Abstract
There was recently an outbreak of malaria in Ubon Ratchathani Province, northeastern Thailand. In the absence of information on malaria vector transmission dynamics, this study aimed to identify the anopheline vectors and their role in malaria transmission. Adult female Anopheles mosquitoes were collected monthly by human-landing catch in Na Chaluai District of Ubon Ratchathani Province during January 2014−December 2015. Field-captured mosquitoes were identified to species using morphology-based keys and molecular assays (allele-specific polymerase chain reaction, AS-PCR), and analysed for the presence of Plasmodium falciparum and Plasmodium vivax using an enzyme-linked immunosorbent assay (ELISA) for the detection of circumsporozoite proteins (CSP). A total of 1,229 Anopheles females belonging to 13 species were collected. Four anopheline taxa were most abundant: Members of the Anopheles barbirostris complex, comprising 38% of the specimens, species of the Anopheles hyrcanus group (18%), Anopheles nivipes (17%) and Anopheles philippinensis (12%). The other nine species comprised 15% of the collections. Plasmodium infections were detected in two of 668 pooled samples of heads/thoraces, Anopheles dirus (1/29) and An. philippinensis (1/97). The An. dirus pool had a mixed infection of P. vivax-210 and P. vivax-247, whereas the An. philippinensis pool was positive only for the latter protein variant. Both positive ELISA samples were confirmed by nested PCR. This study is the first to incriminate An. dirus and An. philippinensis as natural malaria vectors in the area where the outbreak occurred. This information can assist in designing and implementing a more effective malaria control programme in the province.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is one of the most important mosquito-borne diseases of humans. There was an estimated 429,000 malaria deaths globally, mostly among African children, in 2015 (WHO 2016). Of 472 formally recognised Anopheles species worldwide (Harbach 2017), approximately 41 have been incriminated as important malaria vectors (Sinka et al. 2011). In Thailand, malaria remains one of the major causes of morbidity and mortality, due to the presence of efficient vectors and the migration of foreign workers and refugees across international borders. Most malaria cases reportedly occur in forest and forest fringe areas along the borders with Myanmar, Cambodia and Malaysia (Corbel et al. 2013). Currently, the Thai-Cambodia border is recognised as an epicentre of antimalarial drug resistance for Plasmodium falciparum (Cui et al. 2012). Ten provinces in Thailand, Ubon Ratchathani, Tak, Srisaket, Yala, Kanchanaburi, Narathiwat, Mae Hong Son, Surat Thani, Songkla and Prachinburi, recorded the highest prevalence of malaria cases (n = 12,492), with Plasmodium vivax (58.29%) and P. falciparum (33.25%) being responsible for the majority of cases reported in 2015 (Bureau of Vector Borne Diseases, Ministry of Public Health, Thailand 2015).
Of the 77 Anopheles species recognised in Thailand (Rattanarithikul et al. 2006; Harbach et al. 2017), four species, Anopheles dirus, Anopheles baimaii, Anopheles minimus and Anopheles maculatus, have been incriminated as the primary malaria vectors in the country (Manguin et al. 2008; Tainchum et al. 2015). During the past decade, species diversity, biting activity, seasonal abundance, host preference, vector competence and molecular identification of the main malaria vectors was well studied in the western provinces bordering Myanmar. For example, Tananchai et al. (2012) investigated the density and biting activity of An. dirus and An. baimaii in the malaria prone area of Kanchanaburi Province in west-central Thailand. Subsequently, Tainchum et al. (2014) reported the highest numbers of An. minimus collected from February to April during a 2-year study in malaria endemic areas of Tak and Mae Hong Son Provinces, which are located along the Thai-Myanmar border. More recently, Sriwichai et al. (2016) reported that 22 pools of An. minimus s.l., An. maculatus s.l., species of the An. annularis group and An. barbirostris s.l. collected in Tak Province were found ELISA positive for P. vivax circumsporozoite protein (Pv-210 and Pv-247). Unfortunately, although malaria is a serious public health problem in the northeastern region of Thailand, entomological information on the Anopheles fauna and vectorial status of the species, especially those associated with increased malaria transmission in this endemic area, is lacking. In this region, Ubon Ratchathani Province recorded the highest number of malaria cases in Thailand between 2014 (n = 8836) and 2015 (n = 3327) (Bureau of Vector Borne Diseases, Ministry of Public Health, Thailand 2015). In view of the limited information on the anopheline fauna in this endemic area, the aim of the present study was to determine which Anopheles species are present and to identify which species may have vectored malaria in Na Chaluai District of the province.
Materials and methods
Study area and malaria cases
The study area was selected based on high malaria endemicity recorded by the Bureau of Vector Borne Diseases, Thai Ministry of Public Health, Thailand. Of the nine districts of Ubon Ratchathani Province, Na Chaluai District recorded the highest number of malaria cases (4103 out of 12,163), and P. vivax was the most common malarial parasite, compared to P. falciparum, during 2014−2015. Most of the malaria cases were Thai people and fewer than 20 cases were foreigners who had resided in the district for at least 6 months.
