Abstract
Praziquantel (PZQ) is recommended by the WHO as the first line in treatment of schistosomiasis. Unfortunately, it exhibits low oral bioavailability which can compromise its efficacy. Nanostructures showed promising potential to overcome this problem. Accordingly, the aim of this study was to investigate the effect of niosomal encapsulation of PZQ on its activity on Schistosoma mansoni in vitro and in vivo. PZQ was encapsulated in niosomal formulation comprising span 60, cholesterol with peceol being included as absorption enhancer. The in vitro work determined the schistosomicidal activity and morphological changes after incubation with drug solution or PZQ-niosomes. The in vivo study utilized infected mice which received PZQ orally as solution or as niosomes. The activity was assessed by monitoring egg and worm count in addition to histopathological and immunohistochemical studies. The in vitro studies revealed that niosomes alone caused a 30% death of adult parasites and caused completely coiled body, destruction, and peeling of tubercles and spines, with flattening and effacement of gynecophoric canal, blebbing with niosomes vesicles attached to it. Niosomes containing PZQ at a concentration of 0.001 μg/ml increased the death from 30 to 50% with the corresponding PZQ solution causing only 10% death. The in vivo study reflected of niosome-PZQ over PZQ solution as indicated from significant reduction of adult worm count, hepatic and intestinal egg depositions, hepatic granuloma size, and numbers, with marked reduction of vascular endothelial growth factor expression. The study introduced niosomes as promising carriers for enhanced activity of PZQ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schistosomiasis is an endemic disease which is widely distributed with high potential rate in many countries like Africa, Asia, and South America (Angaye 2016). World Health Organization (WHO) considers this disease as a major problem affecting the quality of life of patients with subsequent economic burden on governments (WHO 2016). Development of hepatic periportal fibrosis is one of the most frequent morbid complications of schistosomiasis mansoni (Ahmad and Ahmad 2015). The treatment of this disease relies mainly on chemotherapy which is prescribed with the goal of achieving complete cure or at least reducing the incidence of morbidity. Optimum can also reduce the spreading of infection in endemic area (Inagaki et al. 2003).
The drug of choice for treatment of schistosomiasis is praziquantel (PZQ). This drug is believed to be safe with a broad spectrum of activity (Robert et al. 2017). Unfortunately, PZQ suffers from poor and variable bioavailability after oral administration. This is mainly attributed to poor dissolution of the drug which is the rate-limiting step in its absorption. In addition, PZQ is subject for extensive hepatic metabolism which limits the amount of drug reaching the systemic circulation (Olliaro et al. 2014). This requires an increase in the dose to achieve the therapeutic blood level which results in increased incidence of side effects. Moreover, PZQ is subject to development of resistance which is aggravated by increasing the dose (Bruno et al. 2015).
Accordingly, alternative strategies have been employed to improve the bioavailability of PZQ. These include concurrent administration with drugs like cimetidine (Castro et al. 2000). Enhancement of dissolution rate by inclusion complex formation with β-cyclodextrin is another strategy (El-Arini and Leuenberger 1998; Becket et al. 1999). Simple solid dispersion technique was also used with polyvinylpyrrolidone being employed as the hydrophilic polymer (El-Lakkany et al. 2012a). The use of colloidal drug delivery systems has attracted much interest in the recent years. Colloidal carriers included solid nanoparticulate drug delivery systems such as lipid nanoparticles (SLN) (Xie et al. 2010; de Souza et al. 2014), nanostructured lipid particles which are similar to SLN but contain liquid component to increase drug entrapment efficiency (Kolenyak-Santos et al. 2015), and biodegradable polymeric nanoparticles (de Campos et al. 2001).
These systems are promising candidates for enhancing the bioavailability of drugs like PZQ but suffer from poor physical stability and difficulty of scaling up to the production phase. Fluid colloidal nanostructures provide another promising alternative. These include thermosensitive nanoemulsion and self-emulsifying drug delivery systems (Cong et al. 2017). Liposomes which are vesicular carriers showed promising results in the delivery of PZQ (Frezza et al. 2013). To reduce the cost and increase the stability of vesicular systems, niosomes have been used as substitutes for liposomes. Recently, peceol, a membrane fluidizer, was included in niosome structure with the resulting niosomes being claimed to enhance the oral bioavailability of poorly water-soluble drugs. These vesicles were able to widen the absorption window of acidic drugs. The mechanism of enhanced bioavailability of these niosomes is believed to be due to membrane fluidization and possible lymphatic delivery (Sultan et al. 2016, 2018). In addition, niosomes are capable of entrapping lipophilic drugs with a possibility to invade the membrane of bacteria (Abdelaziz et al. 2015). These characteristics may be extrapolated to parasites but requires verification. Accordingly, the objective of this work was to investigate peceol containing niosomes as a carrier for PZQ (niosomal-PZQ) in treatment of experimental Schistosoma mansoni infection. This was assessed both in vitro and in vivo.
Material and methods
Praziquantel (PZQ) powder was obtained from Egyptian International Pharmaceutical Industry Company (EIPICO), Cairo, Egypt. Peceol was obtained from Gattefosse, Saint-Priest Cedex, France. Span 60 was procured from Sigma Chemical Company, St. Louis, MO, USA. Cholesterol and ethanol were purchased from El-Nasr Pharmaceutical Chemicals Company, Cairo, Egypt.
Preparation of niosomal PZQ
The composition of niosomes is presented in Table 1. Niosomes was prepared according to the well-established technique (Abdelaziz et al. 2015; Sultan et al. 2016). Span 60, cholesterol, peceol, and PZQ were dispersed in ethanol, and the mixture was warmed to 65 ± 1 °C to produce clear liquid. Water (1.5 ml) was added while mixing on the water bath until clarity. This mixture produces proniosome gel upon cooling with continuous mixing. The proniosomal gel was gradually diluted with the rest of water while mixing to yield homogenous niosomal dispersion. The niosomal dispersion was allowed to hydrate and swell by storing at 25 °C for 12 h. The prepared vesicles were subjected to a size reduction operation by bath sonication for 30 min.
