Abstract
We report a young boy with penoscrotal hypospadias, anal atresia (AA) with a recto-urethral fistula, a hypoplastic kidney and a balanced translocation t(6;17)(p21.31;q11.2). Physical mapping of the breakpoints localized the chromosome 6 breakpoint within an intron of the gene lipoma HMGIC fusion partner-like 5 (LHFPL5) whereas the chromosome 17 breakpoint was mapped to the first intron of the 182-FIP gene encoding the Fragile X Mental Retardation Protein Interacting Protein. Sequence analysis across the breakpoints revealed an almost perfectly balanced translocation with a 2 bp deletion on the derivative chromosome 6 and a 7 bp duplication on the derivative chromosome 17. We identified a fusion transcript consisting of the first exon of 182-FIP and the last exon of LHFPL5 in patient-derived cells. Quantitative expression analysis of the genes flanking the breakpoints, revealed increased transcript levels for SFRS protein kinase 1 (SRPK1) and TAO kinase 1 (TAOK1) which suggests a positional effect due to the translocation. We hypothesize that the urogenital and anorectal malformations in the patient result from one or several mechanisms including disruption of the genes 182-FIP and LHFPL5, altered expression of the genes flanking the translocation breakpoints and, a gain of function mechanism mediated by the 182-FIP-LHFPL5 fusion transcript.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypospadias consist of a misplaced urethral orifice along the frontal side of the penis and is one of the most common malformations among males with a frequency of 1 in every 250–300 live births (Baskin 2000; Gallentine et al. 2001; Paulozzi 1999). The degree of hypospadias varies in its severity, ranging from a slight anomaly with the urethral orifice just below the tip of the penis to extreme cases in which the urethral orifice is located in the perineum. Hypospadias is believed to be multifactorial or polygenic and the majority of the cases are sporadic. Some rare familial cases are described where the malformation segregates as a dominant trait (Nordenskjold et al. 1999). Hypospadias is associated with low birth weight in discordant monozygotic twins which has been suggested to be related to inadequacy of the placenta to produce enough human chorionic gonadotropin for two male foetuses (Fredell et al. 1998). Anorectal malformations (ARMs) including anal atresia (AA) have an incidence of 1 in 1,500–5,000 live births with a male to female ratio of 1.2–2:1. ARMs is associated with cytogenetic rearrangements such as 13q deletions, 1q deletions, tetrasomy of the short arm of chromosome 12, trisomy 21 and 7q36 deletions (Bartsch et al. 1996; Seri et al. 1999; Steinbach and Rehder 1987; Takano et al. 1997; Van Buggenhout et al. 1999; Zlotogora et al. 1989). In addition, several defined clinical syndromes are also associated with ARMs. These include VACTERL, primary developmental field defect, CHARGE association, Townes-Brocks, Johanson-Blizzard, Pallister-Hall, Currarino, Opitz, Zellweger, FG syndrome and other multiple congenital anomaly patterns (Christensen et al. 1990; Endo et al. 1999; Hassink et al. 1996; Martinez-Frias 1994; Martinez-Frias and Frias 1999; Rodono et al. 1997; Sutherland et al. 1996). Up to 70% of cases with ARMs present with additional congenital abnormalities most commonly affect the genitourinary system which suggests a common pathological event (Baskin 2000; Cho et al. 2001; Hassink et al. 1996; Martinez-Frias et al. 2000; Shaul and Harrison 1997).
During early mammalian embryonic development, growth of the mesenchymal upper (Tourneux) and lateral (Rathke) folds results in a midline septation event of the cloaca and a separation of the urinary and the fecal compartments. From this point, sex-specific differentiation of the urogenital system takes place. The high proportion of patients with both ARMs and hypospadias, has lead to the assumption of a common developmental defect during formation of the urethra and septation of the cloaca (Dravis et al. 2004). The mechanisms behind these relatively common malformations are still poorly understood and few genes have so far been identified in these events.
