Abstract
Milroy disease (hereditary lymphoedema type I, MIM 153100) is a congenital onset primary lymphoedema with autosomal dominant inheritance. Mutations in the gene, vascular endothelial growth factor receptor 3, VEGFR3 (FLT4), are known to cause Milroy disease, but there is uncertainty about the prevalence of VEGFR3 mutations in patients with primary lymphoedema and more specifically in those with a phenotype that resembles Milroy disease. This study aims to address this issue and thereby delineate the Milroy disease phenotype. Fifty-two patients with primary lymphoedema were analysed for mutations in the coding regions of VEGFR3. Patients were divided into four groups: Typical Milroy disease with family history (group I), typical Milroy disease with no family history (group II), atypical Milroy disease (group III), and complex primary lymphoedema (group IV). Results demonstrated that with rigorous phenotyping the likelihood of detecting VEGFR3 mutations is optimised. Mutation prevalence is 75% in typical Milroy patients with a family history (group I) and 68% if positive family history is not a diagnostic criterion. A positive family history is not essential in Milroy disease. The likelihood of detecting VEGFR3 mutations in patients who have a phenotype which is not typical of Milroy disease is very small (<5%). For the 22 mutation positive patients, 14 novel VEGFR3 mutations were identified, two of which were in exon 22 and one in exon 17, confirming that these exons should be included in VEGFR3 analysis. No mutations were found outside the kinase domains, showing that analysis of this part of the gene is not useful for Milroy disease patients. VEGFC, which encodes the ligand for VEGFR3, was sequenced in all patients with typical Milroy disease (groups I and II) and no mutations were identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary lymphoedema is swelling caused by a congenital abnormality of the lymphatic system. Milroy disease (hereditary lymphoedema type I, OMIM 153100) was first described in 1892. It is characterised by congenital onset of lower limb lymphoedema and is inherited in an autosomal dominant manner (Milroy 1892; Brice et al. 2005). The only gene locus to date is at 5q35.3 and the gene mutated at this position is FLT4, which codes for VEGFR3, Vascular Endothelial Growth Factor Receptor 3 (Ferrell et al. 1998; Evans et al. 1999; Irrthum et al. 2000; Karkkainen et al. 2000). This gene will be referred to in the remainder of the paper as VEGFR3. The prevalence of VEGFR3 mutations in primary lymphoedema patients, and specifically those with a phenotype resembling Milroy disease, has not been clarified. There has been a historical tendency to label all patients with non-syndromic congenital lymphoedema as having Milroy disease but in our experience Milroy disease has a more specific phenotype, for which the diagnosis should be reserved (Levinson et al. 2003; Smeltzer et al. 1985). Our aim was therefore to subdivide a group of primary lymphoedema patients according to their phenotype, and determine the prevalence of VEGFR3 mutations in each group.
The current evidence is that the mutant VEGFR3 receptor has no tyrosine kinase activity, but the effects are presumed not to be solely due to a loss of function, because of the preponderance of mis-sense mutations and the observation that the mutant protein is maintained at the cell surface for longer than the wild type (Karkkainen et al. 2000). The receptor is a dimer and there is less activity in the presence of a mutated and wild type allele than would be the case for haploinsufficiency alone, though heterodimers appear to have residual tyrosine kinase activity (Karkkainen et al. 2000). All mutations so far identified are in the kinase domains of VEGFR3 (coded by exons 17–26), but testing bias may have contributed to this finding, as only Evans et al. (2003) analysed the entire gene. Only nineteen mutations so far, have been reported worldwide (Ferrell et al. 1998; Irrthum et al. 2000; Karkkainen et al. 2000; Evans et al. 2003; Verstraeten et al. 2004; Ghalamkarpour et al. 2006; Carver et al. 2007; Butler et al. 2007). There is genetic heterogeneity in patients labelled as Milroy disease, though the degree of this is unclear (Ferrell et al. 1998; Evans et al. 2003; Witte et al. 1998; Holberg et al. 2001).
It was considered that a family history was required for a diagnosis of Milroy disease (Milroy 1892; Brice et al. 2005) but two recent papers have shown de novo mutations in the VEGFR3 gene in four patients with sporadic, congenital lymphoedema, (Ghalamkarpour et al. 2006; Carver et al. 2007).
