Abstract
Oculocutaneous albinism (OCA) is a common human genetic condition resulting from mutations in at least twelve different genes. OCA1 results from mutations of the tyrosinase gene and presents with the life-long absence of melanin pigment after birth (OCA1A) or with the development of minimal-to-moderate amounts of cutaneous and ocular pigment (OCA1B). Other types of OCA have variable amounts of cutaneous and ocular pigment. We hypothesized that white hair at birth indicates OCA1 and tested this in a sample of 120 probands with OCA and white hair at birth. We found that 102 (85%) of the probands had OCA1 with one or two identifiable tyrosinase gene mutations, with 169 (83%) of the 204 OCA1 tyrosinase gene alleles having identifiable mutations and 35 (17%) having no identifiable change in the coding, splice junction, or proximal promoter regions of the gene. The inability to identify the mutation was more common with OCA1B (24/35, 69%) than with OCA1A (11/35, 31%) alleles. Seven probands with no tyrosinase gene mutations were found to have OCA2 with one or two P gene mutations, and in eleven, no mutations were detected in either gene. We conclude that (1) the presence of white hair at birth is a useful clinical tool suggesting OCA1 in a child or adult with OCA, although OCA2 may also have this presentation; (2) the molecular analysis of the tyrosinase and P genes are necessary for precise diagnosis; and (3) the presence of alleles without identifiable mutations of the tyrosinase gene, particularly in OCA1B, suggests that more complex mutation mechanisms of this gene are common in OCA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human oculocutaneous albinism (OCA) is a common phenotype for a group of recessive genetic disorders of melanin synthesis (King et al. 2001a, 2001b). Mutations in at least twelve genes are responsible for this phenotype, and it is likely that more will be discovered (King et al. 2001a; Shotelersuk et al. 2000; Newton et al. 2001; Anikster et al. 2001; Huizing et al. 2001a; Zhang et al. 2003; Li et al. 2003). The OCA-related genes produce dissimilar products, but mutations in all result in a reduction of melanin synthesis by the melanocyte. The common types of OCA have cutaneous and ocular hypopigmentation without significant involvement of other tissue, whereas less common types such as Hermansky-Pudlak syndrome and Chediak-Higashi syndrome have more complex manifestations (Shotelersuk and Gahl 1998; Introne et al. 1999; Huizing et al. 2001a).
All forms of albinism have, by definition, hypopigmentation of the eye associated with a poorly formed fovea and with abnormal neural connections between the retina and the brain (King et al. 2001a). In OCA, the skin and hair are also hypopigmented, but the degree of pigment reduction is variable. Attempts to define different types of OCA clinically by the amount and color of the melanin present in the hair and skin have been useful but have not succeeded in elucidating the genetic basis for each type; indeed, it has become apparent the characterization of OCA types should be based on the genetic locus involved.
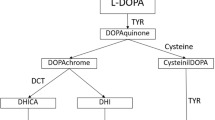
Oculocutaneous albinism type 1 (OCA1, OMIM 203100) is produced by mutations in the tyrosinase gene on chromosome 11q (Tomita et al. 1989; Spritz et al. 1990; Oetting and King 1999). Mutations in this gene produce the classic picture of life-long white hair and skin, and blue eyes with translucent irides, a phenotype that has been described in most ethnic groups worldwide and recognized throughout human history (Pearson et al. 1911). This form is known as OCA1A and results from tyrosinase gene mutations that produce no enzyme (Schnur et al. 1996) or inactive enzyme (Tripathi et al. 1992; Halaban et al. 2000; Toyofuku et al. 2001). Many individuals with OCA1 do not have this phenotype, however, but rather have variable amounts of hair and skin pigment (King et al. 1991; Giebel et al. 1991a, 1991b; Matsunaga et al. 1999; Passmore et al. 1999). This form is known as OCA1B, and the phenotype can vary from minimal to nearly normal cutaneous and hair pigment in adult life and can overlap with the phenotypes resulting from mutations in other OCA-related genes. We now report our analysis of the tyrosinase gene in a large group of individuals who meet clinical criteria proposed for OCA1, in order (1) to determine whether accurate clinical criteria for tyrosinase-related OCA can be developed, and (2) to characterize the associated mutations.