In this study, we report a young male presenting with penoscrotal hypospadias, AA with a recto-urethral fistula and, a hypoplastic kidney. Chromosomal analysis showed that the patient had a de novo reciprocal balanced translocation, t(6;17)(p21.31;q11.2). We report the detailed physical mapping of the translocation breakpoints involving the chromosome 6 gene lipoma HMGIC fusion partner-like 5 (LHFPL5) and the chromosome 17 gene 182-FIP encoding the 82-kD Fragile X Mental Retardation Protein (FMRP) Interacting Protein. A 182-FIP-LHFPL5 fusion transcript was detected as a result of the translocation in the patient. Quantitative real time RT–PCR revealed increased transcript levels for the genes flanking the translocation breakpoints. We hypothesize that the described reciprocal translocation with its molecular consequences is of functional importance for the malformations in the patient.
Materials and methods
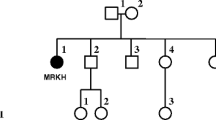
The patient is a ten-year-old boy born in gestational week 36 and after a normal pregnancy (birth weight of 2560 g, Apgar score of 9/10/10). The patient was diagnosed with penoscrotal hypospadias, AA, a recto-urethral fistula and a hypoplastic right-side kidney. The kidney was found silent and removed. Histopathological examination showed agenesia with embryonic and immature kidney structures. Additional clinical examinations and investigations including X-rays of skeleton and intestines, abdominal ultrasound and echocardiography revealed no additional abnormalities. Steroid profile and metabolic screening was found normal. The coding sequence of the Wilms tumour 1 (WT1) gene was analysed with no variations when compared to the reference sequences. Chromosomal analysis revealed a t(6;17)(p21.31;q11.2) karyotype. Both parents have normal karyotypes and display no physical abnormalities. There is no family history of congenital birth defects. The boy has had normal psychomotor development and attends school.
Fluorescence in situ hybridization analysis
Metaphase chromosomes from a lymphoblastoid cell line (LCL) from the patient were used for Fluorescence in situ hybridization (FISH) (Tentler et al. 2003) and mini-FISH analysis as described (Klar et al. 2005; Mansouri et al. 2005). The 17q11.2 specific BAC clones RP11-362P24, RP11-138P22, RP11-192H23, RP11-22N12, RP11-296K13, RP11-82O19, RP11-403E9 were obtained from RZPD-Germany and the 6p21.31 specific PAC clones RP1-368C2, RP3-510O8 and RP3-422H11 were obtained from the Sanger Institute (Roswell Park Cancer Institute). Mini-FISH probes were amplified from the clones RP3-510O8 and RP11-22N12, which span the breakpoints on chromosome 6 and 17, respectively, and with the Advantage 2 PCR kit (Clontech). Primer sequences are available upon request. The PCR products were purified using the GFX PCR DNA and Gel Band Purification Kit (Amersham) and labelled with either digoxigenin-16-dUTP or biotin-16-dUTP (Roche) by nick-translation. After hybridization and washing, the digoxigenin labelled probes were detected by rhodamine labelled anti-digoxigenin antibody and the biotin labelled probes were detected by fluorescein isothiocyanate labelled anti-biotin antibody (Roche). The chromosomes were counterstained with DAPI and anti-fade (Vector labs) and the slides analysed with a Zeiss Axioscope microscope using a cooled CCD camera (Photometrics) and the IPlab software.
Southern blot analysis and cloning of the breakpoints
Refined mapping of the two breakpoint regions was performed by Southern blot analysis. DNA from the patient and controls was prepared from peripheral blood, cleaved with endonucleases EcoRI, BamHI and BglI, separated by agarose gel electrophoresis and transferred to nylon membranes (Amersham). Probes were generated by PCR (primer sequences are available upon request) from the clone RP3-510O8 for chromosome 6 and the clone RP11-22N12 for chromosome 17, respectively.
Amplicons of approximately 3 kb bridging the breakpoints were generated by long-range PCR using chromosome 6 and 17 specific primers. The amplicons were sequenced using a Big Dye Terminator Chemistry (PE Biosystems) and an ABI 3700 DNA analyzer (Applied Biosystems).
