Abstract
Advanced maternal age is a well-documented risk factor of chromosome 21 nondisjunction in humans, but understanding of this association at the genetic level is still limited. In particular, the state of maternal genetic age is unclear. In the present study, we estimated maternal genetic age by measuring telomere length of peripheral blood lymphocytes among age-matched mothers of children with Down syndrome (cases: N = 75) and mothers of euploid children (controls: N = 75) in an age range of 18–42 years. All blood samples were taken within 1 week of the birth of the child in both cases and controls. The telomere length estimation was performed by restriction digestion—Southern blot hybridization method. We stratified the cases on the basis of centromeric STR genotyping into maternal meiosis I (N = 48) and maternal meiosis II (N = 27) nondisjunction groups and used linear regression to compare telomere length as a function of age in the euploid, meiosis I and meiosis II groups. Our results show that all three groups have similar telomere length on average for younger mothers. As age increases, all groups show telomere loss, but that loss is largest in the meiosis II mother group and smallest in the euploid mother group with the meiosis I mother group in the middle. The regression lines for all three were statistically significantly different from each other (p < 0.001). Our results do not support the theory that younger women who have babies with Down syndrome do so because are ‘genetically older’ than their chronological age, but we provide the first evidence that older mothers who have babies with Down syndrome are “genetically older” than controls, who have euploid babies at the same age. We also show for the first time that telomere length attrition may be associated in some way with meiosis I and meiosis II nondisjunction of chromosome 21 and subsequent Down syndrome births at advanced maternal age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association between advanced maternal age and higher incidence of Trisomy 21 Down syndrome (DS) is well known (Allen et al. 2009), particularly for cases where nondisjunction (NDJ) occurs at oogenesis (Sherman et al. 2007). It has been estimated that the percentage of trisomic conceptuses among all clinically recognized pregnancies increases from 2% for women <25 years of age to 35% for women >40 years of age (Hassold and Chiu 1985). Since the oocytes experience meiotic arrest from fetal life to the time of ovulation, several factors may be involved with aging of the oocyte proper or its milieu (Warburton 2005). These include factors maintaining sister chromatid adhesion (Jeffreys et al. 2003), meiotic checkpoints (Zwick et al. 1999) or spindle apparatus (Hawley et al. 1994). Age-related degradations of these systems may increase the risk of NDJ both at meiosis I (MI) and meiosis II (MII) (Yoon et al. 1996). In addition, accumulation of environmentally induced damage to the meiotic machinery over time and/or genetic changes such as mitochondrial deletion (Van Blerkom 2004) may induce aging of the ovary and perturb proper segregation of chromosomes.
In establishing the relationship between maternal age and higher incidence of aneuploid gamete formation, the theory of “biological aging” has been proposed (Warburton 2005). This theory states that biological aging would differ among women of the same chronological age and that the frequency of trisomic conceptions depends upon the biological age of women rather than on the chronological age. Each menstrual cycle of a woman is associated with gradual maturation of antral follicles and it has been estimated that the number of antral follicles also declines with increasing maternal age (Kline et al. 2004). This decline in the number of antral follicles together with an accompanying decrease in the total oocyte pool generates a change in the hormonal environment of the ovary, which causes meiotic errors. Support for this prediction comes from studies in which elevated levels of FSH were found to be more common in women after a DS birth than in controls (van Montfrans et al. 2002). Elevated levels of FSH/estradiol have also been found to be associated with chromosomally abnormal spontaneous abortions (Nasseri et al. 1999). This relationship between hormonal imbalance and increased rate of aneuploidy has also been established experimentally in mice (Roberts et al. 2005) and in in vitro-fertilized human oocytes (Kline et al. 2005). Additionally, studies on human preovulatory oocytes (Volarcik et al. 1998) have shown that oocytes taken from women ≥35 years are more likely to undergo misdivision at MI followed by an abnormal alignment of chromosomes on spindle at MII. These data indicate that oocytes are predisposed to abnormal division before the resumption of MI. Moreover, mathematical modeling has also shown that the age of menopause is a predictor of ovarian age (Kline and Levin 1992) and the model has estimated an earlier menopause among women with trisomic pregnancies than among controls. This notion was later supported by a population-based study (Kline et al. 2000).