Evans et al. (2003), reported VEGFR3 mutations in 10 out of 12 families with congenital onset and lower limb oedema. However, these families were all consistent with linkage to 5q35.3, so had been preselected as being more likely to have mutations in VEGFR3. Conversely, the studies of Witte et al. (1998) and Holberg et al. (2001) reported no mutations in VEGFR3 in patients with a more variable phenotype including oedema of genitalia, hands and feet, and variable age of onset.
The aims of this study are:
-
a.
Determine the prevalence of VEGFR3 mutations for the entire coding region in patients who clinically have Milroy disease, with and without a family history.
-
b.
Determine the prevalence of VEGFR3 mutations in patients with primary lymphoedema but who are not typical for Milroy Disease
-
c.
Report on 14 novel mutations
-
d.
Determine whether any patients described in (a) with no mutation in VEGFR3, have a mutation in its ligand, VEGFC, in view of the lymphatic phenotype reported in the Chy-3 mouse, which is Vegfc haploinsufficient (Dellinger et al. 2007).
Methods
Patient recruitment
Patients were seen in a Specialist Lymphoedema Clinic with Lymphoedema clinicians, therapists, clinical geneticists and nurse counsellors, and a family history and examination were undertaken. Patients not seen at St George’s Hospital were noted as such and clinical details obtained from the referring clinician. Patients were divided into four sub-groups in order that the prevalence of VEGFR3 mutations within each group could be determined. VEGFC was sequenced in all patients from groups I and II in whom no VEGFR3 mutation was found. The criteria for the four groups were developed by experienced clinicians in the field, based on recognised features of Milroy disease (Brice et al. 2005).
Patients fulfilling the criteria for one of the four following groups were included:
-
Group I: Typical Milroy disease with positive family history (bilateral or unilateral lower limb lymphoedema, that was present at birth).
-
Group II: Typical Milroy disease with negative family history.
-
Group III: Atypical Milroy disease [lower limb lymphoedema, unilateral or bilateral, but symptoms not noted at birth, (but onset age ≤ 5 years) or presence of other features not previously associated with Milroy disease].
-
Group IV: Complex primary lymphoedema (primary lymphoedema in which other body parts and not just lower limbs are affected by lymphoedema, syndromic or dysmorphic phenotype).
Typically, Milroy disease is characterised by lymphoedema mainly affecting the dorsum of the foot but which can extend to knee or thigh. The oedema has a ‘woody’ texture and large calibre veins are often noted. Small, upslanting, dysplastic nails and deep interphalangeal toe creases are characteristic as a result of in-utero oedema. Brice et al. (2005) reported that 37% of males with Milroy disease have hydroceles and this is therefore a well recognised associated feature of the condition. If abnormalities (other than hydroceles) were present, the patient was classified as ‘atypical’.
PCR and direct sequencing of VEGFR3 and VEGFC
This was carried out as described in Evans et al. (2003). All coding exons of VEGFR3 were examined. Genetic analysis of the sequencing products was carried out on an ABI 3100 Genetic Analyser. All sequences were run both forward and reverse. All novel mutations were checked in 200 control chromosomes from Caucasians, by sequencing or RFLP analysis. Primers for VEGFC were produced using Primer3 (Rozen and Skaletsky 2000) and sequences are available on request.
Results
In total there were 52 patients in this study. The overall VEGFR3 mutation detection rate in this series of patients was 42% (22/52). Of the 52 patients, 10 were outside referrals and were not examined at St George’s Hospital (SGH) and they were therefore assigned to a group based on clinical details provided by the referring clinician. The results are summarised in Tables 1, 2, 3, 4.
There are 24 patients in the typical Milroy disease group with a positive family history (group I, Table 1). A VEGFR3 mutation was identified in 18 out of 24 (75%) of this group. All 24 patients have at least one affected first degree relative in which vertical transmission of the condition has taken place, illustrating probable autosomal dominant transmission of the lymphoedema. Where possible, affected family members have been tested for the proband’s mutation, confirming co-segregation of disease with mutation. In one family with typical Milroy and positive family history (patient 18), the proband’s sister who also has the VEGFR3 mutation had resolution of the oedema at age two months. She is now six years old and has no oedema, indicating that signs of Milroy disease can resolve, having been present at birth. Such resolution has been reported before in Milroy disease (Brice et al. 2005; Ghalamkarpour et al. 2006). It is worth noting that it was possible to diagnose two patients (1 and 16) in utero given the pedal oedema seen on antenatal ultrasound scan and the positive family history.
