Abstract
Apolipoprotein B (apoB) is the sole protein component of low-density lipoprotein (LDL) and is thought to play an important role in atherogenesis. We performed a meta-analysis of the associations between the three most frequently investigated polymorphisms (XbaI, signal peptide insertion/deletion, EcoRI) in the apolipoprotein B (APOB) gene, lipid parameters, and the risk of ischemic heart disease (IHD). We restricted our analysis to Caucasians. Homozygotes for the XbaI X+ allele had significantly elevated levels of LDL cholesterol (LDL-C) and apoB, but a decreased risk (OR=0.80; 95%CI: 0.66–0.96) of IHD. Homozygosity for the signal peptide deletion allele was associated with similarly increased levels of LDL-C and apoB, and with an increased risk of IHD (OR=1.30; 95%CI: 1.08–1.58). Subjects homozygous for the rare EcoRI allele had significantly decreased levels of total and LDL cholesterol, but unaltered risk of IHD. We conclude that all three polymorphic apoB sites are associated with altered lipid levels, but not necessarily with a consistently altered risk of IHD. These data suggest that the relationship between apoB levels, hypercholesterolemia and IHD risk cannot have a simple molecular basis in the apoB gene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevated plasma levels of low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of coronary artery disease (Castelli et al. 1986). Apolipoprotein B (apoB) is the sole protein component of this particle, and plasma levels of apoB are also associated with cardiovascular disease. Indeed, evidence is accumulating that apoB may be a better risk indicator for cardiovascular events than LDL-C (Sniderman et al. 2003). In a large survey of 175,553 subjects, the apoB concentration was associated with the risk of fatal myocardial infarction, even after adjustment for total cholesterol (Walldius et al. 2001). LDL-C levels are less predictive of cardiovascular events in patients treated with statin therapy. Hence, apoB-guidance of statin treatment may more accurately predict the effect on cardiovascular risk (Miremadi et al. 2002; Sniderman et al. 2003)
Several mechanisms may explain the role of apoB in atherogenesis. ApoB serves as the ligand for LDL-receptor mediated clearance of LDL. Mutations in the APOB gene cause a rare dominant disorder, familial defective apolipoprotein B-100, which is characterized by elevated LDL-C levels and an increased risk of ischemic heart disease (IHD). These rare genetic variants cannot explain the variation of apoB in the general population. Less penetrant but more prevalent variants could have a much larger population-attributable effect. As a consequence, a plethora of studies have assessed a wide variety of APOB polymorphisms with inconsistent results, possibly because of the lack of adequate statistical power, selection bias, population diversity, or genetic admixture (Ioannidis et al. 2001). A meta-analysis may avoid some of these methodological difficulties. Therefore, we have performed a systematic meta-analysis of population-based studies investigating APOB polymorphisms and their association with either lipid parameters or the risk of IHD.
Materials and methods
Nomenclature
Gene symbols used in this article follow the recommendations of the HUGO Gene Nomenclature Committee (Povey et al. 2001).
Literature search
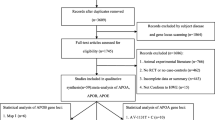
We identified all population-based studies of APOB polymorphisms and their association with lipid parameters and the risk of IHD. The literature was scanned by a formal search of the MEDLINE electronic database. Search terms that were used were both MESH terms and (part of) the text words "acute coronary syndromes", or "myocardial infarction", or "coronary artery disease", or "ischemic heart disease", in combination with "apolipoprotein B", in combination with "polymorphism", or "mutation", or "genetics". The search results were subsequently limited to "human" and "English language". Reference lists of retrieved articles were scanned for additional potentially relevant publications. In addition, for each retrieved publication an electronic "cited reference search" was performed (Web of Science version 4.1.1, Institute for Scientific Information 2000, http://www.isinet.com/isi/products/citation/wos/), identifying all papers citing the index publication.
We checked whether all generated data described in the Methods section were reported in the Results section of each paper. If obtained data were not shown in the article, the principal investigator was contacted and asked to provide the data. Authors were also contacted in case of a potential patient overlap between publications.
