Abstract
Interleukin-1β (IL-1β) activates inflammatory mediator cascades and has been implicated in the pathogenesis of several diseases. Single nucleotide polymorphisms (SNPs) of the IL1B promoter have been associated with various inflammatory diseases. We recently reported that IL1B gene transcription was influenced by four promoter SNPs, and that individual SNP function in vitro was governed by haplotype context. In the present study we tested the in vivo relevance of this observation by comparing IL1B promoter haplotype-pairs with IL-1β protein levels in 900 gingival tissue fluid samples. Three SNPs (−511, −1464, −3737) defined four IL1B promoter haplotypes that occurred in the study population and could be assigned unambiguously to each chromosome. The four haplotypes defined ten haplotype-pairs of which four pairs, representing 57% of the population, were associated with 28–52% higher IL-1β protein levels in vivo. Two of these pairs, characterized by homozygosity for the common allele at −3737, were also associated with raised serum levels of C-reactive protein (p = 0.02). We validated these findings in stimulated peripheral blood mononuclear cells (PBMCs) from a separate population (N = 70). PBMCs with IL1B haplotype-pairs associated with higher in vivo levels of IL-1β produced 86–287% more IL-1β in vitro than the reference group. We believe that this is the first demonstration of a relationship between in vivo levels of an inflammatory mediator and gene promoter haplotypes on both chromosomes. These findings may apply to other inducible genes and could provide a logical framework for exploring disease risk related to genetic variability in pathogenic mediators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathological inflammation underlies many of the chronic diseases of aging (Hansson and Libby 2006; Kornman 2006; McGeer et al. 2006; Shoelson et al. 2006). In overtly healthy populations there is evidence of variation in the level of systemic inflammation as measured by circulating biomarkers, including C-reactive protein (CRP). Some individuals have consistently higher levels of inflammatory markers (Woloshin and Schwartz 2005) and seem to be at increased risk for conditions such as cardiovascular disease, dementia and metabolic disease, when compared with individuals with lower levels (Bo et al. 2005; Kardys et al. 2006; Ridker 2003; Ridker et al. 2005, 1998a, b; Schmidt et al. 2002). Smoking, low-grade chronic infections and body mass index can account for some of the variance in inflammatory biomarker levels in overtly healthy populations. Genetic variation also appears to be a determinant of inter-individual differences in the inflammatory response (Berger et al. 2002; Curran et al. 2005; Kahraman et al. 2006), but the data are inconsistent (Capri et al. 2006; Kozlowski et al. 2006).
Polypeptide cytokines such as IL-1β and tumor necrosis factor α (TNFα) are produced by macrophages in response to pro-inflammatory stimuli and, acting through cognate receptors on many cell types, initiate a self-amplifying cascade of mediators that form a large component of the acute and chronic inflammatory responses. These cytokines are inducible at transcriptional level, and since their gene promoters are polymorphic, it has been postulated that they may contribute to the genetic basis of stable inter-individual differences in inflammatory responsiveness.
Genetic variation in the IL-1 gene cluster has been extensively characterized in several ethnic groups and has been associated with clinical phenotypes including in vivo levels of inflammatory biomarkers and clinical outcomes of inflammatory diseases (Camargo et al. 2006; El-Omar et al. 2000; Engels et al. 2007; Iacoviello et al. 2005; Kornman 2006; Vilaichone et al. 2005). Reports of these associations, however, have not been consistent in terms of specific genetic sequence differences and clinical phenotypes.
We considered that one reason for inconsistent genotype–phenotype association in different studies may be that the SNPs available as genetic markers in these studies were not sufficiently well-characterized in terms of haplotype, haplotype interactions, and functional significance in gene regulation.
To test this in the specific case of IL-1β, which has no recorded variations at protein level, we first mapped all of the SNPs in the IL1B gene, determined the extent of linkage disequilibrium across the chromosomal region (2q13-14) and defined the common haplotypes that existed in different ethnic populations. We then studied IL1B gene promoter function in reporter assays and found that several SNPs of the promoter-enhancer region could affect in vitro transcription and transcription factor binding according to which allele was present upstream of the reporter gene. Furthermore, in these studies we found that the effect of an individual SNP on transcriptional activity was highly dependent on the alleles of other SNPs that were present in the construct, to the extent that an individual SNP could have a positive or negative effect in different haplotype contexts. Moreover, the allelic patterns of these functional SNP combinations corresponded with common haplotypes of the IL1B promoter found in the population (Chen et al. 2006).
A further consideration, however, is that in diploid cells we have very limited knowledge on whether genes of interest are equally active on both chromosomes. This becomes an important consideration in gene association studies based on the hypothesis that the gene makes a biological contribution to the phenotype in question.
In the present study, with an IL-1 system that allows unambiguous assignment of haplotypes, we could define the functional promoter region haplotypes on each of the chromosomes. We found that functional haplotype-pairs were significantly associated with increased in vivo levels of IL-1β in gingival tissue fluid samples from 900 donors. IL1B haplotype-pairs were also tested in relation to IL-1β production by stimulated peripheral blood mononuclear cells from a separate population of 70 healthy donors. The same haplotype-pairs that were associated with higher in vivo levels of IL-1β were also associated with higher levels of IL-1β production in vitro.
The results show that the use of haplotypes on both chromosomes, as compared with a single chromosomal haplotype, provides valuable information concerning genotype/phenotype relationships. In certain situations, it appears that analysis of a single chromosomal haplotype may lead to incorrect conclusions, and could be misleading in terms of disease association studies.
