Abstract
Schistosomiasis is an endemic disease in 74 countries causing more than 250,000 deaths every year. Accordingly, the development of an effective drug for eradication of schistosomiasis is an open research field. The current chemotherapy for control is praziquantel (PZQ). However, PZQ does not improve liver fibrosis. Therefore, the aim of this study is to evaluate the combined effect of alpha lipoic acid (ALA) with PZQ on the liver fibrosis induced by Schistosoma mansoni challenged mice. Evaluation was based on the worm burden count, ova load, granuloma size, and histopathology of the liver. Reduced glutathione (GSH) was measured in the tissue as a biomarker for impaired antioxidant function. Malondialdehyde (MDA) was also measured in the tissue as a biomarker for oxidative stress. The serum level of matrix metalloproteinase 1 was measured as a biomarker for fibrotic status of the liver. Liver function enzymes such as ALT, AST, and GGT were also measured. Four groups of ten mice each were used in this study. The first group was infected with 50 ± 10 S. mansoni cercariae. The second group was also infected and was treated with PZQ 9 weeks post-infection (PI). The third group was treated with PZQ and ALA 9 weeks PI. The fourth group was used a healthy control. The present study revealed remarkable improvement in all parameters measured (parasitological and biochemical) as well as significant improvement of hepatic pathology in the third group which was treated with PZQ and ALA. The treatment of mice with PZQ and ALA results in reduction in the worm burden, egg count, and granuloma size. Furthermore, this combined treatment increased the tissue level of the antioxidant (GSH) and decreased the tissue level of MDA in this group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schistosomiasis is a parasitic disease caused by infection with the helminth Schistosoma species. The arrival of eggs in the liver during Schistosoma mansoni infection initiates a protective granulomatous response. However, as the infection progresses, this response results in chronic liver fibrosis (Harvie et al. 2007), a central event in progressive liver disease. This leads to cirrhosis, and associated morbidity and mortality caused by decompensation. Liver fibrosis is the result of an imbalance between synthesis and degradation of extracellular matrix proteins of the liver (Zou et al. 2007).
Non-invasive diagnosis of liver fibrosis is clinically important. Therefore, measuring some laboratory parameters is a valid method for evaluating the state of liver fibrosis. This research focuses on the interstitial enzyme matrix metalloproteinase-1 (MMP-1). MMP-1 is secreted mainly by Kupffer cells and hepatocytes. It is present as an inactive proMMP-1 and is activated extracellularly by proteolytic enzymes (Murawaki et al. 1999). The decrease in the serum level of MMP-1 during progressive fibrosis is attributed to the decrease of its synthesis in the liver (Murawaki et al. 1999; Zhang et al. 2003).
Schistosomiasis is associated with liberation of free radicals and disturbance in the cellular antioxidant system. Much interest has been focused on compounds that are capable of stimulating glutathione synthesis and acting as antioxidants (Abdallahi et al. 1999; Gharib et al. 1999). One of these compounds which possesses antioxidative and cytoprotective properties is alpha lipoic acid (ALA).
ALA is accessible to all parts of the cell, giving it tremendous ability to trap free radicals throughout. ALA is one of the very few substances capable of crossing the blood–brain barrier. Therefore, the supplementation of ALA causes increasing levels of reduced glutathione, which helps the body to dispose of toxins. In fact, ALA is an antioxidant similar to other antioxidants such as vitamins C and E, with a unique ability to regenerate itself. Accordingly, ALA can continue destroying free radicals. Thus, ALA is known as a network antioxidant (Biewenga et al. 1997). For many years, ALA has been used as a pharmacological agent without serious side effects. Therefore, oral and intravenous applications as well as its bioavailability are well established (Dünschede et al. 2006). Furthermore, ALA was shown to be hepatoprotective, improve liver circulation, and treat chronic liver diseases, such as jaundice, hepatitis, cirrhosis, and hepatic coma (Horáková et al. 1967; Möller et al. 1967; Iasinovskii et al. 1969; Ivkov 1969; Dabski and Brzeski 1970; Romanov 1971). Therefore, in this study, we aimed to evaluate the influence of combined treatment of PZQ with ALA on liver fibrosis induced by S. mansoni challenged mice.
Materials and methods
Animals
Eight-week-old male Balb/c mice weighing 18–22 g each were provided by the Schistosome Biology Supply Center (SBSC), Theodor Bilharz Research Institute (TBRI), Cairo, Egypt. After infection, the mice were housed in standard acclimatized animal house conditions (12 h lighting cycle and 25 ± 2°C temperature). The animals had free access to standard rodent chow and water. All experimental procedures were conducted according to the ethical standards approved by the Institutional Animal Ethics Committee guidelines for animal care and use, Minia University, Egypt.