Selection criteria
We aimed to reduce publication bias by contacting investigators to request unpublished data. Because it was virtually impossible to obtain unpublished data from studies published more than 10 years ago, we restricted our analysis to articles published after 1992. Extension of this period to before 1992 would result in the inclusion of many studies with incomplete data (data not available digitally, only in old digital format, investigator moved, retired, etc.) and would thus introduce publication bias. Only full-length articles in peer review journals were included if published between 1992 and January 2002. We limited our analysis to the three most extensively studied APOB polymorphisms, i.e., the XbaI, signal peptide insertion/deletion, and EcoRI polymorphisms. Moreover, we restricted our analysis to studies performed in Caucasian populations, because genotype distributions may differ substantially between different ethnicities (Peters and Boekholdt 2002). If ethnicity was not explicitly reported, studies were also included if they were performed on European and Australian populations. Data on subjects from other countries were excluded, as were data from articles in which ethnicity and the country were not reported.
Studies were included if (1) they reported the prevalence of one of these polymorphisms in at least one group of patients with IHD and in an appropriate group of population-based controls without cardiovascular disease and representative for the population from which the cases were recruited, or (2) they reported data on both an APOB polymorphism and a lipid parameter in a sample of unrelated individuals. We limited our analysis to the following four plasma lipid parameters: total cholesterol (TC), triglycerides, LDL-C, and apoB. IHD was defined as (1) myocardial infarction, (2) unstable angina, (3) stable angina, or (4) angiographic evidence of coronary artery disease. Data on subjects with lipid disorders or on subjects specifically selected by lipid criteria were not used. Duplicate publications and publications with patient overlap were excluded. All identified publications were independently evaluated and selected by two investigators (S.M.B. and K.F.) for compliance with these criteria. The results were compared and disagreements were resolved by consensus. Considerable inconsistency exists concerning the nomenclature of the polymorphisms and alleles. The nomenclature used in this article is presented in Table 1.
Data extraction and analysis
Data were independently extracted and entered into separate databases by two investigators (S.M.B. and K.F.). The results were compared and disagreements were resolved by consensus.
All populations described in case-control studies were tested for Hardy-Weinberg equilibrium in cases and controls, and the genotype distributions between all groups were compared by χ2 statistics. The relationships between genotype and outcome (either lipid parameter or risk of IHD) were analyzed with meta-analysis. Rare allele homozygotes were compared against wild-type homozygotes, in order to obtain maximal contrast. We did not consider a dominant model (comparing mutant homozygotes + heterozygotes versus wild-type individuals). Thus, heterozygotes were not taken into account in these meta-analyses. For lipid parameters, weighted mean differences (WMD) with corresponding 95% confidence intervals (95% CI) were calculated (Hedges and Olkin 1985). For dichotomous data on disease status, odds ratios (OR) with their corresponding 95% CI were calculated by using the fixed effects model according to Peto and Mantel-Haenszel (see Greenland and Rothman 1998). The raw data from each separately described population were entered as a separate stratum. Tests for heterogeneity were performed with each meta-analysis. Data were analyzed by using Review Manager version 4.1 (The Cochrane Collaboration 2000, http://www.cochrane.org).
Results
Literature search
A total of 143 potentially relevant publications were identified. Of these, 45 were excluded because they were published before 1992. Twenty-one studies were excluded because the populations were non-Caucasian, or because the ethnicity of subjects could not be determined. Thirty-six publications were excluded because they had patient overlap with other publications, because patients were derived from a limited number of families, because they reported data affected by an intervention, because the reported data were not relevant for our analysis, or because subjects were selected on the basis of abnormal cholesterol levels (references available). One additional study selected patients on the basis of abnormal cholesterol levels but did provide potentially relevant data on the control group (Delghandi et al. 1999).