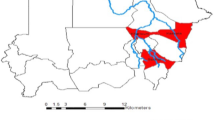
Anopheline mosquitoes were collected at a fixed location (wood hut) located in forest fringe near the Phu Chong Na Yoi National Park (14.43858○ N, 105.23485○ E), Ban Kaeng Ruang village (Fig. 1). The owner of this hut had a history of malaria caused by P. vivax during the study period. The hut is located about 5 km from the village and relatively far from the Thai-Cambodia and Thai-Lao PDR borders, about 12 km and 17 km, respectively. It is approximately 200 m above sea level and surrounded by forest, small rice fields, and cassava and rubber plantations. Most residents in Na Chaluai District are farmers who cut wood in the forest during the rainy and winter seasons.
Mosquito collection methods
Mosquito collections were conducted once monthly from January 2014 to December 2015 (24 months). Adult females were collected landing on the legs of two humans stationed indoors (HLI) and two stationed outdoors (HLO) during four consecutive nights from 1800 to 0600 hours each month. Hourly catches were placed in separate cups, provided with a cotton pad soaked with a 10% sugar solution, and transported to the laboratory. Ambient air temperature and relative humidity were recorded each hour of collection using a digital hygro-thermometer (DHT-1, Daeyoon Scale Industrial, South Korea). The collections encompassed the three Thai seasons, i.e. the hot-dry (March to May), wet (June to October) and cool-dry (November to February) seasons, based on data obtained from the local climatology division (code station 407021) located in Na Chaluai District. For more detailed analysis, biting was divided into four periods of activity: early evening (1800–2100 hours), late night (2100–2400 hours), pre-dawn (2400–0300 hours) and dawn (0300–0600 hour) (Tisgratog et al. 2012). The distance between indoor and outdoor collections was 100 m. Mosquitoes were collected with aspirators as they landed on the legs of the collectors. The collectors rested from collecting for 10 min each hour (Junkum et al. 2007).
Morphological mosquito identification and sample preparations
Each female mosquito was identified to species using available illustrated keys (Reid 1968; Harrison and Scanlon 1975; Rattanarithikul et al. 2006; Somboon and Rattanarithikul 2013), separated into head/thorax (T) and abdomen (A) parts and placed in labelled 1.5-ml microcentrifuge tubes for enzyme-linked immunosorbent assay (ELISA) detection of Plasmodium circumsporozoite proteins. Nested PCR was conducted on ELISA positive samples to confirm Plasmodium infection. The wings and legs of each mosquito were kept in separate 1.5-ml microcentrifuge tubes and immediately frozen at −20 °C for further analysis.
ELISA detection of Plasmodium sporozoites
Pools of one to 10 mosquitoes of the same species collected during the same hour were analysed for the presence of circumsporozoite (CSP) proteins of P. falciparum (Pf), P. vivax-210 (Pv-210) and P. vivax-247 (Pv-247) using the two-site sandwich ELISA of Wirtz et al. (1992). The positive controls and monoclonal antibody (MAB) for the ELISA were obtained from the Center for Disease Control and Prevention, Atlanta, USA. Each ELISA plate contained negative controls and an array of antigen standards to generate a standard curve and quantitatively estimate the amount of circumsporozoite antigen present in each sample. Briefly, the samples were ground in buffer to a final volume of 250 μl, with the pestle rinsed twice in PBS Tween solution. Each well was provided with 50 μl of PBS solution containing the capture antibody (2 μl/ml PBS), covered and stored overnight on a PVC U-shaped micro-titration plate. After 16 h, the solution containing monoclonal antibody was removed. The blocking buffer was added for 1 h, aspirated and 50 μl of mosquito homogenate was added to the control and testing wells for 2-h incubation. The plates were washed twice with PBS Tween solution, 50 μl peroxidase-conjugated antibodies (2 μg/ml blocking buffer) were added. The plates were then incubated for 1 h, subsequently washed three times with PBS-0.05% Tween 20 buffer, and 100 μl of peroxidase substrate was added to each well. Finally, the absorbance was measured at 405 nm in an ELISA reader for the suitable incubation periods: Pv-210 and Pf were read after 30 min of incubation and Pv-247 after 60 min. Specimens were considered positive if the absorbance value was twice that of the average of the negative controls. All positive samples were rerun for confirmation. Sporozoite rate was calculated using the proportion of mosquitoes found with malarial parasites divided by the number of mosquitoes tested.
Nested PCR for Plasmodium species differentiation
Genomic DNA derived from the abdomen of each positive sample was used for nested PCR to identify the Plasmodium species using the primers (Table 1) and conditions described by Kimura and Kawamoto (2000). For primary PCR, primers P1F and P2R were used as a genus-specific primer set corresponding to 18S rRNA. The product for this first reaction was then used as the DNA template for a second amplification reaction. For nested PCR, primers FR, MR, OR and VR were used as a reverse primer in the amplification reaction in which the oligonucleotide primer P1F and one of each reverse primer used recognises sequences contained within the DNA fragment amplified in the first reaction.