Experimental design
The animals were divided into four groups of 10 mice each. The first group was infected with 50 ± 10 S. mansoni cercariae (Egyptian strain) by the tail immersion technique (Oliver and Stirewalt 1952). This group was not treated. The second group was infected with 50 ± 10 S. mansoni cercariae. Nine weeks post-infection (PI), this group was treated with a suspension of PZQ (Distocide; E.I.P.I. Co. Pharmaceuticals, Cairo, Egypt) in PBS (pH 7.4) using a dose of 500 mg/kg (Morsy 2009). PZQ was given intragastrically in two divided doses in the same day. The third group was infected with 50 ± 10 S. mansoni cercariae. At 9 weeks PI, this group was treated intragastrically with PZQ (same dose as the second group) in combination with a suspension of α-lipoic acid (Eva Pharma Company, Cairo, Egypt) with a single dose of 30 mg/kg daily for 2 months. Supplementation dose of ALA was determined according to Melhem et al. (2001), initially 400 mg/kg to maintain an average daily ALA consumption. The fourth group was used as a normal healthy control.
Parasitological parameters
At 10 weeks post-treatment (PT), all animals were sacrificed and were perfused. Liver perfusion was done as described by Smithers and Terry (1965) and Duvall and DeWitt (1967). Worms recovered from perfusion were collected and counted. The percentage of worm reduction after treatment was calculated by the method of Tendler et al. (1968). The anti-schistosomal effect of the drugs was assessed parasitologically by determining the S. mansoni worm load and the tissue egg loads (Cheever 1968).
Egg counts
A portion of the liver was digested in 3% KOH at 37°C for 24 h. The egg number counted in one tenth of the digested fluid was evaluated to determine the total number of eggs (viable and dead) per gram of tissue. The number was determined according to the method of Pellegrino et al. (1962).
Tissue homogenate of liver
Part of the liver tissue was homogenized in a PBS (pH 7.5) buffer with protease inhibitor by using a homogenizer (Tri-R Stir-R, Model K 41). Centrifugation was done at 4,000 rpm for 15 min at 4°C. The supernatant was stored at −80°C until use for estimation of reduced glutathione (GSH) and malondialdehyde (MDA).
Blood collection
Blood was collected and serum was separated by centrifugation at 1,500 rpm for 10 min. Serum samples were stored at −20°C until use for estimation of concentrations of MMP-1. Also, liver function enzymes such as ALT (alanine aminotransferase or SGPT), AST (aspartate aminotransferase or SGOT), and GGT (gamma-glutamyltransferase) were measured.
Biochemical analysis
The serum levels of ALT, AST, and GGT were quantified according to the manufacturers' guidelines using commercially available UV/colorimetric kits (Human GmbH, Germany). The serum level of MMP-1 was determined using ELISA Kits according to manufacturer’s instructions (Uscn Life Science Inc., Wuhan, China). The hepatic GSH level was quantified according to the manufacturers' guidelines using commercially available kits (Biodiagnostic, Egypt). The hepatic MDA level was determined as thiobarbituric acid reacting substance using 1, 1, 3, 3-tetramethoxypropane as the standard (Buege and Aust 1978).
Histopathology
Liver biopsies were fixed in formalin (10%) and embedded in paraffin. Five-micrometer sections were cut and stained with hematoxylin and eosin (H and E) stain according to Hirsch et al. (1997) for evaluation of liver pathology. Masson trichrome stain was performed to examine the histopathological changes and to measure the diameters of hepatic granulomas using an ocular micrometer. Only the granulomas around single eggs were measured. Cell composition of granulomas was also investigated. The granulomas were classified into cellular (inflammatory) or regressive (showing resolution) ones as described by Junqueira et al. (1986).
Immunohistochemistry
The standard avidin–biotin immunoperoxidase technique was used as described by Hsu et al. (1981) and the procedures are outlined below. Paraffin sections (5-μm thick) were dewaxed in xylene and hydrated in descending grades of ethanol. The endogenous peroxidase activity was quenched by incubation in 100% methanol with 3% hydrogen peroxide for 20 min. Antigen retrieval was performed by incubating the sections in citrate buffer (pH 6.0) for 15 min in a humid chamber at 22°C. Sections were incubated overnight at 4°C in a humid chamber with primary antibody against MMP-1 (Abcam Company, UK). The antibody was diluted 1: 50 in PBS. After rinsing in PBS, the sections were incubated at 22°C for 15 min with biotinylated secondary anti-mouse antibody (Vector Laboratories Inc., CA, USA). Further washing in PBS was done. Subsequently, the slides were incubated with an avidin–biotin complex horseradish peroxidase solution (Vector Laboratories). After 10 min of incubation, the peroxidase reaction was developed using 0.01% hydrogen peroxide in 0.05% diaminobenzidine tetrahydrochloride (DAB). Sections were counterstained with Meyer’s hematoxylin and dehydrated in ethanol prior to mounting. Liver sections, with the primary antibody replaced with PBS, were used as negative controls and examined by light microscopy.