In vitro studies
Culture of Adult S. mansoni worms
Egyptian strain of S. mansoni adult worms was recovered from hamsters previously infected with 350 cercariae by perfusion of their livers and mesenteric veins (Smithers and Terry 1965). The worms were washed in Roswell Park Memorial Institute 1640 (RPMI 1640) culture medium (Invitrogen, Carlsbad, California, USA). The medium was supplemented with l-glutamine and antibiotics (20 ml of 20% bovine fetal serum (Gibco) containing 100 U/ml penicillin and 100 mg/ml streptomycin (Invitrogen) and 1.6 μg/ml gentamycin) (Fahmy et al. 2009). After washing, three to six worms (males and females) were transferred to each well of a 24-well culture plate (TPP, St. Louis, MO) containing 2 ml of the same medium and incubated at 37 °C in a humid atmosphere containing 5% CO2 prior to use. All the steps were performed under a sterilized laminar flow chamber (Yousif et al. 2012).
Drug application
Praziquantel (20 μg/ml) was prepared as a solution in dimethyl sulfoxide (DMSO) or encapsulated in niosomes. These were used as stock solutions which were further diluted with either sterile water or plain niosomes, respectively, to obtain working standards containing 20, 10, 4, 2, 1, 0.2, and 0.02 μg/ml. Aliquots of these working solutions were transferred to the wells of the 24 well plate before being diluted with the culture medium to final concentrations of 1, 0.5, 0.2, 0.1, 0.01, 0.05, and 0.001 μg/ml. Adult worms (3–6) were loaded into these wells. Negative control wells contained adults incubated with 1% DMSO or drug-free niosomes plus the culture media that were prepared. The treated worms were incubated at 37 °C in a humid atmosphere containing 5% CO2 for 24 h before examination. All experiments were performed in duplicates.
Treated worms were monitored for motility (worm’s motor activity changes) and mortality rate using an inverted optical microscope (Olympus CK2). Worms which did not show motility for 1 min associated with worm deformity such as blackening, twisting, and contracting were considered dead. Changes in the motor activity (motility) of schistosomes were assessed qualitatively, and their motor activity reduction was defined as slight (slowly moving) or significant (moving the suckers only with loss of motor activity) (Moraes et al. 2013). The effect of the treatment was also assessed with an emphasis on morphological alterations in the tegument which were observed using environmental scanning electron microscopy (ESEM) (Oliveira et al. 2013).
Determination of lethal dose 50 (LC50) and lethal dose 90 (LC90)
The mortality data were utilized to calculate the lethal dose or concentration that produces 50% mortality (LC50) and 90% mortality (LC90) of adult worms for PZQ, niosome-PZQ, plain niosomes, and DMSO (Yousif et al. 2012).
Environmental scanning electron microscope studies
The treated adult worms were immediately processed according to Glauert (1974). The worms were fixed by incubation in a mixture containing equal volumes of glutaraldehyde (4%) and cacodylate (0.2%) for 2 h. The worms were then washed by incubation in a solution containing equal volumes of sucrose (0.4%) and cacodylate 0.2% for 2 h at the end of which the worms were incubated for 1 h in a solution containing equal volumes of osmic acid (2%) and cacodylate (0.3%). The samples were finally rinsed with distilled water before being subjected to dehydration using ascending grades of ethanol for 5 min each (30%, 50%, 70%, and 90%). Complete dehydration was achieved with absolute alcohol which was applied in 3 cycles 10 min each. The dehydrated samples were examined by ESEM (Inspect S; FEI, Holland) at the Electron Microscopy Unit of Theodor Bilharz Research Institute (TBRI).
In vivo studies
Experimental animals
The study employed 200 clean laboratory bred 4–5 weeks age Swiss albino male mice weighing 20–25 g. The mice were housed in standard cages and were fed on a standard diet and water ad libitum. Cercariae of S. mansoni (Egyptian strain) were obtained from infected Biomphalaria alexandrina snails. After exposure to light for at least 4 h, S. mansoni cercariae shed from the snails were used to infect the mice. The mice were infected by subcutaneous injection of dispersion containing 60 S. mansoni cercariae. This was conducted according to the protocol initially established by Peter and Warren (1969). The housing and infection were performed in Schistosome Biological Supply Program (SBSP), Theodor Bilharz Research Institute (TBRI), Giza, Egypt.
Drug regimen
Praziquantel (PZQ) powder was dispersed in water and was administered orally in a dose of 250 mg/kg twice in the same day with 3 h apart or in a dose of 500 mg/kg twice with 24 h apart (Ismail et al. 1996; Rewisha et al. 2003; Abd El-Hady et al. 2013). For niosomal encapsulated PZQ, the drug was given as 250 mg/kg in two successive doses with 3 h apart (Sultan et al. 2016).
Experimental groups
The experimental groups are summarized in Table 2. S. mansoni-infected mice were divided into three groups. Group (I) did not receive any treatment and was utilized as the control. Group (II) was treated with PZQ suspension. This was subdivided into four subgroups (IIa, IIb, IIc, and IId). Subgroup IIa was treated with PZQ suspension 4 weeks post-infection in a dose of 250 mg/kg twice in the day. The remaining subgroups received PZQ suspension in a dose of 500 mg/kg in two successive days with the treatment being administered 6, 10, and 12 weeks post-infection for IIb, IIc, and IId, respectively. Group (III) was subdivided into subgroups IIIa, IIIb, IIIc, and IIId which were treated with niosomal PZQ in a dose of 250 mg/kg twice in a day with the treatment being administered 4, 6, 10, and 12 weeks post-infection, respectively. One week after the last dose, all mice were injected with heparin before being sacrificed. The mice liver and intestine were subjected to parasitological examination which included adult worm and egg count. The livers were also subjected to histopathological and immunohistochemical examinations.
Treatment analyses
The adult worm count employed the well-established animal perfusion technique which involved incision of the portal vein and perfusion of citrated saline through the descending aorta (Smithers and Terry 1965; Duvall and De Witt 1967).
Tissue egg count was performed using defined sections of the liver and colon of each mouse. The number of Schistosoma mansoni ova was estimated using the potassium hydroxide digestion method according to Cheever (1968). The recorded number was expressed for the liver and intestine after correction to the liver weight and to the large intestinal length, respectively.