The telomere, the end of the eukaryotic chromosome, contains (TTAGGG) n repeats (Allshire et al. 1989). It exhibits replicative shortening in aging cells and is considered by many (Benetos et al. 2001; Cawthon et al. 2003; Njajou et al. 2007) to be a genetic marker for estimating aging and cellular senescence as the association between shorter telomere length (TL) and biological aging is evident in both human (Aviv 2008) and mouse (Martinez et al. 2009). Correlation between loss of telomeric repeat in somatic cells and shorter reproductive life span due to ovarian aging has been reported in several studies (Aydos et al. 2005; Keefe and Liu 2009). With respect to DS birth, however, the only study we are aware of (Dorland et al. 1998) did not detect any statistically significant difference in TL between younger mothers bearing a live born DS baby and age-matched controls with an euploid child. In addition, a very recent study (Hanna et al. 2009) on women with a history of recurrent miscarriages of a trisomic fetus found similar TL between cases and controls combining all age categories.
In the present study, we consider TL of maternal origin DS bearing mothers over a range of reproductive ages, and compare age-matched controls using a cross-sectional design. That is, all subjects gave birth within a week before blood samples were collected, but were not followed longitudinally. In addition, we stratified our DS mother population by meiotic outcome groups, i.e., MI and MII to determine whether TL is associated with types of NDJ.
Subjects and methods
Subjects
Three case women and three control women were recruited for each year of age, from 18 to 42 years, for a total of 75 controls and 75 cases with maternal NDJ (two paternal cases were excluded from the total collected blood samples after genotyping; see ‘Genotyping’). The three women at each age were selected randomly to minimize the sampling bias. Blood samples of mothers, children and fathers were collected between 2006 and 2008 from different Medical Colleges and Hospitals of Kolkata. The collections were done very carefully within a week of the birth of the child for both cases and controls. This ensured that the maternal age at which TL is estimated is the same as maternal age at the time of birth. The families (cases and controls) were absolutely unrelated between and within the groups and heterogeneous in respect to their religion and socio-economic status. A detailed family history with informed consent was taken from each participating family. The design of experiments with human tissue samples and subsequent data analyses were reviewed and approved by the institutional ethics committee constituted by the West Bengal University of Technology.
Cytogenetic analysis
To include only the free trisomy 21 cases and exclude mothers with hidden mosaicism, conventional karyotyping was performed. At least 30 metaphase plates were analyzed for each to confirm the chromosomal profiles of cases and controls.
Genotyping
Genotyping was performed in cases only to determine the parental origin and stage of trisomy, so that we could limit our study to maternal MI and MII cases. We used ten highly polymorphic STR markers spanning pericentric region to telomere of 21q. The order of markers was centromere–D21S1432–D21S11–D21S1437–D21S1270–D21S167–D21S1412–D21S2055–D21S1260–D21S1411–D21S1446–qter. The maternal origin of NDJ was determined by establishing contribution of maternal alleles to the DS child. The decision was considered confirmed when at least two markers were informative and the allelic status of the rest of the markers was consistent with that inference. We used additional four pericentric STR markers to determine the stage of meiotic origin of NDJ, i.e., MI errors or MII errors. The markers were D21S369, D21S215, D21S258 and D21S120. We inferred an MI error when parental heterozygosity of these markers was retained in the trisomic child (‘nonreduced’). If parental heterozygosity was ‘reduced’ to homozygosity in the trisomic child, we concluded that the case was of MII origin.
Determination of telomere length
The analysis was done with the kit TeloTAGGG Telomere length Assay [Cat. No.2 209 136 001] from Roche chemicals. The DNA samples (10 µg) were digested with HinfI and RsaI (20 U/µl each), following the method described in the kit. The digested DNA was resolved in 0.8% agarose gel. The gel was dried, denatured, neutralized and then transfer of DNA fragments to the membrane was done by Southern blot technique. UV radiation was used to fix the fragments on the membrane. The membrane was then hybridized with the labeled telomere-specific probe provided in the kit. Autoradiogram was obtained after exposing the membrane to X-ray film. The signal intensity, i.e. density, was recorded and calculated using the freely available NIH software Image. The signal was optimized and subdivided into 1-kbp intervals. The telomere restriction fragment or TRF length (L) was estimated using the formula L = Σ(OD i )/Σ(OD i )/(L i ), where OD i was the signal intensity and L i was the length of the TRF fragment at midpoint of position i. The calculation took into account the higher signal intensity from larger TRF because of multiple hybridization of the telomere-specific probe. TL determination was done blinded to MI/MII origin, but not to case–control status.