Materials and methods
The in vivo study sample was selected from the Atherosclerosis Risk in Communities study (ARIC), a prospective investigation of atherosclerosis and its clinical sequelae. The ARIC population-based cohort contains 15,792 subjects aged 45–65 years, selected by probability sampling from four communities: Forsyth County, NC; Jackson, MS; Northwestern suburbs of Minneapolis, MN; and Washington County, MD. A detailed description of the ARIC study design and methods is published elsewhere (The ARIC Investigators, 1989).
As part of an ancillary study of periodontal disease, a subset of the original ARIC population underwent dental examinations and a further subset was selected for IL1 genotyping. Participants enrolled in the study provided informed consent to the protocol that was reviewed and approved by the Institutional Review Board on Research Involving Human Subjects at the University of North Carolina. Our study sample comprises the 900 Caucasians from ARIC with both dental examinations and IL1 genotypes. More extensive description of the periodontal status of this population, including the level of disease and microbial load, has been recently reported (Offenbacher et al. 2007).
IL-1β levels were assessed from samples of gingival tissue fluid. Since the gingival crevice epithelium is in constant contact with a microbial biofilm, the level of IL-1β within the gingival tissue fluid represents a serum transudate that is enriched by the local evoked gingival tissue response that has reached a steady state. Gingival tissue fluid was collected as described in detail previously (Champagne et al. 2003). Briefly, four paper strips were eluted and analyzed separately (from the mesio-lingual of each first molar) from each subject and pooled to provide a patient mean value in ng/ml. IL-1β concentrations were measured on the collection strip, using Enzyme-Linked Immunoadsorbent Assays (ELISA, Caymen Chemical Ann Arbor, MI).
C-reactive protein in serum was measured with a high sensitivity assay. Fasting blood samples were taken from all subjects and serum was frozen for subsequent analysis as previously described (Papp et al. 1989). Serum CRP concentrations were measured by latex-enhanced nephelometry (High Sensitivity CRP assay) on a BNII nephelometer (Dade Behring, Deerfield, IL). The BN II high sensitivity CRP assay utilizes a monoclonal antibody attached to polystyrene particles and fixed-time kinetic nephelometric measurements. This fully automated system creates a seven point standard curve from 0.4975 μg/ml (1:40 dilution of Rh Standard SL) to 0.0078 μg/ml (1:2,560 dilution). The BN II makes a 1:400 dilution to measure sample CRP concentrations between 3.5 and 210 mg/l and a 1:20 dilution below 3.5 mg/l. This is an FDA, CLIA-complaint assay. Individuals with values above or below the limits of detection were excluded from analysis.
Since the GCF volume and protein composition is influenced by the local tissue inflammation, two periodontal endpoints were included in the study as covariates. One endpoint was the assessment of the percent of pocket depths of 4 or more millimeters. The second variable is composite measure of periodontal disease composed of pocket depth, bleeding on probing and interproximal attachment level of 3 mm or more measured on a 6-point ordinal scale. This composite measure is a more detailed version of an index developed to assess the inflammatory status of the periodontal tissue-biofilm interface (Offenbacher et al. 2005).
Blood samples were collected in ethylenediaminetetraacetic acid (EDTA)-containing tubes and DNA was extracted for genotyping in the Division of Genomic Medicine, University of Sheffield, Sheffield, UK. Blood used for plasma factors was centrifuged and frozen at −70° until analyzed. All genetic and blood analyses were performed by individuals unaware of other data.
Single nucleotide polymorphisms (SNPs) were tested at three locations within the IL1B promoter, IL1B(−511) (C > T transition), IL1B(−1464) (G > C transition), and IL1B(−3737) (C > T transition). Two additional SNPs, IL1A(+4845) (G > T transition) and IL1B(+3954) (C > T transition), were also genotyped to facilitate comparisons with other studies. The first nucleotide designated for each sequence variation is the common allele in Caucasians (e.g. −511C), while the second nucleotide (e.g. −511T) is the less common allele in Caucasians. Genotyping was performed by Taqman™ 5′ nuclease assay, as previously described (di Giovine et al. 2000).
We used HAPLO.SCORE (Schaid et al. 2002) to identify haplotype frequencies with non-negligible frequencies (>0.5%). Next, we formed each possible pair of haplotypes drawn from this set and determined whether the resulting haplotype-pair groups could be recreated unambiguously from phase unknown genotypes of the individual SNPs.
We tested the overall null hypothesis of equal mean IL-1β levels across all haplotype-pair groups using analysis of variance (ANOVA) with degrees of freedom equal to the total number of groups minus one.
To identify specific haplotype groups associated with high IL-1β levels, we compared mean levels of IL-1β between each pair of haplotype groups. Next, we calculated nominal p-values for each comparison and ranked the pairs from most to least significant. Finally, we searched for patterns of haplotypes clustering among the most significant pairs.
We used linear regression to estimate the magnitude of difference in IL-1β for different haplotype-pair groups. Ordinary least squares regression was employed using the software package Splus®. Dependent variables were first log-transformed. The independent variables, other than IL-1 genotypes, were smoking status, diabetes status, body mass index, and degree of periodontal disease. To do so, we identified the set of non-genetic covariates that associate with IL-1β. Then, with these covariates in the model, indicator variables for the haplotype-pair groups were added. A similar approach was taken for CRP analysis except 1-sided p-values were calculated to reflect an a priori expectation of the direction of the effect based on the IL-1β results. IL-1β and CRP values were log-transformed prior to statistical analysis because of skewness in the distribution of both parameters.