Materials and methods
Subjects
Families were obtained through the International Albinism Center at the University of Minnesota or through self and physician referral. A clinical information form was available concerning most affected family members detailing hair, skin, and eye color at birth and at the age of sample submission. All families were fully consenting through a human subjects-approved protocol. DNA was obtained from peripheral blood mononuclear cells by using standard methods (Oetting et al. 1991b).
Clinical criteria for OCA1
The following criteria were used to select individuals with OCA1: ocular features of albinism with white hair and skin, and blue translucent irides at birth. OCA1A was defined as the presence of white hair and skin throughout life. The irides remained blue but became less translucent with age. Sun exposure produced erythema but no tan, and nevi were pink and amelanotic. OCA1B was defined as the presence, at birth, of white scalp hair that subsequently developed pigment in the first decade of life, and eyelash hair that developed darker pigment than the scalp or eyebrow hair. The irides remained blue or developed tan or brown pigment. The skin remained white or developed generalized pigment and tanned with sun exposure, and pigmented freckles and nevi may have developed.
Mutation analysis of the tyrosinase gene
The sequence of the tyrosinase gene was determined in DNA from members of each family by using established methods in our laboratory. This analysis included each of the five exons, the exon:intron boundaries, and 100–200 bp of the adjacent intron, 500 bp of the 5' promoter region, and 90 bp of the 3' untranslanted region. DNA from both parents was analyzed to confirm the origin of each mutation.
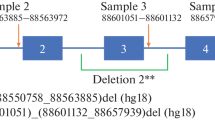
Mutation analysis of the P gene
Mutations of the P gene on chromosome 15q result in OCA2 (Gardner et al. 1992; Rinchik et al. 1993). The sequence of the P gene was determined in DNA from probands who were found to have no detectable mutations of the tyrosinase gene. In brief, the entire coding region and part of the flanking intron sequences for each of the 24 exons were individually amplified by using the polymerase chain reaction (PCR) with the primers listed in Table 1 (Saiki et al. 1988). The amplified product was directly sequenced by using the dideoxy method of Sanger with automated fluorescent DNA sequencing (LiCor). DNA from both parents was analyzed to confirm the origin of each mutation.
Results
Evaluation of clinical criteria
One hundred and twenty probands from the International Albinism Center met the proposed criteria of OCA1 and were selected for this analysis. They included 74 classified as OCA1A and 46 classified as OCA1B, based on examination of hair color for probands seen at the International Albinism Center in Minnesota or on the report of hair color for samples that were submitted for analysis from other locations; the majority of samples from other locations were accompanied by a photograph of the proband. Probands with yellow, blond, red, or brown scalp hair at birth were classified as OCA2 and were not included in this analysis. Only one proband per family was included when multiple siblings were affected. The clinical characteristics of each proband are given in Table 2. All heterozygous parents were normally pigmented and did not have any ocular features associated with albinism.
Our first goal was to determine whether the clinical criteria as proposed could be used to identify an individual with OCA1. The overall results of the mutation analysis are shown in Fig. 1. In our sample of 120, two tyrosinase gene mutations were identified in 67 individuals (56%), one tyrosinase gene mutation was identified in 35 (29%), and no tyrosinase gene mutations were identified in 18 (15%) by using the standard methods described. The finding of 35 probands who were heterozygous for a tyrosinase gene mutation was significantly greater (P<0.001) than the one to two affected individuals that would be expected for a recessive condition with a prevalence of 1/40,000 (King et al. 2001a), indicating that these probands most likely have OCA1 rather than some other type of OCA. Thus, the clinical criteria of albinism with white hair at birth had a positive predictive value of 85% (102 of 120) for OCA1.
The phenotypic range in pigmentation for selected probands with OCA1A and OCA1B is shown in Fig. 2. Scalp hair color varied from white in OCA1A (Cases 1, 9, 34, 36, and 45) to very light yellow blond (Cases 76, 82, and 86) to golden blond (Cases 95, 98, 107, and 110). Three OCA1B probands had brown or auburn hair (Cases 78, 83, and 100). For most OCA1B probands, the eyelash hair was darker than the scalp hair, and some had the ability to develop a tan following sun exposure (Table 2, Fig. 3). Eyebrow hair color was the same or lighter than eyelash or scalp hair color.