Statistical analysis
Results of studies are reported as mean ± standard deviation (SD). Data were entered and analyzed using SPSS version 16 for Windows. Non-parametric statistics were used throughout the analysis. The significance of the difference between two groups was assessed using Mann–Whitney's U statistic. The P value was considered significant when it was less than 0.05.
Results
Parasitological parameters
The experimental results revealed that the group of mice treated with PZQ + ALA significantly enhances the decrease in the total worms number of worm burden (P < 0.00001; 6.13 ± 1.89 vs. 36.50 ± 10.78), the total egg count (P < 0.0001; 15.00 ± 2.97 vs. 46.39 ± 14.17), and the hepatic granuloma diameter (P < 0.0001; 86.13 ± 1.89 vs. 230.50 ± 12.78) when compared to the group of mice infected without treatment (Table 1). However, the decrease in the total worm burden in the group of mice treated with PZQ and ALA (P < 0.06; 6.13 ± 1.89 vs. 7.63 ± 1.49) was statistically insignificant when compared to the group infected and treated with PZQ alone. The total number of adult worms recovered from individual animals of each group and the numbers of male and female worms are shown in Table 2. On the other hand, the decrease in the hepatic granuloma diameter (P < 0.001; 86.13 ± 1.89 vs. 140.63 ± 1.49) was statistically significant when compared to the group infected and treated with PZQ alone (Table 1).
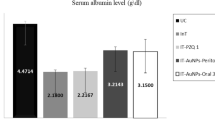
Enzyme assessment
S. mansoni infection significantly increased the serum levels of ALT (P < 0.0001), AST (P < 0.0001), and GGT (P < 0.001), compared to the controls (Table 3). The treatment of mice with PZQ alone or PZQ with ALA recovered the levels of serum, ALT, AST, and GGT relative to the control. The differences in the serum levels of liver enzymes of the group of mice treated with PZQ and ALA were statistically significant when compared to that treated with PZQ alone (Table 3). Moreover, S. mansoni infection significantly decreased the serum level of MMP-1 (P < 0.0001) compared to the control as seen in Table 4. The treatment of mice with PZQ alone or PZQ and ALA increased the serum level of MMP-1 to reach that of the control (Table 4). Furthermore, significant difference in the serum level of MMP-1 was observed between the group treated with PZQ alone and that treated with PZQ and ALA as in Table 4.
Moreover, infection with S. mansoni significantly decreased the tissue level of GSH (P < 0.0001) compared to the control (Table 5). The treatment with PZQ alone or PZQ and ALA has increased the tissue level of GSH to reach that of the control. The treatment of the mice with PZQ and ALA has increased the tissue level of GSH to be very close to that of the control compared to the treatment with PZQ alone as seen in Table 5. Additionally, the infection with S. mansoni significantly increased the tissue level of lipid peroxidase MDA (P < 0.0001) compared to the control (Table 5). Similarly, the treatment with PZQ alone or PZQ and ALA has decreased the tissue level of MDA to be close to that of the control. A significant difference in the tissue level of MDA between the group treated with PZQ alone and that treated with PZQ and ALA was observed as in Table 5.
Histopathological findings
Liver sections of the infected groups (infected without treatment, infected and treated with PZQ alone, and infected and treated with PZQ and ALA) were studied for the granuloma count and size. The histopathological examination showed a significantly greater number of egg granulomas in the infected group than in the treated groups (Table 1 and Fig. 1b, b′, c, d). The mean diameter of granuloma was significantly higher in the treated groups compared to the infected group without treatment (Table 1). Additionally, the number of degenerated ova was higher in the treated groups compared to the infected group without treatment. Sections of the infected and treated mice liver with PZQ alone and with PZQ and ALA showed lesser number of smaller egg granulomas which were usually formed of a central egg surrounded by lymphocytes, epithelioid histiocytes, fibroblasts, and fewer peripherally located eosinophils and neutrophils as in Fig. 1c–d. In contrast, the sections of infected mice liver without treatment revealed greater number of larger egg granulomas which were formed of an ovum surrounded by large number of eosinophils and neutrophils as well as some macrophages and focal area of eosinophilic necrosis as in Fig. 1b′.
