Abstract
The aim of the present study is to explore the possibility to increase the efficacy of mebendazole (MBZ) against secondary cysts of Echinococcus granulosus harbored in mice by augmenting the solubility and bioavailability of the drug. Firstly, the saturated solubility of MBZ in nine kinds of oil was determined by high performance liquid chromatography (HPLC), and MBZ was found exhibiting the highest, secondary, and lowest solubility in oleic acid (OA), glycerol trioleate (GT), and soybean oil (SB), respectively. Secondly, MBZ-OA suspension, MBZ-GT suspension, MBZ-SB suspension, and MBZ suspended in 1 % tragacanth (MBZ-1 % tragacanth) were selected for further studies on pharmacokinetics and experimental therapy in mice. Four groups of mice were treated orally with one of aforementioned four MBZ preparations at a single dose of 25 mg/kg, and concentrations of MBZ in plasma obtained from each mouse at various intervals within 24 h postadministration were determined by HPLC. The major pharmacokinetic parameters calculated by MBZ plasma concentration–time curve demonstrated that the peak concentration of the drug (C max ) values obtained from three MBZ-oil preparation groups was 1.6–2.8 times higher than that of MBZ-1 % tragacanth group. The same was true that the area under the drug concentration–time curve (AUC0−∞) values of 19.8 (2.5)–28.2 (2.5) μg/ml × h revealed in the three MBZ-oil preparation groups was significantly higher than that of 11.6 (2.0) μg/ml × h in MBZ-1 % tragacanth group, and the bioavailability of the three MBZ-oil preparation groups was 71–143 % higher than that of MBZ-1 % tragacanth group. In mice infected with secondary cysts of E. granulosus for 8 months treated orally with MBZ-1 % tragacanth at a daily dose of 25 mg/kg for 14 consecutive days, the mean cyst weight was lower than that of untreated control, but the difference was not statistically significant with cyst weight reduction of 48 %. When the infected mice received three MBZ-oil preparations at the same oral dose schedule as aforementioned, the mean cyst weights were significantly lower than those in MBZ-1 % tragacanth group or control group with cyst weight reductions of 71.2–84.7 %. The results indicate that the solubility of MBZ in oils may increase to various degrees according to the kinds of oil used. Meanwhile, three MBZ-oil (OA, GT, and SB) preparations administered orally to mice not only improve the bioavailability of MBZ relative to that of MBZ suspended in 1 % tragacanth, but their effects against hydatid cysts also significantly enhance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic echinococcosis (CE), caused by metacestode of Echinococcus granulosus, is a serious zoonotic infection (Moro and Schantz 2009) that is detrimental to both human health and animal husbandry (Eckert et al. 2000; Eckert et al. 2001). The disease is endemic extensively in the world and remains an important public health problem in many regions of the world. In China, CE is prevalent mainly in western provinces and autonomous regions including Xinjiang, Sichuan, Qinghai, Gansu, Ningxia, and Inner Mongolia. However, cases of CE have also been reported in provinces of Yunnan, Heilongjiang, Shaanxi, Jilin, Shanxi, Hunan, and Hubei (Eckert et al. 2000; Wang et al. 2010; Jiang 2002; Ma et al. 2008). It is estimated currently that 50 million individuals are at the risk of acquiring Echinococcus, an infection with approximately 380,000 clinical cases (Chai 2009).
In humans, the cysts of E. granulosus metacestode are mainly located in the liver and lungs, accounting for at least 90 % of space-occupying lesions. However, the initial phase of proliferation of the parasite is always asymptomatic for many years or even permanently. Without effective treatment, the development of cysts will eventually results in organ malfunction and death (Spicher et al. 2008; Davis et al. 1989; Davis et al. 1986; Eckert et al. 2001). Until the initial 1980s, surgical operation had still been the only option for the treatment of CE, but this situation had a great change due to the discovery of mebendazole (MBZ) in mid-1970s and albendazole (ABZ) in mid-1980s (Morris et al. 1983; Heath and Chevis 1974), and application of the two benzimidazole derivatives in the treatment of hydatid disease. Particularly, in mid-1980s, WHO organized and coordinated twice multicenter clinical trials to assess and confirm the efficacy of MBZ and ABZ against echinococcosis, followed by recommendation of the both drugs used in treatment of human hydatid disease (Davis et al. 1986; Davis et al. 1989). By the end of last century, a new treatment approach, i.e., puncture, aspiration, injection and re-aspiration (PAIR), has been developed and applied increasingly or even replaced surgical intervention.