Photographs of 12 OCA1 probands. Case numbers from Table 2 are given bottom left for each proband
Distribution and type of tyrosinase gene mutations
We analyzed the distribution and type of the mutations found in the 102 probands with OCA1. As shown in Table 3, we identified two mutations in 53 (83%) of the 64 probands who met the criteria of OCA1A and one of the two mutations in 11 (17%). For the 38 probands who met the clinical criteria of OCA1B, we identified two mutations in 14 (37%) and one of the two mutations in 24 (63%). For the 53 OCA1A probands with two identifiable mutations, eight (15%) were homozygous for a single mutation, and 45 (85%) were compound heterozygous with different maternal and paternal mutations (Table 3). For the 14 OCA1B probands with two identifiable mutations, 2 (14%) were homozygous for a single mutation, and 12 (86%) were compound heterozgotes. For the entire sample of OCA1 probands, 10/102 (10%) were homozygous for a single mutation; consanguinity was reported in only one family.
A total of 66 tyrosinase gene mutations were identified: 45 missense, five nonsense, three single base insertions, 10 deletions of one, two, or ten bases, and three that altered intronic consensus splice sequences (Table 4). Of the 66, 27 have previously been published (Albinism Database). Most of the mutations (44/66, 67%) were identified in only one proband. Recurrent mutations included G47D, P81L, P205T, R217Q, C275F, T373 K, D383 N, R278X, 1467insT, and IVS2–7t→a, with the most common being T373 K [found on 27 of 169 (16%) alleles that contained an identifiable mutation]. The mutations were distributed primarily in exons 1–4 of the gene, and a few were found in exon 5.
Mutations causing OCA1B
Twenty-six mutations were identified in OCA1B probands, but 14 of these were also present in OCA1A, indicating that they were most likely null mutations that encoded no protein or a protein with no catalytic activity. The distribution of the 12 remaining mutations that were found only in OCA1B probands is shown in Table 5. In seven of these cases, the second mutation was not identified and it was not possible to determine whether those that were identified were hypomorphic or null mutations without performing an expression analysis. The mutations W39X, G346X, 53delG, and 731delGT, however, were expected to be null mutations, because they would produce a truncated protein, with the homologous allele carrying the hypomorphic mutation. Two novel mutations, P81S and R422 W, were likely to be hypomorphic because they were found in compound heterozygous probands who had a null mutation on the homologous allele. The IVS2+2 t→g change was also likely to be a hypomorphic mutation as it was found with G47D in one proband; G47D has previously been associated with the OCA1A phenotype (Oetting et al. 1991a, 1992; Gershoni-Baruch et al. 1994) and with a known OCA1B intron 2 mutation (Gershoni-Baruch et al. 1994;Spritz 1993; Matsunaga et al. 1999).
The D383 N mutation was also likely to be a very low-activity hypomorphic mutation. Three Norwegian probands were homozygous for this mutation. All were born with white hair that turned very light yellow blond in the first year of life in two (Cases 81 and 86) or remained unchanged at 5 months of age in the third (Case 22). This mutation was also found in a heterozygous dose in six probands with OCA1A and one with OCA1B. For the six OCA1A probands, two had known null mutations (N371T, 649delC) on the homologous allele, two had novel mutations (G253E, R212 K) on the homologous allele, and two had no detectable mutations on the homologous allele. For the OCA1B proband, the homologous chromosome had no detectable mutation. These results suggest that the D383 N mutation is associated with very little enzyme activity so that hair pigment is seen only when present in a homozygous dose or with another hypomorphic mutation.
Analysis of P gene
The P gene was analyzed to determine whether the 18 probands who had no identifiable tyrosinase gene mutation had OCA2 rather than OCA1. Four of the ten probands classified as OCA1A had mutations in the P gene, including one (Case 69) who was a compound heterozygote for two mutations (Table 6). Three of the eight probands classified as OCA1B had mutations in the P gene, including two (Cases 113 and 120) who were compound heterozygous for two mutations (Table 6). Thus, seven of 18 probands (39%) who presented with the ocular features of albinism and white hair at birth had OCA2.