The first-strand PCR was conducted using 25 μl-volumes containing 12.5 μl of GoTaq Green mastermix (Promega, USA), 1 μl of each primer (P1F and P2R), 2 μl of the extracted DNA and 8.5 μl of ddH20. The amplification profile consisted of initial denaturation at 94 °C for 2 min, 35 cycles at 95 °C for 30 s, 60 °C for 90 s and 72 °C for 1 min, and a final extension at 72 °C for 5 min. The reaction mixture and thermal profile for the second amplification was the same as for the first one, except for the reverse species-specific primers (Table 1). Each amplification run contained a negative control, consisting of water. The amplified PCR products were analysed on 2% agarose gel by Gelstar and UV illumination.
Molecular mosquito identification
The CSP-positive Anopheles species were identified molecularly using allele-specific polymerase chain reaction (AS-PCR) following the protocols of Walton et al. (1999, 2007), with minor modifications. Genomic DNA was extracted from wings and legs of individual mosquitoes using PureLink® Genomic DNA Kits (Invitrogen, USA), according to the manufacturer’s recommendations. Specifically, species of the An. dirus complex were identified using the methods of Walton et al. (1999). Each PCR reaction was carried out using 25 μl-volumes containing 0.5 U of Taq DNA polymerase (Invitrogen, USA), 1X Taq buffer, 1.5 mM of MgCl2, 0.2 mM of each dNTP, 0.25 μM of each primer and 1 μl of the extracted DNA. The amplification profile consisted of an initial denaturation at 94 °C for 5 min, 35 cycles at 94 °C for 30 s, 53 °C for 30 s, 72 °C for 30 s and a final extension at 72 °C for 5 min. For An. philippinensis, each PCR reaction was performed using 25 μl-volumes containing 0.5 U of Taq DNA polymerase, 1X Taq buffer, 2.0 mM of MgCl2, 0.2 mM of each dNTP, 0.2 μM of each primer and 1 μl of the extracted DNA. The amplification profile included an initial denaturation at 94 °C for 5 min, 35 cycles at 94 °C for 1 min, 51 °C for 30 s, 72 °C for 30 s and a final extension at 72 °C for 5 min (Walton et al. 2007).
Data analysis
Landing-capture data were compared by non-parametric Kruskal-Wallis tests. All data were analysed using IBM SPSS statistics, version 22 for Windows (Chicago, SPSS Inc.). Statistical significance was set at P < 0.05.
Ethics approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and national research committee, the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All human participants in this study were approved by the Ethical Research Ethics Committee (PAR-2557−02417, No. 485/2014), Faculty of Medicine, Chiang Mai University, Chiang Mai Province, Thailand. Written consents were obtained from all human participants.
Results
Mosquito species composition
A total of 1229 Anopheles females belonging to 13 species were collected during the 2-year study, with the four most abundant taxa being An. barbirostris s.l. representing 38.41% of the mosquitoes collected, members of the An. hyrcanus group (17.66%), An. nivipes (17.49%) and An. philippinensis (11.72%) (Table 2). Of the 1229 mosquitoes, 1215 (98.86%) were collected outdoors and 14 (1.14%) were collected indoors.
Plasmodium detection by ELISA and nested PCR
A total of 668 pooled samples of heads/thoraces of female Anopheles mosquitoes were subjected to CSP-ELISA. Plasmodium-positive mosquitoes were found in individual samples of An. dirus and An. philippinensis. The infection rates were 3.45% (1/29) and 1.03% (1/97), respectively. Subsequently, the identities of the two positive samples, as well as the identities of other samples of An. dirus (n = 38) and An. philippinensis (n = 28), which had been identified based on morphology, were subsequently identified by AS-PCR. The results showed 100% concordance between morphological and molecular identification for both species. PCR diagnostic amplification products of 163 and 562 bp were recovered for An. philippinensis and An. dirus, respectively. Anopheles dirus had a mixed infection of Pv-210 and Pv-247, whereas An. philippinensis was positive for Pv-247 (Table 3). Additionally, the abdomen of An. dirus tested positive for P. vivax when analysed using nested PCR; however, the abdomen of An. philippinensis was negative when tested (Table 3).
Seasonal dynamics and potential role of An. dirus and An. philippinensis in malaria transmission
The two potential vectors, An. dirus and An. philippinensis, were further characterised to gain in-depth information on seasonal abundance and human biting activity. Included among the 1229 mosquitoes collected during the study, 144 (11.72%) were An. philippinensis and 38 (3.09%) were An. dirus (Table 2). No significant difference was observed in mean numbers captured in 2014 and 2015 (Kruskal-Wallis test = 2.111, df = 1, P = 0.146 for An. dirus and 0.712, df = 1, P = 0.399 for An. philippinensis) and also the mean numbers captured during the three seasons (Kruskal-Wallis test = 5.631, df = 2, P = 0.060 for An. dirus and 0.231, df = 2, P = 0.891 for An. philippinensis).
In 2014, An. dirus was found during most months of the year with peak density in the wet season (July, n = 11); it was not collected in the dry-season months of February, April, November and December. In comparison, the density of An. philippinensis peaked in the dry season during November and December (n = 39), with a minor peak in the hot-season month of March (n = 14) (Fig. 2); it was not collected in April and July. Rainfall was more extensive in 2015 than in 2014, with the wet season extending from June to October. The activity of An. dirus peaked in the wet season in September (n = 10) whereas An. philippinensis was collected in highest numbers in the hot season (May, n = 23), with some collected most months of the year (Fig. 3).