P-values are used in three distinct ways in this report. First, for the overall test of equal mean IL-1β levels, they are used in the traditional hypothesis testing sense. That is, the p-value will reflect the proportion of times we would expect a statistic as large as or larger than the one observed if the null hypothesis were true. Second, p-values are used as a device for ranking all pair-wise comparisons of haplotype pair groups. This allows us to search for patterns of haplotypes that underlie any overall significant differences. Finally, once haplotype pair groups are identified (hopefully with a discernable pattern of constituent haplotypes), p-values will be calculated for the aggregate risk group compared to all other groups. These p-values do not take into account the multiple comparison issue inherent in such a grouping procedure. However, they will offer a heuristic measure of the potential strength of the association. At this stage of analysis, the importance of the gene will have already been established with a statistically valid test and the remaining task is one of identifying the important variants using a combination of statistical inference and possibly pattern recognition.
Effect of IL1B haplotype-pairs on IL-1β release by peripheral blood mononuclear cells (PBMCs) was determined in healthy volunteers, using methods described previously (Iacoviello et al. 2005). PBMCs were obtained from 75 healthy volunteers, of which complete data were available for 70. No subject had received medication or experienced allergic disease or infections within a period of 2 weeks before blood sampling. Freshly drawn whole blood was processed as described previously (Napoleone et al. 2000). The final mononuclear cell preparation was incubated with LPS (0.1 mcg/ml; from Escherichia coli 055:B5; Sigma-Aldrich, St Louis, MO, USA) for 24 h. The concentration of LPS and incubation time were chosen on the basis of preliminary time-course and dose-response experiments which showed an optimal release of IL-1β in the experimental conditions used. Cells were spun down and IL-1β was measured in the supernatants using a high-sensitivity ELISA (Amersham Pharmacia Biotech). Experiments were performed in duplicate by operators who were unaware of sample identity and the genotype of the donor.
Results
Haplotypes
Demographic characteristics of the 900 Caucasian study participants are presented in Table 1.
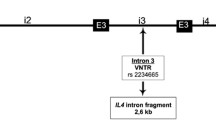
We have previously reported that the gene for IL-1β (IL1B gene) has four functionally active SNPs in the promoter-enhancer region and one synonymous exonic SNP (Chen et al. 2006), as shown in Fig. 1. In several ethnic groups studied, two of the functional SNPs, IL1B(−31) and IL1B(−511) are perfectly concordant (El-Omar et al. 2000; Lee et al. 2004; Muraki et al. 2004); therefore we used the three SNPs shown in Table 2 to characterize the functionally important IL1B genetic variation. Analysis of the haplotypes in the 900 subject Caucasian population indicated that of the eight potential three-SNP haplotypes only four haplotypes were detected, which we have denoted B1, B2, B3, and B4 (Table 2).
General structure of the Human gene for IL-1β. The functional single nucleotide polymorphisms (SNP) in the enhancer-promoter region of the gene for IL-1β are IL1B(−31), IL1B(−511), IL1B(−1464) and IL1B(−3737). They are shown above together with IL1B(+3954), a commonly studied synonymous SNP in exon 5
Based on all possible combinations of the four haplotypes, there are ten genotype patterns for the IL1B promoter (Table 3). Because each of the ten is unique, haplotypes can be assigned unambiguously for any individual. All of the ten possible composite genotype patterns were observed in the study population, but only three individuals (<1%) were homozygous for the B4/B4 haplotype-pair. In addition, we point out that IL1B(−511) and IL1B(−1464) largely convey the same information in this population of Caucasians, as they are concordant in all haplotypes except for the least common, B4.
Haplotype association with IL-1β protein level in vivo
To correlate genotypes with IL-1β levels, we first tested the null hypothesis that the mean in vivo IL-1β protein levels (log IL-1β) were equal across the ten haplotype-pairs shown in Table 3. The null hypothesis was rejected (ANOVA; 9 degrees of freedom; p = 0.005), indicating that there were significantly different IL-1β levels based on haplotype-pairs. Exclusion of the small B4/B4 group did not affect this conclusion (p = 0.003).
Having established an overall difference in mean log IL-1β across haplotype-pair groups, we turned our attention to the identification of specific haplotype-pairs associated with elevated IL-1β levels. To do this, we compared each haplotype-pair against every other pair, producing 45 comparisons; ranked all comparisons by nominal p-value; and identified comparisons in the top tertile, i.e. the 15 comparisons that have the most significant p-values (Table 4). From this evaluation, we found haplotype-pairs to partition very nicely into two groups. The first group comprised any combination of B1 and/or B3 haplotypes (shown in bold in Table 4). The second group (shown in italic in Table 4) included individuals with one copy of B3 and one copy of either of the two haplotypes, B2 or B4, that share allele T at IL1B(−511).
Of the 15 most significant haplotype-pair comparisons, the first group, individuals with any combination of B1 and/or B3 haplotypes (i.e. B1/B1, B3/B3, B1/B3), occurred as the “high IL-1β” haplotype-pair 11 of 15 times. In the top tertile, there were no comparisons in which pairs of B1 and B3 haplotypes were the “low IL-1β” haplotype-pair The second group included individuals with one copy of B3 and one copy of either B2 or B4, and occurred in the remaining 4 of 15 comparisons as the “high IL-1β” haplotype-pair and was the “low IL-1β” haplotype-pair only when compared with the haplotype-pairs in the first group. Linear regression revealed that, relative to all other possible haplotype pairs (42.6% frequency), the first group (42.7% frequency) had a 33% increased level of IL-1β (p < .0001) and the second group (14.8% frequency) had a 28% increased IL-1β level (p < .01).
The magnitude of difference between the haplotype pairs is evident when we compare the geometric means of IL-1β levels for the most common “high” pairs in the top tertile, B3/B3 (180.6 ng/ml) and B1/B1 (163.3 ng/ml) to the most common “low” pairs in that tertile, B2/B2 (122.2 ng/ml) and B1/B2 (117.9 ng/ml) (Table 5).