Discussion
The clinical recognition of oculocutaneous albinism is usually obvious because of the cutaneous hypopigmentation associated with the presence of nystagmus, foveal hypoplasia with little retinal melanin pigment, reduced visual acuity, and strabismus. There are several types of oculocutaneous albinism, however, resulting from mutations of different genes, and their clinical separation can be difficult or impossible (King et al. 2001a). Indeed, the separation of ocular and oculocutaneous albinism in a Northern European male can also be difficult, because it is not always possible to differentiate between pathologic cutaneous hypopigmentation and constitutional light pigmentation. Criteria that could aid in the definition of a particular type of OCA would be helpful in accurate genetic counseling for a family and in understanding the future expectations for the affected individual.
Based on our previous work, we hypothesized that individuals with OCA1 could be identified clinically by having white scalp hair at birth, whereas individuals with other types of OCA are born with some melanin pigment in their scalp hair. Using this approach, we correctly identified 85% (102/120) of our probands with OCA1 (positive predictive value = 0.85). The percentage may indeed be higher if some of the probands with no identifiable mutations are eventually found to have tyrosinase gene mutations that involve other parts of the gene. Although not perfect, this observation provides a reasonable clinical tool that can be used in the initial evaluation of a patient with OCA.
One important issue in this study is the characterization of "white" hair. In a family with light constitutional pigmentation, white hair may truly be white, whereas hair in a family with darker constitutional pigmentation may be called white because it is much lighter than any other hair color in the family, even though it contains some melanin and might be classified by others as light blond or yellow rather than white. A good example of the way in which the perception of white varies can be seen when attempting to choose a "white" paint, as the choices are many. We conclude that there is a range of "white" hair representing various degrees of extreme hypopigmentation. This is important because of the finding that seven probands who had white hair at birth were eventually found to have mutations of the P gene. It is possible that mutations in the P gene could produce OCA associated with no melanin synthesis, but this has not been described in most studies that include clinical detail (Gardner et al. 1992; Puri et al. 1997; Newton et al. 2001; Rinchik et al. 1993; Lee et al. 1994a, 1994b; Passmore 1999). Passmore and co-workers (1999), in an analysis of the tyrosinase and the P genes in DNA from 79 German probands with OCA, identified two siblings who had "snow white" hair, no mutations of the tyrosinase gene, and a heterozygous novel P gene missense mutation, I617L. If this is truly OCA2 resulting from mutations of the P gene, then the phenotypic range for this type of albinism must also extend to white hair at birth.
We identified 35 probands who had only one detectable mutation of the tyrosinase gene; others have reported similar findings (Giebel et al. 1991b; Tripathi et al. 1993; Gershoni-Baruch et al. 1994; Spritz et al. 1997; Passmore et al. 1999). They could, by chance, be heterozygous for a tyrosinase gene mutation, whereas their albinism actually results from mutations in another gene, but the expected general population heterozygote frequency of 1/100 for tyrosinase gene mutations makes this explanation unlikely. They could also be heterozygous for a mutation in the tyrosinase gene and also in another pigment gene, with the combination of two heterozygous mutations producing the albinism, although there is no evidence to support this mechanism in the development of albinism. Heterozygosity at two loci has been reported to influence coat color but not to produce marked hypopigmentation and albinism in the mouse (Silvers 1979). This may be a better explanation for normal variations in human pigmentation. Our conclusion is that the probands with only one identifiable tyrosinase gene mutations have OCA1.