Histopathological examination of liver sections of mice infected with S. mansoni or infected and treated with PZQ alone and/or PZQ with ALA. Hematoxylin and eosin (H&E, ×400). a Uninfected mouse liver. b Infected liver with large portal egg granulomas, formed of central ova (arrow) surrounding with concentric layers of hepatic stellate cells (arrowhead) and inflammatory cell infiltration in the form of mononuclear cells especially eosinophils (*). b′ Infected liver with inflammatory cell infiltration in the form of mononuclear cells mainly eosinophils (*). c Section infected and treated by PZQ alone (c) and/or PZQ with ALA (d). Both sections (c and d) are showing regressive granuloma in the portal tract formed of degenerated ova surrounded by giant cells, pigmented macrophages, lymphocytes, plasma cells, and fibrous tissue
Masson’s trichrome staining showed more fibrocellular granulomas with central ova surrounded by inflammatory cells and irregularly deposited collagen fibers in the infected group without treatment (Fig. 2b). Sections of the infected and treated mice liver with PZQ alone and with PZQ and ALA showed smaller fibrocellular granuloma formed of central ova, surrounded by histiocytes, lymphocytes, macrophages fibroblasts, and concentric collagen fibers as seen in Fig. 2c–d. The most important feature concerning the cellular profile of egg granulomas was the percentages of eosinophils and neutrophils which were much greater in the granulomas of the infected group than the infected and treated ones. The percentages of lymphocytes and macrophages were greater in the infected and treated groups than in the infected group without treatment. The percentage of ova containing degenerated miracidia was also greater in the infected and treated groups compared to that in the infected group without treatment.
Histopathological examination of liver sections of mice infected with S. mansoni or infected and treated with PZQ alone and/or PZQ with ALA using Masson trichrome stain ×200. a Uninfected mouse liver with normal distribution of collagen around the central vein and blood sinusoids (arrow). b Infected liver with large egg granulomas, formed of central ova surrounded by inflammatory cells and irregularly deposited collagen fibers (arrow); collagen deposition could also be seen away from the lesion and around the hepatocytes (*). c Section infected and treated by PZQ alone (c) and PZQ with ALA (d): both sections (c and d) are showing smaller fibrocellular granulomas (arrow) formed of central ova, surrounded by histiocytes, lymphocytes, fibroblasts, and concentric collagen fibers that can be seen in inset
Immunohistochemistry
The periovular granuloma in schistosomiasis exhibits strong positivity for metalloproteinase-1 (MMP-1) (brown staining). The center is occupied by a S. mansoni egg. A loose-structured periovular granuloma showed positive staining for MMP-1 in the cytoplasm of fibroblasts, chronic inflammatory cells, and the interstitium. The positivity for MMP-1 was occasionally observed in elongated cells around the schistosome eggs without ground staining (Figs. 3a and 4a). The more active the inflammatory reaction within the granuloma, the more accentuated is the staining for MMP-1. The most positive staining was obtained for MMP-1, which is an interstitial collagenase. Intense staining was regularly seen in one or two rows of hepatocytes bordering the portal spaces or adjacent to the fibrous septa. Staining for MMP-1 was observed at the same time in hepatocytes and within the apical portion of bile duct epithelium. However, in the infected tissue treated with PZQ, only the positive immunoreactivity was noticed in a very few rows of hepatocytes bordering the portal spaces or adjacent to the fibrous septa. Staining for MMP-1 was also observed at the same time in hepatocytes and within the apical portion of bile duct epithelium (Figs. 3b and 4b). Moreover, in the infected tissue treated with PZQ and ALA, the positive immunoreactivity was noticed only in the center of some granulomas and in a few scattered cells within the hepatic parenchyma as shown in Figs. 3c–d and 4c.
Immunohistochemistry staining of liver sections of mice infected with S. mansoni or infected and treated with PZQ alone and/or PZQ with ALA with metalloproteinase-1 (MMP-1). a Infected liver with strong positivity for metalloproteinase-1 (MMP-1) (brown stain). The immunorecreativity appears as a patchy distribution (arrows) among the hepatocytes. There is also a positive staining for MMP-1 in the cytoplasm of fibroblasts, chronic inflammatory cells, and the interstitium (immunohistochemical method for MMP-1, original magnification ×100). b Section infected and treated by PZQ alone with faint immunorecreativity in the hepatic parenchyma (black arrow). Few scattered immunopositive cells are noticed infiltrating the hepatic parenchyma (red arrow) ×100. c Section infected and treated by PZQ and ALA is showing that positive immunorecreativity is present only in the center of some granulomas (arrow) and in few scattered cells within the hepatic parenchyma (red arrow) ×100. d Section infected and treated by PZQ and ALA is showing that positive immunorecreativity is present only in the center of some granulomas (arrow) and in few scattered cells within the hepatic parenchyma (red arrow) ×1,000
Immunolocalization of MMP-1 within the granuloma of mice infected with S. mansoni or infected and treated with PZQ alone and/or PZQ with ALA with metalloproteinase-1 (MMP-1). a Infected section is showing periovular granuloma exhibiting strong positivity for metalloproteinase-1 (MMP-1) (brown stain). The center is occupied by S. mansoni egg and is showing positive immunorecreativity in the center and in the flattened fibroblast-like cells forming a concentric pattern at the periphery (arrow). b This section, infected and treated with PZQ alone, has the same pattern as section (a). c This section, infected and treated with PZQ alone, is showing a negative expression of MMP-1 (no brown stain) except in a few cells (arrows) ×1,000