Expression analysis and mutation screening
RT–PCR analysis was performed on total RNA from LCLs-derived from the patient and two control individuals using TRIzol solution (Invitrogen). The RNA preparations were analysed for purity using the 2100 Bioanalyzer (Agilent Technologies). The presence of fusion transcripts in the patient was investigated using primers derived from the coding sequences of 182-FIP and LHFPL5, respectively. LCLs from the patient and healthy controls were investigated for the expression of the chromosome 6 genes FKBP5, C6orf81, UNQ3045, CLPS, LHFPL5 and SFRS protein kinase 1 (SRPK1) and the chromosome 17 genes MYO18A, CRYBA1, 182-FIP and TAO kinase 1 (TAOK1) using quantitative real time RT–PCR. Primer sequences are available upon request.
Analysis of the normal expression pattern for the genes LHFPL5, 182-FIP, SRPK1 and TAOK1 was performed by RT–PCR on RNA from the human brain, colon, heart, kidney, liver, lung and placenta purchased from Clontech. β-actin was used as internal control (primer sequences are available upon request).
DNA from ten patients with penoscrotal hypospadias, six patients with AA with or without dysplastic kidneys, four females with cloacal abnormalities and one patient with VACTERL syndrome was collected for mutational analysis. Amplicons of 300–400 nucleotides in size corresponding to the coding sequences and the 5′ and 3′ UTRs of 182-FIP and LHFPL5 transcripts were generated from all 21 DNA samples. Sequencing was performed using BigDye Terminator Chemistry (PE Biosystems) and an ABI 3700 DNA Analyzer (Applied Biosystems).
Results
Mapping of the translocation breakpoints
In order to localize the translocation breakpoints, we performed FISH analysis on metaphase spreads from the patient with genomic clones from chromosomes 6 and 17. The BAC clone RP3-510O8 from the 6p21.31 region hybridized both to the normal chromosome 6 and to the two derivative chromosomes der(6) and der(17). Mini-FISH analysis using the RP3-510O8 derived probe 6mf1 restricted the breakpoint region to within 74 kb (Fig. 1). Refined mapping by Southern blot analysis with several genomic probes from the 74 kb region positioned the breakpoint to a BglI restriction fragment of 2,003 bp on chromosome 6 and within intron 3 of the LHFPL5 gene.
Similarly, the 17q11.2 BAC clone RP11-22N12 hybridized both to the normal chromosome 17 and to the two derivative chromosomes der(6) and der(17) on metaphase spreads from the patient. Mini-FISH experiments showed that the BAC derived probe 17mf4 was translocated to the derivative chromosome 6 and restricted the breakpoint region to be within 21 kb (Fig. 1). Aberrant restriction fragments in patient DNA were observed with the restriction endonucleases EcoRI and BamHI which positioned the breakpoint to a BamHI-BglI restriction fragment of 609 bp within the first intron of the 182-FIP gene.
The detailed mapping allowed us to span both breakpoints by long-range PCR using primers from the two derivative chromosomes. Sequence analysis of the breakpoints revealed a 2 bp deletion on the derivative chromosome 6 and a 7 bp duplication on the derivative chromosome 17 (Fig. 2).
Expression studies and mutation screening
A novel 182-FIP-LHFPL5 fusion transcript consisting of the first exon of 182-FIP and the last exon of LHFPL5 was identified in LCL-derived RNA from the patient but not in controls (Fig. 3a). The transcript has an open reading frame consisting of 123 codons, the first 92 identical to the normal 182-FIP transcript, and the predicted protein has no significant homology to any known functional domains. Quantitative real time RT–PCR performed on LCLs in triplicate measurements revealed significantly reduced levels of the normal 182-FIP transcript in the patient compared to controls (P=9e-8). In contrast, mRNA levels for SRPK1 and TAOK1 were significantly increased in the patient when compared to controls (P=7e-10 and P=2e-94, respectively). The mRNA levels for MYO18A and FKBP5 were equal in the patient and control LCLs (Fig. 3b) whereas, no expression was detected for the genes C6orf81, UNQ3045, CLPS or LHFPL5 in the patient or control derived LCLs.