Statistical analysis
The experimentally recorded TRF length values were used as the outcome variable in linear regression analyses. We fit separate models predicting TL from age in controls, cases with MI NDJ, cases with MII NDJ and cases in combination. We also fit a joint model that included all women, and incorporated age × group interaction terms. The age × group interaction specifically tests whether any changes in telomere length with age are same in the different groups. The rates of telomere shortening were scored in kbp/year from the slopes of regression lines. Statistical significance was tested using standard regression t statistics. In addition, we stratified women into three age groups, viz., young (18–25 years), middle (26–34 years) and old (35–42 years) to test whether the TL was different across the groups (euploid, MI and MII) in each age category.
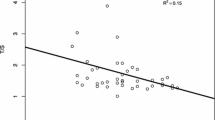
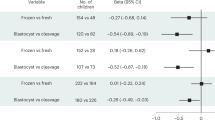
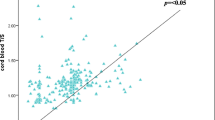
Results
Figure 1 shows the regression line for TL versus age in controls. Figure 2 shows all cases together, while Figs. 3 and 4 show MI and MII cases, respectively. The regression t test shows highly significant declines in TL with age in all groups (p = 0.001 for euploid, p = 0.005 for MI, p < 0.001 for MII). The estimated rate of telomere shortening was 61 bp/year in the euploid mother group. For MII mothers, the estimated TL shortening rate was 111 bp/year and in MII mothers it was 230 bp/year. The model with interaction term showed statistically significant differences between these loss rates (p < 0.001 for euploid vs. MI, p < 0.001 for euploid vs. MII, p = 0.001 for MI vs. MII). Telomere loss with age is greatest in the MII group, followed by MI group, with the least loss in controls.
A notable aspect of our results is that contrary to our predictions, the regression lines do not predict shorter TL among young DS mothers than among young controls. Young women in control, MI and MII groups had very similar TL. Rather the difference appeared among older women. To statistically test this observation, we grouped women by age (see Subjects and methods) and performed t tests to compare TL among control, MI and MII mothers in each age group (Table 1). There were no statistically significant differences between any groups at young or middle ages, but for the older mothers all groups showed statistically significant differences (p = 0.004 for MI vs. MII, p < 0.001 for MI vs. control and p < 0.001 for MII vs. control).
Discussion
The effect of maternal age on DS birth is intriguing. Previous studies suggested an early onset of ovarian aging and menopause as estimated from rapid fall of FSH level (Kline and Levin 1992; Thum et al. 2008) among women bearing a DS baby. Moreover, association among premature genetic aging, decline in TL with subsequent age-related meiotic dysfunction was reported in women (Keefe et al. 2007) and increased risk of NDJ has been evident in mouse (Liu and Keefe 2002; Liu et al. 2004). Considering these findings, it is a natural hypothesis that women having a trisomy 21 child at a young age suffer from early and accelerated genetic aging in comparison to the mothers of euploid children. To test this, we estimated the TL in peripheral blood lymphocytes and then recorded the change in repeat length as a function of maternal age in a range from 18 to 42 years. In addition, we were curious whether types of meiotic error is associated with maternal genetic age, as this issue has not been explored in human to best of our knowledge. We compared the estimated TL of controls, MI and MII cases across the age range.
Our results indicate that among DS bearing mothers, telomeres are much shorter in older mothers than younger mothers. This decrease with age is greater in MII mothers than in MI mothers, and both show a greater decrease than control mothers. Note that these results cannot be interpreted as saying that case women experience rapid genetic aging over the years, as we did not measure the change in TL over the years in a single mother. We compared women who had DS child at young ages with women who had a DS child at older ages. Our study sheds no light on what TL would be expected in older women who had a DS child when they were young.
The most intriguing aspect of our result is that the differences in TL we observed among three groups are only apparent in older women, not in younger, i.e., young MI and MII cases and young controls did not differ in their genetic age and this is some what contrary to our expectation. In other words, our work does not support the theory that young mothers have DS children because their genetic aging has been accelerated. This finding, however, is consistent with the previous result (Dorland et al. 1998), showing no difference in genetic age among young DS mothers and young controls. What we did find is a highly significant difference in genetic age among older cases and controls, with MII mothers genetically oldest among three. This result is quite new, and the interpretation is somewhat open to speculation.