Discussion
Schistosome eggs induce liver fibrosis which is a common pathological process that can lead to the development of irreversible cirrhosis (Xiong et al. 2003) and inability of the liver to perform its biochemical functions (Rehermann and Nascimbeni 2005). Infection by S. mansoni not only triggers the production of reactive oxygen species especially in mouse liver but also leads to alteration of antioxidant defenses. This oxidative stress might contribute to S. mansoni-associated pathology in humans (Pascal et al. 2000). Glutathione (GSH) plays an important role in the detoxification of reactive oxygen intermediates generated at sites of inflammation (Liang et al. 1991). A decreased concentration of GSH is of pathogenic significance in schistosomiasis. Therefore, increasing the concentration of GSH in target cells and the plasma might be beneficial. Prevention of oxidative stress and lowering the level of intracellular peroxides depend mainly on increasing the level of reduced glutathione (GSH) and promoting its metabolizing enzymes to confront the liberated free radicals (Pocernich et al. 2000). Several studies have reported that under such conditions schistosomiasis is associated with free radical liberation and disturbance in the cellular antioxidant system (Abdallahi et al. 1999; Gharib et al. 1999). Thus, much interest has been focused on compounds that are capable of stimulating glutathione synthesis and acting as antioxidants. One of these compounds which possesses antioxidative properties is ALA. Antioxidants have been suggested as therapeutic options in acute and chronic liver diseases. ALA exerts a strong antioxidant activity. It provides protection from toxic liver damage by elevating intracellular glutathione concentrations (Brown et al. 1997). Treatment of schistosomiasis using PZQ alone is efficacious in reducing morbidity. However, it fails to prevent reinfection or liver fibrosis (Lescano et al. 2004). Accordingly, research into new alternatives for the prevention and cure of schistosomiasis and improvement liver fibrosis has attracted the attention of researchers world wide (Cioli 2000).
In the present study, administration of PZQ alone reduced the total number of adult worms significantly (79%). When the treatment is performed with PZQ and ALA the reduction rate increases to about 83%, which is considered to be statistically significant (P < 0.00001). Note that the significance of this case is compared to the case of infected mice without treatment. The difference of 4% total worm reduction from 79% to 83% is statistically insignificant. However, these two values are significant when compared to the infected group without treatment. This can be attributed to the fact that ALA has no anti-helminthic effect against adult worms. Seif el-Din et al. (2011) have reported similar results. These authors found that the use of the antioxidant (NAC) alone during S. mansoni infection produces a significant increase in the percentage of dead ova. Meanwhile, an enhanced reduction in worm burden by about 85.4% and in hepatic ova count by 68.4% is achieved when the antioxidant (NAC) was administrated with artemether. This result also matches our results since the treatment of S. mansoni infected mice with PZQ and ALA produced a significant reduction in the worm burden and an increase in the percentage of dead ova. The reduction in the worm burden may be attributed to the complementary effects of the antioxidant ALA and PZQ treatments. Nare et al. (1990) reported that schistosome glutathione peroxidase (GPx) is an important antioxidant enzyme protecting S. mansoni by reducing hydrogen peroxide (H2O2) and peroxidized lipid. Consequently, the use of ALA for S. mansoni infection may inactivate or reduce the schistosome GPx enzyme activity. This, in turn, may damage one key survival mechanism of the schistosomes.
Hepatic fibrosis can lead to the development of hepatic cirrhosis with the risk of liver failure and hepatocellular carcinoma (Bataller and Brenner 2005). In liver fibrosis, normal hepatic tissue is replaced with collagen-rich extracellular matrix. Hepatic fibrosis is also capable of generating oxygen radicals, inhibiting glutathione synthesis, producing glutathione loss from the tissue, thus increasing malondialdehyde levels and impairing antioxidant defense systems in humans and experimental animals. Lipid peroxidation results from the increased oxygen radical production (Castillo et al. 1992). Lipid peroxidation is not only a reflection of tissue damage but also plays a pathogenic role, such as promoting collagen production (Geesin et al. 1991; Lieber 1994). The removal of the toxic metabolites is believed to be the vital initial step in providing cell survival during treatment of liver fibrosis (Nordmann et al. 1992). The results of our study showed that administration of ALA and PZQ in the treatment regimen of S. mansoni infected mice diminishes oxidative stress by increasing antioxidant enzymes. The antioxidant used in this study has the capacity to prevent collagen accumulation and to improve the histological architecture of the liver. Histopathological examination of liver samples with H and E and/or Masson's trichrome stains showed an improvement effect of PZQ and ALA on the liver tissue. Improvement of hepatic pathology (in the form of reducing the size and the number of granulomas) with improvement of hepatocytes (viability and plating efficiency) indicates a status of structural integrity of liver cells which provides further support to the suggestive mechanism of action. The protection afforded by both ALA and PZQ appears to be superior to PZQ only.