The remaining 40 publications reported potentially relevant data. Eleven of these provided a complete report of all data that were determined in the study (Benes et al. 2000b; Aalto-Setala et al. 1998; Bohn et al. 1994; Gardemann et al. 1998; Louhija et al. 1994; Miettinen et al. 1994; Pajukanta et al. 1996; Salazar et al. 2000; Vilella et al. 1992; Visvikis et al. 1993; Wick et al. 1995). For the remaining 29 publications, the principal investigator was requested to provide data that were not shown in the article, and for 13 of these publications, additional data were provided (Abbey et al. 1995; Benes et al. 2000a; Bohn et al. 1993; Corbo et al. 1997; Delghandi et al. 1999; Hixson et al. 1992; Iso et al. 1996; Lopez-Miranda et al. 1997, 2000; Marshall et al. 1994; Moreel et al. 1992; Turner et al. 1995; Ukkola et al. 1993).
For the remaining 16 publications, the principal investigator could not be contacted, the requested data could not be retrieved, or permission from the local Medical Ethics Committee could not be obtained (references available). From these 16 publications, seven provided no otherwise relevant data, whereas from the remaining nine publications, the incomplete set of reported data was used (Deeb et al. 1992; Gaffney et al. 1993; Glisic et al. 1997; Hansen et al. 1993; Hosking et al. 1992; Machado et al. 2001; Nieminen et al. 1992; Peacock et al. 1992; Pouliot et al. 1994; Series et al. 1993) Thus, data from a total of 33 studies were used. The characteristics of these studies are summarized in Tables 2 and 3.
Genotype and allele distributions
The total population, which was analyzed for the XbaI polymorphism, was not in Hardy-Weinberg equilibrium, and this was attributed completely by the IHD cases (χ2=6.786, df=1, P=0.009), whereas all other populations and groups of cases and controls were in Hardy-Weinberg equilibrium (χ2<1.8, df=1, P>0.18). The XbaI genotypes distribution differed significantly between cases and controls (χ2=9.915, df=2, P=0.007). This was caused by a significantly lower XbaI X+ allele frequency among the cases with IHD (0.462 versus 0.494; χ2=8.522, df=1, P=0.004) that was mainly the result of a lower proportion of XbaI X+ homozygotes among the cases (0.198 versus 0.237; χ2=8.930, df=1, P=0.003). In the individual studies, no indications were found that cases and controls had different inclusion criteria with regards to (LDL) cholesterol and apoB levels. Moreover, a selection bias was very unlikely because XbaI had an unexpected inverse relation with IHD (vide infra). The genotype (χ2<3.1, df=2, P>0.2) and allele frequencies (χ2<3.1, df=1, P>0.08) of the other two polymorphisms were not significantly different between cases and controls.
Homozygous genotypes and lipid parameters
Compared with wild-type (X−X−) individuals, XbaI X+ homozygotes had significantly higher TC and LDL-C levels: 0.15 mmol/l (95% CI=0.09–0.22; P<0.0001) and 0.15 mmol/l (95% CI=0.09–0.20; P<0.0001), respectively (Table 4). The apoB levels were higher in X+ homozygotes, than in wild-type individuals (0.06 g/l; 95% CI=0.04–0.08; P<0.0001).
Homozygosity for the signal peptide deletion allele was associated with elevated TC levels (0.12 mmol/l; 95% CI=0.06–0.18; p<0.0001) and LDL-C levels (0.09 mmol/l; 95% CI=0.03–0.13; p=0.002), compared to wild-type (insertion allele) individuals. ApoB levels were indeed higher in deletion allele homozygotes (0.07 g/l; 95% CI=0.04–0.09; p<0.0001).
Homozygosity for the rare EcoRI E− allele was associated with decreased levels of total cholesterol (0.40 mmol/l; 95% CI=0.23–0.56; P<0.0001) and LDL-C (0.18 mmol/l; 95% CI=0.02–0.35; P=0.03), compared with wild-type E+E+ individuals. The apoB levels were not associated with the E− allele in a recessive model. The triglyceride levels were not significantly associated with homozygosity for any of the three polymorphic sites.