Since the in vivo IL-1β levels were assessed in gingival tissue fluid, a serum transudate that also reflects the severity of local periodontal tissue inflammation (Armitage 2004; Ebersole et al. 1993; Graves and Cochran 2003; Orozco et al. 2006), the analysis included adjustment for two periodontal disease severity endpoints available in this database. Other covariates included smoking status, diabetes status, and body mass index. With the two periodontal endpoints included in the model, no other covariates except for IL-1 genotypes were significant predictors of the in vivo IL-1β levels. An assumption of model linearity was not critical, since all parameters in the final model were categorical variables.
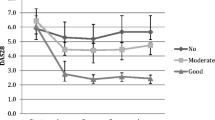
Haplotype association with serum CRP
The first group of IL-1β over-expressing haplotype-pairs (B3/B3; B1/B3; B1/B1) translates more simply into carriage of C/C at IL1B(−511). Equivalently, the second group (B2/B3; B4/B3) includes those who are both C/T at IL1B(−511) and C/C at IL1B(−3737). Because the group comprising individuals with C/C at IL1B(−511) is relatively large (>40% of this study population), we repeated our regression analysis splitting the group into its three haplotype-pair groups: B3/B3, B1/B3, and B1/B1. Each of these components, as well as the B2/B3 + B4/B3 group was significantly higher in IL-1β levels than the reference group (i.e. individuals who were not B3/B3, B1/B3, B1/B1, B2/B3 or B4/B3) (Fig. 2). Interestingly, only two of these four groups were associated with increased serum CRP, namely B3/B3 and B2/B3 + B4/B3 (Fig. 2). The two groups associated with higher CRP levels are distinguished from the other pro-inflammatory patterns by homozygosity for the common allele (C/C) at IL1B(−3737). The combined B3/B3 and B2/B3 + B4/B3 group had 33% higher CRP values when compared with all others (p = .007) after adjustment for BMI, smoking, and gender.
Percent increase of IL-1β and C-reactive protein for pro-inflammatory IL1B haplotype pairs relative to all others. The IL-1β protein level or C-reactive protein (CRP) level for the indicated IL1B promoter haplotype pair (e.g. B3/B3) is shown as the percentage increase, and 95% confidence interval bars, in the mean level of IL-1β or CRP relative to the reference group. The reference group for the IL-1β levels includes all of the subjects with genotypes other than the four pro-inflammatory haplotype pairs shown in the figure. Because CRP levels for B1/B3 and B1/B1 are indistinguishable from those with haplotype pairs associated with low IL-1β, B1/B3 and B1/B1 are considered as part of the reference group for CRP analysis. The genotypes at IL1B(−511) and IL1B(−3737) that constitute each haplotype pair are shown below the haplotype pair. N = 900 Caucasians. ***p < 0.001; **p < 0.01; *p < 0.02
Testing for ‘gene dose’ effect
Two of the commonly occurring pairs, B1/B1 (22% frequency) and B1/B3 (17% frequency), associated with higher levels of IL-1β (Table 4) included the B1 haplotype. In a haplotype analysis for dose effect of B1 haplotype relative to IL-1β levels, i.e. comparison of 0 copies, 1 copy, and 2 copies, the association was not significant (p = 0.114). This appears to be due to the fact that the other commonly occurring B1 pair, B1/B2 (25% frequency), is a low producer of IL-1β in this study, so the single copy of B1 in Caucasians will be found predominantly in both a B1/B3 over-producing pair and a B1/B2 under-producing pair. This will tend to favor a lower level of IL-1β if the B1 single haplotype is assessed out of diploid context, yet the B1/B1 pair is clearly associated with higher levels of IL-1β.
Comparison with other IL-1 region SNPs associated with inflammatory response
Three additional SNPs in the IL-1 gene cluster, IL-1A(+4845), or the concordant allele at IL-1A(−889), and IL1B(−3954) have been associated in the literature with differential expression of inflammatory mediators and clinical phenotypes (Adjers et al. 2004; Berger et al. 2002; Brett et al. 2005; Florez et al. 2006; Haggerty et al. 2005; Kornman 2006; Rainero et al. 2004; Seripa et al. 2005), with carriage of the minor alleles reported to be pro-inflammatory. The frequency of carrying a minor allele at both IL-1A(+4845) and IL1B(−3954) was 35% in our study population, but this frequency increased to 84% in the B3/B3 and B2/B3 + B4/B3 pro-inflammatory haplotype-pairs compared with 23% in others. In this data set, CRP was less strongly associated with IL-1A(+4845), IL1B(+3954), or composites of these two SNPs, than the combined B3/B3 and B2/B3 + B4/B3 groups (data not shown).
Haplotype association with blood monocyte production of IL-1β
To validate the pro-inflammatory potential of the specific IL1B haplotype-pairs found to be associated with higher in vivo levels of IL-1β, we collected PBMCs from a separate population of individuals with no inflammatory diseases (N = 70) and analyzed IL-1β production after stimulation with lipopolysaccharide (LPS) (Fig. 3). Of the four haplotype-pairs associated with higher in vivo IL-1β levels, stimulated PBMCs from three of the four groups (B1/B1; B3/B3, B3/B2-B4) produced significantly more IL-1β protein than cells from those with haplotype-pairs in the reference group. PBMCs from the fourth group (B1/B3) produced more IL-1β protein than the reference group, but the difference was not significant.