Many studies demonstrated that there is a parallel increase in collagen and collagenase synthesis in the liver during the early murine infection with S. mansoni (e.g., Takahashi et al. 1980). Collagenase activity was demonstrated by immunohistochemistry in periovular granulomas formed in the liver of infected mice by several researchers (Dunn et al. 1979; Takahashi et al. 1980; Biempica et al. 1983). Both active and inactive collagenases are secreted simultaneously with the activity of collagen synthesis during the formation of periovular granuloma in the mouse liver (Emonard and Grimaud 1989).
ALA is seen to be the most effective antioxidant as shown in the present study. ALA decreased hepatic lipid peroxidation and GSH depletion. GSH plays an important role in antioxidant defense directly through scavenging of reactive oxygen species and indirectly through functions as a cofactor of antioxidant enzymes (Franco et al. 2007). Remodeling fibrillar collagen in rodents has been attributed to the action of MMP-1. The antioxidant used in the current study resulted in an increase in serum MMP-1 levels. ALA is capable of increasing serum concentration of MMP-1 through hepatic stellate cell activation, which is considered as a critical step in hepatic regeneration.
The immunohistochemistry expression of MMP-1 protein was inversely proportional to the MMP-1 expression in the serum since the treatment with PZQ and ALA activates the hepatic stellate cells as well as hepatocytes. Therefore, secretion of MMP-1 has been increased in the serum (Zhang et al. 2003). The antifibrotic effects of the ALA with PZQ appear to stem from their antioxidant activities as indicated by protection against the increased lipid peroxidation and the decreased GSH contents (Ito et al. 2005). In the present work, a significant increase in serum ALT, AST, and GGT level was observed in S. mansoni-infected mice. Normalization in serum ALT, AST, and GGT levels in the treated infected group with PZQ alone or with PZQ and ALA has been observed. These findings are in agreement with those obtained by Hammad et al. (2000), Ezzat et al. (2001), Mahmoud et al. (2002a, b), and Seif el-Din et al. (2006). These studies reported increase in serum ALT and GGT levels in bilharzial patients and experimental animals. Subsequently, normalization in these serum levels in S. mansoni-infected mice treated with antioxidant (NAC) has been detected. Note that ALT, AST, and GGT enzymes are commonly employed as biological markers for hepatic cell damage and impaired cell membrane permeability or heavy Schistosoma egg deposition as reported by El-Shenawy and Soliman (2003). Serum levels of the aforementioned enzymes have increased in the infected group without treatment when compared with groups treated with a single drug or two drugs. Restoration of serum transaminases, ALT, AST, and GGT to normal levels can be explained by restoration of oxidant/antioxidant balance by administration of antioxidants. The studied parameters (parasitological biochemical and histopathological) indicate a status of structural and functional integrity of liver cells. Moreover, this provides further support to the suggested mechanism of action. Accordingly, the protection afforded by both ALA and PZQ sounds to be superior to PZQ only.
Conclusion
This paper has investigated the effect of the combined treatment (PZQ + ALA) on liver fibrosis induced by S. mansoni challenged mice. It was found that alpha lipoic acid has a synergistic effect with praziquantel on improvement of hepatic fibrosis induced by S. mansoni infection. Therefore, it is better to combine alpha lipoic acid with praziquantel in treatment regimen of S. mansoni-infected patients for better improvement of schistosomiasis-induced fibrosis. Improvement of fibrosis will prevent cirrhosis and associated morbidity and mortality as liver fibrosis is a central event in progressive liver disease.
References
Abdallahi OM, Hanna S, De Reggi M, Gharib B (1999) Visualization of oxygen radical production in mouse liver in response to infection with Schistosoma mansoni. Liver 19:495–500
Bataller R, Brenner DA (2005) Liver fibrosis. J Clin Invest 115:209–18
Biempica L, Takahashi S, Biempica S, Kobayashi M (1983) Immunohistochemical localization of collagenase in hepatic murine schistosomiasis. J Histochem Cytochem 31:488–494
Biewenga GP, Haenen GR, Bast A (1997) The pharmacology of the antioxidant lipoic acid. Gen Pharmacol 29:315–31
Brown KE, Poulos JE, Li L, Soweid AM, Ramm GA, O’Neill R, Britton RS, Bacon BR (1997) Effect of vitamin E supplementation on hepatic fibrogenesis in chronic dietary iron overload. Am J Physiol 272:G116–G123