Genotype and IHD
In addition to the comparison of genotype distributions (rare allele homozygotes, heterozygotes, common allele homozygotes) between IHD cases and controls, we quantified the risk of IHD associated with homozygosity for the rare allele, as compared with homozygosity for the common allele. Homozygosity for the XbaI X+ allele was associated with a reduced risk of IHD (OR=0.80; 95% CI=0.66–0.96; P=0.02; Fig. 1). An analysis restricted to populations whose lipid profiles were available showed similar results (data not shown). Homozygosity for the signal peptide deletion allele was associated with an increased risk of IHD (OR=1.30; 95% CI=1.08–1.58; P=0.007; Fig. 2). The EcoRI polymorphism was not significantly associated with IHD (OR=1.15; 95% CI=0.78–1.70; P=0.5; Fig. 3).
Odds ratios for individual studies and pooled odds ratios for the outcome ischemic heart disease in X+X+ homozygotes compared with X−X− homozygotes as the reference group. Thus, heterozygotes are not taken into account in this model. Point estimates and corresponding 95% CIs, and the absolute number of individuals are presented for individual studies, and for a pooled analysis. Square size is proportional to number of observations
Odds ratios for individual studies and pooled odds ratios for the outcome ischemic heart disease in deletion homozygotes compared with insertion homozygotes as the reference group. Thus, heterozygotes are not taken into account in this model. Point estimates and corresponding 95% CIs, and the absolute number of individuals are presented for individual studies, and for a pooled analysis. Square size is proportional to number of observations
Odds ratios for individual studies and pooled odds ratios for the outcome ischemic heart disease in E−E− homozygotes compared with E+E+ homozygotes as the reference group. Thus, heterozygotes are not taken into account in this model. Point estimates and corresponding 95% CIs, and the absolute number of individuals are presented for individual studies, and for a pooled analysis. Square size is proportional to number of observations
Discussion
In the present meta-analysis, variation at the APOB gene locus exerted differential effects on LDL-C and apoB levels and on IHD risk. In the general population, high levels of apoB lead to an increased risk of IHD (Walldius et al. 2001), and in patients on statin therapy, apoB levels have recently been proposed as a more accurate therapy guidant than LDL-C (Miremadi et al. 2002; Sniderman et al. 2003) The findings of the present study suggest that these relationships may not have a simple molecular basis in the APOB gene.
The XbaI X+ allele was significantly associated with higher LDL-C and apoB levels. Strikingly, the XbaI X+ allele was also associated with a significantly decreased risk of IHD. ApoB acts as ligand for LDL-receptor-mediated uptake of LDL in the liver. Among patients with a mutated LDL receptor, large variation has been observed in the severity of hypercholesterolemia (Sijbrands et al. 2001). The clinical consequences of mutated LDL receptors depend on interactions with unknown additional risk factors (Sijbrands et al. 2000). However, disorders of apoB itself could change the atherogenic properties of LDL without an influence on such additional factors. The inverse associations of the polymorphic XbaI site with hypercholesterolemia and IHD risk could be explained by structural changes of apoB that concomitantly cause hypercholesterolemia and modify LDL toward a less atherogenic particle. ApoB has arginines positioned in the carboxy terminal part of the protein; this results in a receptor-binding site at amino acid residues 3359–3369 (Boren et al. 2001). An interaction between arginine and tryptophan is essential for the correct refolding of apoB during hydrolysis of very low density lipoproteins (VLDL) to LDL. The absence of an arginine leads to reduced affinity for the LDL receptor and may also change the refolding of apoB during the intravascular remodeling of VLDL to LDL (Boren et al. 2001). Alternatively, a structural disorder may affect the interaction site of apoB with proteoglycans of the extracellular matrix (Skalen et al. 2002). Theoretically, such structural changes of apoB could result in accumulation of less atherogenic LDL in the circulation. The polymorphic XbaI site is located in exon 26 and does not cause an amino acid substitution. Therefore, the observed associations probably result from co-segregation with one or more functional variants in the APOB gene or a gene located nearby. Such linkage disequilibrium might exist with variants that affect the LDL-receptor-binding region of apoB and refolding of the protein (Dunning et al. 1993; Umans-Eckenhausen et al. 2002).