IL1 haplotype influence on IL-1β protein levels produced by stimulated peripheral blood mononuclear cells. The IL-1β protein level (ng/ml) produced by LPS stimulated peripheral blood mononuclear cells from individuals with the indicated IL1B promoter haplotype pair (e.g. B3/B3) is shown as the geometric mean level (±SE) of IL-1β relative to the reference group. The reference group for the IL-1β levels includes all of the subjects with genotypes other than the four pro-inflammatory haplotype pairs shown in the figure. N = 70 healthy Caucasians. 1 Geometric mean of IL-1β levels by the indicated group. 2 The haplotype-pair group and number of subjects in the group. 3 The calculated p-value of the indicated haplotype-pair group in comparison to the reference group
Discussion
Inflammation is a major pathological component of many diseases, and the IL-1 family of cytokines, produced by the well-described IL-1 gene cluster (Cox et al. 1998; Nicklin et al. 2002), is a major contributor to the inflammatory process. Following pro-inflammatory challenge with a broad range of stimuli, including microbial products and oxidized LDL cholesterol, IL-1 and TNFα are among the first genes to be activated (Dinarello 1998; Hung et al. 2006; Karouzakis et al. 2006; Rosenwasser 1998). These cytokines activate receptor-mediated signaling mechanisms leading to induction of other pro-inflammatory genes such as IL-6 and COX2 that contribute to the inflammatory response in different tissues.
Given recent in vitro results (Chen et al. 2006) highlighting the importance of haplotype context in the functional expression of IL1B SNPs, we set out to determine whether certain pairs of functional IL1B haplotypes might be predictive of a higher level of in vivo production of IL-1β as well as higher levels of serum CRP. Since most genotyping is performed on DNA extracted from cells with paired chromosomes it is not possible to assign alleles to specific chromosomes within a chromosome pair. Most studies involving genotypes at multiple loci are therefore assessing how pairs of haplotypes relate to phenotypes of interest. Here, we report the results of an in vivo study building on the structure of IL1B haplotypes that can be unambiguously assigned to determine how IL-1 genotype patterns contribute to the differential expression of selected inflammatory responses. We also report validation support of the in vivo findings from experiments in vitro measuring IL-1β production by stimulated PBMCs obtained from a separate population of donors.
We first identified the IL-1 haplotype-pairs that, in comparison with other pairs, had the highest log IL-1β levels. The IL1B haplotype and genotype patterns that were associated with higher in vivo levels of IL-1 and CRP and higher production of IL-β by stimulated PBMCs are summarized in Table 6. Three of the four IL1B haplotype-pairs deemed as pro-inflammatory had one feature in common, namely being C/C homozygous at IL1B(−511). This supports the findings of others (Iacoviello et al. 2005) who reported that, in comparison with those carrying T/T, individuals with the C/C genotype had a significantly higher risk of myocardial infarction and ischemic stroke at a young age, as well as a significantly elevated release of IL-1β from mononuclear cells stimulated with LPS.
Our fourth and final pro-inflammatory haplotype-pair is characterized by a C/T genotype at IL1B(−511) together with a C/C genotype at IL1B(−3737) (Table 6). This result appears to support and clarify findings of Iacoviello et al. (2005). Specifically, they reported that individuals with C/T at IL1B(−511) are also at increased risk of both clinical and biochemical endpoints in cardiovascular disease, but less significantly than those carrying C/C at IL1B(−511). Our data suggest that this intermediate risk group of IL1B(−511) heterozygotes actually comprises two distinct groups of haplotype-pairs, one group includes B2/B3 or B4/B3 with C/C at IL1B(−3737) and the other group includes the B1/B2 or B1/B4 pairs that would give a C/T genotype at IL1B(−3737). The former, we speculate, would be associated with clinical endpoints and biochemical markers, perhaps as significantly as those carrying C/C at IL1B(−511), and the latter would be more similar to those with T/T at IL1B(−511). In this Caucasian population approximately 47% of the individuals carried IL1B(−511) genotype C/T, which was divided between 14% of the population that also carried IL1B(−3737) genotype C/C, which was pro-inflammatory, and 33% that also carried IL1B(−3737) genotype C/T, which was not associated with higher in vivo levels of IL-1β (Table 6). In this population, no individuals carried IL1B(−511) genotype C/T and IL1B(−3737) genotype T/T.
In our previous allele-specific transcription factor binding studies (Chen et al. 2006), NF-κB components showed increased binding to IL1B(−3737) allele C compared with allele T. This is consistent with the findings in the present study of increased IL-1β protein in subjects with the C/C genotype at IL1B(−3737), if they also carried IL1B(−511) genotype C/C or C/T. The IL1B(−511) genotype C/T was only associated with increased IL-1β protein when in combination with IL1B(−3737) C/C. IL1B(−3737) also appears to be a key determinant of whether or not an IL1B promoter pattern associated with high IL-1β expression is also associated with increased serum CRP levels (Table 6). This may be due to potential temporal differences in IL-1β expression with haplotypes that include different IL1B(−3737) alleles or may be due to different transcriptional regulation of IL-1 in Kuppfer cells of the liver where local hepatocytes produce most of the CRP that is detectable in serum. These findings further emphasize the critical role of haplotype context in the clinical expression of inflammatory mediators.