There are several possible mechanisms for the missing mutations of the tyrosinase gene that we could not identify on the second allele (cryptic or hidden mutations). First, a mutation may be present in a regulatory region of the gene that is not sequenced by using our current methods. A locus control region of the murine tyrosinase gene has been identified and is a potential location for a mutation (Porter et al. 1991; Montoliu et al. 1996). Mutations in a locus control region are usually hypomorphic in function and reduce, but do not eliminate, gene transcription (Li et al. 1999); this type of mutation in the tyrosinase gene would most likely be associated with OCA1B rather than OCA1A. Second, a deletion of the entire tyrosinase gene has been identified in one family and could be the mechanism for one or more of the mutations that we could not identify on OCA1 alleles (Schnur et al. 1996). Our analysis by direct sequencing of genomic DNA would not have recognized a deletion mutation on one allele. This is not a likely mechanism, however, because the probands with only one identifiable mutation were heterozygous for these mutations, and the expected base was identified on the homologous allele. This would be missing if a deletion were present. Our approach also identified the missense polymorphisms, Y192S and R402Q, and a polymorphism at −301; non-Mendelian segregation of these polymorphisms in our families was not identified. Finally, a mutation in an intron that altered the normal splicing pattern of the RNA or an intronic regulatory region of the gene would not have been detected by our methods. Studies are being carried out in our laboratory to identify mutation mechanisms that affect the tyrosinase gene in OCA1 but that are not detected by standard sequencing techniques.
We found three Norwegian probands who were homozygous for the D383 N mutation, although consanguinity was not known to be present in these families, suggesting that this may be a Norwegian founder mutation. Other probands who were compound heterozygous with this change as one of their mutations, however, were Northern European but not specifically Norwegian, indicating that this mutation may be found in other populations and may not represent a specific Norwegian mutation. No specific ethnic distribution pattern was found with the other identified mutations in our study.
Do the probands in this study with P gene mutations have OCA2? The three who were compound heterozygous for two mutations clearly have this type of OCA. The possible mechanisms for the albinism in the four individuals with one identified P gene mutation are similar to those with only one identifiable tyrosinase gene mutation. They could, by chance, be heterozygous for a P gene mutation, but their OCA is actually the result of mutations at another gene. As with the tyrosinase gene, this seems unlikely, since the heterozygote frequency in the general population is estimated to be 1 in 95 (~1%), based on a frequency of OCA2 of 1 in 36,000 in the Caucasian population (King et al. 2001b). The finding of four heterozygous probands in a sample of 18 is greater than expected. Furthermore, the P gene has many polymorphic sequence variants, and the probands with only one identifiable P gene mutation show no evidence for deletions in other parts of the gene. We conclude that these probands have OCA2, and that their second mutation cannot be detected by standard sequence techniques of the coding region.
None of the probands in our study had a history of bleeding or bruising, although many were young and had not had sufficient time to challenge their clotting system. Hermansky-Pudlak syndrome (HPS) is an infrequent type of oculocutaneous albinism associated with storage pool deficient platelets and the accumulation of ceroid in tissues (Hazelwood et al. 1997; Shotelersuk et al. 1998, 2000; Gahl et al. 1998; Shotelersuk and Gahl 1998; Huizing et al. 2001a, 2001b; Anikster et al. 2001; White et al. 1973; Witkop et al. 1987; Zhang et al. 2003; Li et al. 2003). Affected individuals have a remarkably broad pigmentation phenotype, including those who appear to have very light blond or white hair (Shotelersuk et al. 1998; Gahl et al. 1998). We do not routinely evaluate new OCA individuals and families for HPS and cannot determine whether any of the probands without detectable mutations had HPS.
The clinical categorization of an individual with OCA has become more complex. Clinical pigmentation patterns are useful, as demonstrated here, and are sufficiently precise for initial diagnosis, prognosis, and family counseling. Accurate diagnosis is only possible with gene analysis. HPS can usually be determined by electron-microscopic analysis of platelet dense bodies, as their absence is critical in making this diagnosis (Witkop et al. 1987). For most individual and family counseling, molecular analyses are usually not necessary because all known OCA types are recessive in inheritance. Ongoing ophthalmologic care is the most crucial for an individual with albinism, and this care is similar for all OCA types. Our study documents the utility of a careful birth and developmental history of pigmentation in providing an initial clinical diagnosis of an individual with OCA.