Buege JA, Aust SD (1978) Microsomal lipid peroxidation. Methods Enzymol 52:302–10
Castillo T, Koop DR, Kamimura S, Triadafilopoulos G, Tsukamoto H (1992) Role of cytochrome P-450 2E1 in ethanol-, carbon tetrachloride- and iron-dependent microsomal lipid peroxidation. Hepatology 16:992–996
Cheever AW (1968) Condition affecting the accuracy of potassium hydroxide digestion technique for counting Schistosoma mansoni eggs in tissue. Bull World Health 39:328–31
Cioli D (2000) Praziquantel: is there real resistance and are there alternatives? Curr Opin Infect Dis 13:659–663
Dabski H, Brzeski Z (1970) Treatment of chronic diseases of the liver parenchyma with thioctic acid. Pol Tyg Lek 25:899–901
Dunn MA, Kamel R, Kamel IA, Biempica L, Kholy AE, Hait PK, Rojkind M, Warren KS, Mahmoud AA (1979) Liver collagen synthesis in schistosomiasis mansoni. Gastroenterology 76:978–82
Dünschede F, Erbes K, Kircher A, Westermann S, Seifert J, Schad A, Oliver K, Kiemer AK, Theodor J (2006) Reduction of ischemia reperfusion injury after liver resection and hepatic inflow occlusion by alpha-lipoic acid in humans. World J Gastroenterol 12:6812–7
Duvall R, DeWitt W (1967) An improved perfusion technique for recovering adult schistosomes from laboratory animals. Am J Trop Med Hyg 16:483–6
Seif el-Din SH, Ebeid FA, Badawy AA, Ezzat AR (2006) Protective effects of β-carotene, N-acetyl-cysteine with and without praziquantel treatment in Schistosoma mansoni-infected mice. Egyptian J Schistosomiasis Infect Endemic Dis 28:67–90
Seif el-Din SH, Al-Hroob AM B, Ebeid FA (2011) Schistosoma mansoni: N-acetylcysteine downregulates oxidative stress and enhances the antischistosomal activity of artemether in mice. Exp Parasitol 128:230–235
El-Shenawy NS, Soliman MFM (2003) Evaluation of the protective effect of two antioxidative agents in mice experimentally induced with Schistosoma mansoni: biochemical and parasitological aspects. J Egypt Ger Zool 40(A):201–216
Emonard H, Grimaud JA (1989) Active and latent collagenase activity during reversal of hepatic fibrosis in murine schistosomiasis. Hepatology 10:77–83
Ezzat AR, Seif el-Din SH, Ebeid FA (2001) Effect of praziquantel treatment on the activities of some liver microsomal enzymes in mice infected with S. mansoni. Arzneimittelforschung 51:325–331
Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI (2007) The central role of glutathione in the pathophysiology of human diseases. Arch Physiol Biochem 113:234–58
Geesin JC, Hendricks LJ, Falkenstein PA, Gordon JS, Berg RA (1991) Regulation of collagen synthesis by ascorbic acid: characterization of the role of ascorbate-stimulated lipid peroxidation. Arch Biochem Biophys 290:127–132
Gharib B, Abdallahi OM, Dessein H, De Reggi M (1999) Development of eosinophil peroxidase activity and concomitant alteration of the antioxidant defenses in the liver of mice infected with Schistosoma mansoni. J Hepatol 30:594–602
Hammad H, Sherif S, Ebeid F (2000) Effect of praziquantel on some biochemical aspects in experimental schistosomiasis. Recent Res Dev Biotechnol Bioeng 3:107–118
Harvie M, Jordan TW, La Flamme AC (2007) Differential liver protein expression during schistosomiasis infection and immunity. Infect Immun 75: 736-744
Hirsch C, Zouain CS, Alves JB, Goes AM (1997) Induction of protective immunity and modulation of granulomatous hypersensitivity in mice using PIII, an anionic fraction of Schistosoma mansoni adult worm. Parasitology 115:21–2
Horáková O, Kostír J, Horák F (1967) The hepatotropic effect of alpha-lipoic acid. Cesk Farm 16:129–33
Hsu SM, Raine L, Protein A (1981) Avidin and biotin in immunohistochemistry. J Histochem Cytochem 29:1349–53
Iasinovskii MA, Terletskaia TM, Bondarchuk AF (1969) Use of lipoic acid in complex therapy of patients with liver diseases. Vrach Delo 5:9–12
Ito K, Kajikawa S, Nii A, Doi K (2005) Nitrofurazone-induced gene expressions in rat hepatocytes and their modification by N-acetylcysteine. Exp Toxicol Pathol 56:333–339
Ivkov VG (1969) Lipoic (thioctic) acid and its significance in hepatology. Sov Med 32(10):122–8
Junqueira L, Montes G, Toledo O, Joarzeino P (1986) Morphological, histochemical and biochemical observations on the connective tissue matrix of in situ and isolated hepatic granulomas in experimental murine schistosomiasis. Ann Trop Med Parasitol 80:27–41
Lescano SZ, Chieffe PP, Canhassi RR, Boulos M, Amato Neto V (2004) Antischistosomal activity of artemether in experimental schistosomiasis mansoni. Rev Saude Publica 38:71–75