One possible interpretation of our results in older women is that our control mothers are actually ‘abnormal’ in that they had successful euploid pregnancies at advanced ages. Perhaps, these women actually have “decelerated aging”, some protective factor keeping their telomeres long. A comparison with other TL literature, however, suggests that this is probably not the case. While other studies were done in very different ethnic groups and in both men and women, they have consistently estimated TL loss rates that are more similar to our controls than to our cases. For example, one recent study (Njajou et al. 2007) involving estimation of TL in a large euploid Amish cohort predicted a TL decline rate of approximately 28 bp/year. Similar trends of TL decline have also been observed in French (Benetos et al. 2001) and Scottish (Batty et al. 2009) cohorts for which the estimated telomere shortening rates are 36 and 85 bp/year, respectively. Moreover, the significant difference in TL among older MI and MII mothers (p = 0.004) that we observed in our dataset strengthens the argument that MI and MII mothers do not show a normal rate of telomere attrition, otherwise they would have similar trends of TL shortening.
Thus, our data support the hypothesis of some alteration in TL among DS mothers, but it is apparently primarily present in older DS mothers. This observation in turn suggests that the factor that induces rapid telomere loss at advanced reproductive age might simultaneously affect the chromosome separation system in oocyte. Alternatively, it is possible that the system maintaining normal TL is related to the apparatus of meiotic chromosome segregation and age-related deterioration in this system simultaneously affects both. In this connection, the effect of environmental degradation is of particular interest as exposure to reactive oxygen species (ROS) has been associated with DNA breaks and subsequent telomere shortening (Chen et al. 2007; Sebastián et al. 2009). On the other hand, ROS probably affects the normal ovarian function by altering hormone concentration (Mendola et al. 2008) that might cause reduction in meiotic competence characterized by sub-optimal spindle formation and subsequent chromosomal NDJ (Eichenlaub-Ritter et al. 2007). Evidence in favor of this prediction is available in the mouse where environment-induced changes in ovarian hormones have been attributed to chromosomal asynapsis and subsequent aneuploid gamete formation (Susiarjo et al. 2007). More interestingly, decline in TL has also been correlated with altered pattern of recombination (Liu et al. 2004), the phenomenon that is strongly associated with NDJ of human chromosome 21 and has been evident in several studies (Oliver et al. 2008; Ghosh et al. 2009). It is probable that environmental aneugens accumulate gradually over the long time in the genome and manifest their effects only after the woman reach her late reproductive years when other natural cellular and genetic degradations have already started. This could explain why our cases and controls differ in their TL only at older ages. Thus, it is possible that the difference in TL among controls and cases begins at the chronological age from which maternal age-related risk of DS birth commences. Interestingly, our “genetic aging hypothesis” is consistent with very recent notion of an “oocyte mosaicism selection model” (Hulten et al. 2010). It is possible that rapid genetic aging might lead to improper operation of an ovarian selection system and subsequent ovulation of aneuploid oocyte.
Our result showing that MII mothers are “genetically older” at their advanced reproductive age than MI mothers is also intriguing, since it is well established that the MII mothers are chronologically older on average than MI mothers (Oliver et al. 2008; Ghosh et al. 2009). Putting these two facts together suggests that the increase in MII risk with age is related to “genetic aging”, but as discussed above there are many possibilities for exactly how genetic aging is linked to NDJ. Moreover, we are not certain whether there might be some critical values of TL that are distinctly associated with MI and MII NDJ and if so, how they are related to the mechanisms of types of errors.
In summary, we have successfully demonstrated a significant difference in telomere shortening with age among MI and MII nondisjoined cases and age-matched controls. Our work strongly suggests that the risk of DS birth in older women does have something to do with “genetic aging”, since we see a large difference not only between DS and non-DS mothers, but also between MI and MII. In contrast, for younger women, our work directly contradicts the “genetic aging” model, and is more consistent with a model in which DS birth in young women is a random stochastic event, perhaps related to unlucky placement of chiasma on meiotic chromosome or some other age-independent factors (Oliver et al. 2008; Ghosh et al. 2009). Our study represents new insight into the intriguing relationship between maternal age and aneuploid gamete formation and will provide a basis for future work to explicitly resolve the issue at molecular level.
