Abstract
Segregation of preeclampsia into early-onset, placental and late-onset, maternal subtypes along with the acknowledgement of the contribution of epigenetics in placentally expressed genes proved to be a key first step in the identification of essential gene variants associated with preeclampsia. Application of this insight to other populations and related pregnancy-induced syndromes, such as HELLP, and acknowledgment of the features shared between chromosomal loci associated with preeclampsia in different populations provide the rationale for new strategies for the identification of susceptibility genes and for new and more effective diagnostic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Preeclampsia and its variants are considered multifactorial pregnancy-associated diseases that form a spectrum of the same illness (Sibai et al. 2005; Redman and Sargent 2005; Baxter and Weinstein 2004). All models proposed (as outlined recently in two complementary reviews) recognize the importance of the placenta (no placenta, no disease), but differ in the order and relative contribution of the immunological and vascular events and effects in the mother (Sibai et al. 2005; Redman and Sargent 2005). However, mouse models and progress in the genetics of preeclampsia indicate that different genes segregating with different populations or disease entities initiate at distinct points a common central pathway (Cross 2003; Van Dijk et al. 2005). The central pathway shared in all patients and responsible for the induction of maternal symptoms, as reflected clinically by changes in plasma levels six to ten weeks prior to clinical symptoms, is the PlGF-sFLT1-endoglin axis (Venkatesha et al. 2006; Tjoa et al. 2001). Placenta-derived sFLT1 in sera of preeclamptic females can induce hypertension, serum levels correlate with disease severity, and, in combination with soluble endoglin, induces preeclampsia in pregnant rats (Venkatesha et al. 2006). Changed levels of these soluble angiogenic factors, as well as other yet unknown mediators of endothelial activation, produced by the hypoxic placenta induce maternal symptoms by interference with TGF-ß-mediated NOS-dependent vasodilation (Venkatesha et al. 2006; Soleymanlou et al. 2005; Li et al. 2005). The questions therefore emerge at which points the preeclamptic pathway is initiated genetically and how these genes induce placental dysfunction.
Early placental and late maternal preeclampsia
Preeclampsia comes in two forms: early (symptoms < week 34) (type I) and late (symptoms > week 34) (type II) (Table 1) (Redman and Sargent 2005; Egbor et al. 2006; Pijnenborg et al. 2006; Duckit and Harrington 2005; Sklaerven et al. 2005). These forms are different in genetic risk and inheritance (Duckit and Harrington 2005; Sklaerven et al. 2005). Late-onset, maternal preeclampsia arises from the interaction between a normal placenta and a predisposed maternal constitution reflecting microvascular disease as occurs with long-term hypertension, diabetes or other states of metabolic dysbalance or reflecting a maternal genetic predisposition due to cis- or transacting genetic variations in interacting genes. Pregnancy in these metabolically or genetically predisposed woman is an increased stress test for life, where the additional demand asked for by the growing feto-placental unit exceeds the maternal resources. The end of pregnancy, i.e. the onset and process of labour, is a temporary, but strong challenge of the maternal system asked for by the feto-placental unit in progress of being disconnected from the maternal (vascular) system. In this situation, decompensation near term will present in predisposed women as late peri- or postpartum preeclampsia. Decompensation in this context is meant as the situation where the maternal haemodynamic and metabolic resources fail to comply with and to follow the dynamic and specific changes in the placenta and uterus that precede the onset of labour. Likewise, the biochemical factors disturbed in and informative for this process can be predicted to be multiple, but related to the induction of labour. In contrast, early-onset placental preeclampsia starts with abnormal placentation, has a high recurrence risk, and runs in families with a clear genetic component (recurrence across generations and occurrence within families) (Redman and Sargent 2005; Pijnenborg et al. 2006; Sklaerven et al. 2005). This distinction between early and late preeclampsia not only correlates with the risk factors (Table 1), but also with all animal models of preeclampsia, when growth restriction is used as discriminator (Supplementary Table 1). It should be stressed that, as for early onset preeclampsia, the early form of the HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome is placental in origin. The existence of discordant monozygous twin sisters with only one sister affected confirms that HELLP starts in a gene expressed in the placenta (Thornton and Onwude 1991). The additional, but different genetic contribution of the partner explains why only one twin sister develops disease in discordant monozygous twins.
A call for consortium style genome-wide association studies
Previous searches for candidate genes (about 50) included genes involved with thrombophilia (F5, F2), haemodynamics (AGT, REN, ACE), endothelial function (NOS3, EDN1), cytokines (TNF, IL1A), oxidative stress (GSTP1, GSTM1), lipid metabolism (LPL), the endocrine system (ESR1) and angiogenesis (VEGF) (Chappell and Morgan 2006). These approaches have failed to identify a single universally accepted susceptibility gene for preeclampsia. Screening for candidate genes with selection based on function, rather than confirmed linkage or association with genome-wide significance, are subject to non-replication and inadequate prioritizing of polymorphisms with different relative risks depending on the SNP selected.