The signal peptide deletion allele of apoB is also associated with hypercholesterolemia and with an increased risk of IHD. This deletion allele results in an absence of three amino acids, which could lead to diminished hydrophobicity of the signal peptide, and this could improve the translocation of apoB from the cytoplasm leading to an increased secretion rate of apoB-containing lipoproteins (Randall and Hardy 1989). To our knowledge, a comparison of LDL properties between XbaI X+ homozygotes and deletion allele homozygotes has not been performed.
Despite a significant and relatively large LDL-C-lowering effect of the EcoRI polymorphism, no effect on the risk of IHD was observed. The EcoRI polymorphism predicts a Glu-Lys substitution in exon 29 of the APOB gene. This mutation may alter the tertiary structure of apoB, thereby affecting the interaction with the LDL receptor.
Design and limitations
Several issues have to be taken into account when interpreting the present meta-analysis. A major weakness of any meta-analysis is publication bias, which results from not publishing "non-significant" data (Ioannidis et al. 2001). An ideal meta-analysis should contain all data from positive and negative studies, but this is impossible because many investigators of unpublished studies remain anonymous, have moved or retired, or are unwilling or unable to provide unpublished data.(Campbell et al. 2002). Because this is particularly true for older studies, we restricted our analysis to the last 10 years. The strength of our analysis lies in the fact that we collected a substantial amount of unpublished data from this recent time span. Consequently, our findings clearly do not incorporate a trend toward selection of positive findings. More importantly, it results in analyses that are not influenced by calendar time, which can have a strong influence on the relationship between genotype and disease (Sijbrands et al. 2001). For example, a finding in a large pedigree with hypercholesterolemia suggests that meta-analyses into the relationship between genotypes and chronic disease should be adjusted for calendar time or should be restricted to present-day patients. Another problem relating to meta-analysis in general is the use of different outcome definitions in the individual studies. However, the methods were identical within each individual study included here, and therefore the inconsistencies could not have introduced an important systematic bias. Moreover, some of the discrepancies between individual studies could be caused by differences in ethnic background or lifestyle, and therefore we restricted our analyses to Caucasian populations. Finally, a particular difficulty may have been introduced by the fact that that we analyzed the relationship between APOB genotypes and intermediate traits (LDL-C and apoB) and the risk of IHD. Such a line of investigation suggests analyses of a causal pathway, but these intermediate traits and clinical endpoints were in part analyzed in different studies. However, similar results were obtained in additional analyses restricted to studies that provided information on lipids and IHD.
Interpretation
The three most frequently analyzed polymorphisms in the APOB gene had differential effects on lipid profile and IHD risk. Hypercholesterolemia associated with polymorphisms in the APOB gene does not necessarily lead to an increased risk of IHD. Future research is needed to assess whether or not the specific polymorphisms influence the atherogenic properties of the LDL particles. Moreover, the effect should be analyzed regarding linkage disequilibria between the polymorphisms. Nonetheless, we conclude that only the signal peptide deletion allele contributes to an increased risk of IHD that is associated with hypercholesterolemia and high apoB levels. However, the findings from the other two frequent polymorphisms (XbaI and EcoRI) emphasize that the relationship between IHD and hypercholesterolemia and high apoB levels in the general population is complex and involves more than variation in the APOB gene.
