Abstract
The combined immuno-chromographic-malaria dipstick (ICT) for the rapid diagnosis of malaria detects both Plasmodium falciparum (P.f.)-specific, histidine-rich protein 2 (HRP-2) and a plasmodial aldolase expressed by all Plasmodium species pathogenic to humans. ICT was applied in 674 febrile returnees from malaria-endemic regions attending our Tropical Diseases Unit. Microscopy confirmed malaria in 69/674 cases, of whom 67/69 had returned from Africa or Madagascar, and 2/69 from the Caribbean. Monoparasitic P.f. infection occurred in 52/69, mixed infection was due to P.f.+P. ovale (P.o.) in 3/69, and P.f.+P. malariae (P.m.) in 1/69 cases. Monoparasitic P. vivax (P.v.) infection occurred in 8/69, P.o. in 3/69, and P.m. in 2/69 cases.
Whereas a positive HRP-2 band on the test was a highly sensitive indicator for P.f. infection (52/52 patients; sensitivity 100%), this was not the case for a positive aldolase band (25/52 patients; sensitivity 48.1%). Sensitivity of aldolase band for non-falciparum plasmodia was even lower: aldolase was positive in only 3/8 (37.5%) of patients with vivax malaria, and in 0/5 cases with P.o.- or P.m. infection. Co-reaction of both bands occurred more frequently in patients with P.f. parasitaemia of ≥40,000/μl (20/25, 80.0%) as compared to patients with P.f. parasitaemia <40,000/μl (5/27, 18.5%; P<0.00005), and to patients with mixed infection (P.f.+P.o., P.f.+P.m.: 2/4, 50.0%; diff. n.s.).
In our series, co-reaction of HRP-2 and aldolase indicated monoparasitic falciparum malaria with high P.f. parasitaemia, rather than mixed infection. Whereas the aldolase band is not a reliable qualitative marker for malaria, co-reaction of HRP-2 and aldolase band may have a potential for indicating high parasitaemia in falciparum malaria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A combined immuno-chromographic-malaria dipstick (ICT) allowing the diagnosis of malaria within minutes has been marketed since 1999 (Malaria-now, Binax, Portland, USA). The test detects parasite antigens in whole blood by binding to specific antibodies, and a subsequent colour reaction produces visible bands on the dipstick: “C” represents the control band, “T1” is the band with antibodies to P.f.-specific, histidine-rich-protein 2 (HRP-2), and “T2” means a band with reaction of antibodies to a plasmodial aldolase. This latter band was primarily introduced to detect vivax malaria, but since aldolase is a pan-plasmodial antigen, it is deemed to react in infections due to all Plasmodium spp. pathogenic to humans.
ICT tests performed between February 1999 and May 2004 were analysed in 674 patients (age 2–78 years, median 29 years) who presented in our Tropical Medicine Unit because of fever after a recent stay in a malaria-endemic area. Patients who had had anti-malarial treatment within 4 weeks were excluded from analysis. The ICT was performed by physicians and laboratory assistants experienced with malaria dipsticks. The manufacturer’s instructions were strictly followed. Results were compared to those of expert microscopy for asexual parasites by Giemsa-stained thick and thin blood films. Parasitaemia was assessed in the thick blood film and related to microlitre of blood according to current standards (White 2002). All patients were followed up until blood films had cleared from parasites.
Microscopy revealed malaria parasites in 69/674 patients investigated (Table 1): 67/69 of infections were acquired in Africa or Madagascar, 2/69 in America and the Caribbean. In all, 52/69 patients had monoparasitic falciparum malaria; 4/69 had P.f.+non-falciparum plasmodia mixed infections, and 13/69 had monoparasitic non-falciparum malaria.
Sensitivity of P.f.-specific HRP-2 was 100.00% in both monoparasitic P.f. infections (52/52) and in mixed infections (4/4). False positive HRP-2 results were not observed in 605 microscopically negative controls. Surprisingly, the sensitivity of the aldolase band was higher in falciparum malaria (25/52, 48.1%) than in non-falciparum malaria (3/13, 23.1%; diff. n.s.); only 37.5% (3/8) of patients with vivax malaria had a positive aldolase band; in the cases of P.o. and of P.m. infection, aldolase did not react at all. Two false positive aldolase reactions were observed: one in a patient with acute infectious mononucleosis, another in a case with stage 1–2 luetic infection.
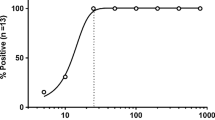
In all, 25/52 (48.1%) patients with monoparasitic falciparum malaria had co-reacting HRP-2 and aldolase bands. The aldolase band co-reacted significantly more frequently in falciparum malaria with elevated parasitaemia: 20/25 (80.0%) patients with a parasitaemia of ≥40,000 parasites/μl had a positive aldolase band as compared to only 5/27 (18.5%) with <40,000 parasites/μl [P<0.00005, Yates-corrected; RR=4.32 (1.91<RR<9.76), OR 17.6 (95% CI: 3.75<OR<93.08)]. Mixed infections were infrequent in our series (Table 1): only in 2/4 cases HRP-2 and the aldolase band co-reacted. In the remaining 2/4, the HRP-2 band but not the aldolase band reacted (two Cameroonian girls with P.f.+P.o. infection). In all four cases, P.f. parasitaemia was lower than 40,000 parasites/μl.
In 22 patients monitored by ICT after treatment, the HRP-2 band turned negative around the 20th day after beginning therapy (range 10–31). The aldolase band turned negative within 9 days post-therapy in all patients. Whereas the high sensitivity and specificity of the HRP-2 band for falciparum malaria was confirmed, this was not the case for the aldolase band, neither in falciparum nor in non-falciparum malaria (Iqbal et al. 2002; Playford and Walker 2002; Richter et al. 2004). In our series of cases with preponderance of malaria acquired in Africa, co-reaction of the aldolase band with the HRP-2 band indicated monoparasitic P.f. infection with elevated parasitaemia, rather than mixed infections.
If developed and standardised further, e.g. by standardised automatic reading of the change in coloration of the bands on the test, the combined ICT may have a potential for semi-quantitation of parasitaemia in falciparum malaria.
References
Iqbal J, Khalid N, Hira PR (2002) Comparison of two commercial assays with expert microscopy for confirmation of symptomatically diagnosed malaria. J Clin Microbiol 40:4675–4678
Playford EG, Walker J (2002) Evaluation of the ICT malaria P.f./P.v. and the OptiMal rapid diagnostic tests for malaria in febrile returned travellers. J Clin Microbiol 40:4166–4177
Richter J, Harms G, Müller-Stöver I, Göbels K, Häussinger D (2004) Performance of an immuno-chromatographic-test (ICT) for the rapid diagnosis of malaria. Parasitol Res 6:518–519
White NJ (2002) Malaria. In: Cook GC, Zumla A (eds) Manson’s tropical diseases, 21st edn. Saunders, London, pp 1205–1295
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Richter, J., Göbels, K., Müller-Stöver, I. et al. Co-reactivity of plasmodial histidine-rich protein 2 and aldolase on a combined immuno-chromographic-malaria dipstick (ICT) as a potential semi-quantitative marker of high Plasmodium falciparum parasitaemia. Parasitol Res 94, 384–385 (2004). https://doi.org/10.1007/s00436-004-1213-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-004-1213-6