Histopathological study
The histopathological study involved treatment of liver sections with 10% neutral formalin and preparation of 5-μm thick sections. Selected sections were stained with hematoxylin and eosin stain. These sections were examined microscopically to determine the number of the granulomas and their average diameter in addition to the description of granuloma tissue (Bancroft and Steven 1975; Jacobs et al. 1997).
Unstained liver sections were subjected to immunohistochemical examination of vascular endothelial growth factor (VEGF) to assess the degree of fibrosis. Briefly, the section was immersed in citrate buffer (PH 6.0) before incubation at 100 °C in microwave for 10 min. The activity of endogenous peroxidase was inhibited by treating the specimen with hydrogen peroxide for 10 min at the end of which the sample was washed with phosphate-buffered saline (PBS). The clean samples were incubated for 10 min in Ultra V block to prevent non-specific background staining, and washing was repeated. The prepared sections were then subjected to an overnight incubation with monoclonal rabbit anti VEGF (Clone: EP1176 y, GENOVA company, Ready to use). The sections were rinsed with PBS before incubation with biotin-labeled secondary antibody for 10 min at ambient temperature. Rinsing was repeated and the sections were incubated with streptavidin peroxidase solution for 10 min at ambient conditions. Finally, the treated sections were washed with PBS and were developed with 3–3′-diamino-benzidine-tetra-hydrochloride (DAB) and hydrogen peroxide as a chromogen. These sections were then subjected to counterstaining with Meyers hematoxylin, dehydrated in alcohol, and mounted in Di-n-butyl-phthalatepolystyrene-xylene (DPX). For negative control, PBS was used instead of primary antibody. The prepared sections were examined using the light microscope and were scored according to Gou et al. (2011) based on the percentage of stained cells and the intensity of staining. “The quantity score ranges from 0 to 4, i.e., 0: no immunostaining; 1: 1–10% of cells are positive; 2: 11–50% are positive; 3: 51–80% are positive; and 4: ≥ 81% of cells are positive. The staining intensity was scored as 0 (negative), 1 (weak), 2 (moderate), and 3 (strong). Raw data were converted to immunohistochemical score (HIS) by multiplying the quantity score (0–4) by the staining intensity score (0–3) with a range from 0 to 12. An IHS of 0 was considered negative; 1–4: weak (+1); 5–8: moderate (+2); and 9–12: a strong immunoreactivity (+3).”
Ethics statement
The study protocol was approved and conducted according to the guidelines of the Laboratory Animal Centre for Research Ethics Committee at Faculty of Medicine, Tanta University (code number 30641/12/2015).
Statistical data analysis
These data were analyzed by one-way ANOVA followed by Tukey’s multiple comparison as a post hoc test to determine significance of differences between groups using Statistical Package for Social Sciences (SPSS) (SPSS Inc., Chicago, Illinois, USA), software for windows, version (20). The difference was considered statistically significant when P < 0.05, highly significant when P < 0.01, and extremely significant when P < 0.001.
Results
In vitro results
Assessment of the effect of niosomal encapsulation of PZQ on its schistosomicidal effect in vitro
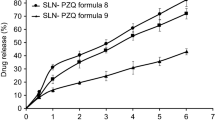
Incubation of the parasite with niosomes alone resulted in a significant death (30%). This effect was even higher than that obtained with low concentration (0.001 μg/ml) of drug solution which resulted in only 10% death. Exposure of the parasite to PZQ-niosomes increased the death to 50 and even to 100% depending on the concentration of the loaded drug (Table 3). Comparing the effects of medicated niosomes to that of PZQ solution reflected the dependence on the concentration of PZQ. Thus, worms exposed to high drug concentration (1, 0.5, or 0.2 μg/ml) show 100% death irrespective to the tested formulation of drug. PZQ (0.1 μg/ml) caused 85% death of the worms, while niosome-PZQ caused 90% death of the worms with non-significant difference between both forms (P > 0.05). PZQ solution at concentrations of 0.05, 0.01, and 0.001 μg/ml caused 65%, 60%, and 10% death of adult worms, respectively, with niosome containing PZQ resulting in significant increase (P < 0.05) in the percent of adult worm death (80%, 65%, and 50%, respectively). Median lethal concentration (LC50) values of 0.011 μg/ml and 0.048 μg/ml were calculated for niosomes-PZQ and PZQ solution, respectively. The concentration required to kill 90% of the worms (LC90) was 0.14 μg/ml for niosomal PZQ and was 0.200 μg/ml for PZQ solution. Worms exposed to the solvent were not affected and were alive after the incubation period. Incubation of the worms with drug free niosomes resulted in 30% death. So, it is important to highlight that the placebo niosomes resulted in a significant increase in the worm death compared with 1% aqueous DMSO which was employed as solvent for the drug (P < 0.001) (Table 3).
The motility of the living worms was monitored periodically after incubation with the drug solution or niosomes using a dissecting microscope. The percentage of worms that had a reduced motility was directly proportional to the concentration and to the period of incubation. After 2-h incubation of adult worms with 1, 0.5, and 0.2 μg/ml concentration of PZQ in solution and in niosomal formulation, live worms showed decreased motor activity and flattened unnatural body attitude with some of them being killed with coiled body. Extending the incubation period to 24 h resulted in complete death and body coiling of all worms. Incubation of the adult worms with the drug solution or encapsulated in niosomes at lower concentrations (0.1, 0.05, 0.01, and 0.001 μg/ml) resulted in gradual reduction in the motility of adult worms. The effect became more evident after 24 h at which there was complete loss of all motility of live worm with the suckers being the active part only. Worms in negative control groups (DMSO 1%) remained motile, while those incubated with plain niosomes show slight decrease in the motility of living worms throughout the analysis period. This finding reflects the potential effect of plain niosomes on the viability for worms.