Expression analysis of genes in the breakpoint regions. a A 182-FIP-LHFPL5 fusion transcript is detected in total RNA derived from a lymphoblastoid cell line from the patient but not in controls. A forward primer was located in exon 1 of the 182-FIP gene and a reverse primer was located in exon 4 of the LHFPL5 gene. b Quantitative real time RT–PCR comparing levels of gene expression to expression levels of β-actin in the patient and controls. Error bars indicate one standard deviation. c The normal expression pattern of the genes LHFPL5, 182-FIP, SRPK1 and TAOK1 determined by tissue specific RT–PCR. The β-actin control is expressed in all tissues
The tissue distribution of LHFPL5, 182-FIP, SRPK1 and TAOK1 transcripts was assessed by tissue specific RT–PCR using RNA derived from the human brain, colon, heart, kidney, liver, lung, and placenta. LHFPL5 expression was detected in the brain and colon, 182-FIP was detected in the brain, colon, kidney, liver, lung and placenta whereas, SRPK1 and TAOK1 were ubiquitously expressed. The β-actin-derived RT–PCR products used as internal control were observed in all samples (Fig. 3c).
Sequence analysis of DNA samples from 21 patients with genital and/or anal malformations identified eight novel silent nucleotide changes in transcript sequences of the 182-FIP and LHFPL5 genes. No coding alterations changing the primary amino acid sequence were detected (Table 1). One of the silent changes was confirmed as a polymorphism in 2/112 control chromosomes. Surprisingly, seven variations were so rare that they could not be identified in any out of 110–116 control chromosomes.
Discussion
Balanced translocations occur at a rate of 1 in 500–2,000 live births and are present in healthy individuals (Baptista et al. 2005; Warburton 1991). However, carriers of de novo balanced translocations have twice the frequency of congenital abnormalities compared to individuals with normal karyotypes. This suggests that there is a causal relationship between translocations and abnormal phenotypes (Warburton 1991). In this study, we have characterized both chromosomal breakpoints from a balanced reciprocal translocation t(6;17)( p21.31;q11.2) associated with hypospadias and AA. Sequence analysis of the breakpoints revealed an almost perfectly balanced translocation with only a small deletion/duplication at the breakpoint sites. Both the breakpoint regions contain polypyrimidine tracts which are associated with chromosomal rearrangements (Abeysinghe et al. 2003). Physical mapping and sequencing allowed us to position the translocation breakpoints within the gene 182-FIP on chromosome 17 and within the LHFPL5 gene on chromosome 6. The 182-FIP gene encodes the 82-kD FMRP Interacting Protein and was recently reported to be associated with polyribosomes as a component of the mRNP complexes containing FMRP. The mRNP complex is associated with actively translating polyribosomes, RNA complexes trafficking in neurites, RNA granules in cytoplasm and, in Drosophila, with the RNAi machinery (Bardoni et al. 2003). The 182-FIP transcript levels in LCL-derived RNA from the patient is reduced to approximately 50% of levels in control samples which confirms the loss of one allele in the patient. It also supports our hypothesis that haploinsufficiency of this gene may contribute to the patient’s phenotype. The 182-FIP transcript is normally expressed in the colon, kidney and placenta, which is consistent with the organs involved in the malformations of our patient. The LHFPL5 gene encodes a protein of yet unknown function with several predicted active domains. Interestingly, one of these domains, Pfam domain PF00822, is also found in claudins which are components of tight junctions. Software analysis predicts four transmembrane motifs at positions 24–46, 97–119, 126–148 and 177–199 which indicates that LHFPL5 is a transmembrane protein. The transcript was detected in RNA from the brain and colon. A mutation in the LHFPL5 mouse ortholog, Lhfpl5, has been reported to cause deafness and vestibular dysfunction in mice (Longo-Guess et al. 2005). In a study by Sebat et al. (2004) looking at large-scale copy number polymorphisms in the human genome, LHFPL5 maps to a region reported to be polymorphic resulting in loss of one gene copy in 10 out of 20 individuals analysed. These observations, in combination with the absence of neurological symptoms in our patient make haploinsufficiency for the LHFPL5 gene unlikely as a mechanism behind the malformation in the patient.