Regarding the potential role of An. dirus and An. philippinensis in malaria transmission, we determined the incidence of malaria during the 2-year study. In 2014, the number of malaria patients gradually increased from January with the highest numbers occurring during May and June, which corresponded with highest numbers of An. dirus collected landing on humans in the present study. Interestingly, although the number of malaria cases was lower during the dry season than during the wet season, CSP was detected in one sample of An. philippinensis that was captured among females collected in highest numbers during the dry season (December) (Fig. 2). In 2015, the overall number of malaria cases was lower than the previous year. The incidence of malaria was also different. High numbers of malaria cases were recorded from January to May. Although fewer numbers of both species were collected in 2015, one sporozoite-positive sample of An. dirus was detected in an outdoor collection made in the wet season, which corresponded with the peak number of females collected in September (Fig. 3). Remarkably, members of the An. minimus complex (n = 12) and the An. maculatus group (n = 32), which include primary malaria vectors, were collected in low numbers in outdoor collections while members of the An. barbirostris complex, which includes only secondary vectors, were collected in higher numbers during the wet and cool-dry seasons.
Feeding activity of An. dirus and An. philippinensis
The mean human-landing rates (HLI and HLO, measures of feeding activity) per person per night were 0.20 and 0.75 for An. dirus and An. philippinensis, respectively. Indoor and outdoor human-landing activity of An. dirus and An. philippinensis is shown in Figs 4 and 5. The results reveal that An. dirus prefers to attack humans outdoors. In 2014, only one female of An. dirus was collected indoors before bedtime (2000–2100 hours) (Fig. 4). The outdoor attach rate of An. dirus during the 2-year study was greatest during the first half of the night (1900–2300 hours) and very low after 2300 hours (2300−0300 hours). Anopheles philippinensis also mainly attacked humans outdoors. Similar to An. dirus, only two females of An. philippinensis were collected indoors between 2000 and 2400 hours in 2014 (Fig. 5). The observed patterns of outdoor attack rate of An. philippinensis were relatively similar for both years with greater numbers of females collected in the first year. Outdoor-landing (feeding) activity occurred in two major peaks, between 1900 and 2100 h and between 0100 and 0200 h (Fig. 5). In addition, the CSP-positive samples of both species were captured outdoors the hour before midnight (2300−2400 hours).
Discussion
Malaria remains one of the most important causes of morbidity and mortality among humans in Thailand. The epidemiological factors that may affect the transmission of malarial parasites includes the distributions of malaria vectors, their host preferences, biting activity, seasonal abundance, vector competence and capacity, and environmental change (e.g. dam and road construction, deforestation and development of plantations). Currently, there is a trend of changing malaria epidemiology in Thailand. In eastern Thailand, e.g. Sa Kaeo Province, P. vivax has replaced P. falciparum as the dominant cause of malaria, with its relative prevalence increasing to almost 90% in recent years. Likewise, nearly 4000 malaria cases have been reported in four provinces along the Thai-Malaysia border, where social conflicts are occurring.
More recently, the highest incidence of malaria has been reported in Ubon Ratchathani Province in northeastern Thailand. However, bionomic information about malaria vectors in this endemic area is scarcely available. Our findings open an avenue to explore the diversity of anopheline species, and provide insights for further investigation into the seasonal abundance and human-biting activity of potential malaria vectors in Na Chaluai District.
Among the sibling species of the An. dirus and An. minimus complexes and the An. maculatus group, the three principal malaria vector taxa in Thailand (Tainchum et al. 2015), only females of An. dirus were found naturally infected with human malarial Plasmodium in the present study. Gingrich et al. (1990) found 0.9% of An. dirus positive for P. falciparum and 0.4% for P. vivax in a malaria hyperendemic village in Chantaburi Province in eastern Thailand, and Frances et al. (1996) detected CSP of P. falciparum in 0.3% of An. dirus collected in the same region. In addition, Rosenberg and Andre (1985) reported that An. dirus was the only malaria vector in Chantaburi Province where 24% of the females collected during the dry season were infected with human Plasmodium. In the present study, only a few females of An. dirus were collected but one captured on human bait outdoors in the wet season was positive for a mixed infection of P. vivax (Pv-210 and Pv-247) based on ELISA and confirmation by PCR. This finding was consistent with the suggestions of Rosenberg et al. (1990) and Trung et al. (2004) that in areas where An. dirus is not dense, the species can maintain malaria transmission. Anopheles dirus is a very important vector in forested and hilly-forested areas of the country. However, it seems to have adapted to land-use change in Ubon Ratchathani Province where large areas of rice paddy were converted to rubber plantations (Yasuoka and Levins 2007).