References
Anikster Y, Huizing M, White J, Shevchenko YO, Fitzpatrick DL, Touchman JW, Compton JG, Bale SJ, Swank RT, Gahl WA, Toro JR (2001) Mutation of a new gene causes a unique form of Hermansky-Pudlak syndrome in a genetic isolate of central Puerto Rico. Nat Genet 28:376–380
Gahl WA, Brantly M, Kaiser-Kupfer MI, Iwata F, Hazelwood S, Shotelersuk V, Duffy LF, Kuehl EM, Troendle J, Bernardini I (1998) Genetic defects and clinical characteristics of patients with a form of oculocutaneous albinism (Hermansky-Pudlak syndrome). N Engl J Med 338:1258–1264
Gardner JM, Nakatsu Y, Gondo Y, Lee S, Lyon MF, King RA, Brilliant MH (1992) The mouse pink-eyed dilution gene: association with human Prader-Willi and Angelman syndromes. Science 257:1121–1124
Gershoni-Baruch R, Rosenmann A, Droetto S, Holmes S, Tripathi RK, Spritz RA (1994) Mutations of the tyrosinase gene in patients with oculocutaneous albinism from various ethnic groups in Israel. Am J Hum Genet 54:586–594
Giebel LB, Tripathi RK, King RA, Spritz RA (1991a) A tyrosinase gene missense mutation in temperature-sensitive type I oculocutaneous albinism. J Clin Invest 87:1119–1122
Giebel LB, Tripathi RK, Strunk KM, Hanifin JM, Jackson CE, King RA, Spritz RA (1991b) Tyrosinase gene mutations associated with type IB ("yellow") oculocutaneous albinism. Am J Hum Genet 48:1159–1167
Halaban R, Svedine S, Cheng E, Smicun Y, Aron R, Hebert DN (2000) Endoplasmic reticulum retention is a common defect associated with tyrosinase-negative albinism. Proc Natl Acad Sci USA 97:5889–5894
Hazelwood S, Shotelersuk V, Wildenberg SC, Chen D, Iwata F, Kaiser-Kupfer MI, White JG, King RA, Gahl WA (1997) Evidence for locus heterogeneity in Puerto Ricans with Hermansky-Pudlak syndrome. Am J Hum Genet 61:1088–1094
Huizing M, Anikster Y, Fitzpatrick DL, Jeong AB, D'Souza M, Rausche M, Toro JR, Kaiser-Kupfer MI, White JG, Gahl WA (2001a) Hermansky-pudlak syndrome type 3 in Ashkenazi Jews and other non-Puerto Rican patients with hypopigmentation and platelet storage-pool deficiency. Am J Hum Genet 69:1022–1032
Huizing M, Anikster Y, Gahl WA (2001b) Hermansky-Pudlak syndrome and Chediak-Higashi syndrome: disorders of vesicle formation and trafficking. Thromb Haemost 86:233–245
Introne W, Boissy RE, Gahl WA (1999) Clinical, molecular, and cell biological aspects of Chediak-Higashi syndrome. Mol Genet Metab 68:283–303
King RA, Townsend D, Oetting WS, Summers CG, Olds DP, White JG, Spritz RA (1991) Temperature-sensitive tyrosinase associated with peripheral pigmentation in oculocutaneous albinism. J Clin Invest 87:1046–1053
King RA, Hearing VJ, Creel DJ, Oetting WS (2001a) Albinism. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic and molecular bases of inherited disease, 8th edn. McGraw-Hill, New York, pp 5587–5627
King RA, Oetting WS, Summers CG, Creel DJ, Hearing V (2001b) Abnormalities of pigmentation. In: Rimoin DL, Connor JM, Pyeritz RE, Korf BR (eds) Emery and Rimoin's principles and practice of medical genetics, 4th edn. Harcourt, London
Lee S-T, Nicholls RD, Bundey S, Laxova R, Musarella M, Spritz RA (1994a) Mutations of the P gene in oculocutaneous albinism, ocular albinism, and Prader-Willi syndrome plus albinism. N Engl J Med 330:529–534
Lee S-T, Nicholls RD, Schnur RE, Guida LC, Lu-Kuo J, Spinner NB, Zackai EH, Spritz RA (1994b) Diverse mutations of the P gene among African-Americans with type II (tyrosinase-positive) oculocutaneous albinism (OCA2). Hum Mol Genet 3:2047–2051