In the typical Milroy disease with negative family history (group II), three out of seven patients (43%) were found to have de novo VEGFR3 mutations (reported in Carver et al. 2007). It can be concluded from these results that a positive family history of primary lymphoedema is not essential for the diagnosis of Milroy disease. Three patients without a mutation in VEGFR3 in Tables 1 and 2 were not heterozygous for SNPs in the coding or non coding regions of the gene. Thus a gene deletion could not be excluded in these three individuals.
In the atypical group (group III), only one patient had a VEGFR3 mutation. In this group, three patients (34, 36 and 37) were considered atypical because their lymphoedema was not present at birth and the lymphoscintigraphy results yielded a pattern of reflux within the lymphatics and this is deemed not to be characteristic of Milroy disease (Gordon and Mortimer 2007). None of these three patients were mutation positive on VEGFR3 sequencing. One of these three patients (36) was the only patient in the atypical group to have a positive family history. This patient has an affected brother but unaffected parents which could be consistent with a recessive inheritance pattern of primary lymphoedema, or dominant inheritance with non penetrance in the parent. In addition, he did not present until the age of five years and his lymphoscintigraphy demonstrated reflux.
The one patient in the atypical group with a VEGFR3 mutation had oedematous feet characteristic of Milroy disease, but also had additional problems—glaucoma (diagnosed age 7 years) and learning difficulties. He had no significant family history. Glaucoma and learning difficulties are not recognised associated features of Milroy disease, hence this patient’s atypical status. However, given his mutation positive result and characteristic lymphoedema it can be proposed that he has two separate aetiologies; Milroy disease and the cause of the glaucoma and learning problems. He has a normal male karyotype, is negative on testing for Fragile X syndrome, and has a normal brain MRI scan. His mutation is novel, but at the same residue as that reported in a Chinese patient with lymphoedema; namely D1055V (Yu et al. 2007).
In the complex primary lymphoedema group (group IV) there were no VEGFR3 mutations found. None of these patients clinically have Milroy disease. This group presented with lymphoedema in areas other than the lower limbs, with or without systemic involvement (e.g. pleural effusions, intestinal lymphangiectasia, ascites). For example, patient 51 is thought to have Aagenaes syndrome (OMIM 214900) given the lymphoedema and intrahepatic cholestasis. Patient 49 has lymphoedema, microcephaly and learning difficulties, and thus the diagnosis of Microcephaly-lymphoedema-chorioretinopathy syndrome (OMIM 152950) is being considered. Patient 46 has systemic involvement of the lymphatics with pleural effusions and ascites. A diagnosis of a generalised lymphatic dysplasia would be appropriate in this case, given the phenotype, and a positive family history (affected sister, unaffected parents) infers that autosomal recessive inheritance is a possibility, or dominant inheritance with non penetrance.
This study adds extensively to the number of mutations in VEGFR3 that appear to be pathogenic for Milroy disease, as fourteen of those reported here are novel, and only nineteen have been previously reported in the literature. The mutations in this report, including those reported by Carver et al. (2007) were in exons 17 (1), 18 (4), 19 (1), 20 (2), 22 (3, of which 2 are recurrent), 23 (8, of which 2 are recurrent), 24 (1) and 25 (2). Three different codons were altered in exon 18, while in exon 23 two mutations affected codon 1037, two were in codon 1041, and one in codon 1042. As previously noted, these amino acids are part of a conserved domain in tyrosine kinase receptors, where changes produce inactivation (Evans et al. 2003; Hanks and Hunter 1995). This is clearly a hot spot for mutations that can produce Milroy disease.
Two mutations, G1024Q (found twice) and G1024R, are novel mutations reported in exon 22, and are absent in 200 control chromosomes (as were all novel mutations presented). Only one mutation in exon 22 has been documented in the literature (Butler et al. 2007). Although there is no functional data for these changes, the same codon in exon 22 was affected in these three unrelated cases. We also found an amino acid change in exon 17, where none have previously been reported. The R844P mutation in exon 17 was found in patient 1 and his daughter, both of whom were affected with lymphoedema characteristic of Milroy disease. The likelihood is that these changes in exons 22 and 17 are pathogenic. All the residues affected are conserved across species. V1051, D1055 and Y1115 are shown in the diagram in Ghalamkarpour et al. 2006. BLAST search for the remaining novel mutations shows that they are conserved in VEGFR3 from chimpanzee, rat, mouse, dog, cat, chicken, quail and zebra fish.