References
Allen EG, Freeman SB, Druschel C, Hobbs CA, O’Leary LA, Romitti PA, Royle MH, Torfs CP, Sherman SL (2009) Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Hum Genet 125:41–52
Allshire RC, Dempster M, Hastie ND (1989) Human telomere contains at least three types of G-rich repeats distributed non-randomly. Nucleic Acids Res 17:4611–4627
Aviv A (2008) The epidemiology of human telomeres: faults and promises. J Gerontol A Biol Sci Med Sci 63:979–983
Aydos SE, Elhan AH, Tükün A (2005) Is telomere length one of the determinants of reproductive life span? Arch Gynecol Obstet 272:113–116
Batty GD, Wang Y, Brouilette SW, Shiels P, Packard C, Moore J, Samani NJ, Ford I (2009) Socioeconomic status and telomere length: the West of Scotland Coronary Prevention Study. J Epidemiol Community Health 63:839–841
Benetos A, Okuda K, Lajemi M, Kimura M, Thomas F, Skurnick J, Labat C, Bean K, Aviv A (2001) Telomere length as an indicator of biological aging: the gender effect and relation with pulse pressure and pulse wave velocity. Hypertension 37:381–385
Cawthon RM, Smith KR, O’Brien E, Sivatchenko A, Kerber RA (2003) Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 361:393–395
Chen JH, Hales CN, Ozanne SE (2007) DNA damage, cellular senescence and organismal ageing: causal or correlative? Nucleic Acids Res 35:7417–7428
Dorland M, van Montfrans JM, van Kooij RJ, Lambalk CB, te Velde ER (1998) Normal telomere lengths in young mothers of children with Down’s syndrome. Lancet 352:961–962
Eichenlaub-Ritter U, Winterscheidt U, Vogt E, Shen Y, Tinneberg HR, Sorensen R (2007) 2-Methoxyestradiol induces spindle aberrations, chromosome congression failure, and nondisjunction in mouse oocytes. Biol Reprod 76:784–793
Ghosh S, Feingold E, Dey SK (2009) Etiology of Down syndrome: evidence for consistent association among altered meiotic recombination, nondisjunction, and maternal age across populations. Am J Med Genet A 149A:1415–1420
Hanna CW, Bretherick KL, Gair JL, Fluker MR, Stephenson MD, Robinson WP (2009) Telomere length and reproductive aging. Hum Reprod 24:1206–1211
Hassold T, Chiu D (1985) Maternal age-specific rates of numerical chromosome abnormalities with special reference to trisomy. Hum Genet 70:11–17
Hawley RS, Frazier JA, Rasooly R (1994) Separation anxiety: the etiology of nondisjunction in flies and people. Hum Mol Genet 3:1521–1528
Hulten M, Patel S, Jonasson J, Iwarsson E (2010) On the origin of the maternal age effect in trisomy 21 Down syndrome: the Oocyte Mosaicism Selection (OMS) model. Reproduction 139:1–9
Jeffreys CA, Burrage PS, Bickel SE (2003) A model system for increased meiotic nondisjunction in older oocyte. Curr Biol 13:498–503
Keefe DL, Liu L (2009) Telomeres and reproductive aging. Reprod Fertil 21:10–14
Keefe DL, Liu L, Marquard K (2007) Telomeres and aging-related meiotic dysfunction in women. Cell Mol Life Sci 64:139–143
Kline J, Levin B (1992) Trisomy and age at menopause: predicted associations given a link with rate of oocyte atresia. Paediatr Perinat Epidemiol 6:225–239
Kline J, Kinney A, Levin B, Warburton D (2000) Trisomic pregnancy and earlier age at menopause. Am J Hum Genet 67:395–404
Kline J, Kinney A, Reuss ML, Kelly A, Levin B, Ferin M, Warburton D (2004) Trisomic pregnancy and the oocyte pool. Hum Reprod 19:1633–1643
Kline J, Kinney A, Kelly A, Reuss ML, Levin B (2005) Predictors of antral follicle count during the reproductive years. Hum Reprod 20:2179–2189
Liu L, Keefe DL (2002) Ageing-associated aberration in meiosis of oocytes from senescence-accelerated mice. Hum Reprod 17:2678–2685
Liu L, Franco S, Spyropoulos B, Moens PB, Blasco MA, Keefe DL (2004) Irregular telomeres impair meiotic synapsis and recombination in mice. Proc Natl Acad Sci USA 101:6496–6501