Li W, Zhang Q, Oiso N, Novak EK, Gautam R, O'Brien EP, Tinsley CL, Blake DJ, Spritz RA, Copeland NG, Jenkins NA, Amato D, Roe BA, Starcevic M, Dell'Angelica EC, Elliott RW, Mishra V, Kingsmore SF, Paylor RE, Swank RT (2003) Hermansky-Pudlak syndrome type 7 (HPS-7) results from mutant dysbindin, a member of the biogenesis of lysosome-related organelles complex 1 (BLOC-1). Nat Genet 35:84–89
Li Q, Harju S, Peterson KR (1999) Locus control regions: coming of age at a decade plus. Trends Genet 15:403–408
Matsunaga J, Dakeishi-Hara M, Tanita M, Nindl M, Nagata Y, Nakamura E, Miyamura Y, Kikuchi K, Furue M, Tomita Y (1999) A splicing mutation of the tyrosinase gene causes yellow oculocutaneous albinism in a Japanese patient with a pigmented phenotype. Dermatology 199:124–129
Montoliu L, Umland T, Schütz G (1996) A locus control region at −12 kb of the tyrosinase gene. EMBO J 15:6026–6034
Newton JM, Cohen-Barak O, Hagiwara N, Gardner JM, Davisson MT, King RA, Brilliant MH (2001) Mutations in the human orthologue of the mouse underwhite gene (uw) underlie a new form of oculocutaneous albinism, OCA4. Am J Hum Genet 69:981–988
Oetting WS, King RA (1999) Molecular basis of albinism: mutations and polymorphisms of pigment genes associated with albinism. Hum Mutat 13:99–115
Oetting WS, Handoko HY, Mentink MM, Paller AS, White JG, King RA (1991a) Molecular analysis of an extended family with type IA (tyrosinase-negative) oculocutaneous albinism. J Invest Dermatol 97:15–19
Oetting WS, Mentink MM, Summers CG, Lewis RA, White JG, King RA (1991b) Three different frameshift mutations of the tyrosinase gene in type IA oculocutaneous albinism. Am J Hum Genet 49:199–206
Oetting WS, Witkop CJ, Brown S, Colomer R, Fryer JP, Bloom KE, King RA (1992) A frequent mutation in the tyrosinase gene associated with type I-A (tyrosinase-negative) oculocutaneous albinism in Puerto Rico. Am J Hum Genet 50:1-10
Passmore LA, Kaesmann-Kellner B, Weber BH (1999) Novel and recurrent mutations in the tyrosinase gene and the P gene in the German albino population. Hum Genet 105:200–210
Pearson K, Nettleship E, Usher CH (1911) A monograph on albinism in man: Drapers' Company Research Memoirs, Biometric Series VI. Dulau, London
Porter S, Larue L, Mintz B (1991) Mosaicism of tyrosinase-locus transcription and chromatin structure in dark vs light melanocyte clones of homozygous chincilla-mottled mice. Dev Genet 12:393–402
Puri N, Durham-Pierre D, Aquaron R, Lund PM, King RA, Brilliant MH (1997) Type 2 oculocutaneous albinism (OCA2) in Zimbabwe and Cameroon: distribution of the 2.7-kb deletion allele of the P gene. Hum Genet 100:651–656
Rinchik EM, Bultman SJ, Horsthemke B, Lee S, Stunk KM, Spritz RA, Avidano KM, Jong MTC, Nicholls RD (1993) A gene for the mouse pink-eyed dilution locus and for human type II oculocutaneous albinism. Nature 361:72–76
Saiki RK, Gelfand DH, Stoffel S, Scharf SJ, Higuchi R, Horn GT, Mullis KB, Erlich HA (1988) Primer-directed enzymatic amplification of DNA with a thermostable DNA polymerase. Science 239:487–491
Schnur RE, Selling BT, Holmes SA, Wick PA, Tatsumura YO, Spritz RA (1996) Type I oculocutaneous albinism associated with a full-length deletion of the tyrosinase gene. J Invest Dermatol 106:1137–1140
Shotelersuk V, Gahl WA (1998) Hermansky-Pudlak syndrome: models for intracellular vesicle formation. Mol Genet Metab 65:85–96