Analysis of the non-kinase domains of VEGFR3 showed 6 previously reported SNPs (synonymous unless indicated); 445A>G/N149D (rs34221241), 507G>T/(rs3736061), 1344C>T (rs3736062, 1480A>G/T494A (rs307826, 1580A>G/S527N (rs35874891), 3971G>T/R1324L (rs307821). We also found 3 SNPs not in the databases; 1133G>A/R378H (patient 49 Table 4) 3860T>C/I1287T (patient 45 Table 4) and 3962G>A/R1321Q (patients 29 Table 2 and patient 20 Table 1). The first SNP, R378H, could not be ruled out as a pathogenic mutation as it was not found in 180 control DNAs, but it was considered more probable that it is a rare polymorphism. The child had a severe phenotype but the mother, who also has the SNP, is unaffected. This amino acid is conserved in VEGFR3 of man, chimpanzee, mouse and rat, but replaced by lysine in zebrafish and chicken. The change to histidine is very conservative and not dissimilar to the substitution of lysine in that position, and this, combined with the unaffected mother having the base change and the lack of cross species conservation, makes non pathogenesis more probable than non penetrance in the mother. However, this cannot be ruled out.
The second of these SNPs, I1287T, was not identified in 100 sequenced control DNAs, but was absent in the affected brother of the proband, the affected father, and the unaffected mother and sister. This de novo base change is therefore clearly not disease causing. The third SNP, R1321Q, was found in three of 50 control DNAs.
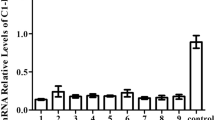
The patients in groups I and II who had no mutation in VEGFR3 (10 individuals) were also investigated for possible mutations in the coding region of the gene for VEGFC, the ligand for VEGFR3. No mutations were identified. Since sequence analysis would not reveal a gene deletion, and samples were not available for FISH analysis, we examined eleven informative SNPs from the databases. Six of the ten patients were heterozygous for these SNPs, showing that gene deletions had not occurred in these individuals. A deletion could not be ruled out in the others.
Discussion
A diagnosis of Milroy disease can be made in patients with congenital lower limb oedema but other factors need to be taken into account. Typical features of Milroy lymphoedema include a brawny texture of oedema on the dorsum of the feet, usually, but not necessarily, bilateral and present at birth, with upturned toe nails and large calibre veins in the feet. A positive family history, with or without a VEGRF3 mutation, with these clinical symptoms would indicate this diagnosis. Lymphoscintigraphy in these patients demonstrates apparent aplasia of the lymphatics in the affected limb(s) and can be a worthwhile tool in helping to make the diagnosis (Gordon and Mortimer 2007). Dysmorphic facial features are not a feature of this group.
The overall mutation detection rate in this series of patients was 42% (22/53). However, with rigorous phenotyping this figure can be improved to 75% if positive family history is a necessary inclusion or 68% if it is not. A positive family history is not considered to be essential for a diagnosis of Milroy disease as there are known de novo mutations in VEGFR3 (Ghalamkarpour et al. 2006; Carver et al. 2007), and it is also possible that a non-penetrant mutation could be present in one of the parents when an apparently isolated case is examined, as penetrance is known to be about 90% (Brice et al. 2005). Butler et al. (2007) reported that the genetic basis of most cases of Milroy disease has not been established but our results indicate that if Milroy disease is diagnosed according to specific phenotype guidelines as described above, the likelihood of the genetic basis being a VEGFR3 mutation is at least 68%.
The lack of a mutation in VEGFR3 does not exclude the diagnosis of Milroy disease, as there must be other, yet to be idenitified, genetic mechanisms that can produce features consistent with a Milroy disease phenotype. However, mutations in VEGFR3 are extremely unlikely in other forms of primary lymphoedema, for example when lymphoedema is not confined to lower limbs or if it is unilateral and not present at birth. This is consistent with the the findings of Witte et al. (1998) and Holberg et al. (2001) who reported no mutations in VEGFR3 in patients with a more variable phenotype.