In order to have a better efficacy, the surgical treatment and PAIR are usually combined with MBZ or ABZ chemotherapy, and in inoperable patients and recrudescent cases, chemotherapy with MBZ and ABZ is the only option (Eckert et al. 2001). Nevertheless, according to the reports from the clinical trials organized by WHO and other subsequent clinical practices, the cure rates of MBZ and ABZ in treatment of CE were about 30 % (Eckert et al. 1995; Horton 1997; Jiang 1996; Vutova et al. 1999; Jamshidi et al. 2008). The therapeutic failures attributed to oral administration with both drugs have been primarily linked to the poor drug absorption rate resulting in low drug level in plasma and hydatid cysts (Daniel-Mwambete et al. 2004). In addition, the metabolism of MBZ in the liver to produce inactive metabolites could be another possible reason contributing to a reduction of the active drug level (Schantz et al. 1982). It was reported that the absolute bioavailability of oral MBZ at therapeutic level was less than 1.2 % (Braithwaite et al. 1982; Dawson et al. 1982; Dawson et al. 1985), suggesting that improvement of efficacy of MBZ could be achieved by increasing the bioavailability (Mueller et al. 1985; Dawson et al. 1985). On the other hand, experimental therapy proceeded in mice indicates that the effect of MBZ against metacestodes of E. granulosus is superior to ABZ, demonstrating that the parasite is more susceptible to MBZ than ABZ (Xiao et al. 1994; Xiao et al. 1990; Yang et al. 1992). Therefore, it is possible to enhance the efficacy of MBZ against echinococcosis through the development of new preparation with a higher bioavailability. Although oral administration of MBZ suspended in edible oil may increase its bioavailability and drug concentration in plasma (Chiba et al. 1991; Dzhabarova et al. 1989; Daniel-Mwuambete et al. 2003; Daniel-Mwambete et al. 2004), no further studies about these MBZ preparations were available. In the present study, we have prepared three kinds of MBZ-oil preparations and determined their solubilities and bioavailabilities, particularly, focusing on the impact of efficacy of MBZ in mice after the solubility and bioavailability of the drug are improved by the oil suspensions.
Materials and methods
Chemicals
Mebendazole powder with the purity over 99.0 % was purchased from Hanjiang Pharm. Co. (Hanzhong, China). MBZ standard and ABZ served as internal standard were purchased from Sigma-Aldrich Co. (St. Louis, USA). The glycerol trioleate, oleic acid ester oil, ethyl oleate, methyl oleate, oleic acid, soybean oil, sunflower oil, olive oil, and peanut oil were provided by Qianwei Oil Technology Co., Ltd. (Shanghai, China). All other chemicals were of the analytical pure grade.
Parasites, animals, and experimental infection
Liver hydatid cysts were obtained from newly slaughtered sheep at abattoirs in Xining City, Qinghai Province, China. Protoscolices of E. granulosus were collected aseptically from the cysts and were kept in cyst fluid at 4°C for no more than 3–4 days before use. Prior to infection, the collected protoscolices were rinsed 5–8 times with Hanks' balanced salt solution containing penicillin (500 U/ml) and streptomycin (500 U/ml). Kunming strain mice were purchased from SLAC Laboratory Animal (Shanghai, China). Among them, female mice, weighing 25–28 g, were used for pharmacokinetic study; while female mice with body weight of 18–22 g were used for experimental therapy. Animals were kept at the animal facility of our institute (Shanghai, China) and had free access to rodent food and tap water throughout the study. After 1 week acclimatization, the mice, applicable for chemotherapy, were inoculated intraperitoneally with 2,000 protocolices.
Solubility of MBZ in oils
An excessive MBZ was added to 10 ml glycerol trioleate, oleic acid, oleic acid ester oil, ethyl oleate, methyl oleate, sunflower oil, olive oil, peanut oil, and soybean oil in glass tubes. After vortex, the tubes were then kept at 25°C water bath for 24 h. Then the saturated solution was centrifuged at 13,000 rpm for 10 min, followed by filtration (0.45 μm membrane filter), dilution, and then assayed by high performance liquid chromatography (HPLC) to estimate the saturated solubility of MBZ in each kind of oil.
