptic modulators. Nat Rev Neurosci 2(1):24–32
Radka SF, Holst PA, Fritsche M, Altar CA (1996) Presence of brain-derived neurotrophic factor in brain and human and rat but not mouse serum detected by a sensitive and specific immunoassay. Brain Res 709(1):122–301
Randolph C, Tierney MC, Mohr E, Chase TN (1998) The repeatable battery for the assessment of neuropsychological status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol 20:310–319
Rizos EN, Rontos I, Laskos E, Arsenis G, Michalopoulou PG, Vasilopoulos D, Gournellis R, Lykouras L (2008) Investigation of serum BDNF levels in drug-naive patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 32:1308–1311
Rosa A, Cuesta MJ, Fatjó-Vilas M, Peralta V, Zarzuela A, Fañanás L (2006) The Val66Met polymorphism of the brain-derived neurotrophic factor gene is associated with risk for psychosis: evidence from a family-based association study. Am J Med Genet B Neuropsychiatr Genet 141B(2):135–138
Sharma T, Antonova L (2003) Cognitive function in schizophrenia. Deficits, functional consequences, and future treatment. J Psychopharmacol 17(1):89–95
Shimizu E, Hashimoto K, Watanabe H, Komatsu N, Okamura N, Koike K, Shinoda N, Nakazato M, Kumakiri C, Okada S, Iyo M (2003) Serum brain-derived neurotrophic factor (BDNF) levels in schizophrenia are indistinguishable from controls. Neurosci Lett 351:111–114
Szeszko PR, Lipsky R, Mentschel C, Robinson D, Gunduz-Bruce H, Sevy S, Ashtari M, Napolitano B, Bilder RM, Kane JM, Goldman D, Malhotra AK (2005) Brain-derived neurotrophic factor val66met polymorphism and volume of the hippocampal formation. Mol Psychiatry 10(7):631–636
Terracciano A, Piras MG, Lobina M, Mulas A, Meirelles O, Sutin AR, Chan W, Sanna S, Uda M, Crisponi L, Schlessinger D (2011) Genetics of serum BDNF: meta-analysis of the Val66Met and genome-wide association study. World J Biol Psychiatry [Epub ahead of print]
Trajkovska V, Marcussen AB, Vinberg M, Hartvig P, Aznar S, Knudsen GM (2007) Measurements of brain-derived neurotrophic factor: methodological aspects and demographical data. Brain Res Bull 73(1–3):143–149
Tramontina J, Frey BN, Andreazza AC, Zandona M, Santin A, Kapczinski F (2007) Val66met polymorphism and serum brain-derived neurotrophic factor levels in bipolar disorder. Mol Psychiatry 12(3):230–231
Tyler WJ, Alonso M, Bramham CR, Pozzo-Miller LD (2002) From acquisition to consolidation: on the role of brain-derived neurotrophic factor signaling in hippocampal-dependent learning. Learn Mem 9(5):224–237
Varnäs K, Lawyer G, Jönsson EG, Kulle B, Nesvåg R, Hall H, Terenius L, Agartz I (2008) Brain-derived neurotrophic factor polymorphisms and frontal cortex morphology in schizophrenia. Psychiatr Genet 18(4):177–183
Vinogradov S, Fisher M, Holland C, Shelly W, Wolkowitz O, Mellon SH (2009) Is serum brain-derived neurotrophic factor a biomarker for cognitive enhancement in schizophrenia? Biol Psychiatry 66(6):549–553
Xiu MH, Hui L, Dang YF, Hou TD, Zhang CX, Zheng YL, da Chen C, Kosten TR, Zhang XY (2009) Decreased serum BDNF levels in chronic institutionalized schizophrenia on long-term treatment with typical and atypical antipsychotics. Prog Neuropsychopharmacol Biol Psychiatry 33(8):1508–1512
Xu MQ, St Clair D, Ott J, Feng GY, He L (2007) Brain-derived neurotrophic factor gene C-270T and Val66Met functional polymorphisms and risk of schizophrenia: a moderate-scale population-based study and meta-analysis. Schizophr Res 91(1–3):6–13
Yi Z, Zhang C, Wu Z, Hong W, Li Z, Fang Y, Yu S (2011) Lack of effect of brain derived neurotrophic factor (BDNF) Val66Met polymorphism on early onset schizophrenia in Chinese Han population. Brain Res 1417:146–150
Yu H, Zhang Z, Shi Y, Bai F, Xie C, Qian Y, Yuan Y, Deng L (2008) Association study of the decreased serum BDNF concentrations in amnestic mild cognitive impairment and the Val66Met polymorphism in Chinese Han. J Clin Psychiatry 69(7):1104–1111
Zhang XY, Zhou DF, Wu GY, Cao LY, Tan YL, Haile CN, Li J, Lu L, Kosten TA, Kosten TR (2008) BDNF levels and genotype are associated with antipsychotic-induced weight gain in patients with chronic schizophrenia. Neuropsychopharmacology 33(9):2200–2205
Zhang BH, Tan YL, Zhang WF, Wang ZR, Yang GG, Shi C, Zhang XY, Zhou DF (2009) Repeatable battery for the assessment of neuropsychological status (RBANS) as a screening test in Chinese: reliability and validity. Chin Ment Health J 28:865–869
Zhou DH, Yan QZ, Yan XM, Li CB, Fang H, Zheng YL, Zhang CX, Yao HJ, Chen da C, Xiu MH, Kosten TR, Zhang XY (2010) The study of BDNF Val66Met polymorphism in Chinese schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry 34(6):930–933
Acknowledgment
This study was funded by the Stanley Medical Research Institute (03T-459 and 05T-726), and the Department of Veterans Affairs, VISN 16, Mental Illness Research, Education and Clinical Center (MIRECC), United States National Institute of Health K05-DA0454, P50-DA18827 and U01-MH79639.
Conflict of interest
No conflict of interest was disclosed for each author.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhang, X.Y., Chen, D.C., Xiu, M.H. et al. Cognitive and serum BDNF correlates of BDNF Val66Met gene polymorphism in patients with schizophrenia and normal controls. Hum Genet 131, 1187–1195 (2012). https://doi.org/10.1007/s00439-012-1150-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-012-1150-x