Liang SM, Liang CM, Hargrove ME, Ting CC (1991) Regulation by glutathione of the effect of lymphokines on differentiation of primary activated lymphocytes. Influence of glutathione on cytotoxic activity of CD3-AK. J Immunol 146:1909–1913
Lieber CS (1994) Alcohol and the liver update. Gastroenterology 106:1085–1105
Mahmoud MR, EI-Abhar HS, Saleh S (2002a) The effect of Nigella sativa oil against liver damage induced by Schistosoma mansoni infection in mice. J Ethnopharmacol 79:1–11
Mahmoud MR, Zoheiry MMK, Nosseir MF (2002b) Effect of combined chemotherapy and anti-inflammatory drugs on murine schistosomiasis. Arzneimittelforschung 52:294–301
Melhem MF, Craven PA, DeRubertis FR (2001) Effects of dietary supplementation of α-lipoic acid on early glomerular injury in diabetes. J Am Soc Nephrol 12:124–133
Möller E, Brinkmann W, Weber O, Wildhirt E (1967) Treatment of chronic liver diseases with thioctic acid. Med Klin 62:380–4
Morsy GH (2009) Parasitological and histo-pathological studies on schistosomiasis mansoni infected mice and treated with praziquantel and/or oltipraz. J Egypt Soc Parasitol 39:687–701
Murawaki Y, Ikuta Y, Idobe Y, Kawasaki H (1999) Serum matrix metalloproteinase-1 in patients with chronic viral hepatitis. J Gastroenterol Hepatol 14:138–45
Nare B, Smith JM, Prichard RK (1990) Schistosoma mansoni: levels of antioxidants and resistance to oxidants increase during development. Exp Parasitol 70:389–397
Nordmann R, Ribiere C, Rouach H (1992) Implication of free radical mechanisms in ethanol-induced cellular injury. Free Radic Biol Med 12:219–240
Oliver L, Stirewalt MA (1952) An efficient method for the exposure of mice to cercariae of S. mansoni. J Parasitol 39:19–23
Pascal M, Abdallahi OM, Elwali NE, Mergani A, Qurashi MA, Magzoub M, de Reggi M, Gharib B (2000) Hyaluronate levels and markers of oxidative stress in the serum of Sudanese subjects at risk of infection with Schistosoma mansoni. Trans R Soc Trop Med Hyg 94:66–70
Pellegrino J, Oliveria CA, Faria J, Cunha A (1962) New approach to the screening of the drugs in experimental Schistosoma mansoni in mice. Am J Trop Med Hyg 1:201–15
Pocernich CB, La Fontaine M, Butterfield DA (2000) In-vivo glutathione elevation protects against hydroxyl free radical-induced protein oxidation in rat brain. Neurochem Int 36:185–191
Rehermann B, Nascimbeni M (2005) Immunology of hepatitis B virus and hepatitis-C virus infection. Nature Rev Immunol 5:215–229
Romanov VS (1971) Use of lipoic acid and its amide in chronic liver diseases. Sov Med 34:43–5
Smithers RS, Terry RJ (1965) The infection of laboratory hosts with cercariae of S. mansoni and the recovery of worm. Parasitology 55:695–700
Takahashi S, Dunn MA, Seifter S (1980) Liver collagenase in murine schistosomiasis. Gastroenterology 78:1425–1431
Tendler M, Pinto RM, Lima AO, Gebara G, Katz N (1968) Schistosoma mansoni: vaccination with adult worm antigen. Int J Parasitol 16:347–352
Xiong LJ, Zhu JF, Luo DD, Zen LL, Cai SQ (2003) Effects of pentoxifylline on the hepatic content of TGF-β1 and collagen in schistosomiasis japonica mice with liver fibrosis. World J Gastroent 9:152–154
Zhang BB, Cai WM, Weng HL, Hu ZR, Lu J, Zheng M, Liu RH (2003) Diagnostic value of platelet derived growth factor-BB, transforming growth factor-beta matrix metalloproteinase-1 and tissue inhibitor of matrix metalloproteinase-1 in serum and peripheral blood mononuclear cells for hepatic fibrosis. World J Gastroenterol 9:2490–6
Zou WL, Yang Z, Zang YJ, Li DJ, Liang ZP, Shen ZY (2007) Inhibitory effects of prostaglandin E1 on activation of hepatic stellate cells in rabbits with schistosomiasis. Hepatobiliary Pancreatol Distrib Int 6:176–181
Acknowledgments
The authors would like to thank Prof. Nabil S. Gabr, Head of the Department of Parasitology, Faculty of Medicine, Minia University, Egypt, for his continuous advice in technical procedures. Thanks are extended to Prof. Nawras M. Mowafy, Professor of Parasitology, Faculty of Medicine, Minia University for her guiding us through the technical procedures. The authors would also like to thank Prof. Refaat M. A. Khalifa, Professor of Parasitology, Faculty of Medicine, Assuit University for his continuous advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel-Hafeez, E.H., Ahmad, A.K., Abdulla, A.M. et al. Therapeutic effect of alpha lipoic acid combined with praziquantel on liver fibrosis induced by Schistosoma mansoni challenged mice. Parasitol Res 111, 577–586 (2012). https://doi.org/10.1007/s00436-012-2871-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-012-2871-4