Quantitative real time RT–PCR analysis on mRNA from patient-derived LCLs revealed an increased expression of two genes flanking either breakpoint when compared to control LCLs. The SRPK1 gene, located centromeric of the derivative chromosome 6 breakpoint, showed a two-fold increase in transcript levels. SRPK1 is believed to regulate intracellular localization of splicing factors in the cell cycle (Gui et al. 1994). On chromosome 17, the TAOK1 gene, encoding a serine/threonine protein kinase with an unknown function, located telomeric of the breakpoint was also found to be expressed at significantly higher levels in the patient when compared to controls. The increased expression from SRPK1 and TAOK1 may be due to an altered chromatin structure and/or the separation of the promoter and transcription units from a distant cis-acting regulatory element. Further studies are needed to clarify the potential role of these genes in mammalian development.
RT–PCR analysis of LCL-derived RNA from the patient also revealed the presence of a 182-FIP-LHFPL5 fusion transcript with an open reading frame composed of the first exon of 182-FIP and the last exon of LHFPL5. If translated, this transcript results in the formation of a unique protein consisting of the N-terminus of a normal 182-FIP protein and a C-terminus without similarities to any known protein sequence or known functional domain (http://www.ncbi.nih.gov/Structure/cdd/cdd.shtml). The 182-FIP-LHFPL5 fusion transcript will be regulated by the 182-FIP promoter active in the colon, kidney, liver, brain, lung and placenta. No clinical signs related to the brain, lung or liver were detected in our patient and it is possible that the resulting fusion protein might have a dominant negative effect restricted to certain tissues. The other possible fusion transcript derived from a LHFPL5-182-FIP fusion gene could not be detected in RNA derived from patient LCLs. However, we cannot exclude the existence of such a fusion transcript as it would act under the regulation of the LHFPL5 promoter which is inactive in lymphocytes.
Sequencing analysis of 21 patients with genital and/or anal malformations revealed no mutation altering the codons of the 182-FIP and LHFPL5 genes. Out of the eight silent variations found, one was confirmed as a polymorphism whereas, the rest were excluded in more than 100 control chromosomes and are not yet confirmed as polymorphisms.
Few studies have so far identified candidate genes involved in anorectal and urogenital development. Hori et al. (2001) presented evidence for a susceptibility locus on pig chromosome 15 for a form of AA in pigs which has close similarities with those found in humans. In addition to AA, the pigs also develop a fistula between the anorectum and the urethra in males and a fistula between the anorectum and the vagina in females. In another study, GLI-Kruppel family member GLI2 (GLI2) -/- mutant mice showed imperforate anus and recto-urethral fistula (Kimmel et al. 2000). GLI2 is a sonic hedgehog (Shh) responsive transcription factor. Shh is a secreted signalling protein that plays an important role in various development processes (Kato et al. 2001). In a recent study, expression of the proteins Shh and bone morphogenic protein 4 (Bmp4) was disrupted in both the urinary tract and the hindgut region of mice embryos displaying ARMs when treated by a teratogenic agent. These results indicate that the urinary tract may undergo the same pathological process as seen in the hindgut (Sasaki et al. 2004). Mutations in ephrin-B2 result in severe hypospadias and incomplete or failed cloacal septation indicating a role in midline cell–cell adhesion and fusion events (Dravis et al. 2004). Furthermore, there are several genes implicated in genital malformation syndromes. Mutations in the WT1 gene are associated with urogenital malformations and lack of testosterone 5α-reductase type 2 results in feminization of external male genitalia (Nordenskjold et al. 1999; Pelletier et al. 1991). Partial androgen insensitivity syndromes due to mutations in the androgen receptor may also be associated with hypospadias and urogenital malformations (Sutherland et al. 1996). Recent data suggests that genes necessary for limb development play a role in the formation of the genital tubercle (GT). These genes include members of the fibroblast growth factor (Fgf8 and Fgf10), Shh, Hox (Hoxa-13 Hoxd-13) and the bone morphogenic protein genes Bmp4 and Bmp7 (de Santa Barbara and Roberts 2002; Haraguchi et al. 2001; Haraguchi et al. 2000; Morgan et al. 2003; Mortlock and Innis 1997; Perriton et al. 2002; Podlasek et al. 1997; Stadler 2003; Warot et al. 1997).