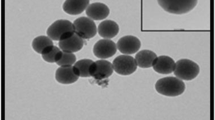
Tegumental changes of S. mansoni adult worms in response to PZQ, niosome-PZQ, niosomes, and DMSO 1% visualized by scanning electron microscope (SEM)
Ultramorphological alterations were observed in S. mansoni adult worms after 24 h incubation in vitro by SEM. No tegumental changes in the adult worms were observed for the DMSO 1% negative control group as male worms had a tegument that was covered with tubercles and tiny projections (spines). The back was long and contained the gynecophoral canal. The area between the oral and ventral suckers did not have any tubercles, spines, or sensory papillae. Also, large number of tubercles with typical spines was observed (Fig. 1a, b). Incubation of the adult worms with plain niosomes resulted in moderate contracture and destruction in their morphology. This destruction occurred in the oral and ventral suckers (Fig. 1c). Tegumental changes occurred in the form of destruction, peeling of spines, tubercles, and tegument peeling or sloughing. Also, gynecoghoric canal flattening and effacement were observed (Fig. 1d). Figure 1e showed blebbing of tubercles and niosome vesicles in between them. Exposure of the adult worms to low concentration of PZQ resulted in minimal destruction and peeling of tubercles and spines with ulceration of the tegument (Fig. 2a), while exposure to moderate concentration showed tegument peeling, blebbing, ulceration, and destruction of tubercles and spines (Fig. 2c). The effect became more evident on exposure to high concentration of PZQ, as adult worms showed extensive body coiling, changes in acetabular suckers, tegument peeling, and destruction of tubercles and spines (Fig. 2e). Scanning electron microscope of adult worms incubated with low concentration of niosome-PZQ resulted in minimal destruction and peeling of tubercles and spines (Fig. 2b). Exposure to moderate concentration showed moderate destruction and peeling of tubercles and spines (Fig. 2d). At high concentration, niosomal-PZQ resulted in extensive coiling of the body, marked destruction, and peeling of tubercles and spines (Fig. 2f).
a Scanning electron microscopy (SEM) of normal male and female adult Schistosoma mansoni incubated with DMSO1% (male anterior end showing gynecophoric canal, oral sucker, and ventral sucker). b Higher magnification of the tubercles and spines. c SEM of Schistosoma mansoni adult worm after incubation with plain niosomes showing oral and ventral suckers alterations or destructions. d SEM of Schistosoma mansoni male adult worm after incubation with plain niosomes showing completely coiled body, tegumental peeling with destruction and peeling of tubercles and spines with flattening, and effacement of gynecophoric canal. e SEM of Schistosoma mansoni adult worm after incubation with plain niosomes showing tegumental peeling and blebbing (bubbles surrounding the morphologically altered tubercles) with niosomes vesicles attached to it
SEM of Schistosoma mansoni adult worm after incubation with different concentrations (conc.) of PZQ or niosome-PZQ. a PZQ at low conc. showing very minimal destruction and peeling of tubercles and spines with ulceration of the tegument. b Niosome-PZQ at low conc. showing minimal destruction and peeling of tubercles and spines. c PZQ at moderate conc. showing tegument peeling, blebbing, ulceration, and destruction of tubercles and spines. d Niosome-PZQ at moderate conc. showing moderate destruction and peeling of tubercles and spines. e PZQ at high conc. of showing extensive body coiling, changes in acetabular suckers, tegument peeling, and destruction of tubercles and spines. f Niosome-PZQ at high conc. of showing extensive coiling of the body, marked destruction, and peeling of tubercles and spines
In vivo results
Effect of PZQ and niosome-PZQ on S. mansoni adult worms
Oral administration of PZQ to S. mansoni-infected mice resulted in a significant reduction in the average worm burden compared to the infected un-treated mice (P < 0.001). This effect was recorded irrespective to the formulation of PZQ. Comparing PZQ solution to niosome-PZQ, the latter was more efficient with the worm count being significantly lower than that calculated after administration of the drug solution (Table 4).
Effect of PZQ and niosome-PZQ on the oviposition of S. mansoni
Treatment of infected mice with either PZQ or niosome-PZQ induced a significant reduction in the mean liver and intestinal S. mansoni egg count compared to the infected un-treated mice (control) (P < 0.001). As for the worm count, niosomal PZQ was more efficient than the drug solution with respect to reduction in the egg count (P < 0.05) (Table 5).
Effect of PZQ and niosome-PZQ on the number and size of granulomas/liver section
Treatment of S. mansoni-infected mice with either PZQ or niosome-PZQ at 6, 10, and 12 weeks P.I. induced a significant reduction in the mean number of granulomas in the H&E-stained liver sections compared to the infected un-treated mice (P < 0.001). Again, the niosome encapsulated PZQ was more efficient in reducing the granuloma number and size as compared to drug solution. The difference becomes more distinct when comparing the longer duration P.I. (P < 0.001). The same trend was recorded after measuring the size of the granulomas (Table 6).
Histopathological examination of the liver parynchyma
Histopathological examination of the liver sections obtained 4 weeks after infection of untreated mice showed blood vessel containing adult S. mansoni worm with hematin. This is surrounded by mild inflammatory infiltrate mainly of lymphocytes (Fig. 3a). The liver sections of the corresponding group which was treated with PZQ solution revealed moderate inflammatory cellular infiltrate which comprises macrophages, plasma cells, lymphocytes, and eosinophilis surrounding transversally cut intact adult worm and also in the liver lobule (Fig. 3b). Treating the corresponding group with niosome-PZQ resulted in disintegration of adult worms with subsequent marked inflammatory infiltrate mainly of polymorph nuclear lymphocytes, eosinophilis, macrophages, and plasma cells around them (Fig. 3c).
a Liver section of a mouse of the control subgroup Ia (4 weeks P.I.) showing adult worm with haematin inside the blood vessel (arrow). b Liver section of a mouse of the PZQ subgroup IIa (4 weeks P.I.) showing adult worm intact inside the the portal vein surrounded with moderate inflammatory infilterate mainly formed of lymphocytes and eosinophilis (arrow). c Liver section of a mouse of the niosome-PZQ subgroup IIIa (4 weeks P.I.) showing marked inflammatory infilterate surrounding destroyed adult worm formed mainly of polymorph nuclear lymphocytes, eosinophilis, macrophages, and plasma cells (arrow) (H&E × 400)
In untreated-infected mice sacrificed 6 weeks P.I., liver sections showed multiple schistosomal granulomas which may contain S. mansoni ova. The majority of granulomas were of cellular type with the others being fibrocellular (Fig. 4a). Extending the infection period of untreated group to 10 weeks changed the type of granulomas which became of fibrocellular and fibrotic types mainly (Fig. 4d). Further extension of the infection period to 12 weeks compromized the granuloma to be mainly of fibrotic type (Fig. 4g). Treatment of the infected mice with PZQ solution improved the histopathological features within the granulomas which became fibrocellular with mild fibrous tissue depending on the duration of infection. This was associated with a reduction in the size and number of the granulomas compared to the untreated group (Fig. 4b, e, h). Replacing PZQ solution with niosome-PZQ showed marked decrease in the number and size of granulomas with the majority of them being of cellular types (Fig. 4c, f, i).