The findings of mutations in exons 17 and 22 bring into question the proposal from a recent paper by Ghalamkarpour et al. (2006) that suggests exclusion of exons 17 and 22 in molecular diagnosis of Milroy disease. Based on the mutations reported here, and those in the literature, it appears a sound approach is to analyse exons 18, 19, 20 and 23 initially, and if these are negative examine the remainder of the exons that code for the kinase domains (17–26).
The absence of any mutations in VEGFC in those typical Milroy cases where there is no VEGFR3 mutation, indicates that changes in this ligand for the receptor are not a common cause of this phenotype. We were unable to conduct FISH on these patients but SNP analysis for VEGFC showed seven of the ten patients to be heterozygous. Although we could not rule out entire gene deletions in the other three cases, this is unlikely considering the findings in the other seven patients. The fact that no mutations were found outside the kinase domains of VEGFR3 also suggests that lack of ligand binding to the receptor is not a probable cause of Milroy disease in humans, and the absence of any mutations in VEGFC supports this. Sequence analysis of VEGFC was not performed in the patients with a more complex phenotype, as the lymphoedema in the Chy-3 mouse is very similar to that seen in the mouse with a VEGFR3 mutation.
This study also highlights the continuing difficulty in gene analysis in establishing whether a base change is causative for a disease. This is shown both by the previously unknown SNPs identified in the non-kinase domains of VEGFR3, and by the appearance in trans of P1008L in patient 6 Table 1. We have not found this in 150 control individuals, yet it has been identified in the family with lymphoedema here, and by us previously (Evans et al. 2003). In both cases it has been in trans and did not track with affected status, so could be proved not to be causative. Had this change been consistent with linkage, it would have appeared a very good candidate for a pathological mutation. Two of the novel SNPs in the non kinase domains of VEGFR3 both initially appeared good candidates for mutations as we could not identify them in control DNAs. I1287T was de novo in the proband. There were 3 other affected family members, including the father, who did not have this change, so it could be definitely shown to be non pathogenic. Had the de novo SNP been in an isolated case, it would have been tempting indeed to assume causality. The other SNP, R378H, cannot be definitively ruled out as a causative mutation. However, the fact that it is a conservative change, is not conserved across species, and is absent in the clinically normal mother, makes non-pathogenicity more probable.
This study provides evidence to support guidelines as to when VEGFR3 mutation analysis in primary lymphoedema patients is most appropriate. Patients with congenital lower limb oedema with or without a family history of lymphoedema should be tested. It is highly unlikely that patients with other forms of primary lymphoedema (i.e. other features not associated with Milroy disease and/or more widespread lymphoedema) have Milroy disease and therefore other diagnoses should be considered in the first instance. Analysis of non kinase domains is not indicated for any primary lymphoedemas.
References
Brice G, Child AH, Evans A, Bell R, Mansour S, Burnand K, Sarfarazi M, Jeffery S, Mortimer P (2005) Milroy disease and the VEGFR3 mutation phenotype. J Med Genet 42:98–102
Butler MG, Dagenais SL, Rockson SG, Glover TW (2007) A novel VEGFR3 mutation causes Milroy disease. Am J Med Genet A 143:1212–1217
Carver C, Brice G, Mansour S, Ostergaard P, Mortimer P, Jeffery S (2007) Lymphodema Consortium. Three children with Milroy disease and de novo mutations in VEGFR3. Clin Genet 71:187–189
Dellinger MT, Hunter RJ, Bernas MJ, Witte MH, Erickson RP (2007) Chy-3 mice are Vegfc haploinsufficient and exhibit defective dermal superficial to deep lymphatic transition and dermal lymphatic hypoplasia. Dev Dyn 236:2346–2355