Anopheles dirus is found in most areas of the country, especially in the northern, central and eastern regions. In this study, An. dirus was abundant during the rainy season, which is in agreement with the study reported by Peyton and Harrison (1979). Similar to the study of Rattanarithikul et al. (1996), our findings show that An. dirus exhibits anthropophilic and exophilic behaviour and has a peak of biting activity between 1900 and 2300 hours. Only one An. dirus was captured indoors, between 2000 and 2100 hours. During the present study, An. dirus exhibited a longer period of peak feeding activity than in the study of Sungvornyothin et al. (2009), who reported a short peak of feeding activity between 2000 and 2100 hour both indoors and outdoors based on human-landing collections conducted in Kanchanaburi Province in western Thailand. Numerous investigators have reported variation in human-biting activity in different regions of Thailand. For example, An. dirus in the central region showed a peak of biting activity between 2000 and 2400 hours (Wilkinson et al. 1970; Baimai et al. 1988), whereas it exhibited a peak between 2200 and 0100 hours in northwestern (Harbach et al. 1987) and southeastern Thailand (Rosenberg et al. 1990), and between 2400 and 0300 hours in southern areas of the country (Scanlon and Sandhinand 1965). Recently, Tananchai et al. (2012) reported short periods of indoor (1900–2000 hours) and outdoor (2300−0100 hours) biting activity for An. dirus in a malaria endemic area of western Thailand.
Anopheles philippinensis has been incriminated as a malaria vector in the northeastern states of Assam and Meghalaya in India (Prakash et al. 2006), and is considered to be the most important vector of malarial parasites in Bangladesh (Alam et al. 2012). The results of the present 2-year study revealed a major peak in the biting activity of An. philippinensis in the wet and dry seasons. Notably, a minor peak of biting activity was observed in March 2014, which agrees with the study conducted in Bangladesh by Bashar and Tuno (2014). Anopheles philippinensis females prefer to bite humans outdoors, with a pattern of activity similar to that of An. dirus but with a second peak of activity during the early morning hours. It is interesting to note that sporozoite-positive females of both species were captured in the wet and dry seasons, respectively, late at night. So far, An. philippinensis has been considered a suspected vector in Thailand since females have only been found positive for circumsporozoite antigens by ELISA (Rattanarithikul et al. 2006). In this study, a female of An. philippinensis collected in the dry season was found positive for P. vivax (Pv-247) based on the detection of CSP. However, An. philippinensis is morphologically very similar to An. nivipes and is often misidentified as that species based on characters of the wings, compounded by the coexistence of high populations. Thus, the identity of the CSP-positive sample of An. philippinensis required confirmation using AS-PCR. Basically, the recognition of a mosquito as a potential transmitter of malaria is dependent on the detection of Plasmodium sporozoites in the salivary glands (Somboon et al. 1994). CSP-ELISA has been widely used to determine sporozoite rates in mosquito vectors (Wirtz et al. 1992) and has proven to be specific, robust and inexpensive, but it is insensitive to low-level infections (Arez et al. 2000). To enhance sensitivity, therefore, the nested PCR assay was employed for Plasmodium detection (Snounou et al. 1993), and is recommended to reconfirm the results of CSP-ELISA (Durnez et al. 2011). Unfortunately, the CSP-positive sample of An. philippinensis that tested positive by ELISA was found to be negative by PCR, but this may have been due to a low concentration of DNA (Alam et al. 2012).
Unlike the study on the vectorial status of anophelines in a malaria endemic area in western Thailand (Sriwichai et al. 2016), the relatively few specimens of An. minimus s.l. and the An. maculatus group collected during the present study were negative for CSP. Harbach et al. (1987) reported that An. minimus and An. nivipes collected in Mae Tha Waw in Tak Province in northwestern Thailand were found to be naturally infected with P. falciparum and P. vivax, respectively, based on detection of CSP. Furthermore, Sriwichai et al. (2016) reported natural infections of P. vivax (Pv-210 and Pv-247) and P. falciparum in An. minimus s.l. and members of the An. maculatus group collected in six villages in Tak Province.
According to available records (Bureau of Vector Borne Diseases, Thai Ministry of Public Health, Thailand 2014), the number of malaria cases recorded in Ubon Ratchathani Province increased from 618 cases in 2013 to 8836 cases in 2014. Most cases were individuals 15–24 years of age, predominantly males (74%), the majority of which often worked in nearby forest (Imwong et al. 2015). Thus, the factors that influence this outbreak should be addressed and discussed for planning an effective control programme for disrupting malarial transmission. Petney et al. (2009) used data on changes in land-use patterns to predict the likelihood of malaria reemergence in northeastern Thailand. They documented that the planting of large tracts of rubber trees potentially increases the likelihood of the reemergence of malaria in northeastern Thailand. Rubber plantations develop dense undergrowth of vegetation and, therefore, high humidity and shade, which provide suitable environmental conditions for larval habitats for An. dirus, even during the dry season. Likewise, Obsomer et al. (2007) noted that during the rainy season, conditions at the edges of fragmented forests, where human settlements are often located, become favourable for larval habitats, rendering villagers susceptible to the disease. More recently, Lyttleton (2016) reported that deforestation, expansion of rubber plantations and improved surveillance or lack of access to resources are not potential factors that caused an outbreak of malaria in Ubon Ratchathani Province. The major cause of this outbreak was instead the market for the luxury timber trade, Siamese rosewood (Dalbergia cochinchinense) or Mai pha-yung (Thai Name), which boomed from 2013 to 2014.