Haplotypes are often used to explore clinical associations with genetic variation over a relatively broad physical region of the genome. The primary value of haplotypes in that application is efficiency, i.e. to capture much of the genetic variation by means of a limited subset of known SNPs. The haplotypes used in this study served a different purpose. The enhancer-promoter region of a gene regulates expression of that gene by multiple transcription factors binding to specific DNA sequences. Complexes of bound transcription factors may influence binding of additional factors and ultimately initiate or regulate activation of transcription. This process has been extensively described for the IL1B gene (Listman et al. 2005). The IL1 SNPs included in this study have allele-specific influences on binding of transcription factors and/or transcription activity, and the biological activity of specific IL1 alleles was shown to change based on haplotype context (Chen et al. 2006). Since this group of SNPs work together to regulate transcription, associations with biological activity should focus on haplotype context rather than single SNP analysis. The approach used in this study appears to overcome two challenges with complex genetic systems. Firstly, it is often the case that multiple “risk” haplotypes have different alleles at a specific SNP. In that situation, analysis of individual SNPs will be misleading since both alleles may involve risk, given certain context. Secondly, the complexity also complicates a standard haplotype analysis. For example, the usual programs designed to derive and analyze haplotypes are not set up to consider the possibility of different protein production for each distinct pair of haplotypes that a specific individual inherited. In fact, this is what we did. The fact that haplotypes in the beta promoter can be scored unambiguously allowed us to sidestep the usual programs and to proceed by direct analysis of the pairs of haplotypes.
Although confidence in genotype–phenotype associations is strengthened when gene variants are used that have functional relevance to the clinical phenotype, molecular function studies on specific regulatory region SNPs are rarely consistent with clinical disease associations (Ioannidis and Kavvoura 2006). With current knowledge, there is no simple way to extrapolate the in vitro molecular observations on IL1B promoter haplotype activity (Chen et al. 2006) to predict the observed clinical associations with composite genotypes in this study. However, in this study we have specifically analyzed pairs of predominant haplotypes that have been shown to have distinctly different molecular functions and determined that those functional haplotypes were associated with significantly different in vivo and in vitro levels of IL-1β when analyzed as haplotype-pairs.
In several studies, investigators have concluded that carriage of minor alleles at IL-1A(+4845) and/or IL1B(+3954) represents a pro-inflammatory genotype (Brett et al. 2005; Haggerty et al. 2005; Seripa et al. 2005). For example, allele 2 at IL1B(+3954) is strongly associated with increased CRP in individuals presenting for cardiac catheterization (Berger et al. 2002). However, not all studies demonstrate such significance. One possibility is that IL-1A(+4845) and IL1B(+3954) act only as surrogate markers in linkage disequilibrium with causative genetic variants, possibly defined by IL1B haplotype-pair groups. In fact, among our haplotype-pair groups associated with elevated log IL-1β expression, 84% carried a minor allele at both IL-1A(+4845) and IL1B(−3954) compared with 23% in the remaining haplotype-pair groups.
It should be emphasized that these observations were made only in a Caucasian population. Investigators have recently reported (Wen et al. 2006) that peripheral blood leukocytes from Chinese individuals with haplotypes that include IL1B(−511) allele C produce more IL-1β protein than individuals with allele T, consistent with the findings of this study and those reported previously for Caucasians (Iacoviello et al. 2005). We have reported substantial differences in the distribution of IL1B haplotypes between Caucasian and African-American populations (Chen et al. 2006) and evaluation of the relationship of IL1B haplotype-pairs with inflammatory mediators in other population groups is in progress. The differences in distribution of these functional IL1B haplotypes may influence results of associations with individual SNPs or haplotypes in different populations. This is evident in the data for the B1 haplotype-pairs, where the predominant pairs include two (B1/B1 and B1/B3) associated with higher levels of IL-1β and one pair (B1/B2) associated with low levels of IL-1β. In an Asian population (data not shown) the B1/B1 frequency is similar to that found in Caucasians (21 and 22%, respectively), but the B1/B2 frequencies (38 and 25%) and B1/B3 frequencies (3 and 17%) are different. These may produce confusing results with either single SNP or haplotype analyses, but appear to be readily explained in an analysis of haplotype-pairs.
This study has certain limitations. First, it is reasonable to assume that the present study reflects tissue inflammatory responses in which monocytes/macrophages are the main contributors to local production of IL-1β. In other tissues, such as bone, muscle, or brain, in which other cell types may be involved in IL-1β production, the relationships between variations in regulatory regions and tissue IL-1β production may be different. Second, haplotype assignment is usually a mathematical assignment and has certain limitations. In this study, due to the predominant genotypes found in Caucasians, the assignment of these specific IL1B promoter haplotypes is unambiguous and was done by direct assignment. Finally, the study may only reflect functional relationships in Caucasians. As discussed above, the population differences in distributions of some of the IL1B haplotypes may produce misleading genotype–phenotype associations in different populations. We believe those differences may be resolvable by the use of haplotype-pairs. In addition, studies in both Caucasians (Iacoviello et al. 2005) and Asians (Wen et al. 2006) suggest the populations have some similarities in IL-1 genetic influence on monocyte expression of IL-1β.
Confirmation that these biomarker-genotype associations relate to risk of clinical disease phenotypes will be a key step in linking inflammation genetics to disease. These studies are underway. The identification of functionally distinct promoter haplotypes in the gene for IL-1β, and the use of pairs of those haplotypes, seems to have the potential to increase our understanding of how IL-1 promoter SNPs relate to biomarker phenotypes and the risk of clinical events in diseases with an inflammatory component.