Martinez P, Siegl-Cachedenier I, Flores JM, Blasco MA (2009) MSH2 deficiency abolishes the anticancer and pro-aging activity of short telomeres. Aging Cell 8:2–17
Mendola P, Messer LC, Rappazzo K (2008) Science linking environmental contaminant exposures with fertility and reproductive health impacts in the adult female. Fertil Steril 89:e81–e94
Nasseri A, Mukherjee T, Grifo JA, Noyes N, Krey L, Copperman AB (1999) Elevated day 3 serum follicle stimulating hormone and/or estradiol may predict fetal aneuploidy. Fertil Steril 71:715–718
Njajou OT, Cawthon RM, Damcott CM, Wu SH, Ott S, Garant MJ, Blackburn EH, Mitchell BD, Shuldiner AR, Hsueh WC (2007) Telomere length is paternally inherited and is associated with parental lifespan. Proc Natl Acad Sci USA 104:12135–121359
Oliver TR, Feingold E, Yu K, Cheung V, Tinker S, Yadav-Shah M, Masse N, Sherman SL (2008) New insight into human nondisjunction of chromosome 21 in oocyte. PloS Genet 4(3):e1000033
Roberts R, Iatropoulou A, Ciantar D, Stark J, Becker DL, Franks S, Hardy K (2005) Follicle-stimulating hormone affects metaphase I chromosome alignment and increases aneuploidy in mouse oocytes matured in vitro. Biol Reprod 72:107–118
Sebastián C, Herrero C, Serra M, Lloberas J, Blasco MA, Celada A (2009) Telomere shortening and oxidative stress in aged macrophages results in impaired STAT5a phosphorylation. J Immunol 183:2356–2364
Sherman SL, Allen EG, Bean LH, Freeman SB (2007) Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev 13:221–227
Susiarjo M, Hassold TJ, Freeman E, Hunt PA (2007) Bisphenol A exposure in utero disrupts early oogenesis in the mouse. PLoS Genet 3:e5
Thum MY, Abdalla HI, Taylor D (2008) Relationship between women’s age and basal follicle-stimulating hormone levels with aneuploidy risk in vitro fertilization treatment. Fertil Steril 90:315–321
Van Blerkom J (2004) Mitochondria in human oogenesis and preimplantation embryogenesis: engines of metabolism, ionic regulation and developmental competence. Reproduction 128:269–280
van Montfrans JM, van Hooff MH, Martens F, Lambalk CB (2002) Basal FSH, estradiol and inhibin B concentrations in women with a previous Down’s syndrome affected pregnancy. Hum Reprod 17:44–47
Volarcik K, Sheean L, Goldfarb J, Woods L, Abdul-Karim FW, Hunt P (1998) The meiotic competence of in vitro matured human oocytes is influenced by donor age: evidence that folliculogenesis is compromised in the reproductively aged ovary. Hum Reprod 13:154–160
Warburton D (2005) Biological aging and the etiology of aneuploidy. Cytogenet Genome Res 111:266–272
Yoon PW, Freeman SB, Sherman SL, Taft LF, Gu Y, Pettay D, Flanders WD, Khoury MJ, Hassold TJ (1996) Advanced maternal age and the risk of Down syndrome characterized by meiotic stage of chromosomal error: a population-based study. Am J Hum Genet 58:628–633
Zwick ME, Cutler DJ, Langley CH (1999) Classic Weinstein: tetrad analysis, genetic variation and achiasmate segregation in Drosophila and humans. Genetics 152:1615–1629
Acknowledgments
We would like to thank the families participated in the study and the professionals who helped us in collection of blood samples. The project was funded by University Grants Commission (UGC), New Delhi, India; Sanctioned No. F-3-111/2001 (SR-II).
Conflict of interest statement
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghosh, S., Feingold, E., Chakraborty, S. et al. Telomere length is associated with types of chromosome 21 nondisjunction: a new insight into the maternal age effect on Down syndrome birth. Hum Genet 127, 403–409 (2010). https://doi.org/10.1007/s00439-009-0785-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-009-0785-8