Plasma concentration of MBZ in mice treated with three MBZ-oil preparations
Mebendazole, suspended in oleic acid (MBZ-OA), glycerol trioleate (MBZ-GT), or soybean oil (MBZ-SB) at a concentration of 2.5 g/l (w/v), were served as oil suspensions; while MBZ, suspended in 1 % tragacanth (MBZ-1 % tragacanth) at the same concentration, was served as control. Mebendazole or albendazole suspended in 1 % tragacanth was usually applied in experimental treatment of mice infected with hydatid cysts (Xiao et al. 1994, 2002). The volume of each drug preparation administered to mice was 10 ml/kg. Ninety-six mice were divided equally into four groups, and three groups were administered orally with one of the three MBZ-oil preparations at a single dose of 25 mg/kg. The remaining one group of mice was treated orally with the same dose of MBZ-1 % trangacanth. Subgroups of three mice in each MBZ-oil preparation group were bled at 0.25, 0.5, 1, 2, 4, 8, 16, and 24 h postadministration. Plasma sample of each mouse was then separated from heparin-anticoagulated blood and stored at −20°C pending HPLC analysis. For MBZ assay, 0.5 ml plasma with ABZ as internal standard was extracted with Oasis HLB Cartridges (Waters, USA) according to the instruction. The final collection of methanol elution was dried and redissolved in methanol. All samples were filtrated with 0.45-μm membrane filter before injection.
Quantitative analysis by HPLC
The system of instrument consisted of a 1525 Binary HPLC Pumps, a 717 plus Autosampler, and a 2457 Dual λ Absorbance Detector (Waters, USA). The assay of MBZ, dissolved in various kinds of oils aforementioned or present in plasma-extracted samples of mice treated orally with three MBZ-oil preparations, was performed in a 5-μm C18 250 × 4.6 mm column (Beckman Coulter, USA) and a mobile phase containing 350 ml of 0.05 M ammonium sulfate and 650 ml of methanol at a flow rate of 1 ml/min. The MBZ concentration was measured by its absorbance at a wavelength of 289 nm.
Pharmacokinetic parameters
Using the noncompartmental model present in DAS 2.0 (Drug Analyze System, Shanghai University of T.C.M, China), the pharmacokinetic parameters of AUC0−∞ (the area under the drug concentration–time curve), C max (the peak concentration of the drug), MRT0−∞(mean residence time), Tmax (time to the drug peak concentration), and T1/2 (half-life) were estimated.
Effect against secondary cysts of E. granulosus
Ninety mice inoculated with E. granulosus proscolices for 8 months were divided into five groups of 16–21 mice. Four groups were treated orally with MBZ-OA, MBZ-GT, MBZ-OB, and MBZ-1 % tragacanth, respectively, at a daily dose of 25 mg/kg for 14 consecutive days. The remaining one group of 21 infected but untreated mice served as control. The mice were sacrificed 2 weeks posttreatment. The cysts in the peritoneal cavity were isolated and removed for weighing. The efficacy was assessed by mean cyst weight and mean cyst weight reduction calculated by the following formula:
Statistical analysis
The difference of pharmacokinetic parameters between one of each three MBZ-oil preparations and MBZ-1 % tragacanth was analyzed using LSD Duncan test. The statistical differences in mean cyst weight between each treated group and control group, or between each two treated groups, were analyzed by nonparametric method (Mann–Whitney test) in SPSS 17.0.
Results
Solubility of MBZ in various kinds of oil
As shown in Table 1, among the nine oil solutions of MBZ, the highest solubility of MBZ was 329.4 ± 9.7 μg/ml revealed in the compound dissolved in oleic acid, while the next one of 54.1 ± 1.9 μg/ml was seen in the compound dissolved in glycerol trioleate. The solubilities of the other seven MBZ-oil solutions were similar at a range of 12–20 μg/ml, and the lowest solubility of 12.1 ± 0.2 μg/ml was seen in MBZ dissolve in soybean oil. In addition, the solubility of MBZ in 1 % tragacanth (MBZ-1 % tragacanth) was 5.5 ± 0.7 μg/ml (Table 1). According to aforementioned results, oleic acid, glycerol trioleate, and soybean oil, which possess high, medium, and low solubility of MBZ, respectively, were selected for further study, and 1 % tragacanth served as control.