In this study, we describe a male patient with congenital urogential and anal malformations associated with a balanced chromosomal rearrangement. We have performed a detailed molecular characterization of this rearrangement and have identified genes and mechanisms behind the aberrant development of the urogenital and anorectal systems. We suggest possible mechanisms for the urogenital malformation in our patient to be haploinsufficiency of the genes 182-FIP and/or LHFPL5, gain of function of the fusion transcript, altered expression of the genes flanking the breakpoints or a combination of the above. Further screening of patients with similar phenotypes for mutations in these genes may reveal additional support for our hypothesis.
Reference
Abeysinghe SS, Chuzhanova N, Krawczak M, Ball EV, Cooper DN (2003) Translocation and gross deletion breakpoints in human inherited disease and cancer I: Nucleotide composition and recombination-associated motifs. Hum Mutat 22:229–44
Baptista J, Prigmore E, Gribble SM, Jacobs PA, Carter NP, Crolla JA (2005) Molecular cytogenetic analyses of breakpoints in apparently balanced reciprocal translocations carried by phenotypically normal individuals. Eur J Hum Genet 13:1205–12
Bardoni B, Castets M, Huot ME, Schenck A, Adinolfi S, Corbin F, Pastore A, Khandjian EW, Mandel JL (2003) 82-FIP, a novel FMRP (fragile X mental retardation protein) interacting protein, shows a cell cycle-dependent intracellular localization. Hum Mol Genet 12:1689–98
Bartsch O, Kuhnle U, Wu LL, Schwinger E, Hinkel GK (1996) Evidence for a critical region for penoscrotal inversion, hypospadias, and imperforate anus within chromosomal region 13q32.2q34. Am J Med Genet 65:218–21
Baskin LS (2000) Hypospadias and urethral development. J Urol 163:951–6
Cho S, Moore SP, Fangman T (2001) One hundred three consecutive patients with anorectal malformations and their associated anomalies. Arch Pediatr Adolesc Med 155:587–91
Christensen K, Madsen CM, Hauge M, Kock K (1990) An epidemiological study of congenital anorectal malformations: 15 Danish birth cohorts followed for 7 years. Paediatr Perinat Epidemiol 4:269–75
de Santa Barbara P, Roberts DJ (2002) Tail gut endoderm and gut/genitourinary/tail development: a new tissue-specific role for Hoxa13. Development 129:551–61
Dravis C, Yokoyama N, Chumley MJ, Cowan CA, Silvany RE, Shay J, Baker LA, Henkemeyer M (2004) Bidirectional signaling mediated by ephrin-B2 and EphB2 controls urorectal development. Dev Biol 271:272–90
Endo M, Hayashi A, Ishihara M, Maie M, Nagasaki A, Nishi T, Saeki M (1999) Analysis of 1,992 patients with anorectal malformations over the past two decades in Japan. Steering Committee of Japanese Study Group of Anorectal Anomalies. J Pediatr Surg 34:435–41
Fredell L, Lichtenstein P, Pedersen NL, Svensson J, Nordenskjold A (1998) Hypospadias is related to birth weight in discordant monozygotic twins. J Urol 160:2197–9
Gallentine ML, Morey AF, Thompson IM, Jr. (2001) Hypospadias: a contemporary epidemiologic assessment. Urology 57:788–90
Gui JF, Lane WS, Fu XD (1994) A serine kinase regulates intracellular localization of splicing factors in the cell cycle. Nature 369:678–82
Haraguchi R, Mo R, Hui C, Motoyama J, Makino S, Shiroishi T, Gaffield W, Yamada G (2001) Unique functions of Sonic hedgehog signaling during external genitalia development. Development 128:4241–50
Haraguchi R, Suzuki K, Murakami R, Sakai M, Kamikawa M, Kengaku M, Sekine K, Kawano H, Kato S, Ueno N, Yamada G (2000) Molecular analysis of external genitalia formation: the role of fibroblast growth factor (Fgf) genes during genital tubercle formation. Development 127:2471–9