Histopathological examination of liver section stained with H&E (× 200) showing hepatic granulomas. a Infected untreated subgroup Ib (6 weeks P.I.) showing multiple schistosomal granulomas. The majority of them are of cellular type, while the others are fibrocellular. Some of them containing S. mansoni ova (arrows). b PZQ-treated subgroup IIb (6 weeks P.I.) showing multiple schistosomal granulomas consisting of marked inflammatory infiltrate within the portal tracts with few egg depositions inside (arrows). c Niosome-PZQ treated subgroup IIIb (6 weeks P.I.) showing smaller size of schistosomal granulomas of cellular type and fewer number of deposition of eggs (arrow). d Infected untreated subgroup Ic (10 weeks P.I.) showing multiple schistosomal granulomas mainly of fibrocellular type (arrows) around S. mansoni ova. e PZQ-treated subgroup IIc (10 weeks P.I. showing multiple schistosomal granulomas mainly of fibrocellular type consisting of inflammatory infiltrate mainly lymphocytes and few fibroblasts. Some of them containing S.mansoni ova (arrows). f Niosome-PZQ-treated subgroup IIIc (10 weeks P.I.) showing marked reduction in the number and size of schistosomal granuloma as compared to the control group. The granuloma is of fibrocellular type consisting of inflammatory infiltrate mainly lymphocytes and mild fibrosis (arrow). g Infected untreated subgroup Id (12 weeks P.I.) showing multiple schistosomal granulomas, most of them are fibrous with centrally located concentric fibrous tissue around Schistosoma mansoni ovum with few lymphocytes (arrows). h PZQ-treated subgroup IId (12 weeks P.I.) showing multiple schistosomal granulomas mainly of fibrocellular type (arrows). i Niosome-PZQ-treated subgroup IIId (12 weeks P.I.) showing significant reduction in the number and size of schistosomal granulomas as compared to the control subgroup Id. They are mainly of cellular type surrounded by inflammatory cells mainly lymphocytes (arrows)
Immunohistochemical study of liver sections for vascular endothelial growth factor (VEGF)
Treatment with PZQ solution or niosomes resulted in significant reduction in the VEGF intensity and percentage compared to the infected untreated group. This was also reflected in the percentage score and the total score of VEGF. Comparing PZQ solution to niosomes-PZQ, the latter was superior. the difference being significant especially 12 weeks post-infection with other periods showing at least a trend of enhanced treatment after niosomal encapsulation (Table 7).
The S. mansoni-infected untreated group showed a high expression on proliferating blood vessels around the granulomas (score 4, score 6, score 6) at 6, 10, and 12 weeks P.I., respectively. This score was reduced to score 2 irrespective to the duration of infection after treatment with PZQ solution. Treatment with niosomes-PZQ produced further reduction in the score to record score 2, score 1, and score 1 at 6, 10, and 12 weeks P.I., respectively (Fig. 5).
Immunohistochemical expression of VEGF (immunoperoxidase × 400). a Infected untreated group (6 weeks P.I.) showing cytoplasmic VEGF expression within proliferating blood vessels and inflammatory cells (score 4). b PZQ-treated subgroup IIb (6 weeks P.I.) showing cytoplasmic VEGF expression within inflammatory cells (score 2). c Niosome-PZQ subgroup IIIb (6 weeks P.I.) showing cytoplasmic VEGF expression within proliferating blood vessels and inflammatory cells (score 2). d Infected control subgroup Ib (10 weeks P.I.) showing cytoplasmic VEGF expression within proliferating blood vessels and inflammatory cells (score 6). e PZQ-treated subgroup IIc (10 weeks P.I.) showing cytoplasmic VEGF expression within inflammatory cells (score 2). f Niosome-PZQ-treated subgroup IIIc (10 weeks P.I.) showing cytoplasmic VEGF expression within inflammatory cells (score 1). g Infected control subgroup Id (12 weeks P.I.) showing cytoplasmic VEGF expression within proliferating blood vessels and inflammatory cells (score 6). h PZQ-treated subgroup IIId (12 weeks P.I.) showing cytoplasmic VEGF expression within inflammatory cells (score 2). i Niosome-PZQ-treated subgroup IIId (12 weeks P.I.) showing cytoplasmic VEGF expression within inflammatory cells (score 1)
Discussion
PZQ remains as the drug of choice for the treatment of schistosomiasis. This is based on its low cost and ease of administration (single oral dose of 40–50 mg/kg) in addition to high patient tolerability. Unfortunately, the drug has poor water solubility and cannot prevent re-infection and is not effective against schistosomula and juvenile worms of S. mansoni. Moreover, the development of drug-resistant strains of Schistosoma and tolerance can contribute to the factors of therapeutic failures (Gryseels et al. 2006). These factors explain the low cure rate in areas where schistosomiasis is hyper endemic (Liang et al. 2001). Accordingly, development of new drugs or improving the existing ones is a necessity. However, development of new chemical entity requires massive research and is of high cost. Therefore, authors concentrated on improving the specifications of the existing drugs. This is being achieved using modern drug delivery systems with emphasis on nanostructures. Of these, vesicular systems like niosomes are very promising carriers to enhance the biopharmaceutical properties of PZQ (Nasr et al. 2008). The enhanced properties were reflected in this study.
The effects of niosomal encapsulation on the antiparasitic effect of PZQ were first monitored in vitro. This involved investigation of the effect of different concentrations of PZQ in solution or encapsulated in niosomes on adult schistosomes. The results indicated the superiority of niosomal PZQ which reduced the LC50 and LC90. Surprisingly, the non-medicated niosomes were able to provide measurable amount of death in the worm which was even greater than that recorded by very low PZQ solution. This effect can be attributed to the ultramorphological changes which were induced by the vesicles. The developed changes in the morphology of parasite can be due to the potential membrane disrupting effect of noisome components (Sultan et al. 2016). Encapsulation of PZQ in these niosomes resulted in further increase in the percentage death. The superiority of medicated niosomes over drug solution with respect to worm death may be due to synergistic effect of niosomal formulation and PZQ. However, the experimental design did not indicate whether the recorded effect is the sum of the effect of niosome components and free PZQ or due to PZQ entrapped in the vesicles. Detailed investigations using niosomes having different composition are necessary to answer this question.