Pharmacokinetics measured in mice administered orally with three MBZ-oil preparations and MBZ-1 % tragacanth
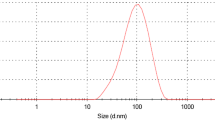
MBZ concentration in plasma of mice
MBZ absorption amount in plasma of mice treated orally with MBZ-OA, MBZ-GT, MBZ-SB, or MBZ-1 % tragacanth at a single dose of 25 mg/kg were showed in Figure 1. After the mice were treated orally with MBZ-1 % tragacanth at a single dose of 25 mg/kg, the highest MBZ concentration of 1.3 μg/ml was seen in plasma 4 h posttreatment. Thereafter, the MBZ levels in plasma declined significantly and maintained in low levels for longer periods of time up to 24 h. On the other hand, highest MBZ concentrations of 3.0–4.8 μg/ml, which were significantly higher than that of MBZ-1 % tragacanth, emerged in plasma of mice after oral administration of MBZ-OA, MBZ-GT, and MBZ-SB at the same single dose. Although the time reaching to the highest plasma concentrations of MBZ after the mice received the three MBZ-oil preparations was similar, or somewhat delayed relative to MBZ-1 % tragacanth, decline of the drug concentration in plasma was slow at 4–15 h posttreatment. Meanwhile, the plasma concentration of MBZ in each time point during this period was significantly higher than that of MBZ-1 % tragacanth (P < 0.05). Particularly, higher MBZ concentration of 0.8 μg/ml was seen in plasma in mice that received the MBZ-OA upon 24 h.
Pharmacokinetic parameters
According to the MBZ concentration–time curve obtained by measurement of plasma from mice treated orally with aforementioned three MBZ-oil preparations and MBZ-1 % tragacanth at a single dose of 25 mg/kg, the major pharmacokinetic parameters of MRT0−∞, T 1/2, T max, C max, and AUC0−∞ were calculated and listed in Table 2. The results showed that the values of T 1/2 or T max in each group were somewhat higher or lower, but differences between each of the three MBZ-oil preparation groups and MBZ-1 % tragacanth group, or each two of the three MBZ-oil preparation groups, were not statistically significant (P > 0.05). It was found that in mice treated with MBZ-OA, the MRT0−∞ was longer than that of MBZ-1 % tragacanth, but the difference between these two groups was not statistically significant. In contrast, administration of MBZ-GT and MBZ-SB to mice resulted in significantly shortened MRT0−∞ compared to MBZ-1 % tragacanth (P < 0.05, Table 2). As to C max, the values obtained from three MBZ-oil preparation groups were 3.32 ± 0.56 μg/ml, 4.84 ± 0.55 μg/ml, and 4.42 ± 1.96 μg/ml, respectively, and each of them was significantly higher than that of 1.28 ± 0.42 μg/ml in MBZ-1 % tragacanth group (P < 0.05 or <0.01, Table 2). Although the C max value of MBZ-GT group was higher than that of other two MBZ-oil preparation groups, the differences of C max between each two of three MBZ-oil preparation groups were not statistically significantly (P > 0.05, Table 2). Finally, the values of AUC0−∞ obtained from three MBZ-oil preparation groups were 1.70–2.43 times higher than that of MBZ-1 % tragacanth group, which also represented the relative bioavailability of the three MBZ-oil preparations (Table 2), and the differences of AUC0−∞ between each of three MBZ-oil preparation groups, and MBZ-1 % tragacanth group were statistically significant (P < 0.01, Table 2). Meanwhile, the AUC0−∞ of 28.2 ± 2.5 μg/ml × h in MBZ-OA group was higher than that of 25.1 ± 4.4 μg/ml × h in MBZ-SB group and 19.8 ± 2.5 μg/ml × h in MBZ-GT group, but the differences of AUC0−∞ between each two of three MBZ-oil preparation groups were not statistically significant.