In the present study, anopheline mosquitoes were collected at a single fixed location in a malaria endemic area of Ubon Ratchathani Province. This was a hot spot located in an area of forest fringe, chosen for its proximity to the forest where many persons are known to contract malaria while conducting illegal activities and later fostering subsequent transmission in villages that lie some distance from the forest. A single site was also chosen for logistical and security reasons, and because it lies on a transect between the village and the forest. The forest is part of the Phu Chong Na Yoi National Park, and research in the forest is limited by Park regulations and the need to avoid face to face encounters with individuals working illegally therein. Most of the malaria cases were Thai people and only 11 and 4 cases were M1 (residents more than 6 months, registered) and M2 (less than 6 months, unregistered/illegal) migrants, respectively. The higher proportion of Thai patients occurred during the entire study period. Most patients were farmers who cultivate rice and other crops, and cut rosewood in the forest. They usually stay in huts for 7–10 days while cutting wood, and are more highly exposed to malaria vectors. During the 2-year period, malaria cases were reported throughout each year, with higher numbers of malaria patients recorded during the hot-dry to rainy seasons. It is interesting to note that the peak numbers of malaria cases correspond to periods when humans are active in the forest, i.e. most villagers went into the forest (Phu Chong Na Yoi National Park) annually from March to April to harvest malva nuts (“Sum Rong”, Scaphium macropodium). This plant provides a traditional Chinese medicine used for treating fevers, phlegm, coughs and sore throats and respiratory conditions, and to improve general health. Likewise, villagers illegally cut wood in the forest during the rainy and winter seasons. In addition, the peak numbers of malaria patients were also compatible with the high densities of two known malaria vectors, An. dirus and An. philippinensis.
However, the vector competence of members of An. barbirostris complex requires further intensive investigation since their biting activity and population peaks co-occur with the forest activities of humans. Furthermore, species of the complex are considered to be secondary and potential vectors of malarial protozoa in other regions of Thailand (Sriwichai et al. 2016; Tainchum et al. 2015). In western Thailand, Coleman et al. (2002) reported finding two specimens of An. campestris naturally infected with P. vivax-210, and Rattanarithikul et al. (2006) detected circumsporozoite antigen of P. falciparum and P. vivax in An. barbirostris s.l. collected in the southern region of the country. Recently, An. wejchoochotei, a recently described species of the An. barbirostris complex, was identified as the potential vector of P. vivax in an experimental infection study (Thongsahuan et al. 2011). Additionally, Sriwichai et al. (2016) detected the presence of CSP of P. vivax-210 in An. barbirostris s.l. collected in Tak Province of western Thailand.
Conclusion
This study revealed evidence of natural infections of human plasmodia in An. dirus and An. philippinensis in a malaria endemic area in Ubon Ratchathani Province in northeastern Thailand. However, the role that An. philippinensis may play in transmission requires further investigation before its vector status is definitely established. Anopheles dirus and An. philippinensis both showed a propensity for attacking humans outdoors. Therefore, people who work and overnight in forests during both the wet and dry seasons require the use of personal protection as they are at high risk of malaria infection. The information on species composition, biting activity and the seasonal abundance of the potential vectors generated in this study will be of use for implementing malaria prevention and control programmes in the province.
References
Alam MS, Chakma S, Khan WA, Glass GE, Mohon AN, Elahi R, Norris LC, Podder MP, Ahmed S, Haque R, Sack DA, Sullivan DJ Jr, Norris DE (2012) Diversity of anopheline species and their Plasmodium infection status in rural Bandarban, Bangladesh. Parasit Vectors 5:150
Arez AP, Lopes D, Pinto J, Franco AS, Snounou G, do Rosário VE (2000) Plasmodium sp.: optimal protocols for PCR detection of low parasite numbers from mosquito (Anopheles sp.) samples. Exp Parasitol 94:269−272
Baimai V, Kijchalao U, Sawadwongporn P, Green CA (1988) Geographic distribution and biting behaviour of four species of the Anopheles dirus complex (Diptera: Culicidae) in Thailand. Southeast Asian J Trop Med Public Health 19:151−161