References
Aalto-Setala K, Palomaki H, Miettinen H, Vuorio A, Kuusi T, Raininko, Salonen O, Kaste M, Kontula K (1998) Genetic risk factors and ischaemic cerebrovascular disease: role of common variation of the genes encoding apolipoproteins and angiotensin-converting enzyme. Ann Med 30:224–233
Abbey M, Hirata F, Chen GZ, Ross R, Noakes M, Belling B, Clifton P, Nestel PJ (1995) Restriction fragment length polymorphism of the apolipoprotein B gene and response to dietary fat and cholesterol. Can J Cardiol 11 (Suppl G):79G–85G
Benes P, Muzik J, Benedik J, Elbl L, Znojil V, Vacha J (2000a) Apolipoprotein B signal peptide polymorphism in relation to lipids and diabetes in male CAD patients. Atherosclerosis 152:257–258
Benes P, Muzik J, Benedik J, Frelich M, Elbl L, Vasku A, Znojil V, Vacha J (2000b) Single effects of apolipoprotein B, (a), and E polymorphisms and interaction between plasminogen activator inhibitor-1 and apolipoprotein(a) genotypes and the risk of coronary artery disease in Czech male caucasians. Mol Genet Metab 69:137–143
Bohn M, Bakken A, Erikssen J, Berg K (1993) XbaI polymorphism in DNA at the apolipoprotein B locus is associated with myocardial infarction (MI). Clin Genet 44:241–248
Bohn M, Bakken A, Erikssen J, Berg K (1994) The apolipoprotein B signal peptide insertion/deletion polymorphism is not associated with myocardial infarction in Norway. Clin Genet 45:255–259
Boren J, Ekstrom U, Agren B, Nilsson-Ehle P, Innerarity TL (2001) The molecular mechanism for the genetic disorder familial defective apolipoprotein B100. J Biol Chem 276:9214–9218
Campbell EG, Clarridge BR, Gokhale M, Birenbaum L, Hilgartner S, Holtzman NA, Blumenthal D (2002) Data withholding in academic genetics. Evidence from a national survey. JAMA 287:473–480
Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousdian S, Kannel WB (1986) Incidence of coronary heart disease and lipoprotein cholesterol levels. JAMA 256:2835–2838
Corbo RM, Vilardo T, Mantuano E, Ruggeri M, Gemma AT, Scacchi R (1997) Apolipoproteins B and E, and angiotensin I-converting enzyme (ACE) genetic polymorphisms in Italian women with coronary artery disease (CAD) and their relationships with plasma lipid and apolipoprotein levels. Clin Genet 52:77–82
Deeb SS, Failor RA, Brown BG, Brunzell JD, Albers JJ, Motulsky AG, Wijsman E (1992) Association of apolipoprotein B gene variants with plasma apoB and low density lipoprotein (LDL) cholesterol levels. Hum Genet 88:463–470
Delghandi M, Thangarajah R, Nilsen M, Grimsgaard S, Bonaa KH, Tonstad S, Jorgensen L (1999) DNA polymorphisms of the apolipoprotein B gene (XbaI, EcoRI, and MspI RFLPs) in Norwegians at risk of atherosclerosis and healthy controls. Acta Cardiol 54:215–225
Dunning AM, Renges HH, Hamsten A, Talmud P, Humphries S (1993) A postulated phylogenetic tree for the human apolipoprotein B gene: unpredicted haplotypes are associated with elevated apo B levels. Biochim Biophys Acta 1165:271–278
Gaffney D, Freeman DJ, Shepherd J, Packard CJ (1993) The ins/del polymorphism in the signal peptide of apolipoprotein B has no effect on lipid parameters. Clin Chim Acta 218:131–138
Gardemann A, Ohly D, Fink M, Katz N, Tillmanns H, Hehrlein FW, Haberbosch W (1998) Association of the insertion/deletion gene polymorphism of the apolipoprotein B signal peptide with myocardial infarction. Atherosclerosis 141:167–175
Glisic S, Prljic J, Radovanovic N, Alavantic D (1997) Study of apoB gene signal peptide insertion/deletion polymorphism in a healthy Serbian population: no association with serum lipid levels. Clin Chim Acta 263:57–65
Greenland S, Rothman KJ (1998) Introduction to stratified analysis. In: Williams A, Wilkins B (eds) Modern epidemiology. Lippincott, Philadelphia, pp 253–279
Hansen PS, Gerdes LU, Klausen IC, Gregersen N, Faergeman O (1993) Polymorphisms in the apolipoprotein B-100 gene contributes to normal variation in plasma lipids in 464 Danish men born in 1948. Hum Genet 91:45–50