References
Adjers K, Pessi T, Karjalainen J, Huhtala H, Hurme M (2004) Epistatic effect of IL1A and IL4RA genes on the risk of atopy. J Allergy Clin Immunol 113:445–447
Armitage GC (2004) Analysis of gingival crevice fluid and risk of progression of periodontitis. Periodontol 2000 34:109–119
Berger P, McConnell JP, Nunn M, Kornman KS, Sorrell J, Stephenson K, Duff GW (2002) C-reactive protein levels are influenced by common IL-1 gene variations. Cytokine 17:171–174
Bo S, Gambino R, Uberti B, Mangiameli MP, Colosso G, Repetti E, Gentile L, Cassader M, Pagano GF (2005) Does C-reactive protein identify a subclinical metabolic disease in healthy subjects? Eur J Clin Invest 35:265–270
Brett PM, Zygogianni P, Griffiths GS, Tomaz M, Parkar M, D’Aiuto F, Tonetti M (2005) Functional gene polymorphisms in aggressive and chronic periodontitis. J Dent Res 84:1149–1153
Camargo MC, Mera R, Correa P, Peek RM Jr., Fontham ET, Goodman KJ, Piazuelo MB, Sicinschi L, Zabaleta J, Schneider BG (2006) Interleukin-1beta and interleukin-1 receptor antagonist gene polymorphisms and gastric cancer: a meta-analysis. Cancer Epidemiol Biomarkers Prev 15:1674–1687
Capri M, Salvioli S, Sevini F, Valensin S, Celani L, Monti D, Pawelec G, De Benedictis G, Gonos ES, Franceschi C (2006) The genetics of human longevity. Ann N Y Acad Sci 1067:252–263
Champagne CM, Buchanan W, Reddy MS, Preisser JS, Beck JD, Offenbacher S (2003) Potential for gingival crevice fluid measures as predictors of risk for periodontal diseases. Periodontol 2000 31:167–180
Chen H, Wilkins LM, Aziz N, Cannings C, Wyllie DH, Bingle C, Rogus J, Beck JD, Offenbacher S, Cork MJ, Rafie-Kolpin M, Hsieh CM, Kornman KS, Duff GW (2006) Single nucleotide polymorphisms in the human interleukin-1B gene affect transcription according to haplotype context. Hum Mol Genet 15:519–529
Cox A, Camp NJ, Nicklin MJ, di Giovine FS, Duff GW (1998) An analysis of linkage disequilibrium in the interleukin-1 gene cluster, using a novel grouping method for multiallelic markers. Am J Hum Genet 62:1180–1188
Curran JE, Jowett JB, Elliott KS, Gao Y, Gluschenko K, Wang J, Abel Azim DM, Cai G, Mahaney MC, Comuzzie AG, Dyer TD, Walder KR, Zimmet P, MacCluer JW, Collier GR, Kissebah AH, Blangero J (2005) Genetic variation in selenoprotein S influences inflammatory response. Nat Genet 37:1234–1241
di Giovine FS, Camp N, Cox A, Chaudhary A, Crane A, Duff G (2000) Detection and population analysis of IL-1 and TNF gene polymorphisms in Cytokine Molecular Biology. Oxford University Press, Oxford
Dinarello CA (1998) Interleukin-1, interleukin-1 receptors and interleukin-1 receptor antagonist. Int Rev Immunol 16:457–499
Ebersole JL, Singer RE, Steffensen B, Filloon T, Kornman KS (1993) Inflammatory mediators and immunoglobulins in GCF from healthy, gingivitis and periodontitis sites. J Periodontal Res 28:543–546
El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, Herrera J, Lissowska J, Yuan CC, Rothman N, Lanyon G, Martin M, Fraumeni JF Jr., Rabkin CS (2000) Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature 404:398–402
Engels EA, Wu X, Gu J, Dong Q, Liu J, Spitz MR (2007) Systematic evaluation of genetic variants in the inflammation pathway and risk of lung cancer. Cancer Res
Florez O, Zafra G, Morillo C, Martin J, Gonzalez CI (2006) Interleukin-1 gene cluster polymorphism in chagas disease in a Colombian case-control study. Hum Immunol 67:741–748
Graves DT, Cochran D (2003) The contribution of interleukin-1 and tumor necrosis factor to periodontal tissue destruction. J Periodontol 74:391–401
Haggerty CL, Ferrell RE, Hubel CA, Markovic N, Harger G, Ness RB (2005) Association between allelic variants in cytokine genes and preeclampsia. Am J Obstet Gynecol 193:209–215
Hansson GK, Libby P (2006) The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol 6:508–519
Hung YC, Hong MY, Huang GS (2006) Cholesterol loading augments oxidative stress in macrophages. FEBS Lett 580:849–861
Iacoviello L, Di Castelnuovo A, Gattone M, Pezzini A, Assanelli D, Lorenzet R, Del Zotto E, Colombo M, Napoleone E, Amore C, D’Orazio A, Padovani A, de Gaetano G, Giannuzzi P, Donati MB (2005) Polymorphisms of the interleukin-1beta gene affect the risk of myocardial infarction and ischemic stroke at young age and the response of mononuclear cells to stimulation in vitro. Arterioscler Thromb Vasc Biol 25:222–227
Ioannidis JP, Kavvoura FK (2006) Concordance of functional in vitro data and epidemiological associations in complex disease genetics. Genet Med 8:583–593
Kahraman S, Yilmaz R, Arici M, Altun B, Erdem Y, Yasavul U, Turgan C (2006) IL-10 genotype predicts serum levels of adhesion molecules, inflammation and atherosclerosis in hemodialysis patients. J Nephrol 19:50–56
Kardys I, Knetsch AM, Bleumink GS, Deckers JW, Hofman A, Stricker BH, Witteman JC (2006) C-reactive protein and risk of heart failure. The Rotterdam Study. Am Heart J 152:514–520
Karouzakis E, Neidhart M, Gay RE, Gay S (2006) Molecular and cellular basis of rheumatoid joint destruction. Immunol Lett 106:8–13
Kornman KS (2006) Interleukin 1 genetics, inflammatory mechanisms, and nutrigenetic opportunities to modulate diseases of aging. Am J Clin Nutr 83:475S–483S