Evans AL, Brice G, Sotirova V, Mortimer P, Beninson J, Burnand K, Rosbotham J, Child A, Sarfarazi M (1999) Mapping of primary congenital lymphedema to the 5q35.3 region. Am J Hum Genet 64:547–555
Evans AL, Bell R, Brice G, Comeglio P, Lipede C, Jeffery S, Mortimer P, Sarfarazi M, Child AH (2003) Identification of eight novel VEGFR3 mutations in families with primary congenital lymphoedema. J Med Genet 40:697–703
Ferrell RE, Levinson KL, Esman JH, Kimak MA, Lawrence EC, Barmada MM, Finegold DN (1998) Hereditary lymphedema: evidence for linkage and genetic heterogeneity. Hum Mol Genet 7:2073–2078
Ghalamkarpour A, Morlot S, Raas-Rothschild A, Utkus A, Mulliken JB, Boon LM, Vikkula M (2006) Hereditary lymphedema type I associated with VEGFR3 mutation: the first de novo case and atypical presentations. Clin Genet 70:330–335
Gordon K, Mortimer PSM (2007) A guide to lymphoedema. Expert Rev Dermatol 2:741–752
Hanks SK, Hunter T (1995) Protein kinases 6. The eukaryotic protein kinase superfamily: kinase (catalytic) domain structure and classification. FASEB J 9:576–596
Holberg CJ, Erickson RP, Bernas MJ, Witte MH, Fultz KE, Andrade M, Witte CL (2001) Segregation analyses and a genome-wide linkage search confirm genetic heterogeneity and suggest oligogenic inheritance in some Milroy congenital primary lymphedema families. Am J Med Genet 98:303–312
Irrthum A, Karkkainen MJ, Devriendt K, Alitalo K, Vikkula M (2000) Congenital hereditary lymphedema caused by a mutation that inactivates VEGFR3 tyrosine kinase. Am J Hum Genet 67:295–301
Karkkainen M, Ferrell R, Lawrence E, Kimak M, Levinson K, Mcligue M, Alitalo K, Finegold D (2000) Missense mutations interfere with VEGFR3 signalling in primary lymphoedema. Nat Genet 25:153–159
Levinson KL, Feingold E, Ferrell RE, Glover TW, Traboulsi EI, Finegold DN (2003) Age of onset in hereditary lymphedema. J Pediatr 142:704–708
Milroy WF (1892) An undescribed variety of hereditary oedema. NY Med J 56:503
Rozen S, Skaletsky HJ (2000) Primer3 on the www for general users and for biologist programmers. In: Krawetz S, Misener S (eds) Bioinformatics methods and protocols: methods in molecular biology. Humana Press, Totowa, pp 365–386
Smeltzer DM, Gunnar B, Stickler GB, Schirger A (1985) Primary lymphoedema in children and adolescents: A follow-up study and review. Paediatrics 76:206–218
Verstraeten VLRM, van Steensel MAM, Veraart JCJM, Bladergroen RS, Steijlen PM, van Geel M (2004) A compound heterozygous mutation in VEGFR3 does not cause a more severe form of Nonne-Milroy Lymphedema. J Invest Dermatol 123:A77
Witte MH, Erickson R, Bernas M, Andrade M, Reiser F, Conlon W, Hoyme HE, Witte CL (1998) Phenotypic and genotypic heterogeneity in familial Milroy lymphedema. Lymphology 31:145–155
Yu Z, Wang J, Peng S, Dong B, Li Y (2007) Identification of a novel VEGFR3 missense mutation in a Chinese family with hereditary lymphedema type 1. J Genet Genomics 34:861–867
Acknowledgments
F. C. Connell and C. Carver were supported by the British heart Foundation (BHF). P. Ostergaard was supported by the Daphne Jackson Trust and now the British Skin Foundation (BSF). We would like to thank the Reece Spence Fund for their support. The research used the resources of the Biomics Unit at St George’s University of London. Members of the Lymphoedema Consortium not in the author list were: Kevin Burnand, Russell Mellor, Alberto Smith, Mansoor Sarfarazi, David Goudie, Jill Clayton-Smith, Sarjhu Mehta, Ruth Newbury Ecob, Sarah Smithson, Fancesca Forzano, Beatrice Vesti, Andrea Guala, Cesare Danesino, Anne Child.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
F. C. Connell and P. Ostergaard contributed equally to this work.
An erratum to this article can be found at http://dx.doi.org/10.1007/s00439-009-0633-x
Rights and permissions
About this article
Cite this article
Connell, F.C., Ostergaard, P., Carver, C. et al. Analysis of the coding regions of VEGFR3 and VEGFC in Milroy disease and other primary lymphoedemas. Hum Genet 124, 625–631 (2009). https://doi.org/10.1007/s00439-008-0586-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-008-0586-5