Effect against secondary cysts of E. granulosus
In four groups of mice infected with hydatid cysts and treated orally with MBZ-OA, MBZ-GT, MBZ-SB, or MBZ-1 % tragacanth at a daily dose of 25 mg/kg for 14 days, the mean cyst weights of the three MBZ-oil preparations were significantly lower than that of control group (P < 0.05 or 0.01) with mean cyst weight reductions of 71.5 %, 71.2 %, and 84.7 %, respectively, whereas the mean cyst weight of MBZ-1 % tragacanth group was not statistically lower than that of control (P > 0.05) with cyst weight reduction of 48.9 % (Table 3). Meanwhile, the differences of mean cyst weights between each of the three MBZ-oil preparation groups and MBZ-1 % tragacanth group were also statistically significant (P < 0.05 or 0.01). Although the mean cyst weight reduction of MBZ-SB group was higher than that of the other two MBZ-oil preparation groups, no difference was seen in mean cyst weight between MBZ-SB group and one of the other two MBZ-oil preparation groups (P > 0.05).
Discussion
As we know, MBZ was developed primarily to target parasite in the gastrointestinal tract. For this reason, low bioavailability outside the intestine was considered important for the treatment of the drug. However, in order to effectively treat hydatid cysts in the tissue of animal and humans, this feature is inappropriate since the solubility and permeability of the drug are associated directly to the drug absorption in gastrointestinal tract (Dressman and Reppas 2000), which may impact on the bioavailability of the drug. MBZ is a substance difficult to dissolve in water and various solvents, and only 1/10 of the drug administered orally to the patients could be absorbed with a very low bioavailability (Keystone and Murdoch 1979). Meanwhile, the low bioavailability is considered to link to the low cure rate in treatment of hydatid disease with MBZ (Dawson et al. 1985; Ceballos et al. 2008). Under this background, we have tried to determine the solubility of MBZ in various kinds of oils in order to develop new MBZ preparation with higher bioavailability
Our results showed that the solubilities of MBZ increased to various degrees in nine kinds of oil, and three of them, i.e., oleic acid, glycerol trioleate, and soybean oil showing high, medium, or low solubility of MBZ, have been selected to prepare the drug-oil preparations for further study. Indeed, the bioavailabilities of the three MBZ-oil preparations possessed similar improvement, and they were significantly higher than that of MBZ-1 % tragacanth. Although the solubility of MBZ in OA was five and 26 times higher than that in GT and SB, respectively, the increase in bioavailabilties of the three MBZ-oil preparations was not proportional to the degrees of MBZ solubility in the three kinds of oil. Generally, T max is a parameter relevant to the rate of drug absorption; but in our experiment, the T max values of the three MBZ-oil preparations were somewhat lower or higher, accompanied by no significant differences in T max values between each two of the three MBZ-oil preparations. Meanwhile, their C max and AUC0−∞ values were also similar. The results suggest that increase in solubility of MBZ in the solvent is helpful to enhance the bioavalability of MBZ, but the absorption rate and amount of the drug absorbed may also be restricted by other factors, especially the absorption mechanism from the host (Bekhti et al. 1986). Similar results have been seen in the study on the intestinal absorption of albendazole oil surfactant suspension or its cyclodextrin solutions in humans (Rigter et al. 2004; Daniel-Mwambete et al. 2004).
The results from experimental therapy showed that the three MBZ-oil preparations possessed similarily potential effect against hydatid cysts in mice, and this probably associated in maintaining the higher MBZ levels in plasma for about 15 h postadministration, which was similar to the manifestation of mice following administration of soybean oil-emulsified albendazole (Xiao et al. 2002). It deserved to be noted that among the three groups treated with the three MBZ-oil preparations, the highest cyst weight reduction accompanied by many collapsed cysts was seen in MBZ-SB group. Since soybean oil is a mixture of several fats in a form of esters vitamin E and vitamin K (Jaselskis et al. 1982; Clemente and Cahoon 2009), whether these components display some auxiliary role in combination with MBZ during the treatment remained to be further elucidated. Overall, the findings revealed in the present study clearly point out that increase in solubility of MBZ to an appropriate level in oil to develop the new preparation for treatment of hydatid disease is necessary, but it is not suitable to pursue the high solubility of MBZ in the solvent.