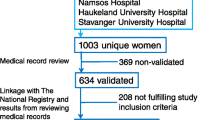
Efforts allowing consortium style, large scale genome-wide association studies permitting convincing statistical evidence (P < 10−8) at the genome-wide level are urgently needed. To detect an effect with an odds ratio of 1.5 at a minor allele frequency of 0.1 with 80% power at α = 5 × 10−7, the analysis of 2,000 cases and 3,000 controls is needed (Todd 2006). This number is now clearly within reach for preeclampsia. Combination of the initiatives as the Dutch Preeclampsia study (150 affected sibpair families selected from 3,000 patients), the British Genetics of Pre-Eclampsia (GOPEC) consortium (627 index pregnancies), and the Norwegian HUNT cohort (1138 preeclamptic women) complemented with the cohorts from Australia/New Zealand (34 pedigrees), Finland (15 families, 350 index pregnancies) and other countries provide adequate size and therefore power to provide precise genetic risks with narrow confidence intervals (The GOPEC consortium 2005; Lachmeijer et al. 2001; Arngrimsson et al. 1999; Moses et al. 2000; Laasanen et al. 2003; Laivuori et al. 2003; Moses et al. 2006; Holmen et al. 2003).
However, several aspects should be taken into account before embarking on this expedition. The affected sibpair selection as done in the Dutch study, besides permitting powerful linkage analysis, had two additional advantages (Van Dijk et al. 2005; Lachmeijer et al. 2001). The preeclamptic females studied were not restricted to primigravids. The majority of affected sibpairs in these families, in addition to having preeclamptic pregnancies themselves, were born from preeclamptic mothers, i.e. from females that had more than one preeclamptic pregnancy. By design, these preeclamptic patients were therefore not limited to first pregnancies. Although the preferential occurrence of preeclampsia in first pregnancies is considered central to the primiparity concept underlying the immune-maladaptation hypothesis (Sibai et al. 2005), our cohort neither supports this nor selects for this. The latter guarantees the absence of confounding factors. Secondly, this selection with inclusion of both parents and two affected sibs targets the early familial form of preeclampsia associated with intrauterine growth retardation, i.e. placental preeclampsia (Van Dijk et al. 2005; Lachmeijer et al. 2001; Oudejans et al. 2004). The GOPEC study and studies with similar design appear biased towards maternal preeclampsia, as indicated by the absence of growth restriction (The GOPEC consortium 2005). Given this difference in the type of preeclampsia studied in both cohorts and provided this distinction is recognized in other cohorts, the Dutch and British cohorts likely target different genes, but are complementary for placental and maternal preeclampsia, respectively.
Transcription based prioritization of candidate regions and genes
The high incidence of preeclampsia with androgenetic pregnancies, the induction of preeclampsia in knockout mice mutated for the imprinted, maternally expressed p57kip2 (CDKN1C) gene, and the presence of confirmed or predicted imprinted genes in loci associated with preeclampsia led to the exploration of the contribution of epigenetics in the aetiology of preeclampsia (Van Dijk et al. 2005; Oudejans et al. 2004). This approach proved essential in the Dutch preeclampsia study with identification of STOX1, coding for a novel member of the winged helix domain containing proteins related to the forkhead (FOX) multigene family. Following confirmation of linkage with the 10q22 region and the identification of a parent-of-origin effect, candidate genes were prioritized by transcription-based analysis (Van Dijk et al. 2005; Oudejans et al. 2004). Genes were targeted for mutation analysis by selection for genes with downregulated expression in androgenetic placentas. This approach of transcription-based prioritization of candidate genes in regions with linkage was recently taken to a higher level through genome-wide expression screening by the Australian/New Zealand group (Moses et al. 2006). Assuming that perturbed mRNA expression in the decidua is a recognizable signature for maternal preeclampsia, gene expression was quantified using Whole Genome Bioarrays comprising ∼55,000 30-mer oligonucleotide probes. Comparison of normalized expression intensity between normotensive and preeclamptic decidua yielded 17 transcripts within the region with linkage (2q22) with at least a 2.5-fold upregulation in association with preeclampsia. Highest priority was given to the activin receptor gene, ACVR2. This gene, in addition to a greater than tenfold difference in gene expression between normotensive and preeclamptic decidua, yielded the highest score by GeneSniffer analysis. One SNP (rs1424954) showed preliminary evidence of association with preeclampsia (P = 0.007). The gene within the 1-LOD support interval on 2q with the largest increase in relative intensity (>70 fold) encodes the candidate mediator of the p53-dependent G2 arrest (REPRIMO). The potential of this approach has been confirmed recently. In the Norwegian population, three SNPs within the ACVR2 gene were confirmed to be associated with preeclampsia (Tommerdal et al. 2006). The strongest association was found with rs1424941 (P = 0.013). Therefore, the 2q22 region appears to contain a common susceptibility locus associated with maternal preeclampsia, which is present in multiple populations (Australia/New Zealand, Iceland, Norway) (Table 2). Restricted association analysis by chromosome-specific, high density SNP analysis might permit identification in a timely and less costly manner of the actual polymorphic variations responsible for preeclampsia in these populations.