Hedges LV, Olkin I (1985) Statistical methods for meta-analysis. Academic Press, San Diego
Hixson JE, McMahan CA, McGill HC Jr, Strong JP (1992) Apo B insertion/deletion polymorphisms are associated with atherosclerosis in young black but not young white males. Arterioscler Thromb 12:1023–1029
Hosking JL, Bais R, Sobecki SK, Tallis GA, Bradley J, Thomas DW (1992) Lipid parameters and apolipoprotein B RFLP studies: comparison of normal and coronary heart disease groups as defined by angiography. Clin Biochem 25:303–308
Ioannidis JPA, Ntzani EE, Trikalinos TA, Contopoulos-Ioannidis DG (2001) Replication validity of genetic association studies. Nat Genet 29:306–309
Iso H, Harada S, Shimamoto T, Folsom AR, Koike K, Sato S, Iida M, Komachi Y (1996) Polymorphism of the apolipoprotein B gene and blood lipid concentrations in Japanese and Caucasian population samples. Atherosclerosis 126:233–241
Lopez-Miranda J, Ordovas JM, Ostos MA, Marin C, Jansen S, Salas J, Blanco-Molina A, Jimenez-Pereperez JA, Lopez-Segura F, Perez-Jimenez F (1997) Dietary fat clearance in normal subjects is modulated by genetic variation at the apolipoprotein B gene locus. Arterioscler Thromb Vasc Biol 17:1765–1773
Lopez-Miranda J, Marin C, Castro P, Gomez P, Gonzalez-Amieva A, Paz E, Bravo D, Ordovas JM, Jimenez-Pereperez J, Perez-Jimenez F (2000) The effect of apolipoprotein B XbaI polymorphism on plasma lipid response to dietary fat. Eur J Clin Invest 30:678–684
Louhija J, Miettienen HE, Kontula K, Tikkanen MJ, Miettinen TA, Tilvis RS (1994) Aging and genetic variation of plasma apolipoproteinns. Arterioscler Thromb 14:1084–1089
Machado MO, Hirata MH, Bertolami MC, Hirata RDC (2001) Apo B gene haplotype is associated with lipid profile of higher risk for coronary heart disease in Caucasian Brazilian men. J Clin Lab Anal 15:19–24
Marshall HW, Morrison LC, Wu LL, Anderson JL, Corneli PS, Stauffer, DM, Allen A, Karagounis LA, Ward RH (1994) Apolipoprotein polymorphisms fail to define risk of coronary artery disease. Results of a prospective, angiographically controlled study. Circulation 89:567–577
Miettinen HE, Korpela K, Hamalainen L, Kontula K (1994) Polymorphisms of the apolipoprotein and angiotensin converting enzyme genes in young North Karelian patients with coronary heart disease. Hum Genet 94:189–192
Miremadi S, Sniderman A, Frohlich J (2002) Can measurement of serum apolipoprotein B replace the lipid profile monitoring of patients with lipoprotein disorders? Clin Chem 48:484–488
Moreel JF, Roizes G, Evans AE, Arveiler D, Cambou JP, Souriau C, Parra HJ, Desmarais E, Fruchart JC, Ducimetiere P, Cambien F (1992) The polymorphism ApoB/4311 in patients with myocardial infarction and controls: the ECTIM Study. Hum Genet 89:169–175
Nieminen MS, Mattila KJ, Aalto-Setala K, Kuusi T, Kontula K, Kauppinen-Makelin R, Ehnholm C, Jauhiainen M, Valle M, Taskinen MR (1992) Lipoproteins and their genetic variation in subjects with and without angiographically verified coronary artery disease. Arterioscler Thromb 12:58–69
Pajukanta PE, Valsta LM, Aro A, Pietinen P, Helio T, Tikkanen MJ (1996) The effects of the apolipoprotein B signal peptide (ins/del) and XbaI polymorphisms on plasma lipid responses to dietary challenge. Atherosclerosis 122:1–10
Peacock R, Dunning A, Hamsten A, Tornvall P, Humphries S, Talmud P (1992) Apolipoprotein B gene polymorphisms, lipoproteins and coronary atherosclerosis: a study of young myocardial infarction survivors and healthy population-based individuals. Atherosclerosis 92:151–164
Peters RJ, Boekholdt SM (2002) Gene polymorphisms and the risk of myocardial infarction—an emerging relation. N Engl J Med 347:1963–1965