References
Bekhti A, Pirotte J, Woestenborghs R (1986) A correlation between serum mebendazole concentrations and the aminopyrine breath test. Implications in the treatment of hydatid disease. Br J Clin Pharmacol 21:223–226
Braithwaite PA, Roberts MS, Allan RJ, Watson TR (1982) Clinical pharmacokinetics of high dose mebendazole in patients treated for cystic hydatid disease. Eur J Clin Pharmacol 22:161–169
Ceballos L, Elissondo C, Moreno L, Dopchiz M, Sanchez Bruni S, Denegri G, Alvarez L, Lanusse C (2008) Albendazole treatment in cystic echinococcosis: pharmacokinetics and clinical efficacy of two different aqueous formulations. Parasitol Res 103:355–362
Chai JJ (2009) Echinococcosis control in China: challenges and research needs. Chin J Parasitol Parasit Dis 27:379–383
Chiba Y, Kohri N, Iseki K, Miyazaki K (1991) Improvement of dissolution and bioavailability for mebendazole, an agent for human echinococcosis, by preparing solid dispersion with polyethylene glycol. Chem Pharm Bull (Tokyo) 39:2158–2160
Clemente TE, Cahoon EB (2009) Soybean oil: genetic approaches for modification of functionality and total content. Plant Physiol 151:1030–1040
Daniel-Mwambete K, Torrado S, Cuesta-Bandera C, Ponce-Gordo F, Torrado JJ (2004) The effect of solubilization on the oral bioavailability of three benzimidazole carbamate drugs. Int J Pharm 272:29–36
Daniel-Mwuambete K, Ponce-Gordo F, Torrado J, Torrado S, Cuesta-Bandera C (2003) Effect of two formulations of benzimidazole carbamates on the viability of cysts of Echinococcus granulosus in vivo. Parasite 10:371–373
Davis A, Pawlowski ZS, Dixon H (1986) Multicentre clinical trials of benzimidazolecarbamates in human echinococcosis. Bull World Health Organ 64:383–388
Davis A, Dixon H, Pawlowski ZS (1989) Multicentre clinical trials of benzimidazole-carbamates in human cystic echinococcosis (phase 2). Bull World Health Organ 67:503–508
Dawson M, Allan RJ, Watson TR (1982) The pharmacokinetics and bioavailability of mebendazole in man: a pilot study using [3H]-mebendazole. Br J Clin Pharmacol 14:453–455
Dawson M, Braithwaite PA, Roberts MS, Watson TR (1985) The pharmacokinetics and bioavailability of a tracer dose of [3H]-mebendazole in man. Br J Clin Pharmacol 19:79–86
Dressman JB, Reppas C (2000) In vitro-in vivo correlations for lipophilic, poorly water-soluble drugs. Eur J Pharm Sci 11(Suppl 2):S73–80
Dzhabarova VI, Dobrotvorskii AE, Krotov AI (1989) Experimental chemotherapy of alveolar hydatid disease. 12. The efficacy of drug forms of mebendazole and nocodazole with high bioavailability. Med Parazitol (Mosk)43-46
Eckert J, Pawlowski Z, Dar FK, Vuitton DA, Kern P, Savioli L (1995) Medical aspects of echinococcosis. Parasitol Today 11:273–276
Eckert J, Conraths FJ, Tackmann K (2000) Echinococcosis: an emerging or re-emerging zoonosis? Int J Parasitol 30:1283–1294
Eckert J, Gemmell MA, Meslin FX, Pawlowski ZS (2001) WHO/OIE Manual on echinococcosis in humans and animals: a public health problem of global concern. Paris: Office International des Epizooties:21-72
Heath DD, Chevis RA (1974) Letter: mebendazole and hydatid cysts. Lancet 2:218–219
Horton RJ (1997) Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Acta Trop 64:79–93
Jamshidi M, Mohraz M, Zangeneh M, Jamshidi A (2008) The effect of combination therapy with albendazole and praziquantel on hydatid cyst treatment. Parasitol Res 103:195–199
Jaselskis B, Stemm NL, Johnston WD (1982) Determination of the fatty-acid composition of soybean oil by high-pressure liquid chromatography. Talanta 29:54–56