Dichotomous nature of genetic variations
A prevalent mutation consisting of an absolutely conserved Y153H variation in the DNA binding region of the winged helix domain containing STOX1 gene segregates maternally and is associated with the preeclamptic phenotype in all Dutch families studied (Van Dijk et al. 2005). However, the Y153H variation occurs in the normal population as well, and is in fact the predominant variation in certain populations such as the CHB population (Han Chinese in Beijing) (www.hapmap.org). Given the large region on 10q22 with parent of origin effect and the fact that similar variations in related forkhead genes (such as FOXC1) cause disease by interaction with downstream genes differentially interacting with wildtype and mutant variants, a second gene variation is needed to explain the full phenotype in Dutch females (Van Dijk et al. 2005). This second gene most likely resides on 10q22 as well. This dichotomous nature of two gene variations in interacting genes appears common rule rather than the exception in preeclampsia. This parallels the recent findings from other common diseases with low effect involving frequently occurring polymorphisms. This has been demonstrated for the two genes (complement factor B, CBF; complement component 2, C2) associated with age-related macular degeneration and can be expected to be the case for the variant of transcription factor 7-like 2 gene (TCF7L2) associated with type 2 diabetes (Gold et al. 2006; Grant et al. 2006). The Australian/New Zealand group corrected for this by applying variance components-based linkage analysis (Moses et al. 2006). Using this approach, data from pedigree structures of arbitrary complexity can be used to make inference regarding the localization and effect sizes of quantitative trait loci (QTL). This led to the identification of the ACVR2 gene and as confirmed in the Norwegian population (Moses et al. 2006; Tommerdal et al. 2006).
Epigenetic inheritance in preeclampsia
A striking parallel exists in the epigenetic and other features between the 10q22 locus and the 2p13 locus associated with preeclampsia in Dutch and Icelandic females, respectively (Van Dijk et al. 2005; Arngrimsson et al. 1999; Oudejans et al. 2004). Within a large region in both chromosomes, shared features include the presence and similar line-up of paralogous genes (EGR2-CTNNA3-HK1-TACR2), genes predicted to be imprinted (LOXL3, DOK1, HK2, TACR1) and other features (FRA10D, FRA2E) (Table 3) (Luedi et al. 2005). The 2p13 locus previously found to segregate with two large Icelandic families has now been confirmed to be associated with the Finnish populations as well (Arngrimsson et al. 1999; Laasanen et al. 2003). Ongoing searches for the 2p13 gene are likely to be successful if these similarities are taken into account, i.e. by searching for placentally expressed genes on 2p13 potentially subject to epigenetics within the region of 10q22 and 2p13 with common evolutionary origin. The region on 2p13 flanked by D2S2111-D2S1777 fulfills these criteria (Table 3).
Genetics of polyploidy
The variant STOX1 gene carried and transmitted by Dutch preeclamptic females has been predicted to induce premature trophoblast differentiation (Van Dijk et al. 2005). By premature differentiation from diploid, invasive into polyploid, non-invasive giant cells, the process normally controlled by these cells, establishment of feto-maternal vascular connection, becomes defective by a partial failure in trophoblast invasion (Van Dijk et al. 2005; Pijnenborg et al. 2006). Giant cell transformation is also a normal feature of liver cells and megakaryocytes, i.e. the cells predominantly affected in the HELLP syndrome. This suggests parallels in control. However, as explained above, the HELLP syndrome is placental in origin. This indicates that, if parallels in genetic control of polyploidy exist, they are indirect. Support for this exists. Molecules (e.g. soluble FLT1 receptors) that prevent the VEGF-FLT1 interaction on the membrane of precursor megakaryocytes significantly inhibit polyploidization, while addition of exogenous VEGF or PlGF markedly potentiates megakaryocyte maturation (Casella et al. 2003). These data confirm a potential relation between polyploidy, the cells affected in HELLP and the effector molecules of preeclampsia and warrant further exploration. Secondly, genetic linkage analysis has shown that the HELLP syndrome is a distinct genetic entity. In fact, discrimination of preeclampsia patients without HELLP and those with HELLP only was essential in the Dutch genome-wide linkage analysis (Lachmeijer et al. 2001). In Dutch females, the 12q24 region is linked with HELLP. As no epigenetic parallels exist between 12q24 and 10q22/2p13, and given the existence of discordant monozygous twin sisters, the HELLP susceptibility gene is likely to involve a placentally expressed gene inherited in an autosomal recessive manner by the child.