Hassink EA, Rieu PN, Hamel BC, Severijnen RS, vd Staak FH, Festen C (1996) Additional congenital defects in anorectal malformations. Eur J Pediatr 155:477–82
Hori T, Giuffra E, Andersson L, Ohkawa H (2001) Mapping loci causing susceptibility to anal atresia in pigs, using a resource pedigree. J Pediatr Surg 36:1370–4
Kato M, Seki N, Sugano S, Hashimoto K, Masuho Y, Muramatsu M, Kaibuchi K, Nakafuku M (2001) Identification of sonic hedgehog-responsive genes using cDNA microarray. Biochem Biophys Res Commun 289:472–8
Kimmel SG, Mo R, Hui CC, Kim PC (2000) New mouse models of congenital anorectal malformations. J Pediatr Surg 35:227–30; discussion 230–1
Klar J, Asling B, Carlsson B, Ulvsback M, Dellsen A, Strom C, Rhedin M, Forslund A, Anneren G, Ludvigsson JF, Dahl N (2005) RAR-related orphan receptor A isoform 1 (RORa1) is disrupted by a balanced translocation t(4;15)(q22.3;q21.3) associated with severe obesity. Eur J Hum Genet 13:928–34
Longo-Guess CM, Gagnon LH, Cook SA, Wu J, Zheng QY, Johnson KR (2005) A missense mutation in the previously undescribed gene Tmhs underlies deafness in hurry-scurry (hscy) mice. Proc Natl Acad Sci USA 102:7894–9
Mansouri MR, Marklund L, Gustavsson P, Davey E, Carlsson B, Larsson C, White I, Gustavson KH, Dahl N (2005) Loss of ZDHHC15 expression in a woman with a balanced translocation t(X;15)(q13.3;cen) and severe mental retardation. Eur J Hum Genet 13:970–7
Martinez-Frias ML (1994) Epidemiological analysis of outcomes of pregnancy in diabetic mothers: identification of the most characteristic and most frequent congenital anomalies. Am J Med Genet 51:108–13
Martinez-Frias ML, Bermejo E, Rodriguez-Pinilla E (2000) Anal atresia, vertebral, genital, and urinary tract anomalies: a primary polytopic developmental field defect identified through an epidemiological analysis of associations. Am J Med Genet 95:169–73
Martinez-Frias ML, Frias JL (1999) VACTERL as primary, polytopic developmental field defects. Am J Med Genet 83:13–6
Morgan EA, Nguyen SB, Scott V, Stadler HS (2003) Loss of Bmp7 and Fgf8 signaling in Hoxa13-mutant mice causes hypospadia. Development 130:3095–109
Mortlock DP, Innis JW (1997) Mutation of HOXA13 in hand-foot-genital syndrome. Nat Genet 15:179–80
Nordenskjold A, Friedman E, Tapper-Persson M, Soderhall C, Leviav A, Svensson J, Anvret M (1999) Screening for mutations in candidate genes for hypospadias. Urol Res 27:49–55
Paulozzi LJ (1999) International trends in rates of hypospadias and cryptorchidism. Environ Health Perspect 107:297–302
Pelletier J, Bruening W, Kashtan CE, Mauer SM, Manivel JC, Striegel JE, Houghton DC, Junien C, Habib R, Fouser L, et al. (1991) Germline mutations in the Wilms’ tumor suppressor gene are associated with abnormal urogenital development in Denys-Drash syndrome. Cell 67:437–47
Perriton CL, Powles N, Chiang C, Maconochie MK, Cohn MJ (2002) Sonic hedgehog signaling from the urethral epithelium controls external genital development. Dev Biol 247:26–46
Podlasek CA, Duboule D, Bushman W (1997) Male accessory sex organ morphogenesis is altered by loss of function of Hoxd-13. Dev Dyn 208:454–65
Rodono A, Romeo MG, Sanges G, Distefano G (1997) [CHARGE association: report of a clinical case with anal atresia and rectovaginal fistula]. Pediatr Med Chir 19:469–71