Pouliot MC, Despres JP, Dionne FT, Vohl MC, Moorjani S, Prud'homme D, Bouchard C, Lupien PJ (1994) Apo B-100 gene EcoRI polymorphism. Realtions to plasma lipoprotein changes associated with abdominal visceral obesity. Arterioscler Thromb 14:527–533
Povey S, Lovering R, Bruford E, Wright M, Lush M, Wain H (2001) The HUGO Gene Nomenclature Committee (HGNC). Hum Genet 109:678–680
Randall LL, Hardy SJ (1989) Unity in functions in the absence of consensus in sequence: role of leader peptides in export. Science 243:1156-1159
Salazar LA, Hirata MH, Giannini SD, Forti N, Diament J, Lima TM, Hirata RDC (2000) Seven DNA polymorphisms at the candidate genes of atherosclerosis in Brazilian women with angiographically documented coronary artery disease. Clin Chim Acta 300:139–149
Series JJ, Gaffney D, Packard CJ, Shepherd J (1993) Frequency of the XbaI, EcoRI, PvuII and MspI polymorphisms of the apolipoprotein B gene in relation to hypercholesterolaemia in the general population. Clin Chim Acta 215:89–98
Sijbrands EJ, Westendorp R, Lombardi P, Havekes L, Frants A, Kastelein JJ, Smelt AH (2000) Additional risk factors influence excess mortality in heterozygous familial hypercholesterolaemia. Atherosclerosis 149:421–425
Sijbrands EJ, Westendorp RG, Defesche JC, Meier PH de, Smelt AH, Kastelein JJ (2001) Mortality over two centuries in large pedigree with familial hypercholesterolaemia: family tree mortality study. BMJ 822:1019–1023
Skalen K, Gustafsson M, Rydberg EK, Hulten LM, Wiklund O, Innerarity TL, Boren J (2002) Subendothelial retention of atherogenic lipoproteins in early atherosclerosis. Nature 417:750–754
Sniderman AD, Furberg CD, Keech A, Roeters van Lennep JE, Frohlich J, Jungner I, Walldius G (2003) Apolipoproteins versus lipids as indices of coronary risk and as targets for statin treatment. Lancet 361:777–780
Turner PR, Talmud PJ, Visvikis S, Ehnholm C, Tiret L (1995) DNA polymorphisms of the apoprotein B gene are associated with altered plasma lipoprotein concentrations but not with perceived risk of cardiovascular disease: European Atherosclerosis Research Study. Atherosclerosis 116:221–234
Ukkola O, Savolainen MJ, Salmela PI, Xyz DK von, Kesaniemi YA (1993) Apolipoprotein B gene DNA polymorphisms are associated with macro- and microangiopathy in non-insulin-dependent diabetes mellitus. Clin Genet 44:177–184
Umans-Eckenhausen MA, Sijbrands EJ, Kastelein JJ, Defesche JC (2002) Low-density lipoprotein receptor gene mutations and cardiovascular risk in a large genetic cascade screening population. Circulation 106:3031–3036
Vilella E, Balanya J, Masana L, Marsal S, La Ville AE, Turner PR (1992) Low density lipoprotein ligand-receptor interactions in normal healthy individuals characterized by their XbaI apolipoprotein B DNA polymorphism. Atherosclerosis 93:145–153
Visvikis S, Cambou JP, Arveiler D, Evans AE, Parra HJ, Aguillon D, Fruchart JC, Siest G, Cambien F (1993) Apolipoprotein B signal peptide polymorphism in patients with myocardial infarction and controls. "The ECTIM study". Hum Genet 90:561–565
Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E (2001) High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet 358:2026–2033
Wick U, Witt E, Engel W (1995) Restriction fragment length polymorphisms at the apoprotein genes AI, CIII and B-100 and in the 5' flanking region of the insulin gene as possible markers of coronary heart disease. Clin Genet 47:184–190
Acknowledgements
The authors gratefully acknowledge all authors who provided additional unpublished information regarding publications included in this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boekholdt, S.M., Peters, R.J.G., Fountoulaki, K. et al. Molecular variation at the apolipoprotein B gene locus in relation to lipids and cardiovascular disease: a systematic meta-analysis. Hum Genet 113, 417–425 (2003). https://doi.org/10.1007/s00439-003-0988-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-003-0988-3