Jiang CP (1996) Preliminary clinical obserations on mebendazole and traditional Chinese medicine treatment in 57 cases with echinococcosis. Chin J Parasitol Parasit Dis 4:209–210
Jiang CP (2002) Today's regional distribution of echinococcosisi in China. Chin Med J 115:1244–1247
Keystone JS, Murdoch JK (1979) Mebendazole. Ann Intern Med 91:582–586
Ma SM, Maillard S, Zhao HL, Huang X, Wang H, Geng PL, Bart JM, Piarroux R (2008) Assessment of Echinococcus granulosus polymorphism in Qinghai province, People's Republic of China. Parasitol Res 102:1201–1206
Moro P, Schantz PM (2009) Echinococcosis: a review. Int J Infect Dis 13:125–133
Morris DL, Dykes PW, Dickson B, Marriner SE, Bogan JA, Burrows FG (1983) Albendazole in hydatid disease. Br Med J (Clin Res Ed) 286:103–104
Mueller PR, Dawson SL, Ferrucci JT Jr, Nardi GL (1985) Hepatic echinococcal cyst: successful percutaneous drainage. Radiology 155:627–628
Rigter IM, Schipper HG, Koopmans RP, van Kan HJ, Frijlink HW, Kager PA, Guchelaar HJ (2004) Relative bioavailability of three newly developed albendazole formulations: a randomized crossover study with healthy volunteers. Antimicrob Agents Chemother 48:1051–1054
Schantz PM, Van den Bossche H, Eckert J (1982) Chemotherapy for larval echinococcosis in animals and humans: report of a workshop. Parasitol Res 67:5–26
Spicher M, Roethlisberger C, Lany C, Stadelmann B, Keiser J, Ortega-Mora LM, Gottstein B, Hemphill A (2008) In vitro and in vivo treatments of echinococcus protoscoleces and metacestodes with artemisinin and artemisinin derivatives. Antimicrob Agents Chemother 52:3447–3450
Vutova K, Mechkov G, Vachkov P, Petkov R, Georgiev P, Handjiev S, Ivanov A, Todorov T (1999) Effect of mebendazole on human cystic echinococcosis: the role of dosage and treatment duration. Ann Trop Med Parasitol 93:357–365
Wang LY, Wu WP, Zhu XH (2010) The endemic status of hydatidosis in China from 2004 to 2008. Chin J Zoonoses 26:699–702
Xiao SH, You JQ, Jiao PY, Guo HF (1990) Studies on the effects of mebendazole, albendazole and their metabolites in an experimental therapy of mice infected with secondary cysts of Echinococcus granulosus. Endem Dis Bull 5:11–19
Xiao SH, Yang YQ, You JQ, Shen BG, Jiao W, Chai JJ (1994) Effects of benzimidazole compounds on mice infected with secondary cysts of Echinococcus granulosus. Chin Med J (Engl) 107:521–532
Xiao SH, You JQ, Wang MJ, Jiao PY, Gao FH, Chai JJ, Jiao W, Hotez P (2002) Augmented bioavailability and cysticidal activity of albendazole reformulated in soybean emulsion in mice infected with Echinococcus granulosus or Echinococcus multilocularis. Acta Trop 82:77–84
Yang YQ, Zhang CW, Xiao SH (1992) Histological comparison of the effects of praziquantel, mebendazole and albendazole on Echinococcus granulosus Cyst in Vivo and in Vitro. Endem Dis Bull 5:17–20
Acknowledgments
We are most grateful to Qinghai Institute for Endemic Disease Prevention and Control for their kind provision with protoscolices. We are also grateful to Professor Xiao Shuhua for his advice and help in preparing this manuscript. This investigation was funded by International collaboration on drug and diagnostics innovation of tropical diseases in PR China (International S&T Cooperation 2010DFB73280) and special funds of technology development research for science research institute (2011EG150312).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Cs., Zhang, Hb., Jiang, B. et al. Enhanced bioavailability and cysticidal effect of three mebendazole-oil preparations in mice infected with secondary cysts of Echinococcus granulosus . Parasitol Res 111, 1205–1211 (2012). https://doi.org/10.1007/s00436-012-2954-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-012-2954-2