In addition to mortality, all worms underwent significant changes in the seed coat followed by muscle contractions. Muscle contraction and paralysis are among the effects of PZQ on S. mansoni and are followed by ultrastructural changes and destruction of the integument which may result in membrane depolarization and the influx of extracellular calcium. The tegument of S. mansoni is extremely important for successful infection with subsequent survival in the host (Shuhua et al. 2000). Taking this into consideration together with the augmented effects of niosomal encapsulation of PZQ, the work was extended to monitor the in vivo efficacy of niosomal PZQ. The in vivo assessment involved oral administration of the drug in solution form or as PZQ-niosomes. This route was selected to mimic the actual administration in human.
To date, no work is available in literature on the in vitro efficacy of niosome formulations on parasites. Most of the available reports concerned with the effect of vesicular drug delivery systems on the bacteria with one of them recording enhanced antibacterial activity and reduced bacterial resistance after encapsulation of drugs into similar niosomes (Abdelaziz et al. 2015). Liposomal encapsulation was able to augment the in vitro efficacy of PZQ (Mourão et al. 2005). Other nanostructures have been tested in vitro with promising results being shown for nanostructured lipid carriers (NLC) which were better than PZQ solution (Kolenyak-Santos et al. 2015). Solid lipid nanoparticles have been also shown to enhance the schistosomicidal activity of PZQ in vitro (de Souza et al. 2014). The enhanced schistosomicidal activity after niosomal encapsulation can be explained based on the recorded findings with other organisms. Vesicular systems are believed to get adsorbed on or fused to the surface of the organism with subsequent direct transfer of high concentration of the drug into the organism. This effect has been shown for niosomes with bacteria (Abdelaziz et al. 2015) and can be extrapolated to Schistosoma. This supposition is supported by the recorded ultrastructure changes in the worm after incubation with niosomal formulation.
Treatment of infected mice with either PZQ-free solution or niosomes-PZQ resulted in significant reduction in the worm count and tissue egg count. This was associated with reduction in the hepatic granuloma size and number. In all parameters, niosomes were superior. The reduction of worm burden is similar to that recorded by other investigators who tested PZQ solution (Issa 2007; Abdel-Rahman 2009; El-Sisi et al. 2011; Sharaf EL-Deen et al. 2017). Reduction of worm burden can be explained on the basis that PZQ can directly affect adult schistosomes leading to their contraction, paralysis, and subsequent shift from mesenteric veins to the liver where they are finally destroyed by the phagocytic cells. In addition, the drug can enhance calcium uptake by parasite leading to damage of adult schistosome tegument, exposing antigens on the worm surface to trigger cellular and humoral immune responses (Fallon et al. 1995).
Reduction in tissue egg count after treatment can be due to the possible effect of PZQ on vitelline cells and ovaries in addition to killing adult worms with subsequent elimination of the source of eggs (Liu et al. 2012). The decrease in the size and number of hepatic granuloma after treatment with PZQ formulations is due to PZQ regulatory effect on cell immune responses which reduces CD4 T cells and increase CD8 T cells resulting in reduction of hepatic schistosomal granuloma size (Elhenawy et al. 2017). The superiority of niosomes-PZQ over the corresponding drug solution can be related to the improved drug bioavailability after niosomal encapsulation. This can be explained by overcoming some of the problems associated with oral administration of PZQ as slow and erratic dissolution rate with a strong dependence on the type of food. The latter can result in inter-subject variability in oral bioavailability of the drug (El-Lakkany et al. 2012b). In addition, the drug has been shown to undergo extensive first-pass metabolism (Olliaro et al. 2014). These factors result in low and variable oral bioavailability.
Niosomes can help in this direction, as they were claimed to deliver the drug through the lymphatic pathway bypassing the liver. This can eliminate or at least reduce the extensive first-pass metabolism. Another possible explanation is the presence of peceol which can fluidize the lipid bilayer of the intestinal membrane allowing for more drugs to pass through (Sultan et al. 2018). Similar enhancement has been recorded for other vesicular carrier. For example, praziquantel liposomes showed better effectiveness than the free drug treatment. In addition, praziquantel liposomes associated to hyperbaric oxygen treatment (HBO) exhibited synergistic action with better effects than those presented by free drug treatment (Frezza et al. 2013). The superiority of niosomal PZQ was reflected in the histopathological examination of the liver tissues. This can be attributed to the ability of niosome to deliver a higher concentration of PZQ to kill the adult worms and reduce the amount of parasite eggs. These histopathological findings simulate the results reported by other investigators who employed nanoparticles as carriers (Dkhil et al. 2016).
In the current study, immunohistochemical staining demonstrated a high expression of VEGF of proliferating blood vessels around the granulomas which gradually increased with progression of the infection. This is evidenced by significant increase in its expression in the infected untreated mice that reached the highest level (score 3+++) at 12th weeks P.I. This finding runs in parallel with the results of Lenzi et al. (2002) and Botros et al. (2010) who reported that the VEGF immunoexpression in the liver section from S. mansoni-infected mice showed a high expression of proliferating blood vessels. Treatment with PZQ as simple solution or niosomal formulation decreased the angiogenesis. Once again niosome-PZQ was superior where differences in VEGF expression were significantly less in the sinusoids when compared with those of mice treated with PZQ. These data are in comparable to the results of the study of Botros et al. (2010) that showed that treatment of S. mansoni-infected mice with PZQ in combination with artemether led to moderate expression in few angiogenesis and less severe histopathological changes. This confirms the positive effects of niosomal formulation as promising carrier for PZQ in the therapy of S. manosni. It is important to highlight the possibility of reduced toxicity of drugs after niosomal encapsulation. This has been reported for an antileishmanial compound where niosomal encapsulation was able to reduce the hepatic and renal toxicity compared to the free drug (Lala et al. 2003). However, detailed toxicological studies are required for the developed niosomal formulation.