The paraHOX paralogon
Under a strict diagnostic model, the 4q34 region between D4S450-D4S610 was identified in the Australian/New Zealand cohort by parametric linkage analysis (Harrison et al. 1997). Using the same strict diagnostic criteria, but following variance-components-based linkage, two additional susceptibility loci were identified on 5q (D5S644) and 13q (D13S173) (Johnson et al. 2006). Interestingly, these three regions, all associated with the Australian/New Zealand loci, coincide with the paraHOX paralogon cluster (Fredriksson et al. 2003). Phylogenetic analysis of the superfamily of G-protein coupled receptors identified four paralogon regions, 4q, 5q, 13q and X, the so-called paraHOX paralogon, enriched for G-protein receptors of the β-group of rhodopsin receptors (Fredriksson et al. 2003). This cluster contains the endothelin-related receptors EDNRA and EDNRB. In addition, the 4q region contains the STOX2 gene. These parallels could assist in the identification of the susceptibility genes associated with preeclampsia in specific populations.
Malice in wonderland
The majority, if not all, loci associated with preeclampsia, when grouped according to disease entity or epigenetic features, share phylogenetic features reflecting a common evolutionary origin and/or function. In other words, the conserved genetic functions underlying the development of hemochorial placentation in mammals in general, and in humans in particular, are mirrored in the genetics of preeclampsia.
References
Arngrimsson R et al (1999) Hum Mol Genet 8:1799
Baxter JK, Weinstein L (2004) Obstet Gynecol Sur 59:838
Casella I et al (2003) Blood 101:1316
Chappell S, Morgan L (2006) Clin Sci 110:443
Cross JC (2003) Clin Genet 64:96
Duckit K, Harrington D (2005) Br Med J 330:565
Egbor M et al (2006) BJOG 113:580
Fredriksson R, Lagerstrom MC, Lundin LG, Shioth HB (2003) Mol Pharmacol 63:1258
Gold B et al (2006) Nat Genet 38:458
Grant SFA et al (2006) Nat Genet 38:320
Harrison GA et al (1997) Am J Hum Genet 60:1158
Holmen J et al (2003) Norsk Epidemiol 13:19
Johnson MP et al (2006) Hypertens Pregnancy 25(suppl 1):46
Laasanen J et al (2003) Eur J Hum Genet 11:232
Lachmeijer AM et al (2001) Eur J Hum Gen 9:758
Laivuori H et al (2003) Am J Hum Genet 72:168
Li H, Gu B, Zhang Y, Lewis DF, Wang Y (2005) Placenta 26:210
Luedi PP, Hartemink AJ, Jirtle RL (2005) Genome Res 15:875
Moses EK et al (2000) Am J Hum Genet 67:1581
Moses EK et al (2006) Mol Hum Reprod 12:505
Oudejans CBM et al (2004) Mol Hum Reprod 10:589
Pijnenborg R, Vercruysse L, Hanssens M (2006) Placenta (Epub ahead of print)
Redman CW, Sargent IL (2005) Science 308:1592
Sibai B, Dekker G, Kupferminc M (2005) Lancet 365:785
Sklaerven R et al (2005) BMJ 330:633
Soleymanlou N et al (2005) J Clin Endocrinol Metab 90:4299
The GOPEC consortium (2005) Am J Hum Gen 77:127
Thornton J, Onwude J (1991) Br Med J 303:1241–1242
Tjoa ML et al (2001) Obstet Gynecol 98:600
Todd JA (2006) Nat Genet 38:731
Tommerdal L et al (2006) Hypertens Pregnancy 25(suppl 1):44
Van Dijk M et al (2005) Nat Genet 37:514
Venkatesha S et al (2006) Nat Med 12:642
Acknowledgments
Marie van Dijk is supported by the Special Non-Invasive Advances in Fetal and Neonatal Evaluation (SAFE) Network of Excellence (LSHB-CT-2004-503243).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Oudejans, C.B.M., van Dijk, M., Oosterkamp, M. et al. Genetics of preeclampsia: paradigm shifts. Hum Genet 120, 607–612 (2007). https://doi.org/10.1007/s00439-006-0259-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-006-0259-1