Bashar K, Tuno N (2014) Seasonal abundance of Anopheles mosquitoes and their association with meteorological factors and malaria incidence in Bangladesh. Parasit Vectors 7:442
Bureau of Vector Borne Diseases (2014) Annual Report 2014, Bureau of Vector Borne Diseases, Ministry of Public Health
Bureau of Vector Borne Diseases (2015) Annual Report 2015, Bureau of Vector Borne Diseases, Ministry of Public Health
Coleman RE, Sithiprasasna R, Kankaew P, Kiaattiut C, Ratanawong S, Khuntirat B, Sattabongkot J (2002) Naturally occurring infection of Plasmodium vivax VK210 and P. vivax VK247 in Anopheles mosquitoes (Diptera: Culicidae) in western Thailand. J Med Entomol 39:556–559
Corbel V, Nosten F, Thanispong K, Luxemburger C, Kongmee M, Chareonviriyaphap T (2013) Challenges and prospects for dengue and malaria control in Thailand, Southeast Asia. Trends Parasitol 29:623–633
Durnez L, Van Bortel W, Denis L, Roelants P, Veracx A, Trung HD, Sochantha T, Coosemans M (2011) False positive circumsporozoite protein ELISA: a challenge for the estimation of the entomological inoculation rate of malaria and for vector incrimination. Malar J 10:195
Frances SP, Klein TA, Wirtz RA, Eamsila C, Linthicum KJ (1996) Plasmodium falciparum and Plasmodium vivax circumsporozoite antigen in Anopheles collected in eastern Thailand. J Med Entomol 33:990–991
Gingrich J, Weatherhead A, Sattabongkot J, Pilakasiri C, Wirtz RA (1990) Hyperendemic malaria in Thai village: dependence of year-round transmission on focal and seasonally circumscribed mosquito (Diptera: Culicidae) habitats. J Med Entomol 27:1016–1126
Harbach RE (2017) Anopheles classification. Mosquito taxonomic inventory. http://mosquito-taxonomic-inventory.info/. Accessed 20 May 2017
Harbach RE, Gingrich JB, Pang LW (1987) Some entomological observations on malaria transmission in a remote village in northwestern Thailand. J Am Mosq Control Assoc 3:296–301
Harbach RE, Rattanarithikul R, Harrison BA (2017) Anopheles prachongae, a new species of the Gigas complex of subgenus Anopheles (Diptera: Culicidae) in Thailand, contrasted with known forms of the complex. Zootaxa 4236(1):65–81
Harrison BA, Scanlon JE (1975) Medical entomology studies II. The subgenus Anopheles in Thailand (Diptera: Culicidae). Contrib Am Entomol Inst 12(1):iv + 1–307
Imwong M, Jindakhad T, Kunasol C, Sutawong K, Vejakama P, Dondorp AM (2015) An outbreak of artemisinin resistant falciparum malaria in eastern Thailand. Sci Rep 5:17412
Junkum A, Pitasawat B, Tuetun B, Saeung A, Rattanachanpichai E, Jariyapan N, Komalamisra N, Mogi M, Chaithong U, Choochote W (2007) Seasonal abundance and biting activity of Anopheles aconitus (Diptera: Culicidae) in Chiang Mai, northern Thailand. Southeast Asian J Trop Med Public Health 38(Suppl 1):215–223
Kimura M, Kawamoto F (2000) PCR diagnosis of four human malaria parasites. The Toyota Foundation mini-symposium on malaria, Faculty of Tropical Medicine, Mahidol University, Bangkok
Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, Fan Q, Fang Q, Jongwutiwes S, Parker D, Sirichaisinthop J, Kyaw MP, Su XZ, Yang H, Yang Z, Wang B, Xu J, Zheng B, Zhong D, Zhou G (2012) Malaria in the greater Mekong subregion: heterogeneity and complexity. Acta Trop 121:227–239
Lyttleton C (2016) Deviance and resistance: malaria elimination in the greater Mekong subregion. Soc Sci Med 150:144–152
Manguin S, Garros C, Dusfour I, Harbach RE, Coosemans M (2008) Bionomics, taxonomy, and distribution of the major malaria vector taxa of Anopheles subgenus Cellia in Southeast Asia: an updated review. Infect Genet Evol 8:489–503
Obsomer V, Defourny P, Coosemans M (2007) The Anopheles dirus complex: spatial distribution and environmental drivers. Malar J 6:26
Petney T, Sithithaworn P, Satrawaha R, Grundy-Warr C, Andrews WYC, Feng CC (2009) Potential malaria reemergence, northeastern Thailand. Emerg Infect Dis 15:1330
Peyton EL, Harrison BA (1979) Anopheles (Cellia) dirus, a new species of the Leucosphyrus Group from Thailand (Diptera: Culicidae). Mosq Syst 11:40–52
Prakash A, Walton C, Bhattacharyya DR, Mohapatra PK, Mahanta J (2006) Characterization of ITS2 rDNA of Anopheles philippinensis and Anopheles nivipes (Diptera: Culicidae) from north-east India. Southeast Asian J Trop Med Public Health 37:1134–1138
Rattanarithikul R, Harrison BA, Harbach RE, Panthusiri P, Coleman RE (2006) Illustrated keys to the mosquitoes of Thailand IV. Anopheles. Southeast Asian J Trop Med Public Health 37:1–128
Rattanarithikul R, Konishi E, Linthicum KJ (1996) Detection of Plasmodium vivax and Plasmodium falciparum circumsporozoite antigen in anopheline mosquitoes collected in southern Thailand. Am J Trop Med Hyg 54:114–121
Reid JA (1968) Anopheline mosquitoes of Malaya and Borneo. Stud Inst Med Res Malaya 31:1–520
Rosenberg R, Andre RG (1985) Highly efficient, dry season transmission of malaria in eastern Thailand. Southeast Asian J Trop Med Public Health 16:188–189