Shotelersuk V, Hazelwood S, Larson D, Iwata F, Kaiser-Kupfer MI, Kuehl E, Bernardini I, Gahl WA (1998) Three new mutations in a gene causing Hermansky-Pudlak syndrome: clinical correlations. Mol Genet Metab 64:99–107
Shotelersuk V, Dell'Angelica EC, Hartnell L, Bonifacino JS, Gahl WA (2000) A new variant of Hermansky-Pudlak syndrome due to mutations in a gene responsible for vesicle formation. Am J Med 108:423–427
Silvers WK (1979) The coat colors of mice. A model for mammalian gene action and interaction. Springer, Berlin Heidelberg New York
Spritz RA (1993) Molecular genetics of oculocutaneous albinism. Semin Dermatol 12:167–172
Spritz RA, Strunk KM, Giebel LB, King RA (1990) Detection of mutations in the tyrosinase gene in a patient with Type IA oculocutaneous albinism. N Engl J Med 322:1724–1728
Spritz RA, Oh J, Fukai K, Holmes SA, Ho L, Chitayat D, France TD, Musarella MA, Orlow SJ, Schnur RE, Weleber RG, Levin AV (1997) Novel mutations of the tyrosinase (TYR) gene in type 1 oculocutaneous albinism (OCA1). Hum Mutat 10:171–174
Tomita Y, Takeda A, Okinaga S, Tagami H, Shibahara S (1989) Human oculocutaneous albinism caused by a single base insertion in the tyrosinase gene. Biochem Biophys Res Commun 164:990–996
Toyofuku K, Wada I, Spritz RA, Hearing VJ (2001) The molecular basis of oculocutaneous albinism type 1 (OCA1): sorting failure and degradation of mutant tyrosinases results in a lack of pigmentation. Biochem J 355:259–269
Tripathi RK, Hearing VJ, Urabe K, Aroca P, Spritz RA (1992) Mutational mapping of the catalytic activities of human tyrosinase. J Biol Chem 267:23707–23712
Tripathi RK, Bundey S, Musarella MA, Droetto S, Strunk KM, Holmes SA, Spritz RA (1993) Mutations of the tyrosinase gene in Indo-Pakistani patients with Type I (tyrosinase-deficient) oculocutaneous albinism (OCA). Am J Hum Genet 53:1173–1179
White JG, Witkop CJ, Gerritsen SM (1973) The Hermansky-Pudlak syndrome: ultrastructure of bone marrow macrophages. Am J Pathol 70:329–344
Witkop CJ, Krumwiede M, Sedano H, White JG (1987) The reliability of absent platelet dense bodies as a diagnostic criterion for Hermansky-Pudlak syndrome. Am J Hematol 26:305–300
Zhang Q, Zhao B, Li W, Oiso N, Novak RK, Rusiniak ME, Gautam R, Chintala S, O'Brien EP, Zhang Y, Roe BA, Elliott RW, Eicher EM, Liang P, Kratz C, Legius E, Spritz RA, O'Sullivan TN, Copeland NG, Jenkins NASRT (2003) Ru2 and Ru encode mouse orthologs of the genes mutated in human Hermansky-Pudlak syndrome types 5 and 6. Nat Genet 33:145–153
Acknowledgements
The authors thank the wonderful families who have participated in this research and the many physicians who have referred the families to the International Albinism Center. This research was supported in part by United States Public Health grant AR44649 and by the Bernard and Mary Ellen Black family.
Author information
Authors and Affiliations
Corresponding author
Additional information
Electronic database Information: accession numbers and URLs for data presented in this article are as follows:
Albinism Database, http://www.cbc.umn.edu/tad, for a list of published mutations of the tyrosinase gene
Online Mendelian Inheritance in Man (OMIM), http://www.ncbi.nlm.nih.gov/Omim/, for OCA1 (MIM 203100), OCA2 (MIM 203200)
Rights and permissions
About this article
Cite this article
King, R.A., Pietsch, J., Fryer, J.P. et al. Tyrosinase gene mutations in oculocutaneous albinism 1 (OCA1): definition of the phenotype. Hum Genet 113, 502–513 (2003). https://doi.org/10.1007/s00439-003-0998-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-003-0998-1