Conclusion
The study introduced niosomes as promising carriers for oral delivery of praziquantel. These vesicles can enhance both in vivo and in vitro efficacy of praziquantel against Schistosoma mansoni. The enhanced activity can be attributed to improved oral bioavailability in addition to the ability of niosomal praziquantel to develop ultrastuctural tegumental changes in adult worms with subsequent enhancement of calcium influx into the worm. This can increase the schistosomicidal activity. Future pharamacokinetic-pharmacodynamic correlations are required to confirm the mechanism of enhanced praziquantel activity after niosomal encapsulation.
References
Abd El-Hady MH, Abaza BE, Fathy GM, Badawey MS, Nada SM, El-Shafei MA, Abd El-Aziz HR (2013) Impact of treatment with praziquantel supplemented by silymarin on Schistosoma mansoni- induced fibrosis in mice. PUJ 6(1):77–88
Abdelaziz AA, Elbanna TE, Sonbol FI, Gamaleldin NM, El Maghraby GM (2015) Optimization of niosomes for enhanced antibacterial activity and reduced bacterial resistance: in vitro and in vivo evaluation. Expert Opin Drug Deliv 12:163–180
Abdel-Rahman SA (2009) Monitoring Th1 and Th2 cytokine patterns after praziquantel and mirazid treatment in experimental mansoniasis. PUJ 6(1):66–77
Ahmad A, Ahmad R (2015) Understanding the mechanism of hepatic fibrosis and potential therapeutic approaches. Saudi J Gastroenterol 18:155–167
Angaye TCN (2016) A review on the epidemiology and control of schistosomiasis in Nigeria. J Med Health Res 1(2):1–23
Bancroft JD, Steven A (1975) Histopathological stains and their diagnostic uses. Churchil. Livingstone, pp 1–20
Becket G, Schep LJ, Tan MY (1999) Improvement of the in vitro dissolution of praziquantel by complexation with alpha-, beta- and gamma-cyclodextrins. Int J Pharm 179(1):65–71
Botros S, Hammam O, Mahmoud M, Bergquist R (2010) Praziquantel efficacy in mice infected with PZQ non susceptible Schistsoma mansoni isolate treated with artemether: parasitological, biochemical and immunohistochemical assessment. APMIS 118:692–702
Bruno J, Neves BJ, Andrade CH, Cravo PVL (2015) Review natural products as leads in schistosome drug discovery. Molecules 20:1872–1903
Castro N, Medina R, Sotelo J, Jung H (2000) Bioavailability of praziquantel increases with concomitant administration of food. Antimicrob Agents Chemother 44(10):2903–2904
Cheever AW (1968) Conditions affecting the accuracy of potassium hydroxide digestion in techniques for counting Schistosoma mansoni eggs in tissues. Bull WHO 39:328–331
Cong Z, Shi Y, Peng X, Wei B, Wang Y, Li J (2017) Design and optimization of thermosensitive nanoemulsion hydrogel for sustained-release of praziquantel. Drug Dev Ind Pharm 43(4):558–573
De Campos AM, Sánchez A, Alonso MJ (2001) Chitosan nanoparticles: a new vehicle for the improvement of the delivery of drugs to the ocular surface. Application to cyclosporin. A Int J Pharm 224:159–168
de Souza ALR, Andreanib T, de Oliveirad RN, Kiill CP, dos Santosa FK (2014) In vitro evaluation of permeation, toxicity and effect of praziquantel-loaded solid lipid nanoparticles against Schistosoma mansoni as a strategy to improve efficacy of the schistosomiasis treatment. Int J Pharm 463:31–37
Dkhil MA, Bauomy AA, Diab MSM, Al-Quraishy S (2016) Protective role of selenium nanoparticles against Schistosoma mansoni induced hepatic injury in mice. Biomed Res 27(1):214–219
Duvall RH, De Witt WB (1967) An improved perfusion technique for recovering adult schistosome from laboratory animal. Am J Trop Med Hyg 16:483–486
El-Arini SK, Leuenberger H (1998) Dissolution properties of praziquantel−PVP systems. Pharm Acta Helv 73:89–94
Elhenawy AA, Rehab H, Ashourb NN, Naglaa MS, Nirmeen M (2017) Possible antifibrotic effect of GDC-0449 (Vismodegib), a hedgehog-pathway inhibitor, in mice model of Schistosoma–induced liver fibrosis. Parasitol Int 66:545–554
El-Lakkany N, El-Din SS, Ebeid F (2012a) The use of pentoxifylline as adjuvant therapy with praziquantel down regulates profibrogenic cytokines, collagen deposition and oxidative stress in experimental schistosomiasis mansoni. Exp Parasitol 129:152–157
El-Lakkany N, Seif El-Din SH, Heikal L (2012b) Bioavailability and in vivo efficacy of a praziquantel-polyvinylpyrrolidone solid dispersion in Schistosoma mansoni-infected mice. Eur J Drug Metab Pharmacokinet 37(4):289–299
El-Sisi A, Awara W, El-Masry T (2011) Effects and mechanism of action of immunomodulating agents against schistosomiasis-induced hepatic inflammation and fibrosis in mice. Res Pharm Biotechnol 3:32–45
Fahmy ZH, El-Shennawy AM, El-Komy W (2009) Potential antiparasitic activity of pomegranate extracts against shistosomules and mature worms of Schistosoma mansoni: in vitro and in vivo study. Aust J Basic Appl Sci 3:4634–4643
Fallon PG, Sturrock RF, Niang AC, Doenhoff MJ (1995) Diminished susceptibility to praziquantel in a Senegal isolate of Schistosoma mansoni. Am J Trop Med Hyg 53:61–62
Frezza TF, Gremião MP, Zanotti-Magalhães EM, Magalhães LA, De Souza AL, Allegretti SM (2013) Liposomal-praziquantel: efficacy against Schistosoma mansoni in a preclinical assay. Acta Trop 128(1):70–75
Glauert AM (1974) Fixation, dehydration and embedding of biological specimens. In: AM Glauert (ed) Practical Methods in Electron Microscopy. Amsterdam Oxford, pp 77–163