Rosenberg R, Andre RG, Somchit L (1990) Highly efficient dry season transmission of malaria in Thailand. Trans R Soc Trop Med Hyg 84:22–28
Scanlon JE, Sandhinand J (1965) The distribution and biology of Anopheles balabacensis in Thailand (Diptera: Culicidae). J Med Entomol 2:61–69
Sinka ME, Bangs MJ, Manguin S, Chareonviriyaphap T, Patil AP, Temperley WH, Gething PW, Elyazar IR, Kabaria CW, Harbach RE, Hay SI (2011) The dominant Anopheles vectors of human malaria in the Asia-Pacific region: occurrence data, distribution maps and bionomic précis. Parasit Vectors 4:89
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, Thaithong S, Brown KN (1993) High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol 61:315–320
Somboon P, Rattanarithikul R (2013) Mosquito surveys, rearing, preservation of mosquito specimens and identification of Anopheles in Thailand. Bureau of Vector Borne Disease, Ministry of Public Health
Somboon P, Suwonkerd W, Lines JD (1994) Susceptibility of Thai zoophilic anophelines and suspected malaria vectors to local strains of human malaria parasites. Southeast Asian J Trop Med Public Health 25:766–770
Sriwichai P, Samung Y, Sumruayphol S, Kiattibutr K, Kumpitak C, Payakkapol A, Kaewkungwal J, Yan G, Cui L, Sattabongkot J (2016) Natural human Plasmodium infections in major Anopheles mosquitoes in western Thailand. Parasit Vectors 9:17
Sungvornyothin S, Kongmee M, Muenvorn V, Polsomboon S, Bangs MJ, Prabaripai A, Tantakom S, Chareonviriyaphap T (2009) Seasonal abundance and bloodfeeding activity of Anopheles dirus sensu lato in western Thailand. J Am Mosq Control Assoc 25:425–430
Tainchum K, Kongmee M, Manguin S, Bangs MJ, Chareonviriyaphap T (2015) Anopheles species diversity and distribution of the malaria vectors of Thailand. Trends Parasitol 31:109–119
Tainchum K, Ritthison W, Chuaycharoensuk T, Bangs MJ, Manguin S, Chareonviriyaphap T (2014) Diversity of Anopheles species and trophic behavior of putative malaria vectors in two malaria endemic areas of northwestern Thailand. J Vector Ecol 39:424–436
Tananchai C, Tisgratog R, Juntarajumnong W, Grieco JR, Manguin S, Prabaripai A, Chareonviriyaphap T (2012) Species diversity and biting activity of Anopheles dirus and Anopheles baimaii (Diptera: Culicidae) in a malaria prone area of western Thailand. Parasit Vectors 5:211
Thongsahuan S, Baimai V, Junkum A, Saeung A, Min GS, Joshi D, Park MH, Somboon P, Suwonkerd W, Tippawangkosol P, Jariyapan N, Choochote W (2011) Susceptibility of Anopheles campestris-like and Anopheles barbirostris species complexes to Plasmodium falciparum and Plasmodium vivax in Thailand. Mem Inst Oswaldo Cruz 106:105–112
Tisgratog R, Tananchai C, Juntarajumnong W, Tuntakom S, Bangs MJ, Corbel V, Chareonviriyaphap T (2012) Host feeding patterns and preference of Anopheles minimus (Diptera: Culicidae) in a malaria endemic area of western Thailand: baseline site description. Parasit Vectors 5:114
Trung HD, Van Bortel W, Sochantha T, Keokenchanh K, Quang NT, Cong LD, Coosemans M (2004) Malaria transmission and major malaria vectors in different geographical areas of Southeast Asia. Tropical Med Int Health 9:230–237
Walton C, Handley JM, Kuvangkadilok C, Collins FH, Harbach RE, Baimai V, Butlin RK (1999) Identification of five species of the Anopheles dirus complex from Thailand, using allele-specific polymerase chain reaction. Med Vet Entomol 13:24–32
Walton C, Somboon P, Harbach RE, Zhang S, Weerasinghe I, O'Loughlin SM, Phompida S, Sochantha T, Tun-Lin W, Chen B, Butlin RK (2007) Molecular identification of mosquito species in the Anopheles annularis group in southern Asia. Med Vet Entomol 21:30–35
WHO (2016) World malaria report 2016. WHO Global Malaria Programme
Wilkinson RN, Miller TA, Esah S (1970) Anthropophilic mosquitoes in central Thailand, with notes on Anopheles balabacensis Baisas and malaria. Mosq News 30:146–148
Wirtz RA, Sattabongkot J, Hall T, Burkot TR, Rosenberg R (1992) Development and evaluation of an enzyme-linked immunosorbent assay for Plasmodium vivax-VK247 sporozoites. J Med Entomol 29:854–857
Yasuoka J, Levins R (2007) Impact of deforestation and agricultural development on anopheline ecology and malaria epidemiology. Am J Trop Med Hyg 76:450–460
Author information
Authors and Affiliations
Corresponding author
Additional information
Atiporn Saeung and Udom Chaithong equal contributors
Rights and permissions
About this article
Cite this article
Poolphol, P., Harbach, R.E., Sriwichai, P. et al. Natural Plasmodium vivax infections in Anopheles mosquitoes in a malaria endemic area of northeastern Thailand. Parasitol Res 116, 3349–3359 (2017). https://doi.org/10.1007/s00436-017-5653-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-017-5653-1