Sasaki Y, Iwai N, Tsuda T, Kimura O (2004) Sonic hedgehog and bone morphogenetic protein 4 expressions in the hindgut region of murine embryos with anorectal malformations. J Pediatr Surg 39: 170–3; discussion 170–3
Sebat J, Lakshmi B, Troge J, Alexander J, Young J, Lundin P, Maner S, Massa H, Walker M, Chi M, Navin N, Lucito R, Healy J, Hicks J, Ye K, Reiner A, Gilliam TC, Trask B, Patterson N, Zetterberg A, Wigler M (2004) Large-scale copy number polymorphism in the human genome. Science 305:525–8
Seri M, Martucciello G, Paleari L, Bolino A, Priolo M, Salemi G, Forabosco P, Caroli F, Cusano R, Tocco T, Lerone M, Cama A, Torre M, Guys JM, Romeo G, Jasonni V (1999) Exclusion of the Sonic Hedgehog gene as responsible for Currarino syndrome and anorectal malformations with sacral hypodevelopment. Hum Genet 104:108–10
Shaul DB, Harrison EA (1997) Classification of anorectal malformations–initial approach, diagnostic tests, and colostomy. Semin Pediatr Surg 6:187–95
Stadler HS (2003) Modelling genitourinary defects in mice: an emerging genetic and developmental system. Nat Rev Genet 4:478–82
Steinbach P, Rehder H (1987) Tetrasomy for the short arm of chromosome 12 with accessory isochromosome (+i(12p] and a marked LDH-B gene dosage effect. Clin Genet 32:1–4
Sutherland RW, Wiener JS, Hicks JP, Marcelli M, Gonzales ET, Jr., Roth DR, Lamb DJ (1996) Androgen receptor gene mutations are rarely associated with isolated penile hypospadias. J Urol 156:828–31
Takano T, Yamanouchi Y, Mori Y, Kudo S, Nakayama T, Sugiura M, Hashira S, Abe T (1997) Interstitial deletion of chromosome 1q [del(1)(q24q25.3)] identified by fluorescence in situ hybridization and gene dosage analysis of apolipoprotein A-II, coagulation factor V, and antithrombin III. Am J Med Genet 68:207–10
Tentler D, Johannesson T, Johansson M, Rastam M, Gillberg C, Orsmark C, Carlsson B, Wahlstrom J, Dahl N (2003) A candidate region for Asperger syndrome defined by two 17p breakpoints. Eur J Hum Genet 11:189–95
Van Buggenhout G, Trommelen J, Hamel B, Fryns JP (1999) 13q deletion syndrome in an adult mentally retarded patient. Genet Couns 10:177–81
Warburton D (1991) De novo balanced chromosome rearrangements and extra marker chromosomes identified at prenatal diagnosis: clinical significance and distribution of breakpoints. Am J Hum Genet 49:995–1013
Warot X, Fromental-Ramain C, Fraulob V, Chambon P, Dolle P (1997) Gene dosage-dependent effects of the Hoxa-13 and Hoxd-13 mutations on morphogenesis of the terminal parts of the digestive and urogenital tracts. Development 124:4781–91
Zlotogora J, Abu-Dalu K, Lernau O, Sagi M, Voss R, Cohen T (1989) Anorectal malformations and Down syndrome. Am J Med Genet 34:330–1
Acknowledgments
We would like to thank the patient and his family for their contribution to this study. This work was supported by grants from the Swedish Research Council, the Swedish Cancer Society, The Sävstaholm Society, Torsten and Ragnar Söderbergs Fund, the Borgström Foundation and Uppsala University. We would also like to thank Mats Gustafsson, Department of Genetics and Pathology at Uppsala University, for his help with the statistics. The study was approved by the appropriate Swedish review board and an informed consent was obtained.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mansouri, M.R., Carlsson, B., Davey, E. et al. Molecular genetic analysis of a de novo balanced translocation t(6;17)(p21.31;q11.2) associated with hypospadias and anorectal malformation. Hum Genet 119, 162–168 (2006). https://doi.org/10.1007/s00439-005-0122-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-005-0122-9