Gou HF, Chen XC, Zhu J, Jiang M, Yang Y, Cao D, Hou M (2011) Expressions of COX-2 and VEGF-C in gastric cancer: correlations with lymphangiogenesis and prognostic implications. J Exp Clin Cancer Res 30(1):14
Gryseels B, Polman K, Clerinx J (2006) Human schistosomiasis. Lancet 368:1106–1118
Inagaki Y, Nemoto T, Kushida M, Sheng Y, Higashi K (2003) Interferon alfa down-regulates collagen gene transcription and suppresses experimental hepatic fibrosis in mice. Hepatol 38:890–899
Ismail M, Metwally A, Farghaly A, Bruce J, Tao L, Bennet JL (1996) Characterization of isolates of Schistosoma mansoni from Egyptian villagers that tolerate high doses of praziquantel. Am J Trop Med Hyg 55:241–218
Issa RM (2007) Schistosoma mansoni: the prophylactic and curative effects of propolis in experimentally-infected mice. Rawal Med J 32:94–98
Jacobs W, Bogers J, Deelder A, Wery M, Marck E (1997) Adult Schistosoma mansoni worms positively modulate soluble egg antigen induced inflammatory hepatic granuloma formation in vivo. Serological analysis and immunophenotyping of extracellular matrix proteins, adhesion molecules and chemokines. Am J Pathol 150(6):2033–3045
Kolenyak-Santos F, Garnero C, de Oliveira RN, de Souza ALR, Chorilli M (2015) Nanostructured lipid carriers as a strategy to improve the in vitro schistosomiasis activity of Praziquantel. JNN 14:1–12
Lala S, Nandy AK, Mahato SB, Basu MK (2003) Delivery in vivo of 14-deoxy-11-oxoandrographolide, an antileishmanial agent, by different drug carriers. IJBB 40:169–174
Lenzi JA, Mota EM, Pelajo- Machado M, Vale LS, Vale BS, Andrade ZA (2002) Intestinal fibro-vascular nodules caused by Schistosoma mansoni infection in Calomys callosus-Rengger, 1830 (Rodentia:Cricetidae): a model of concomitant fibrosis and angiogenesis. Mem Inst Oswald Cruz 97:117–127
Liang YS, Coles G, Doenhoff MJ, Vaughan RS (2001) In vitro responses of praziquantel-resistant and susceptible Schistosoma mansoni to praziquantel. Int J Parasitol 31:1227–1235
Liu Y, Meyer C, Muller A, Herweck F, Li Q et al (2012) IL-13 signaling in liver fibrogenesis. Front Immunol 3:116
Moraes J, Nascimento C, Lopes PO, Nakano E, Yamaguchi LF, Kato MJ (2013) Schistosoma mansoni: in vitro schistosomicidal activity of piplartine. Exp Parasitol 127:357–364
Mourão SC, Costa PI, Salgado HR, Gremião MP (2005) Improvement of antischistosomal activity of praziquantel by incorporation into phosphatidylcholine containing liposomes. Int J Pharm 295:157–162
Nasr M, Mansour S, Mortada ND, Elshamy AA (2008) Vesicular aceclofenac systems: a comparative study between liposomes and niosomes. J Microencapsul 25:499–512
Oliveira RN, Rehder VLG, Oliveira ASS, Montarinari-Júnior I, Carvalho JE et al (2013) Schistosoma mansoni: in vitro schistosomicidal activity of essential oil of Baccharis trimera (less) DC. Exp Parasitol 132(2):135–143
Olliaro P, Delgado-Romero P, Keiser J (2014) The little we know about the pharmacokinetics and pharmacodynamics of praziquantel (racemate and R-enantiomer). J Antimicrob Chemother 69(4):863–870
Peter PA, Warren KS (1969) A rapid method of infecting mice and other laboratory animals with Schistosoma mansoni: subcutaneous injection. J Parasitol 55:558
Rewisha E, Asel F, El Nouby KH, El-Refaie A, Baalash A (2003) Evaluation of antifibrotic effect of silymarin and myrrh on schistosomal hepatic fibrosis: an experimental study. Tanta M J 31(3):745–759
Robert B, Jürg U, Jennifer K (2017) Controlling schistosomiasis with praziquantel: how much longer without a viable alternative? Infect Dis Poverty 6:74
Sharaf EL-Deen SA, Brakat RM, Mohamed ASE (2017) Artichoke leaf extract protects liver of Schistosoma mansoni infected mice through modulation of hepatic stellate cells recruitment. Exp Parasitol 178:51–59
Shuhua X, Binggui S, Chollet J, Utzinger J, Tanner M (2000) Tegumental changes in adult Schistosoma mansoni harbored in mice treated with artemether. J Parasitol 86:1125–1132
Smithers SR, Terry RJ (1965) The infection of laboratory hosts with cercariae of Schistosoma mansoni and the recovery of adult worms. Parasitol 55:695–710
Sultan AA, El-Gizawy SA, Osman MA, El Maghraby GM (2016) Colloidal carriers for extended absorption window of furosemide. J Pharm Pharmacol 68:324–332
Sultan AA, El-Gizawy SA, Osman MA, El Maghraby GM (2018) Niosomes for oral delivery of nateglinide: in situ-in vivo correlation. J Liposome Res 2:1–9
WHO (2016) Summary of global update on preventive chemotherapy implementation in 2015. Wkly Epidemiol Rec 91(39):456–459
Xie S, Pan B, Wang M, Zhu L, Wang F, Dong Z, Wang X, Zhou W (2010) Formulation, characterization and pharmacokinetics of praziquantel-loaded hydrogenated castor oil solid lipid nanoparticles. Nanomedicine 5:693–701
Yousif F, Wassel G, Boulos L, Labib T, Mahmoud K (2012) Contribution to in vitro screening of Egyptian plants for schistosomicidal activity. Pharm Biol 50(6):732–739
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Handling Editor: Julia Walochnik
Rights and permissions
About this article
Cite this article
Zoghroban, H.S., El-Kowrany, S.I., Aboul Asaad, I.A. et al. Niosomes for enhanced activity of praziquantel against Schistosoma mansoni: in vivo and in vitro evaluation. Parasitol Res 118, 219–234 (2019). https://doi.org/10.1007/s00436-018-6132-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-018-6132-z