Kozlowski P, Miller DT, Zee RY, Danik JS, Chasman DI, Lazarus R, Cook NR, Ridker PM, Kwiatkowski DJ (2006) Lack of association between genetic variation in 9 innate immunity genes and baseline CRP levels. Ann Hum Genet 70:574–586
Lee KA, Ki CS, Kim HJ, Sohn KM, Kim JW, Kang WK, Rhee JC, Song SY, Sohn TS (2004) Novel interleukin 1beta polymorphism increased the risk of gastric cancer in a Korean population. J Gastroenterol 39:429–433
Listman JA, Wara-Aswapati N, Race JE, Blystone LW, Walker-Kopp N, Yang Z, Auron PE (2005) Conserved ETS Domain Arginines Mediate DNA Binding, Nuclear Localization, and a Novel Mode of bZIP Interaction. J Biol Chem 280:41421–41428
McGeer PL, Rogers J, McGeer EG (2006) Inflammation, anti-inflammatory agents and Alzheimer disease: the last 12 years. J Alzheimers Dis 9:271–276
Muraki Y, Tsutsumi A, Takahashi R, Suzuki E, Hayashi T, Chino Y, Goto D, Matsumoto I, Murata H, Noguchi E, Sumida T (2004) Polymorphisms of IL-1 beta gene in Japanese patients with Sjogren’s syndrome and systemic lupus erythematosus. J Rheumatol 31:720–725
Napoleone E, Di Santo A, Camera M, Tremoli E, Lorenzet R (2000) Angiotensin-converting enzyme inhibitors downregulate tissue factor synthesis in monocytes. Circ Res 86:139–143
Nicklin MJ, Barton JL, Nguyen M, FitzGerald MG, Duff GW, Kornman K (2002) A sequence-based map of the nine genes of the human interleukin-1 cluster. Genomics 79:718–725
Offenbacher S, Barros S, Champagne CM, Moss K, Welborn A, Levy RI, Lin D, Beck JD (2005) Diagnosis of periodontal disease at the periodontal tissue-biofilm interface: biological correlates. Oral Biosci Med 213:215–220
Offenbacher S, Barros SP, Singer RE, Moss K, Williams RC, Beck JD (2007) Periodontal disease at the biofilm-gingival interface. J Periodontol 78:1911–1925
Orozco A, Gemmell E, Bickel M, Seymour GJ (2006) Interleukin-1beta, interleukin-12 and interleukin-18 levels in gingival fluid and serum of patients with gingivitis and periodontitis. Oral Microbiol Immunol 21:256–260
Papp AC, Hatzakis H, Bracey A, Wu KK (1989) ARIC hemostasis study—I. Development of a blood collection and processing system suitable for multicenter hemostatic studies. Thromb Haemost 61:15–19
Rainero I, Bo M, Ferrero M, Valfre W, Vaula G, Pinessi L (2004) Association between the interleukin-1alpha gene and Alzheimer’s disease: a meta-analysis. Neurobiol Aging 25:1293–1298
Ridker PM (2003) Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 107:363–369
Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, McCabe CH, Pfeffer MA, Braunwald E (2005) C-reactive protein levels and outcomes after statin therapy. N Engl J Med 352:20–28
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH (1998a) Plasma concentration of C-reactive protein and risk of developing peripheral vascular disease. Circulation 97:425–428
Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, Flaker GC, Braunwald E (1998b) Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation 98:839–844
Rosenwasser LJ (1998) Biologic activities of IL-1 and its role in human disease. J Allergy Clin Immunol 102:344–350
Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA (2002) Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet 70:425–434
Schmidt R, Schmidt H, Curb JD, Masaki K, White LR, Launer LJ (2002) Early inflammation and dementia: a 25-year follow-up of the Honolulu-Asia Aging Study. Ann Neurol 52:168–174
Seripa D, Matera MG, Dal Forno G, Gravina C, Masullo C, Daniele A, Binetti G, Bonvicini C, Squitti R, Palermo MT, Davis DG, Antuono P, Wekstein DR, Dobrina A, Gennarelli M, Fazio VM (2005) Genotypes and haplotypes in the IL-1 gene cluster: analysis of two genetically and diagnostically distinct groups of Alzheimer patients. Neurobiol Aging 26:455–464
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Vilaichone RK, Mahachai V, Tumwasorn S, Wu JY, Graham DY, Yamaoka Y (2005) Gastric mucosal cytokine levels in relation to host interleukin-1 polymorphisms and Helicobacter pyloricagA genotype. Scand J Gastroenterol 40:530–539
Wen AQ, Wang J, Feng K, Zhu PF, Wang ZG, Jiang JX (2006) Effects of haplotypes in the interleukin 1beta promoter on lipopolysaccharide-induced interleukin 1beta expression. Shock 26:25–30
Woloshin S, Schwartz LM (2005) Distribution of C-reactive protein values in the United States. N Engl J Med 352:1611–1613
Acknowledgments
The study was supported in part by Interleukin Genetics. The Atherosclerosis Risk in Communities (ARIC) Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, N01-HC-55022 and Grant. R01-DE11551 from the National Institute of Dental Research. The authors thank the staff and participants of the ARIC Study for their important contributions. MIUR (Ministero dell’Università e Ricerca, Italia) -Programma Triennale di Ricerca, grant D. 1588, supported the in vitro peripheral blood mononuclear cell work by Catholic University in Campobasso, Italy. Drs. Kornman, Rogus, and Huttner are employees of Interleukin Genetics. Dr. Duff is a scientific advisor to Interleukin Genetics, and Dr. Wang is a consulting statistician for Interleukin Genetics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rogus, J., Beck, J.D., Offenbacher, S. et al. IL1B gene promoter haplotype pairs predict clinical levels of interleukin-1β and C-reactive protein. Hum Genet 123, 387–398 (2008). https://doi.org/10.1007/s00439-008-0488-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-008-0488-6